SLHS 340 Unit 4 Test
1/86
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
87 Terms
What questions do you ask during case history for children?
-Were there any difficulties at birth?
-Any medications during pregnancy?
-Any physical trauma?
-Any Confirmed illness, disease, disorders, or disabilities?
-History of Ear Infections?
-Is there a family history of HL?
-When did the parent suspect a problem?
-What amount of HL do they suspect?
For Pediatrics are you more interested in finding out the DEGREE or TYPE of hearing loss?
Type-sensorineural, mixed, conductive
Physical Problems for Children w/ HL
Pain, drainage, dizziness, tinnitus, fullness
Perceptual Problems for Children w/ HL
Delayed speech development, child does not respond, slurred speech
What test is used during a Newborn Hearing Screening?
OAEs and ABRs
OAEs measure
Outer Hair Cell function
ABRs measure
Neural function
If a child needs further testing during newborn hearing screening, what is the first thing you do?
RETEST
Steps for testing Pediatrics:
1. Otoscopy
2. Tympanogram
3. Behavioral Testing
4. Speech Perception(if possible)
If a child has a type A tymp then that is confirmation that...
Air and Bone are overlapping; sensorineural
If behavioral testing is abnormal or inconclusive (with normal middle-ear function), then
Test OAE & ABR
-OAEs to evaluate inner ear function
-ABRs to determine degree of hearing loss
In the sound field
Stimuli presented through speakers in a sound-treated room, no headphones (Problems — do not know what ear is responding
-Positive reinforcer (R+) - an illuminating animated toy
Variability occurs with determining a minimum response level or threshold. Why?
What is considered a reliable reaction
Three types of Behavioral Testing
-Behavioral Observation Audiometry(BOA)
-Visual Reinforcement Audiometry (VRA)
-Conditioned Play Audiometry(CPA)
Behavioral Observation Audiometry(BOA)
-Used for infants up to 4-6 months.
-Relies on unconditioned responses
-Careful observation of any change in the infant's behavior.
Potential Problems with BOA
-Sound field does not provide ear specific information.
-Reliability and validity may be questionable.
-No threshold information.
-OAEs and ABRs can provide a more complete assessment.
Visual Reinforcement Audiometry (VRA)
-Used for children 5 months to 2 or 3 years.
-Relies on the child's ability to localize by turning toward the source of the sound.
Conditioning Phase for VRA
-Acoustic stimuli is presented at a level at which the child should be able to hear.
-Pair the presentation of the stimuli with positive reinforcement (e.g. Illuminating, moving toy)
Testing Phase for VRA
-Present the acoustic stimuli alone
-Child associates the sound with the positive reinforcement and looks in that direction.
-After a response is noted, decrease the level again in an attempt to determine threshold.
Potential problems with VRA
-May not be able to use earphones and obtain ear-specific information.
-Possible interference from the parent.
-May need more specific information from OAEs and/or ABRs.
Conditioned Play Audiometry(CPA)
-Used with children from 2 to 5 years.
-Conditioned motor response to acoustic stimuli.
-Dropping a block in a bucket, placing a ring onto a post with the assistance of a second audiologist.
Conditioning Phase for Conditioned Play
-With both the child and the second audiologist under earphones, the audiologist prompts the child to put a block in the bucket when a tone is presented through the earphones.
-This is done until the child puts the block in the bucket independently.
Testing phase for Conditioned Play
-Prompting by audiologist is removed.
-Thresholds are obtained.
Potential Problems with Conditioned Play
-Children are required to wear earphones.
-Child has to wait for the stimuli before responding.
-Motivation
True or False: If someone has a hearing loss that automatically means they need a hearing aid
False
What fraction of the world's population of people 65 and older are affected by hearing loss?
one third
Causes of hearing loss from in the womb to adulthood
-Prenatal period: Genetic factors
-Perinatal period: Lack of oxygen at birth (ototoxic medication), Low-birth weight
-Childhood and adolescence: Chronic middle ear infections, Meningitis
-Adulthood and older age: Chronic diseases, Smoking, Presbycusis
Psychophysical Consequences of HL
Recruitment, Loss of frequency resolution, Loss of temporal resolution
Loss of frequency resolution — Psychophysical Consequences of HL
reduction in the ability of the cochlea to separate complex sounds into the individual components.
Listening in background noise is more difficult.
More difficult to differentiate between frequencies
LOSS OF TEMPORAL RESOLUTION — Psychophysical Consequences of HL
reduction in the ability of the auditory system to detect changes in sound over time.
Problems with voice onset time (VOT) and other time characteristics of speech
RECRUITMENT — Psychophysical Consequences of HL
Abnormal sensitivity to loudness and a reduced dynamic range
Affects speech perception.
Has implications of the types of amplification used for intervention.
Hearing loss with age (EHLS)
-14.6% of participants with hearing loss were current hearing aid users.
-A substantial majority of older adults with hearing loss are not using hearing aids.
-30% reduction in word rec scores(bottom half) because they added a background noise
Voice Onset time
the interval between the release of a stop consonant and the onset of vocal cord vibrations
Signal to noise ratio
it becomes harder to detect a signal as background noise increases
Aural rehabilitation
person had hearing, then they lost it, and they want to gain some back
Aural habilitation:
Never had hearing, but wanting to hear
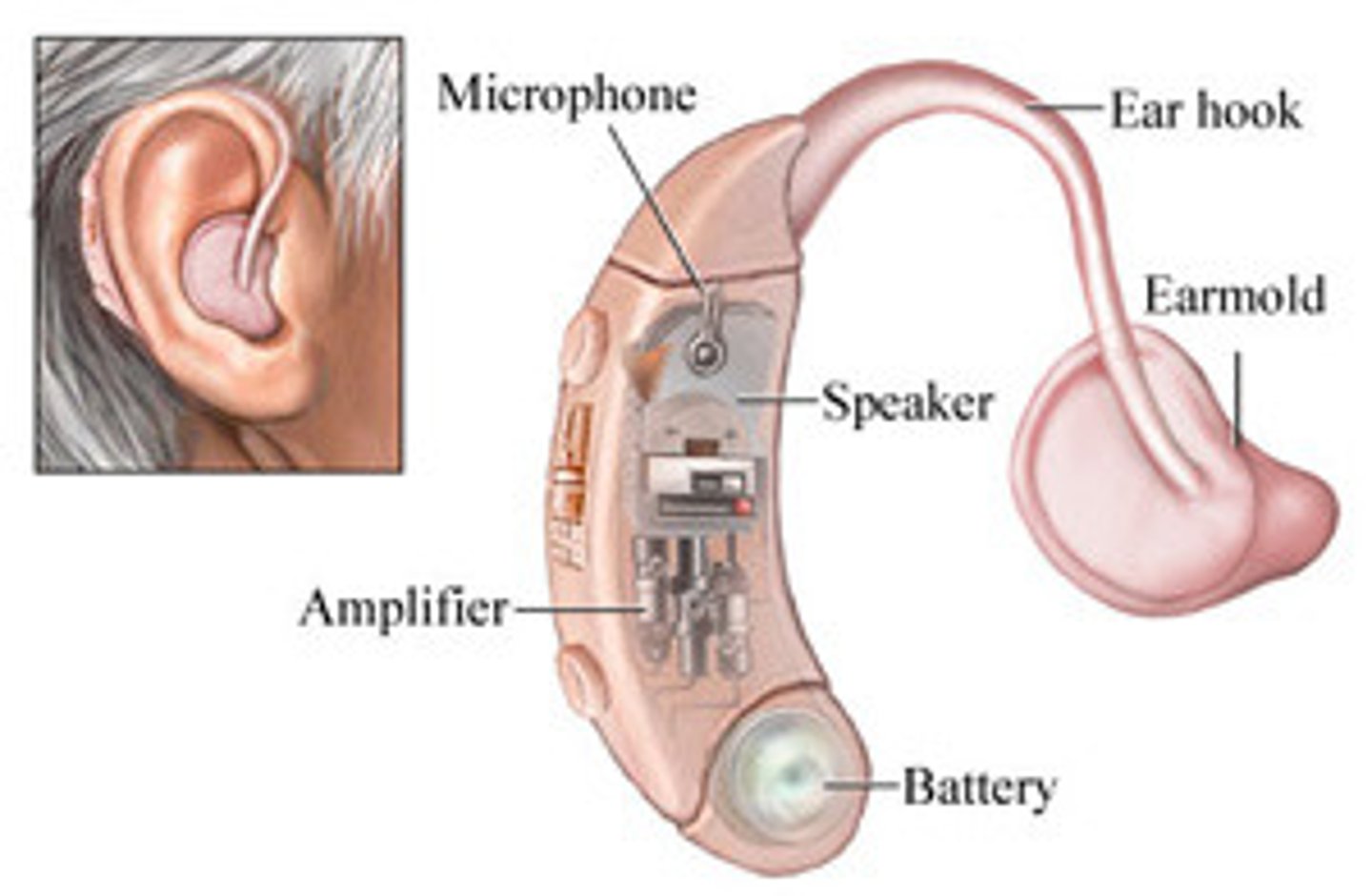
Behind the ear(BTE) aids
-Used for mild to profound hearing losses.
-Bigger instruments — more room for the electroacoustic components, specifically more gain (amplification)
-More beneficial for older individuals with dexterity problems.
-Microphone is on top of BTE, pinna does not help
In the Ear(ITE) aid
-Use for mild to profound hearing losses.
-Because of the placement of the aid, utilizes the pinna
-Not used as much because of advances in technology
-Microphone is on top of the concha and fills entire concha

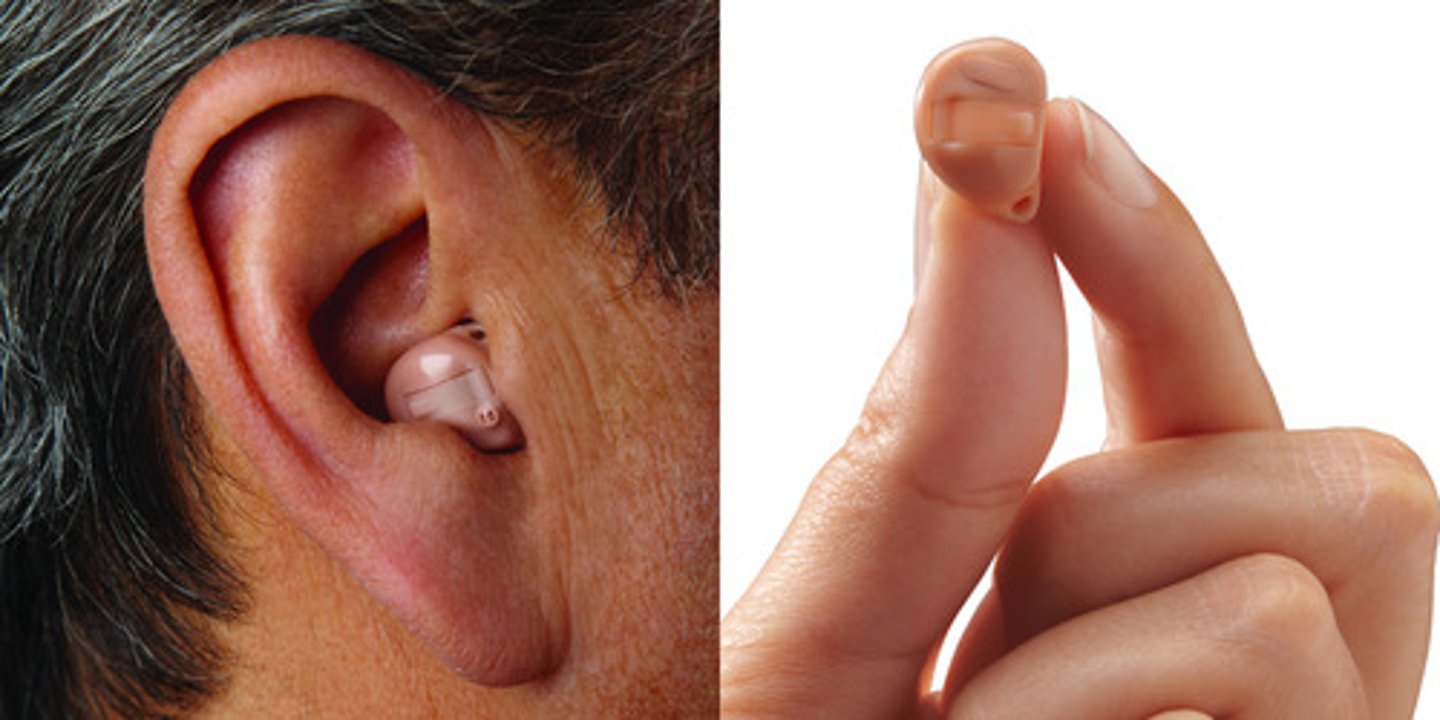
In the Canal (ITC) and Completely in the Canal (CIC)
-Used for mild to severe hearing losses.
-NOT FOR PROFOUND (too small)
-Slightly less power because of the SIZE of the instrument.
-Provides more gain(amplification) at higher frequencies because of the acoustic resonance of the ear canal.
-CIC — All pinna, concha, and some ear canal
Receiver in the canal (RIC) or Receiver in the ear (RITE) aids
-Used for all degrees of hearing loss.
-Discreet fitting.
-Reduced feedback(whistle sound) and occlusion effect.
-More comfortable than other hearing aids

Occlusion effect
plugged up and hear yourself via bone conduction
Bone Conduction or Bone-Anchored
-Oscillator placed directly on the mastoid to transmit stimuli to the cochlea.
-Snap surgically implanted into mastoid and the hearing aid clips into the snap.
-This is for conductive hearing loss when it cannot be fixed if referred out. Non repairable conductive loss
-sound localization difficulties (bone conduction stimulates both cochlea)

Localization
the ability to determine the location of a sound source, including its direction and distance, based on the sound waves received by the ears
1. power supply
2. microphone
3. amplifier/processor
4. Receiver
5. Earmorlds
Hearing aid components
Power supply-hearing aid
usually zinc-air or mercury zinc batteries.
Microphone on hearing aid
converts the acoustic signal into an analog/digital electrical signal.
Amplifier/Processor for HA
increases the level of the electrical signal
Receiver for HA
converts the amplified electrical signal back to an acoustic (or vibratory for bone aids) signal.
Earmold for HA
relatively air-tight fit in the canal to not get any feedback.
Wireless FM system
-Wireless FM system receiver that clips to shirt and connects directly to the hearing aid.
-The teacher/speaker wears a similar looking device, but is a microphone and transmitter.
-Volume control shown is used to control the volume of the FM signal received.
Earmold impression steps
1) do otoscopy (no occluding wax)
2) put a cotton block deep into the ear canal
3) do otoscopy for the second time (make sure the cotton block is completely occluding the ear canal)
4) Put two solutions together and put in a plunger and put the impression as tight as you can into the ear canal and concha. Might go all the way up to the helix
5) Takes 4-5 mins to set
6) Take the impression out carefully (move pinna, patient opens and closes mouth)
7) Do otoscopy for the last time to make sure nothing was leftover (there may be redness in ear canal)
Otoscopy is very important for this!!!
Programmable hearing aids
-Adjusted by a hand-held programmer or by computer software.
-Visualize changes to hearing aid characteristics on a display.
-Utilize pure-tone data, loudness discomfort levels, and other audiometric data to obtain target satisfaction with the hearing aid.
Multiple-Memory Hearing Aids
-The frequency response(what the hearing aid is putting out into the persons ear) and maximum output of the hearing aids can be changed by the individual depending on the listening environment.
-The first program can be used in a relatively quiet environment.
-And the second can be used in a moderately noisy environment.
What type of hearing aid is preferred for children?
behind the ear (ear canal grows)
Assistive listening devices
-Any non-hearing aid device designed to improve the ability of an individual with any hearing loss to communicate and to function more independently
-Done either by transmitting AMPLIFIED sound more directly from its source or by transforming it into a tactile or visual signal
-FOR HEARING AID HATERS
Assistive Listening Devices
Hardwire System, Infrared System, FM System
Hardwire system
-This system provides a direct physical connection from the sound source to the listener
-Used in nursing homes, doctor's offices, or at home
-easier to operate because of larger controls
-physically connected to another unit

Infrared system
-Sound is converted to infrared light waves and transmitted throughout the listening environment
A receiver worn by the individual changes the light waves back into the amplified signal
-Used in movie theaters, for TV, churches, and work environment
-more mobility
-can only be used in closed rooms (INfrared — INside
FM System
-Sound is converted into FM waves and transmitted to the listener using a microphone and receiver worn by the individual
-Used primarily in educational settings
-can be used outdoors or in any indoor facility
-can pick up interference from other wireless signals passed along the same FM wave
Patient has high WR% but mild HL (what intervention)
Either nothing (cost), or fit for hearing aids
Task of all assistive listening devices
Improve SNR
With hardwire and infrared systems you can only adjust volume
With FM you can adjust volume and frequency components
World's youngest recipient of Bilateral CI surgery
9 months old
Cochlear Implant components
Microphone
Speech processor
Transmitter
receiver/stimulator
Electrode array
Cochlea
Auditory nerve
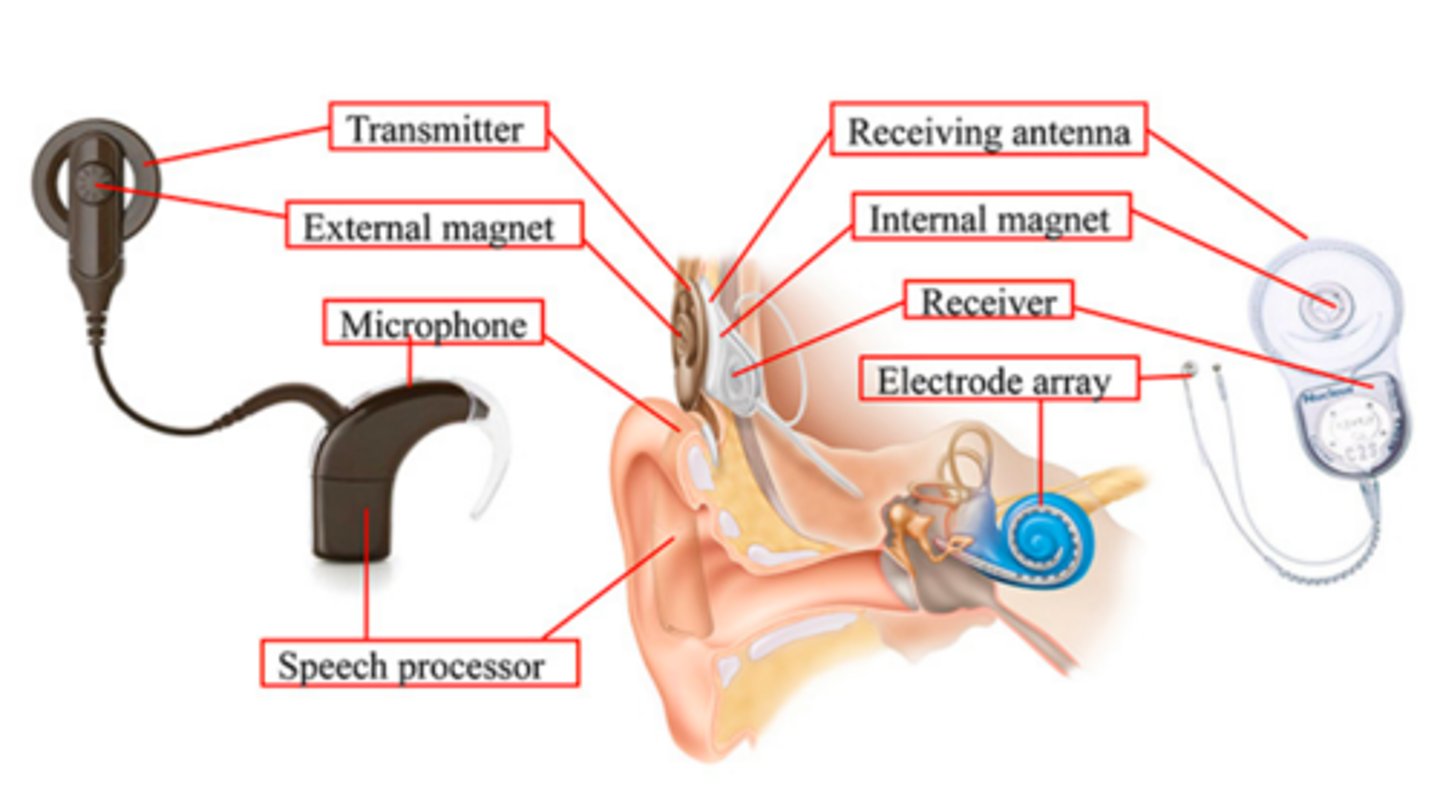
How do cochlear implants work?
1. External speech processor captures sound and converts it into digital signals
2. Processor sends digital signals to internal implant
3. Internal implant turns signals into electrical energy, sending it to an array inside the cochlea
4. Electrodes stimulate hearing nerve, bypassing damaged hair cells, and the brain perceives signals; you hear sound
Internal components of cochlear implants
electrode array and internal receiver/stimulatory
Electrode array
lays adjacent to the basilar membrane and transmits the electrical signal to the auditory nerve fibers.
Evolved from 1 electrode/channel to 8- 22 electrodes.
Disadvantage - each channel is larger than the frequency region for which it is substituting (less precise; more robotic)
Internal receiver/stimulatory for CI
placed in the mastoid of the skull.
Receives information from the external components and conveys that information to the electrode array
External components of Cochlear implants
microphone, speech processor, transmitter
Microphone-CI
collects auditory information and delivers it to the speech processor.
Speech processor-CI
computerized filtering system that converts sound wave information to electrical impulses to enhance speech perception.
Transmitter CI
sends coded information across the skin to the internal receiver
Speech processor
Worn at the ear level and it resembles a BTE.
simulates speech, it does not replicate speech (CI sounds more mechanicial)
Cochlear implant candidacy for children
<12 months: severe-profound bilateral sensorineural hearing loss.
>12 months: moderately-severe to profound sensorineural bilateral hearing loss and gap in auditory/language skills.
-Little or no benefit from hearing aids.
-Educational setting that provides auditory skill development.
Cochlear implant candidacy for adults
-Referral for Cochlear Implant Evaluation: "60/60 Rule"
≥60dB PTA (500, 1000, 2000 Hz) ≤60% WRS
-Moderate hearing loss in the low frequencies and profound in the middle and high frequencies.
-Little or no benefit from hearing aids - < 60% correct in the best aided listening condition in the ear to be implanted for open-set sentence recognition (tested at ~50 dB HL).
-Desire to be a part of the hearing world.
Medical contraindications for cochlear implants
-No surgical problems placing the electrode in the cochlea and the receiver in the mastoid bone.
X-rays performed to confirm placement of electrode.
-Malformations of the cochlea may prevent implantation or make it more difficult.
-Not performed during active infection of the middle ear.
-Not performed if the auditory nerve is NOT functioning
Factors affecting performance(cochlear implants)
-Large variability in cochlear implant patient outcomes (e.g., success using the device)
-Age of implantation (especially children)
-Duration of hearing loss
-Hearing aid use prior to implantation
-Motivation (aural rehabilitation)
-Etiology of hearing loss (pure cochlear etiology best)
What type of tymps for Sensorineural HL
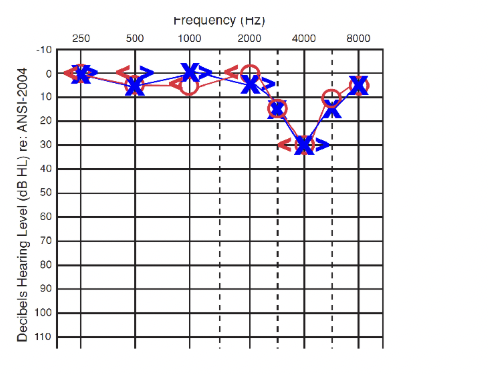
NORMAL TYMP (A)
What path does Cochlear Implants take in the auditory system
Bypasses outer, middle ear AND cochlea —> goes straight to neural
Try cochlear implant if…
Not benefiting from hearing aids
60/60 rule (moderately-severe — severe)
If Tymps come up as flat
REFER OUT — sensorineural = normal tymp
When to suggest BAHA
Possible pathologies: atresia, chronic infections
Non fixable CONDUCTIVE hearing loss
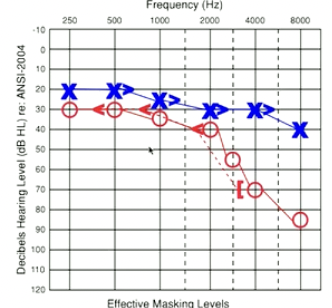
Growth of spongy bone around the ossicular chair and stapes footplate (stiffens chain)
More common in pregnant women
Bilateral
Conductive Hearing Loss
Carhart Notch (10-15 db worse at 2000 Hz)
Otosclerosis & Intervention
INTERVENTION: Refer out — Need surgery to remove spongy bone
Pressure equalization problems in the cochlea and semicircular canals
TINNITUS, VERTIGO
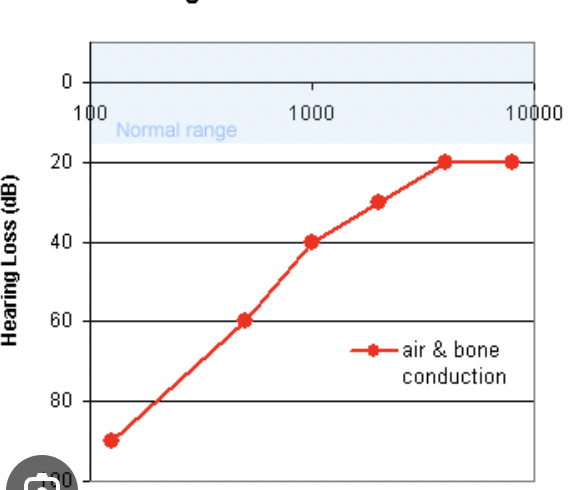
Fluctuating sensorineural hearing loss (low frequency loss — rising audiogram)
Unilateral
Poor word recognition scores
Menieres Disease and intervention
REFER OUT FOR SURGERY OR DRUG TREATMENTS
Work in loud environment with no earplugs (musicians, military, factories, etc)
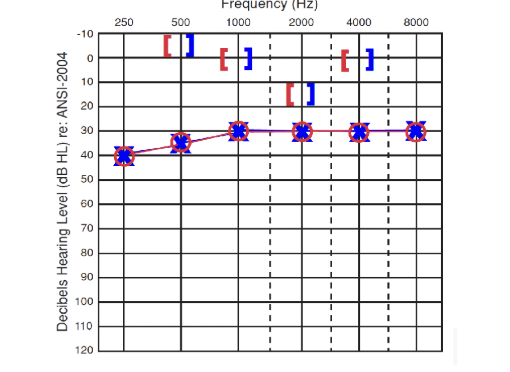
Notch at 3000, 4000, or 6000 Hz
Progressive high frequency hearing loss (sloping)
Noised Induced Hearing Loss and Intervention
INTERVENTION: hearing aids for poorer frequencies, suggest ear plugs or monitor if WR % is high
Auditory Neuropathy and Intervention
Normal OAES but absent/abnormal ABR
Normal hearing using pure tones but may show hearing loss
Mild-profound HL but VERY POOR WORD REC
“Hear but dont understand”
INTERVENTION: CI (mod-severe HL), ALD (mild)
Unilateral high frequency SNHL (one side sloping)
Adults 30 year old +
Poor WR% on bad ear
Benign tumors/ tinnitus
Vestibular Schwannoma
INTERVENTION: REFER OUT FOR SURGERY
Afferent fibers
The electrode array stimulates which fibers from the cochlea