Microbio: Host Defense Mechanisms
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
First Line of Defense
Type of non-specific immunity. It includes:
1. Skin and Mucous Membranes
2. Cellular and Chemical Factors
3. Microbial Antagonism
Second Line Defense
Type of non-specific immunity. It includes:
1. Fever
2. Interferons
3. Complement System
4. Cytokines
5. Inflammation
6. Phagocytosis
Skin Mucous Membranes
Part of the body's first line of defense. They are physical barriers that should be intact and unbroken.
Cellular and Chemical Factors
Part of the body's first line of defense.
- Dry skin inhibits colonization of pathogens
- Fatty acid in sebum
- Perspiration flushes organisms + enzyme LYSOZYME
- Mucus, rapidly dividing mucosal cells, lactoferrin, lactoperoxidase
Also includes cilia, saliva, digestive enzymes, acidity of stomach, alkalinity of intestines, peristalsis, frequent urination, and acidic vaginal pH
Microbial Antagonism
Part of the body's first line of defense. This occurs when an indigenous microbiota prevents the establishment of arriving pathogens. It includes the skin, oral cavity, upper respiratory tract, colon.
Superinfection
Overgrowth or "population explosion" of organisms.
Pyrogens
Substances that stimulate production of fever; may be endogenous (interleukin) or exogenous.
Fever
Part of the body's second line of defense. It is stimulated by pyrogens. It slows down the growth of some pathogens and actually kills some. Some effects of this method of defense are an increase in heart rate, metabolic rate, and caloric demand, as well as dehydration.
Interferons
Part of the body's second line of defense. They are small, antiviral proteins produced by virus-infected cells that interfere with viral replication.
Complement System
Part of the body's second line of defense. It is a group of approximately 30 proteins that are found in normal plasma. This method of defense initiates and amplifies inflammation and chemotaxis, activates leukocytes, lysis of bacteria and other cells, as well as initiates opsonization.
Opsonization
Increased phagocytosis by phagocytic cells.
Inflammation
Part of the body's second line of defense. Its purpose is to localize infection and promote healing. It is stimulated by physical, chemical, or biological agents.
Three Major Events of Inflammation
1. Vasodilation
2. Increased capillary permeability
3. Accumulation of leukocytes in site of injury
Cardinal Signs and Symptoms of Inflammation
Redness, heat, swelling, pain, and loss of function.
Sequence of Inflammation
1. Tissue Injury
2. Vasodilation
3. Increased Permeability
4. Emigration of Leukocytes
5. Chemotaxis
6. Phagocytosis
Tissue Injury
First step in inflammation.
Vasodilation
Second step in inflammation. This increases blood flow to injured areas which in turn increases the delivery of plasma proteins, neutrophils, and phagocytes.
Increased Permeability
Third step in inflammation. It occurs when protein-rich exudate containing immunoglobins and complement moves into injured areas.
Emigration of Leukocytes
Fourth step in inflammation. This occurs when neutrophils and macrophages adhere to endothelial cells of capillaries. Leukocytes squeeze through the gaps created by contraction of endothelial cells.
Chemotaxis (inflammation)
Fifth step in inflammation. Occurs when neutrophils and macrophages move to the site of injury in response to gradient of chemotactic mediators released by injured tissue.
Phagocytosis
Sixth step in inflammation. It occurs when the phagocyte attaches to bacterium or other foreign material and engulfs it by endocytosis.
Four Steps of Phagocytosis
1. Chemotaxis
2. Attachment
3. Ingestion
4. Digestion
Chemotaxis (phagocytosis)
First step in phagocytosis. Occurs when phagocytes are attracted by chemotactic agents to the site where they are needed.
Attachment
Seconds step in phagocytosis. It occurs when the phagocyte attaches to the foreign object.
Ingestion
Third step in phagocytosis. It occurs when pseudopodia surrounds the object and is taken into the cell.
Digestion
Final step of phagocytosis. This is when the foreign object is broken down and dissolved by digestive enzymes and other mechanisms.
Humoral Immunity
Type of immunity that always involves the production of antibodies. Thus, antibodies play a major part of this type of immunity.
Cell-Mediated Immunity
Type of immunity that includes macrophages, T-helper cells, cytotoxic cells, delayed hypersensitivity T cells, natural killer cells, killer cells, and granulocytes. Antibodies do not play a major role.
Natural Active Acquired Immunity
Immunity that is acquired in response to the entry of a live pathogen into the body.
Artifical Active Acquired Immunity
Immunity that is acquired in response to vaccines.
Natural Passive Acquired Immunity
Immunity that is acquired by a fetus when it receives maternal antibodies in utero or by an infant when it receives maternal antibodies contained in colostrum.
Artificial Passive Acquired Immunity
Immunity acquired when a person receives antibodies contained in antisera or gamma globulin.
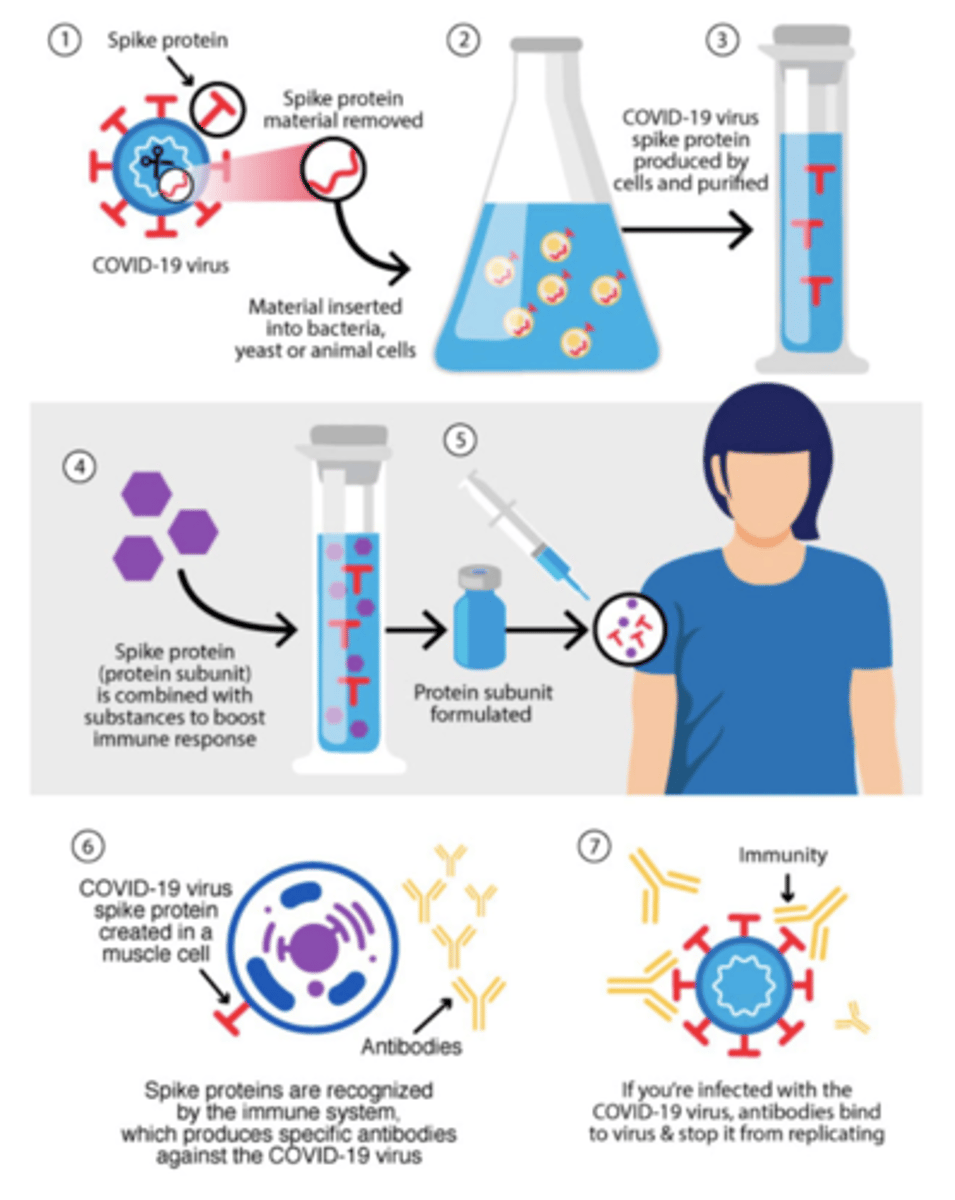
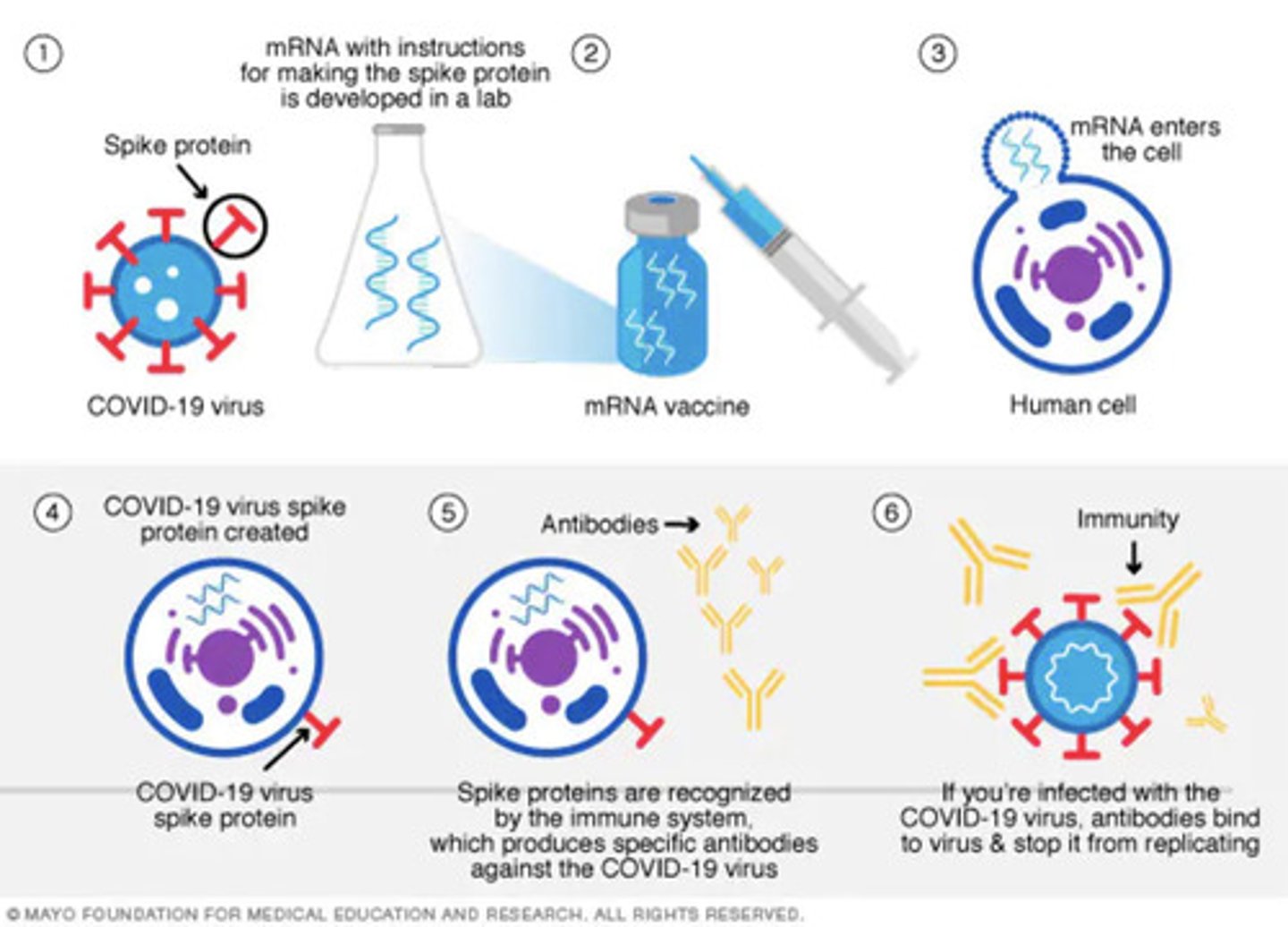
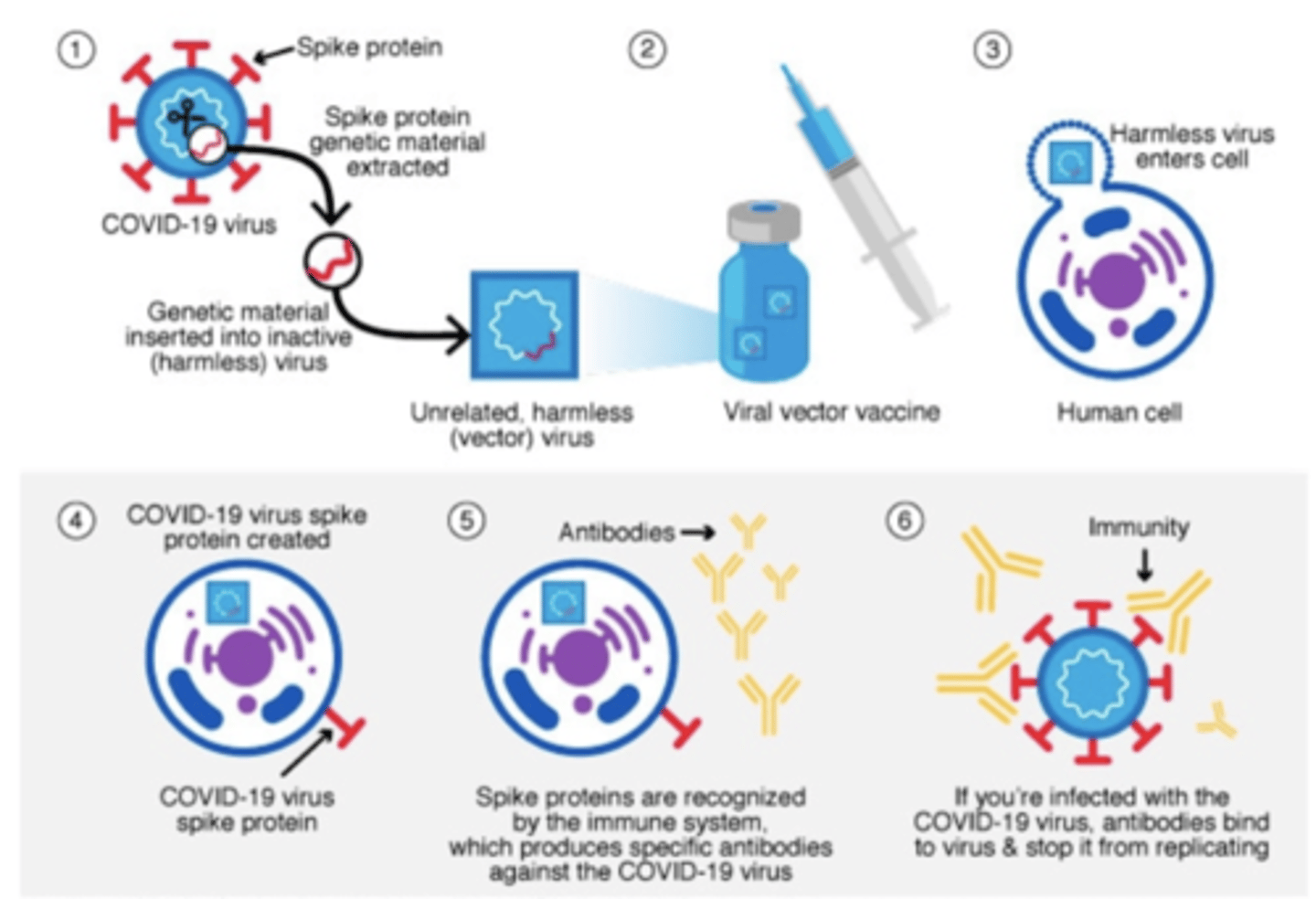
Vaccines
Stimulates the recipients' immune system to produce protective antibodies and/or memory cells. It is also stimulated to produce antibodies directed against the surface antigens, which prevents pathogens from adhering to the host cells.
Attenuated (Weakened) Vaccine
Type of vaccine that should not be given to immunosuppressed individuals. Examples include BCG, OPV, MMR, and Rotavirus.
Inactivated Vaccines
Type of vaccines that are produced faster and more easily. However, they are less effective because they produce a shorter period of immunity. Examples include DPT, Hepa B vaccine, and Rabies vaccine.
mRNA Vaccines
Pfizer and Moderna
Viral Vector Vaccines
Janssen/Johnson & Johnson and AstraZeneca
Protein Subunit Vaccines
Novavax