BIOL 318L: EXAM 2 - ENDOCRINE, MUSCLES, & RESPIRATORY SYSTEM
1/123
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
124 Terms
Exocrine glands
secretes substances onto epithelial surface
what are some examples of exocrine glands?
salivary or sweat glands
endocrine glands
produces hormones (chemical messengers) which are releaased into the blood and act on a target organ
can some glands be both endocrine and exocrine?
yes
what are some examples of both endocrine and exocrine glands?
pancreas
liver
kidneys
pituitary gland aka hypophysis
endocrine gland
“master endocrine”
8 hormones associated with this gland
adenohypophysis
Produces and secretes 6 hormones
Growth hormone (GH)
Prolactin (PRL)
Adrenocorticotropic hormone (ACTH
Thyroid-stimulating hormone (TSH)
Gonadotropins (LH & FSH)
neurohypophysis
Secretes 2 hormones that are produced in the hypothalamus
Antidiuretic hormone (ADH aka vasopressin)
Oxytocin
Goiter
enlargement of colloids
If a rat had a hypophysectomy, what could restore normal BMR?
administering TSH or TH (thyroid hormone) directly could restore normal basal metabolic rate (BMR), since the pituitary gland normally stimulates the thyroid to release TH.
If a rat had a thyroidectomy, what could restore normal BMR?
administering TH (e.g., thyroxine/T4 or triiodothyronine/T3) would restore normal BMR, as the thyroid is the main source of these hormones.
If a rat had a thyroid tumor producing too much TH, what could restore normal BMR?
administering PTU could restore normal BMR by reducing excess TH levels.
If a rat had a pituitary tumor producing too much TSH, what could restore normal BMR?
administering a drug to suppress TSH secretion (e.g., somatostatin analogs) or surgically removing the tumor could help restore normal BMR by reducing excessive stimulation of the thyroid.
parathyroid glands
4 total parathyroid glands
releases PTH
increases blood calcium
when is PTH secreted?
when the blood calcium is too low
what does PTH do?
PTH raises blood calcium levels
what does PTH stimulate?
PTH stimulates osteoclast production
what does PTH inhibit?
PTH inhibits osteoblasts
no bone deposition
what is a hormone that is produced by the zona glomerulosa?
aldosterone
what is a hormone that is produced by the zona fasciculata?
cortisol
what is a hormone that is produced by the zona reticularis?
androgens (testosterone)
is the pancreas endocrine or exocrine?
the pancreas has both endocrine and exocrine functions
what type of cells does the pancreas contain?
alpha cells
beta cells
delta cells
acinar cells
what do acinar cells do in the pancreas?
they produce digestive enzymes
why does type I diabetes occur?
because it destroys insulin-making (beta cells) cells in your pancreas
you can be born with type I diabetes
why does type II diabetes occur?
because your body is not able to effectively use insulin to bring glucose into your cells
also known as insulin resistance
when does type I diabetes occur?
it usually develops during childhood, but can develop at any age
when does type II diabetes occur?
it can develop at any age, but usually develops in adults over 45
what are some symptoms of type I diabetes?
increased thirst
frequent urination
extreme hunger
unintended weight loss
what are some symptoms of type II diabetes?
frequent urination
increased thirst
blurry vision
patches of dark skin
increased appetite
How does oxygen move from the lungs to the blood?
Oxygen diffuses down its partial pressure gradient across the respiratory membrane.
What happens after oxygen crosses the respiratory membrane?
After oxygen crosses the respiratory membrane, it moves across the endothelium of the blood vessel.
Once oxygen reaches the blood, where does it go?
Oxygen enters the blood and binds to hemoglobin in red blood cells (RBCs).
How does carbon dioxide enter the red blood cells?
Carbon dioxide enters the blood as bicarbonate (HCO3-) as Cl- leaves (chloride shift).
What happens to bicarbonate once inside the red blood cells?
Bicarbonate binds with hydrogen ions (H+) to form carbonic acid (H₂CO₃).
What happens to carbonic acid after it forms in the red blood cells?
Carbonic acid dissociates into carbon dioxide (CO₂) and water (H₂O).
How does carbon dioxide leave the red blood cells?
Carbon dioxide diffuses down its partial pressure gradient from the red blood cells into the alveoli.
What happens to the carbon dioxide once it reaches the alveoli?
Carbon dioxide is exhaled out of the body.
What occurs when tissue has higher CO2, increased acidity, and higher temperature?
In tissue with higher CO2, increased acidity, and higher temperature, the affinity for oxygen decreases.
What is the effect of a lower affinity for oxygen in tissues?
A lower affinity for oxygen causes oxygen to diffuse down the partial pressure gradient.
Where does oxygen go after diffusing in the tissue?
Oxygen enters the mitochondria after diffusing down the partial pressure gradient.
What happens to oxygen inside the mitochondria?
Inside the mitochondria, oxygen accepts electrons and forms H2O.
How does CO2 leave the mitochondria?
CO2 diffuses down the partial pressure gradient from the mitochondria into the blood.
What are the two forms CO2 takes when it enters the blood?
CO2 either binds to hemoglobin or remains dissolved in the blood.
What happens to CO2 once it enters red blood cells?
In red blood cells, CO2 combines with water to form H₂CO₃.
What does H₂CO₃ dissociate into?
H₂CO₃ dissociates into HCO₃- and H+.
What is the chloride shift?
The chloride shift is the exchange of HCO₃- for Cl- from the blood.
What happens when an acid enters the bloodstream?
An acid entering the bloodstream causes bicarbonate (HCO3̅) to react with hydronium ions (H3O+).
What is formed when bicarbonate reacts with hydronium ions (H3O+) in the bloodstream?
When bicarbonate reacts with hydronium ions, carbonic acid (H2CO3) and water (H2O) are formed.
What happens when a base enters the bloodstream?
When a base enters the bloodstream, carbonic acid (H2CO3) reacts with hydroxide ions (OH̅).
What is formed when carbonic acid reacts with hydroxide ions (OH̅) in the bloodstream?
When carbonic acid reacts with hydroxide ions, bicarbonate (HCO3̅) and water (H2O) are formed.
What happens when you hold your breath in terms of CO2 and pH?
When you hold your breath, CO2 is still produced by tissues, leading to higher acidity and a lower pH.
What happens during hyperventilation in terms of CO2 and pH?
During hyperventilation, CO2 is expelled faster than it is produced, leading to lower acidity and a higher pH.
Can respiratory alkalosis or acidosis occur due to medical issues?
Yes, respiratory alkalosis and acidosis can occur due to a variety of medical issues.
Can metabolic alkalosis or acidosis occur due to medical issues?
Yes, metabolic alkalosis and acidosis can also occur due to a variety of medical issues.
What is the larynx?
The larynx is a cartilaginous chamber that houses the vocal cords and the glottis, which is the opening into the trachea.
What is the thyroid cartilage?
The thyroid cartilage is the largest cartilage of the larynx and has a shield-like shape.
What is the cricoid cartilage?
The cricoid cartilage is a ringlike structure that is located inferior to the thyroid cartilage.
What is the epiglottis made of?
The epiglottis is made of spoon-shaped elastic cartilage.
What is the function of the epiglottis?
The epiglottis forces food away from the windpipe (trachea) during swallowing to prevent choking.
What is the trachea?
The trachea, also known as the windpipe, is a tube that leads to the primary bronchi and is supported by 16-20 C-shaped rings of hyaline cartilage.
What type of epithelial cells line the trachea?
The trachea is lined with ciliated pseudostratified columnar epithelial cells.
What type of cells are found in the tracheal epithelium that secrete mucus?
The tracheal epithelium contains mucus-secreting goblet cells, which are shaped like wine glasses.
What is the trachealis muscle?
The trachealis muscle is a thick band of smooth muscle that spans between the cartilage at the back of the trachea.
What is the function of the trachealis muscle?
The trachealis muscle adjusts airflow by contracting or relaxing to regulate the diameter of the trachea.
What type of epithelium lines the trachea?
The tracheal epithelium is composed of pseudostratified epithelium.
What type of glands are found in the submucosa of the trachea?
The tracheal glands are seromucous glands located in the submucosa.
What is the function of seromucous glands in the trachea?
Seromucous glands secrete a watery substance that helps to humidify air as it passes through the trachea.
What is pseudostratified epithelium?
Pseudostratified epithelium is a type of epithelial tissue that falsely appears stratified, but each cell is in contact with the basement membrane.
Why does pseudostratified epithelium appear stratified?
Pseudostratified epithelium appears stratified because of the arrangement of nuclei in two rows, but all cells still touch the basement membrane.
What is the function of goblet cells in pseudostratified epithelium?
Goblet cells secrete mucus that helps trap dirt and dust from the air.
What is the function of cilia in pseudostratified epithelium?
Cilia protrude from the apical surface and move mucus up towards the trachea to clear trapped particles.
Why is epithelial tissue considered avascular?
Epithelial tissue is avascular because it lacks blood vessels and relies on nutrients from the loose connective tissue underneath its basement membrane.
What type of connective tissue supports epithelial tissue?
Epithelial tissue is supported by loose connective tissue beneath its basement membrane.
What is a distinguishing feature of the bronchi compared to the trachea?
The bronchi have cartilage in plates rather than a single C-shaped arch like the trachea.
What are bronchioles?
Bronchioles are the small airways in the lungs that branch from the bronchi and lead to the alveoli, where gas exchange occurs.
What is the correct order of airflow from the primary bronchi to the alveoli?
Air flows in the following order: primary bronchi → bronchioles → terminal bronchioles → respiratory bronchioles (where alveoli begin budding from the walls) → alveolar ducts (atrium) → alveolar sacs → alveoli of the lungs.
What happens at the respiratory bronchioles?
At the respiratory bronchioles, alveoli begin to bud from the walls, marking the transition from the conducting zone to the respiratory zone, where gas exchange occurs.
What structure comes after the respiratory bronchioles in the airflow pathway?
After the respiratory bronchioles, air moves into the alveolar ducts, which further lead to alveolar sacs and ultimately the alveoli of the lungs.
What are alveolar sacs, and how do they function in respiration?
Alveolar sacs are clusters of alveoli where gas exchange occurs, allowing oxygen to enter the blood and carbon dioxide to be expelled from the body.
What do the bronchioles lack?
The bronchioles lack cartilage and glands, unlike the bronchi.
What is the respiratory membrane?
The respiratory membrane is a thin barrier between the alveolar air and blood where gas exchange occurs between the lungs and blood.
What type of alveolar cell is classified as Type I?
Type I alveolar cells are squamous alveolar cells that are flat and pancake-like, providing a large surface area and a thin barrier for gas exchange.
What is the function of Type I alveolar cells?
Type I alveolar cells facilitate gas exchange by creating a thin surface for oxygen and carbon dioxide to diffuse between the alveoli and blood.
What type of alveolar cell is classified as Type II?
Type II alveolar cells are called great alveolar cells and are responsible for producing surfactant.
What is the function of Type II alveolar cells?
Type II alveolar cells produce surfactant, which reduces surface tension in the alveoli and helps prevent their collapse.
Which alveolar cell is the most abundant?
Alveolar macrophages are the most abundant cells in the alveoli.
What is the function of alveolar macrophages?
Alveolar macrophages help remove debris, dust, and pathogens from the alveoli to keep the lungs clean and free of infections.
What is a terminal bronchiole?
A terminal bronchiole is the last part of the conducting airway, characterized by thicker walls and a cuboidal epithelium, marking the end of the pseudostratified epithelium.
What type of epithelium is found in the terminal bronchioles?
The terminal bronchioles initially have a ciliated columnar epithelium, which transitions to a low cuboidal epithelium.
What are respiratory bronchioles?
Respiratory bronchioles are small airways with thin walls lined by simple squamous epithelium, serving as a transition between the conducting zone and gas exchange areas.
What type of epithelium lines the respiratory bronchioles?
The respiratory bronchioles are lined by simple squamous epithelium, which allows for gas exchange.
What are alveoli?
Alveoli are small air sacs composed of simple squamous epithelium that serve as the primary sites of gas exchange in the lungs.
What type of epithelium makes up the alveoli?
The alveoli are made up of simple squamous epithelium, which is flat and scale-like, allowing for efficient gas diffusion.
What is the function of an arteriole?
An arteriole is responsible for carrying deoxygenated blood from the heart to the lungs.
What is the structure of an arteriole?
Arterioles have very thin walls, typically consisting of one or two cell layers of smooth muscle.
What is the difference between venules and arterioles in terms of their muscle layer?
Venules tend to have a less developed muscle layer than arterioles, which results in thinner walls.
What is the function of venules in the circulatory system?
Venules return oxygenated blood to the heart.
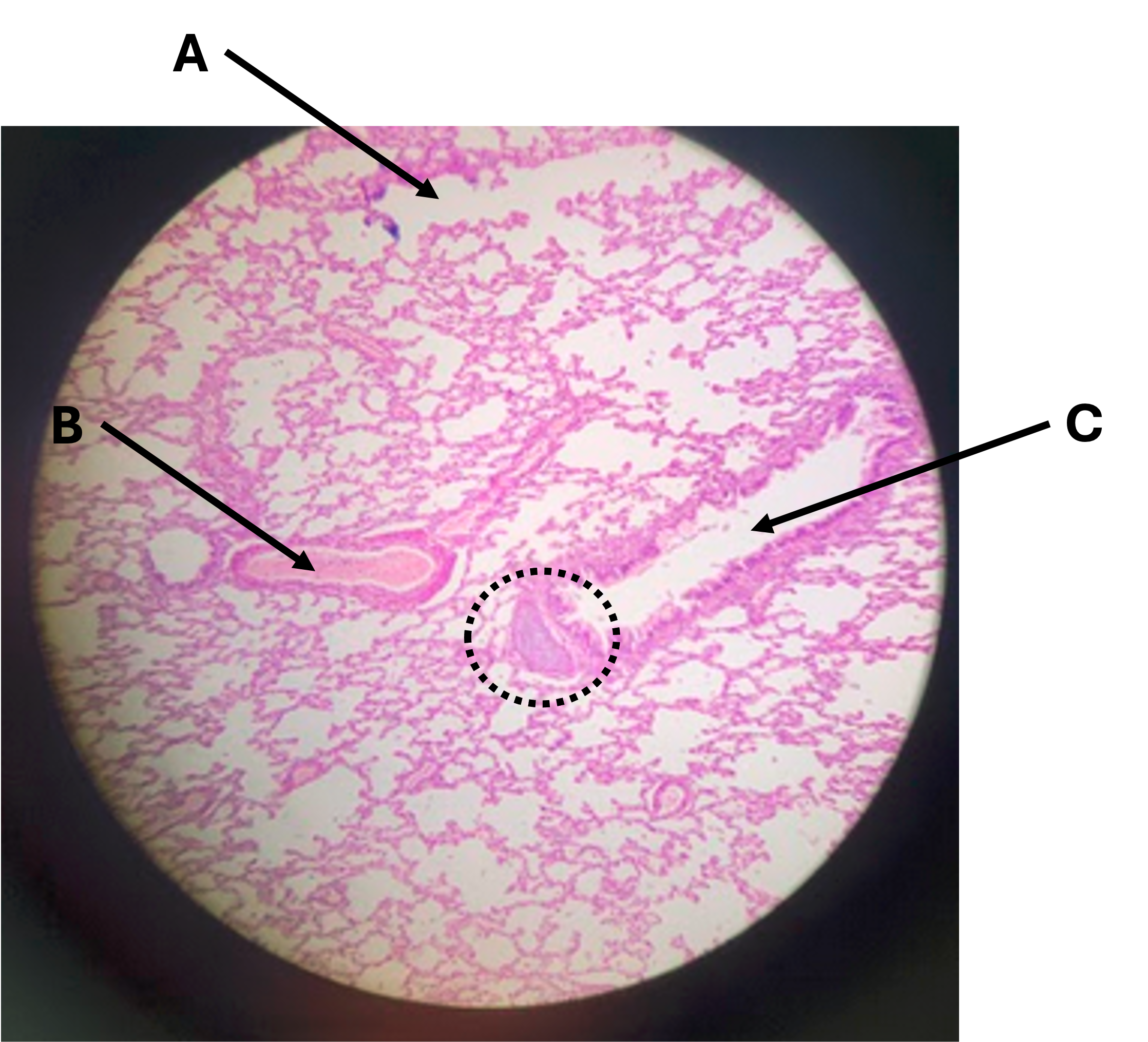
What is the name of structure A (the white space)?
Alveoli
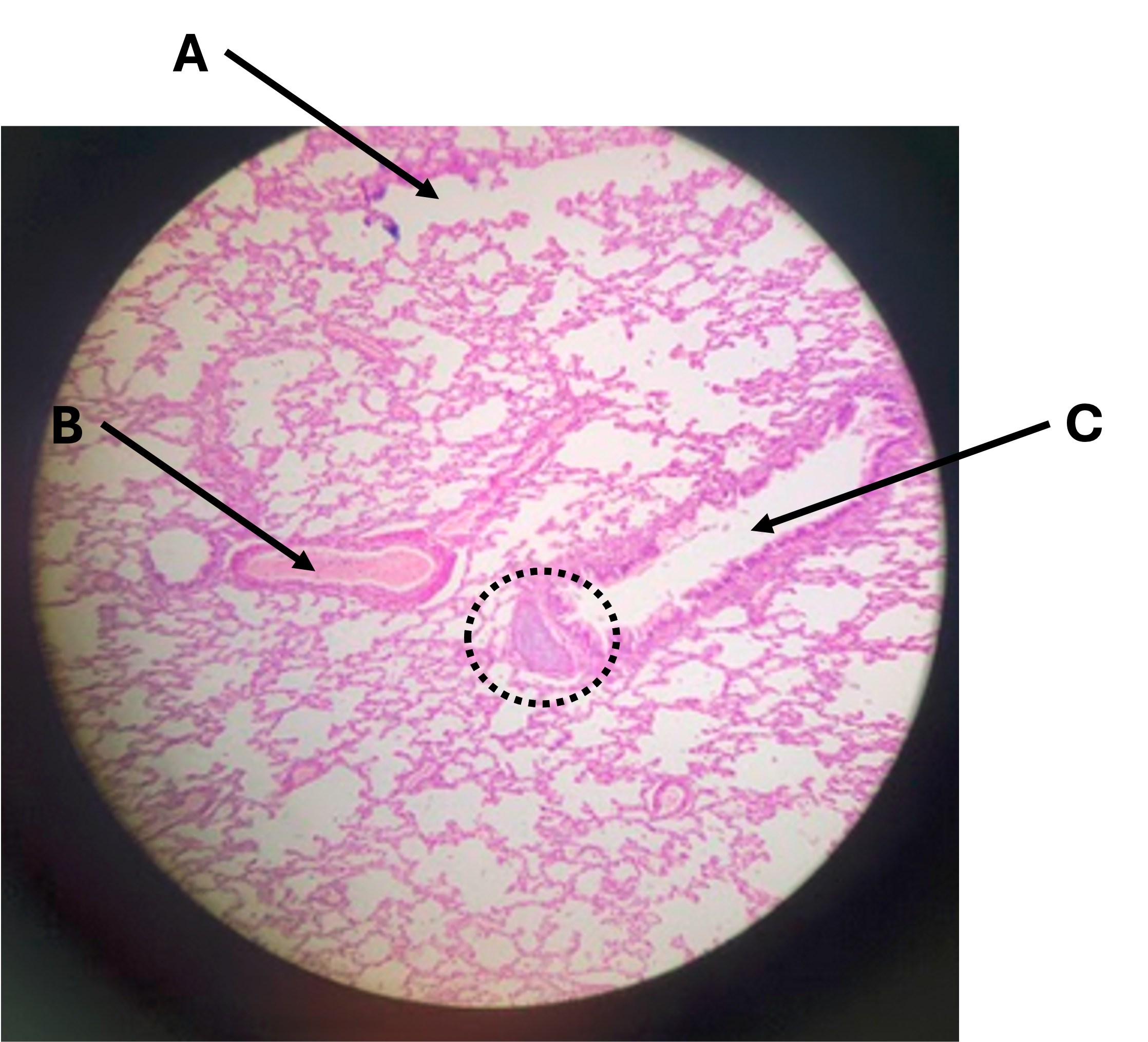
What is the name of structure B?
Arteriole, look at the thickness of the tissue surrounding.
Arterioles are thicker than venules as they must withstand more pressure.