Adult Psychopathology- Prelim 2
1/171
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
172 Terms
dissociation definition
detachment from body, self, and surroundings
everyday dissociation examples
“zoning out” while driving, getting lost in a book/movie/activity, looking at a beautiful landscape or familiar landmark, deep daydreaming
what makes a diagnosis of dissociative disorder different from everyday dissociation?
change or disturbances in identity, memory, or consciousness
3 types of dissociative disorders
depersonalization/derealization disorder (DDD)
dissociative amnesia (DA)
dissociative identity disorder (DID)
DDD criteria A
A. the presence of persistent or recurrent experiences of depersonalization, derealization, or both
depersonalization: experiences of unreality, detachment, or being an outside observer with respect to ones’ thoughts, feelings, sensations, body, or actions (e.g. perceptual alterations, distorted sense of time, unreal or absent self, emotional, and/or physical numbing)
derealization: experiences of unreality or detachment with respect to surroundings (e.g. individuals or objects are experienced as unreal, dreamlike, foggy, lifeless, or visually distorted)
DDD criteria continued
B. during the depersonalization or derealization experiences, reality testing remains intact
C. the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
D. the disturbance is not attributable to the physiological effects of a substance (e.g. a drug of abuse, medication) or other medical conditions (e.g. seizures)
E. the disturbance is not better explained by another mental disorder, such as schizophrenia, panic disorder, MDD, acute stress disorder, PTSD, or another dissociative disorder
reality testing definition + with DDD
ability to differentiate between one's own internal thoughts, feelings, and perceptions and the external, objective world
with DDD: may feel detached from themselves or their surroundings, but they still recognize these feelings are unusual and not "real" in the sense of being actual events. This awareness is a key factor that differentiates dissociative experiences from psychotic disorders
DDD full simplified criteria
persistent or recurrent experiences of depersonalization, derealization, or both
during the depersonalization or derealization experiences, reality testing remains intact
the symptoms cause clinically significant distress or impairment in functioning
disturbance is not attributable to the physiological effects of a substance or other medical conditions
the disturbance is not better explained by another mental disorder or another dissociative disorder
DDD additional facts (prevalence, gender ratio, average age of onset, cognitive profile, preceded by)
prevalence: 0.8-2.8%
gender: equally prevalent across men/women
avg age of onset: around 16 yrs old
cognitive profile: tend to have relative weaknesses in processing speed, attention, and spatial reasoning
often preceded by: periods of intense stress, depression, anxiety, or drug use
DA criteria A
A. an inability to recall important autobiographical information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting
note: dissociative amnesia most often consists of localized/selective amnesia for a specific event(s); or generalized amnesia for identity and life history
autobiographical memory
the personal recollection of life events, encompassing both specific episodic memories and broader self-related information
2 types of amnesia
localized: events during a specific span of time, usually the first few hours after a disturbing event
generalized: no memory of life, including identity or previously acquired knowledge (e.g. recent political events), people usually but not always retain well-learned skills (e.g. putting in contact lenses)
people are usually unaware or only partially aware of their memory problems
DA criteria continued
B. the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
C. the disturbance is not attributable to the physiological effects of a substance (e.g. alcohol or other drug abuse, a medication) or a neurological or other medical conditions (e.g. partial complex seizures, transient global amnesia, sequelae of a closed head injury/traumatic brain injury, other neurological condition)
D. the disturbance is not better explained by DID, PTSD, acute stress disorder, somatic symptom disorder, or major or mild neurocognitive disorder
DA specifier
with or without dissociative fugue: apparently purposeful travel or bewildered wandering that is associated with amnesia for identity or for other important autobiographical information
DA full simplified criteria
an inability to recall important autobiographical information, usually of a traumatic or stressful nature, that is inconsistent with ordinary forgetting
the symptoms cause clinically significant distress or impairment in functioning
the disturbance is not attributable to the physiological effects of a substance or a neurological or other medical condition
the disturbance is not better explained by DID, PTSD, acute stress disorder, somatic symptom disorder, or major or mild neurocognitive disorder
how is DA different from amnesia in cognitive disorders?
DA onset is attributed to psychological trauma/extreme stress
DA can be exacerbated by stress
DA memory deficits are primarily with autobiographical memory
DA patients’ ability to learn new information is intact (not the case for neurodegenerative cognitive disorders)
additional DA facts (onset, gender ratio, duration, main risk factor, etc)
onset: typically sudden
gender: more prevalent in women
duration of memory loss: can range from minutes to decades
main risk factor: severe, acute, or chronic traumatization
when memory returns, suicidality is common since individuals may experience a flood of unwanted memories
Bhutan in the 1990s: correlational study of DA and trauma
country in South Asia
reclassified Lhotshampas (Bhutanese citizens of Nepalese descent, one of three main ethnic groups in Bhutan) as “illegal immigrants”
many were persecuted and tortured by the govt, resulting in the flight or expulsion of nearly 100k ppl
compared to under 5% of refugees who had not been tortured, around 20% of those who had experienced torture experienced DA (4x more likely)
treatments for DA
presently no evidence based treatments specific for the treatment of dissociative amnesia
ppl sometimes recover spontaneously on their own
ppl may also use therapy techniques designed for trauma and coping with stress
DID criteria A
disruption of identity characterized by 2+ distinct personality states, which may be described in some cultures as an experience of possession
the disruption in identity involves marked discontinuity in sense of self and sense of agency, accompanied by related alterations in affect, behavior, consciousness, memory, perception, cognition, and/or sensory-motor functioning
these signs and symptoms may be observed by others or reported by the individual
DID criteria continued
recurrent gaps in recall of everyday events, important personal information, and/or traumatic events that are inconsistent with ordinary forgetting
the symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning
the disturbance is not a normal part of broadly accepted cultural or religious practice (in children: the symptoms are not better explained by imaginary playmates or other fantasy play)
the symptoms are not attributable to the physiological effects of a substance (e.g. blackouts or chaotic behavior during alcohol intoxication) or another medical condition (e.g. complex partial seizures)
DID full simplified criteria
disruption of identity characterized by 2+ distinct personality states
marked discontinuity in sense of self and sense of agency
accompanied by related alterations in affect, behavior, consciousness, memory, perception, cognition, and/or sensory-motor functioning
recurrent gaps in recall of everyday events, important personal information, and/or traumatic events that are inconsistent with ordinary forgetting
the symptoms cause clinically significant distress or impairment in functioning
the disturbance is not a normal part of broadly accepted cultural or religious practice
the symptoms are not attributable to the physiological effects of a substance or another medical condition
DID terms
switch: transition from one personality state to the next (may be sudden but also frequently subtle to an observer, e.g. within a conversation)
host: personality of the person before the disorder began
alters: later-developing personalities
most ppl with DID have around 13-15 alters
if given personality tests, alters generally score differently from each other and from hosts
interidentity amnesia: when different identities have no knowledge of each other
Kong, Allen, & Glisky (2008) procedure
participants with DID chose 2 identities to participate in research study
study phase
given 3 lists of 24 neutral words (list A, list B, and distractor words)
identity A listened to list A and identified length of syllable of each word in the list
participants were asked to switch to identity B
identity B reported no knowledge of identity A’s experiences
identity B listened to list B and identified the length of the words’ syllables
test phase
identity B was given a list of words made up of list A, B, and distractor words; asked to identify which words appeared on list B
participants were equally likely to report that words from list A and B had appeared and less likely to report that distractor words appeared
Kong, Allen, & Glisky (2008) conclusion
although ppl with DID often report interidentity amnesia, identities share some memories (ultimately, they are encoding with the same brain)
DID is controversial
highly sensationalized in media representations
at least one high-profile case admitted to faking personalities
previously been used in legal cases to suggest lack of guilt or responsibility
very rare disorder, not much research on it
is DID a disorder of trauma?
yes, virtually all cases of ppl with DID involve severe trauma, often extremely early in life/childhood (suggested to be a form of PTSD from childhood trauma)
consensus is that dissociation is a coping mechanism to manage trauma
DID is an unusual response; PTSD and depression are more common sequelae of trauma
we don’t know why some ppl develop DID as a response
DID is often treated similarly to PTSD
false memories and dissociative disorders
1990s rise in dissociative amnesia
contributed to confusion around dissociative disorders
we know some ppl do not remember emotionally charged, often traumatic events that have happened to them
we also know that memory is suggestible and frequently distorted
Freyd’s Betrayal Trauma
betrayal trauma: traumas that occur in situations where someone is dependent on the perpetrator for their survival (e.g. child sexual abuse)
different type of trauma than if the perpetrator was someone random
what did Freyd hypothesize about betrayal trauma and attention?
divided attention (e.g. paying attention to more than one thing at the same time) is important to dissociation
betrayal trauma leads to difficulties in dividing attention
DePrince & Freyd (2004) procedure
participants were asked to memorize a list of words (intentionally valenced) while simultaneously doing another task
some words related to trauma (e.g. incest, assault) and others were not (e.g. curtain, light)
suggests ppl high in dissociation can keep threatening information from their awareness, especially if they allocate attention to other tasks in their environment
DePrince & Freyd (2004) conclusion
demonstrated that under divided-attention demands, high dissociators have impaired memory for words associated with trauma
Somatic disorders
characterized by prominent bodily (somatic) symptoms and/or anxiety around illness (ex. pseudocyesis)
4 somatic disorders
Somatic Symptom Disorder (SSD)
Illness Anxiety Disorder (IAD)
Functional Neurological Symptom Disorder (FND)
Factitious Disorder (FD)
SSD Diagnostic Criteria
one or more somatic symptoms that are distressing or result in significant disruption of daily life
somatic symptoms may or may not have a clear cause
can include pain, swelling, coughing, fatigue, palpitations, dizziness, GI symptoms
excessive thoughts, feelings, or behaviors related to the somatic symptoms or associated health concerns as manifested by at least one of the following:
disproportionate and persistent thoughts about the seriousness of one’s symptoms
persistently high level of anxiety about health or symptoms
excessive time and energy devoted to these symptoms or health concerns
although any one somatic symptom may not be continuously present, the state of being symptomatic is persistent (typically more than 6 months)
specify if pain is predominant and if symptoms are mild, moderate, or severe
Example of somatic symptom disorder from textbook: Jada
Jada’s entire life revolved around her symptoms… her symptoms were her identity. Without them, she would not know who she was… would not know how to relate to people except in the context of discussing her symptoms
Barlow text, page 182
Prevalence and correlates of SSD
relatively common, in 5-7% of population
more common in women
more common in people who have a tendency to experience bodily sensations intensely and to pay attention to bodily cues
IAD Diagnostic Criteria
preoccupation with having or acquiring serious physical illness
somatic symptoms are not present, or if present are only mild in intensity
if another medical condition is present or there is a high risk for developing a medical condition (e.g. strong family history is present), the preoccupation is clearly excessive or disproportionate
high level of anxiety about health, easily alarmed about personal health status
performs excessive health-related behaviors (repeatedly checks his or her body for signs of illness) or exhibits maladaptive avoidance (avoids doctor appointments and hospitals)
illness preoccupation has been present for 6+ months but the specific illness that is feared may change over that period of time
the illness-related preoccupation is not better explained by another mental disorder (such as somatic symptom disorder, panic disorder, generalized anxiety disorder, body dysmorphic disorder, OBD), or delusional disorder, somatic type
How to differentiate across SSD and IAD
There are physical symptoms in SSD, not IAD → SSD is about finding relief from symptoms, while IAD is characterized by a recurrent worry and reassurance seeking
What is a common thing that happens when of having IAD when seeing doctors?
frequently consult multiple doctors in case the previous doctor missed something
Disease Conviction
strong persistent belief in having a serious physical illness, despite a lack of medical evidence and information/reassurance from healthcare professionals
often present in IAD
Predictors of SSD and IAD
related to cognition and perception of physical signs
enhanced sensitivity to cues of illness
high levels of current stress
belief that severe illnesses are common
disproportionate early life experiences of disease in family members
COVID-19 pandemic increased somaticizing and illness anxiety globally
Prevalence of IAD
1-7% of the population experiences it annually
Treatment for IAD and SSD
CBT is first line treatment
can yield strong effects with relatively brief course (ex. 6 sessions)
modifying thoughts around symptoms or illness
can you go about daily life with somatic symptoms? how?
evaluating likelihood a physical change, ex. headache, is indicative of serious illness
adding behaviors to boost quality of life and relationships
help people interpret physical symptoms without assuming they are dangerous
What does functional mean in neurology?
a symptom without an identifiable, organic cause
Functional Neurological Symptom Disorder (FND) aka Conversion Disorder
A. One or more of the symptoms of altered voluntary motor or sensory function
B. Clinical findings provide evidence of incompatibility between the symptom and recognized neurological or medical conditions
C. The symptom or deficit is not better explained by another medical or mental disorder
D. The symptom or deficit causes clinically significant distress or impairment in social, occupational, or other important areas of functioning or warrants medical evaluation
What is it like to have FND aka Conversion Disorder?
a person experiences neurological symptoms (e.g., paralysis, seizures, blindness, movement or sensory disturbances) that cannot be explained by neurological disease or injury, but are genuine and distressing.
The symptoms mimic neurological disorders, yet medical testing (MRI, EEG, etc.) shows no structural brain damage or disease to account for them
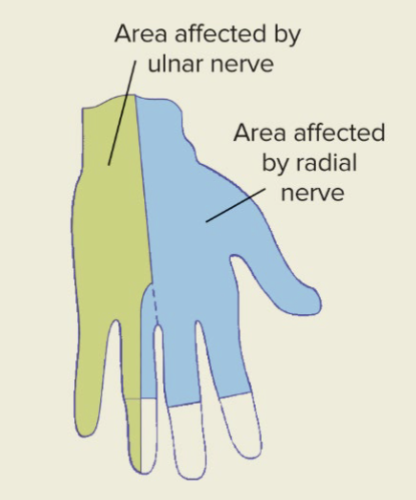
Glove anesthesia, symptom of FND (sensory)
when people lose all feeling and become numb in one hand
physical damage to the ulnar nerve causes numbness in the ring and pinky fingers and up the arm
physical damage to the radial nerve causes numbness in the ring, middle, index fingers and thumb
Specify if FND is with:
with weakness or paralysis
with abnormal movement (ex. tremor, dystonia, myoclonus, gait disorder)
with swallowing symptoms
with speech symptoms (ex. dysphonia, slurred speech)
with attacks or seizures
with anesthesia or sensory loss
with special sensory symptom (ex. visual, olfactory, or hearing disturbance)
with mixed symptoms (multiple of the above)
In FND, are symptoms experienced or produced?
Symptoms are genuinely experienced and not intentionally produced
Strange things can happen to people with FND
people with paralysis may run in an emergency and are often shocked they were able to do this; people with functional blindness cannot do many things that real blind people can do, like touch their fingers together
Freud’s thoughts on FND/Conversion Disorder (2 types of gains)
primary gain: anxiety around an unconscious conflict is reduced by “converting” psychological symptoms to physical ones
secondary gain: symptoms may be prolonged or exacerbated if they result in some kind of benefit, sympathy, attention
although our perspectives on FND have changed, these terms are still sometimes used
Prevalence of FND + what is the most common functional symptom?
episodes of unresponsiveness/seizures are the most common functional symptom globally
more common in women
overall prevalence is unclear and likely very rare, but accounts for about 16-20% of new neurology patients
Risk factors of FND
Primarily environmental
achievement-related pressure
trauma and stress
high rates of functional blindness among Cambodian refugees who witnessed war trauma
infections and inflammation
Prognosis (the likely course of a disease or ailment) for FNSD
long term prognosis for this is similar to that for Multiple Sclerosis and Parkinson’s
significant decrements in quality of life due to symptoms
course of this disorder can be waxing and waning
FND prevalence over time
prevalence has shifted over history
common in turn-of-the-century Europe, particularly in women (Freud’s population, often termed hysteria)
less prevalent now than 100 years ago
increased during WW1 and 2, resulting in many soldiers being unable to return to the front
FND is to some degree contagious
considered a mass psychogenic illness
outbreaks of FND within a group of people who share daily activities (ex. school, workplace)
spread of symptoms is often very rapid
first reported in Europe’s Middle Ages with tarantism and “dancing manias”
documented globally: Singapore, Tanzania, Uganda, Mali, England, France, Germany, Italy, Russia, Sweden, India, Nepal, Kenya
Le Roy, NY (2011-2012) case from reading
high school girls experiencing tics/spasms which spread around the school, everyone was freaking out about this
there was talk of environmental toxins
no cause discovered, nobody got better, more people got sick
example of mass psychogenic illness
Spread of mass psychogenic illness is exacerbated by:
rumors and misinformation about causes
community pressure to solve the problem
lack of attention to psychological explanations
anxiety related to presumed causes (vaccines, chemical exposure)
negative perception of government and health authorities
psychological stressors
media and social media coverage
physical proximity or close-knit group
Factitious Disorder Diagnostic Criteria
falsification of physical or psychological signs or symptoms, or induction of injury or disease, associated with identified deception
people create signs of injury to deceive others
falsification of symptoms can be extreme
ex. creating lesions/swelling, ingesting substances to create abnormalities in blood, contamination of medical samples with blood or stool
the individual presents themselves to others as ill, impaired, or injured
the deceptive behavior is evident even in the absence of obvious external rewards
the behavior is not better explained by another mental disorder, such as delusional disorder or another psychotic disorder
Factitious Disorder can occur for oneself or be imposed on another person (by proxy, such as a child, spouse, pet)
this is usually the case of making someone who is reliant on them sick
Münchhausen’s Syndrome
older nickname given to Factitious Disorder, the name is derived from an 18th century novel about Baron von Münchhausen that’s filled with elaborate, obviously false adventures
“extravagantly untruthful pseudo-autobiographical stories”
Malingering
intentionally presenting false symptoms for personal gain
usually but not always financially motivated (ex. malingering to avoid military service)
not considered a psychological disorder
not the same as Factitious Disorder
How is Malingering different from Factitious Disorder?
In malingering, the symptoms are linked to personal gain (not in FD)
Additional information for Factitious Disorder
early life maltreatment (particularly physical and emotional)
around 60% of cases report experiencing a severe childhood illness
higher prevalence among healthcare professionals
patients describe uncontrollable urge to maintain behaviors
Treatment for Factitious Disorder
FD by proxy is often a legal issue, and one identified/prosecuted as maltreatment rather than treated
no standard treatments for FD
people frequently do not consent to treatment
prognosis is considered poor
some improvement documented with CBT and supportive treatments
some improvement documented when comorbid conditions (like depression) are treated
What is anxiety?
Emotional state marked by the anticipation of danger of misfortune, intense distress, bodily tension, and nervousness
Accompanied by physical sensations
Why are people anxious?
It is a functional response- lack of anxiety is problematic, since it emerges in response to perceived threat
Throughout human history, anxiety played a pivotal role in the survival of our species
Creates physical change (aka fight or flight response) that mobilizes us to guard against or escape from danger successfully
What is the effect of anxiety being part of our evolutionary heritage?
We will all always experience it
What do anxiety disorders entail?
Levels of anxiety that are frequent, debilitating, and disproportionate to the circumstances
General prevalence of anxiety disorders
Among the most prevalent psychological disorders, ~1/3 of people will experience an anxiety disorder at some point
When does an anxiety disorder commonly start?
In childhood
What is one explanation for the high prevalence of anxiety disorders?
Humans who are alive today are the ones whose ancestors developed the keenest reactions to threats
How does evolution explain the early onset of anxiety?
Even a very young child needs to be prepared for fight or flight
What are physical signs of anxiety derived from?
Derived from fight-or-flight response, it prioritizes directing energy to the most essential functions for survival
Does anxiety bring on the same or different symptoms depending on the circumstances?
The same symptoms manifest in you, regardless of the circumstances that bring them on, reflecting how fight-or-flight is effective against many types of threat
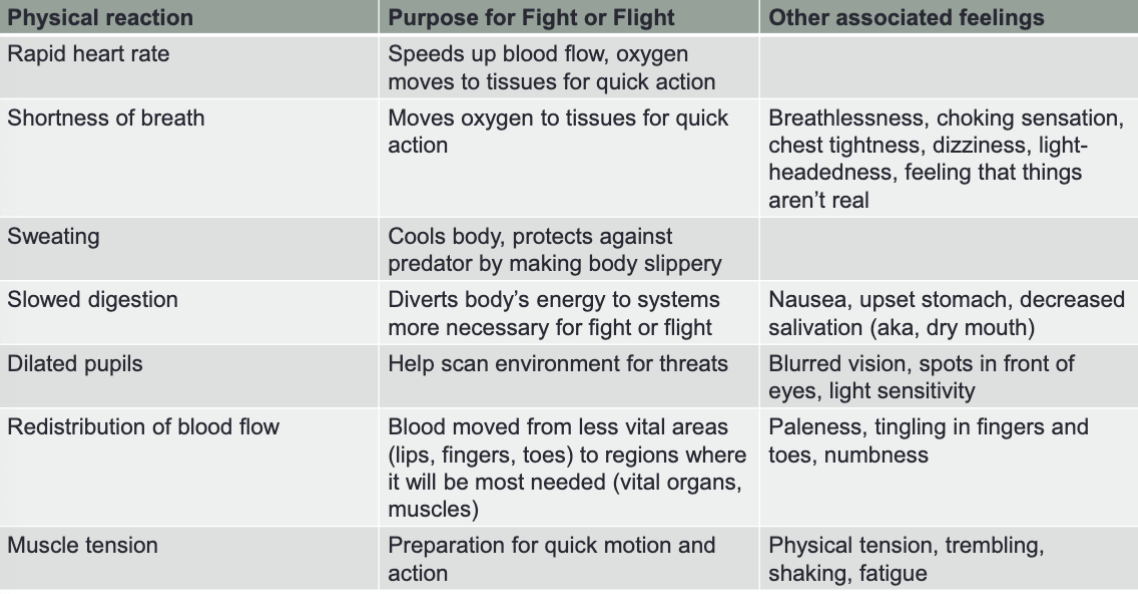
Examples of physical reactions / purpose for fight or flight / other associated feelings
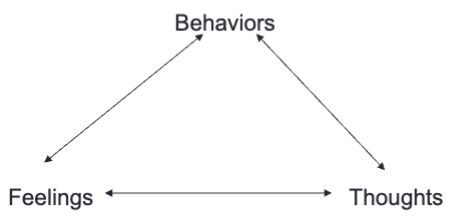
2 main cognitive symptoms of anxiety
Fear/Perception of threat or danger- when we are anxious, we perceive ourselves as in danger even though we are physically safe
Worry- repetitive negative thoughts about the possibility of future danger, misfortune, or hardship
Are worry and perception of threat short-term or long-term?
Both worry and the perception of threat are often illusory
How are fear and worry different?
Fear and worry are related, but fear tends to be present-oriented (right now) whereas worry tends to be future oriented (anticipation)
“I’ve had a lot of worries in my life — most of which have never happened.” -Mark Twain
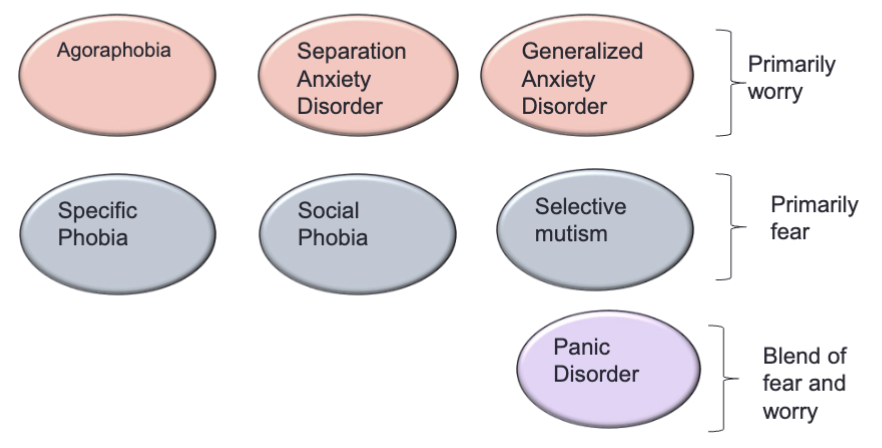
7 anxiety disorders in the DSM-5
Comorbidity and anxiety disorders
Anxiety disorders are highly comorbid with each other.
People may often have predisposition towards anxiety, but will have different anxiety disorders at different points in their lives
Specific Phobia criteria
Marked fear or anxiety about a specific object or situation (e.g. flying, heights, animals, needles, blood, etc.)
Phobic object or situation almost always provokes immediate fear or anxiety. It is actively avoided or endured with intense fear or anxiety.
The fear or anxiety is out of proportion to the actual danger posed by the specific object or situation and to the sociocultural context.
The fear, anxiety, or avoidance is persistent, typically lasting 6+ months.
The fear, anxiety, or avoidance causes clinically significant distress or impairment in social, occupational or other important areas of functioning
Failure to meet the functioning criteria is why most of our normal fears are not considered phobias
Specific Phobia: main phobia categories
Blood, injection, injury
Situations (e.g. enclosed spaces, airplanes, elevators, bridges)
Natural environment (e.g. storms, heights)
Animals
In terms of evolutionary psychology, what is a theory about the main phobia categories?
These stimuli are things that posed a consistent threat to human survival throughout history, such as poisonous animals, dangerous environmental situations, and events that could cause injury or infection, like bleeding
Specific Phobia: if a phobic stimulus is encountered, what will happen?
The person will experience immediate fear/horror
What is the main behavioral symptom of anxiety?
Avoidance, because people do not want to feel that level of fear/distress
How is avoidance a paradox?
It reduces anxiety short-term, but will increase anxiety long-term, because it solidifies beliefs around phobic stimulus.
It also limits the opportunity to learn that seemingly threatening circumstances are not dangerous, so there is no formation of new beliefs or experiences.
Avoidant behavior provides negative reinforcement
Each time you engage in avoidant behavior, you eliminate aversive feelings of anxiety, making it more likely that you will engage in that behavior again/repeat it in the future
Treating phobias
The core of treatment is to eliminate reinforcement associated with avoidance.
If we consciously modify an avoidant behavior, we can change the beliefs that maintain anxiety and anxious feelings themselves
How can we eliminate the reinforcement associated with avoidance?
Through exposure therapy
Exposures (aka CBT for Specific Phobia)
The most effective treatments for phobias all involve exposure to a fear-provoking stimulus, but limiting the anxiety-reducing response (avoidance)
With prolonged exposure, people habituate (body acclimates to the feeling of anxiety), affirming that they can deal with a situation like this
Exposures help people form new beliefs about the feared situation and their ability to cope with it
What happens when confronting the phobic stimulus without avoidance?
Anxiety will be experienced → through this, exposure therapy is essentially making people more anxious right now, so that they will become less anxious in general
Fear and Avoidance Hierarchy
Part of exposure therapy
Developed collaboratively with therapist
Ordered list of situations in which a client experiences fear of phobic stimulus
Used as a guide for exposures in therapy, clients will work from least feared to most feared stimulus
Each situation gets rated in terms of how much fear it generates and the lengths to which a client will go to avoid that situation
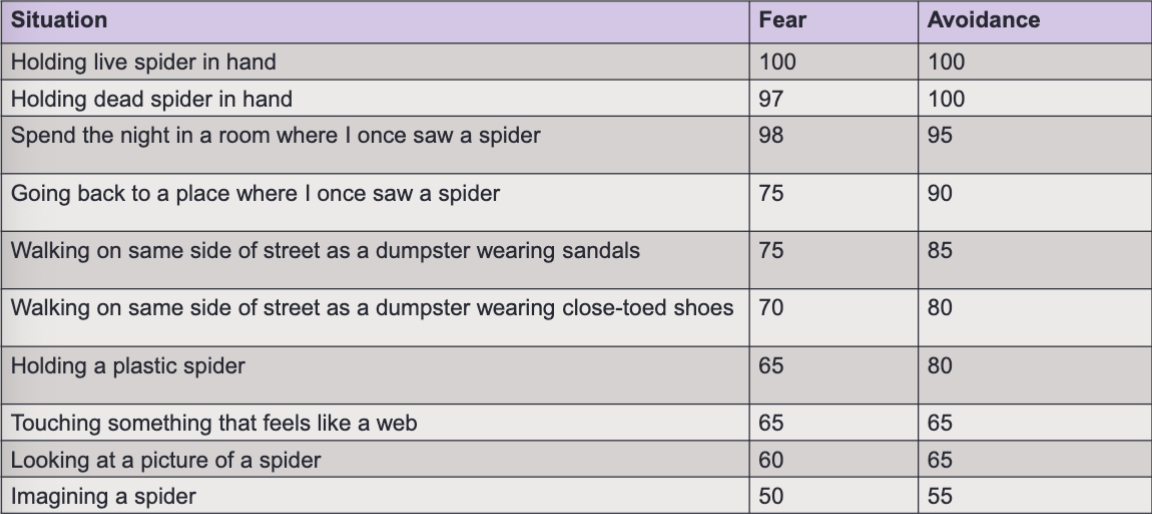
How are Fear and Avoidance Hierarchies individualized?
Every hierarchy is individualized to the client’s specific fears
Steps for effective exposure
Identify thoughts about situation before exposure occurs
Rate level of distress before exposure begins
During exposure, continue to rate distress every 5 minutes
During exposure, stay focused, do not try to distract self (avoidant behavior)
During exposure, maintain objective awareness of physical symptoms and thoughts
Continue exposure until anxiety goes down, 3 or 4 on a scale of 10 is optimal aka manageable feelings
After exposure, rate level of distress and evaluate thoughts again
Most important rule of anxiety treatment in general
Never stop an exposure before habituation occurs.
Otherwise, all that is reinforced is the sense that the anxiety producing stimulus is something that should be feared.
What are the 3 ways that exposures be conducted?
In session
In vivo (in life) - return to the place where the stimulus occurred
Imaginal
Goal for anxiety treatment
Realization that even though anxiety is uncomfortable, the risks of anxiety are minimal.
The goal is not to “get rid of anxiety”
Social Anxiety Disorder/Social Phobia (SAD) criteria
Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others. Examples include social interactions (ex. having a conversation, meeting unfamiliar people), being observed (ex. eating or drinking), and performing in front of others (ex. giving a speech)
Fear that you will act in a way or show anxiety symptoms that will be negatively evaluated (i.e. it will be humiliating or embarrassing, it will lead to rejection or offend others)
The social situations almost always provoke fear or anxiety
The social situations are avoided or endured with intense fear or anxiety
The fear or anxiety is out of proportion to the actual threat posed by the social situation and to the sociocultural context
The fear anxiety or avoidance:
is persistent, typically lasting 6+mo
causes clinically significant distress or impairment in social, occupational, or other important areas of functioning
not attributable to substances or another medical condition
not better explained by the symptoms of another mental disorder (ex. panic, body dysmorphic, or autism spectrum)
if another medical condition (ex. Parkinson’s obesity, disfigurement from burns or injury) is present, the fear/anxiety/avoidance is clearly unrelated or excessive