Cardiovascular Physiology Oct 2023
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
120 Terms
Aorta = small cross-sectional area
capillaries = large cross-sectional area
Rationale for higher blood velocity in the aorta than in the sum of all of the capillaries.
= lower velocity of blood in the capillaries optimizes conditions for exchange of substances across the capillary wall
Rationale for large cross-sectional areas in capillaries
Poiseuille equation
Equation / formula used in resistance
Capacitance (Compliance)
Describes the distensibility of blood vessels
DECREASES unstressed volume and INCREASES stressed volume by shifting blood from the veins to the arteries
Decrease in venous capacitance's effect on unstressed and stress volume
PR interval increases
Effect of decrease AV node conduction on PR interval
Positive staircase or Bowditch staircase (or treppe)
Increased heart rate increases the force of contraction in a stepwise fashion as the intracellular Ca increases cumulatively over several beats
Refers to the increase force of contraction in a stepwise fashion as the intracellular calcium increases cumulatively
Post-extrasystolic potentiation
The beat that occurs after an extrasystolic beat has increased force of contraction because "extra'' Ca has entered the cells during the extrasystole
Refers to the beat that occurs after an extrasystolic beat that has increased force of contraction
CO = 5000 mL/min and SV = 69.4 mL/beat;
Fick Principle for measuring CO:
· O2 consumption / O2 Pulmonary veins - O2 Pulmonary Artery
· CO = 250mL/min / (0.20mL - 0.15 mL O2/mL)
· SV = CO x HR
70-kg man;
· Resting O2 consumption = 250mL/min
· Systemic arterial O2 = 0.20mL O2/mL
· Systemic mixed venous O2 = 0.15mL O2/mL
· heart rate = 72 beats/min
What is his cardiac output?
What is his stroke volume?
Filtration;
(30 mmHg -0 mmHg) – (28 mmHg -4 mmHg) = +6mmHg
At the arteriolar end of a capillary;
· Capillary HP = 30 mm Hg
· Capillary OP = 28 mm Hg
· Interstitial HP = 0 mm Hg
· Interstitial OP = 4 mm Hg
Filtration or absorption?
Absorption;
(16 mmHg -0 mmHg) – (28 mmHg -4 mmHg) = -8mmHg
At the venous end;
· Capillary HP = 16 mm Hg
· Capillary OP = 28 mm H
· Interstitial HP = 0 mm Hg
· Interstitial OP = 4 mm Hg
Filtration or absorption?
Vasoconstriction;
Without vasoconstriction, blood flow would increase as a result of the increased pressure
Response of vessels in myogenic hypothesis during an increase in perfusion pressure
Vasodilation of coronary vessels
increases blood flow, and increases O2 delivery to the tissue to meet demand.
Response of coronary vessels during an increase in myocardial contractility and increase O2 demand
Decrease to 1/16
If the radius is decreased by 1/2, then resistance would increase by 2(4) or 16. But since blood flow is INVERSELY PROPORTIONAL to resistance, flow will decreased to 1/16.
50% narrowing of an artery leads to how much decrease in blood flow
Increased contractility
Baroreceptors detect the decrease in arterial pressure and thus activates the sympathetic outflow and decreases parasympathetic outflow.
Cardiac contractility compensation during change from supine to a standing position
Renal Artery
Pressure on the venous side is LOWER than the arteria side. Systolic pressure is slightly higher in the downstream arteries than in the aorta because of the reflection o pressure waves at BRANCH POINTS.
SBP is highest in which vessel?
Renal artery, Renal vein, Aorta, Pulmonary Artery
AV node
The absent P wave indicates that the atrium is not depolarizing and therefore, the pacemaker cannot be in the SA Node. Both QRS and T wave are positive, indicating that the depolarization and repolarization of the ventricles occurred in the normal sequence.
(-) P wave, (+) QRS complex, (+) T wave. Where is the pacemaker?
ESV
Increased EF causes and increase End Diastolic Volume since more blood is ejected out, thus smaller volume is left inside the heart after contraction - Lower End Systolic Volume
Increase in ejection fraction causes decrease in what cardiac parameter?
decreased pulse pressure because stroke volume is decreased
On the extrasystolic beat, pulse pressure decreases because there is INADEQUATE ventricular filling time; the ventricle beats too soon.
In ventricular extrasystoles, extrasystolic beat's effect on pulse pressure?
increased pulse pressure because the contractility of the ventricle is increased
Postextrasystolic contraction produces increased pulse pressure because contractility is increased. Extra Ca enters the cell during the extrasystolic beat.
In ventricular extrasystoles, next "normal" contraction's effect on pulse pressure?
Increased cardiac output for a given end-diastolic volume
Increase in contractility causes _____ in CO for a given end-_____ volume
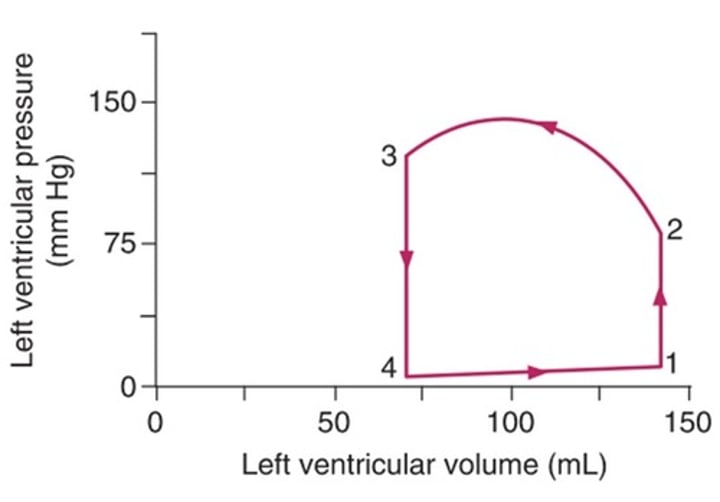
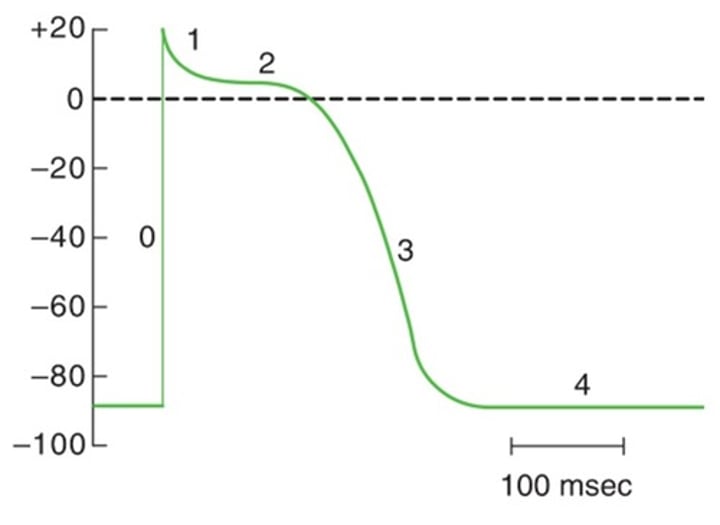
Points 1 to 2;
Isovolumetric contraction occurs during ventricular systole, before the aortic valve opens. Ventricular pressure increases, but volume remains constant because blood cannot be ejected into the aorta against a closed valve
locate isovolumic contraction
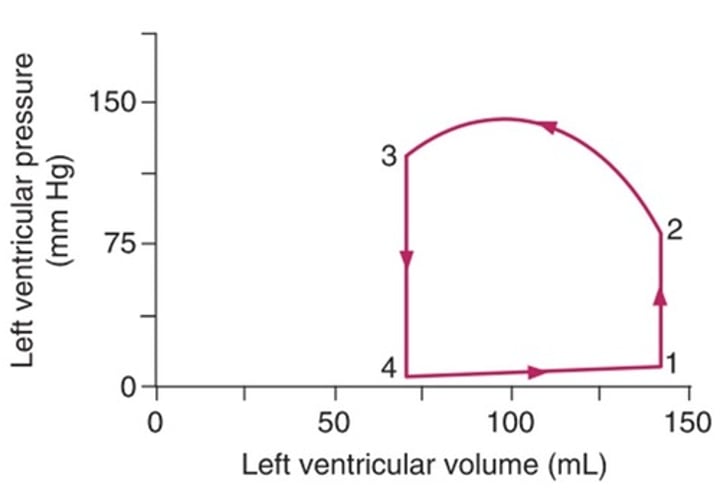
Point 3
ALL VALVES ARE CLOSED DURING Points 1-2 (Iso. Contraction) and Points 3-4 (Iso. Relaxation).
But, according to BRS, Point 3 is the answer; Closure of the aortic valve occurs once ejection of blood from the ventricle has occurred and the left ventricular pressure has decreased to less than the aortic pressure.
locate where Aortic valve closes
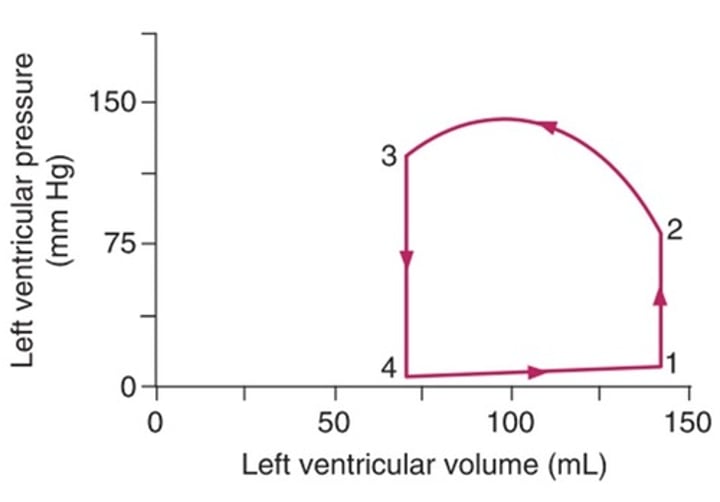
Point 1
The first heart sound corresponds to closure of the atrial ventricular valves. Before this closure occurs, the ventricle fills (phase 4 to l). After the valves close, isovolumetric contraction begins and ventricular pressure increases (phase 1 to 2).
Locate the first heart sound
[(30-(-2)) – (25-2)] mmHg = 32mmHg – 23mmHg = +9mmHg
Filtration; 9 mm Hg
· CapillaryHP = 30 mmHg
· CapillaryOP = -2 mm Hg
· InterstitialHP = 25 mm Hg
· InterstitialOP = 2 mm Hg
Direction of fluid movement and the net driving force?
Kf x net pressure = 0.5 x 9mmHg = 4.5 mL/min
· CapillaryHP = 30 mmHg
· CapillaryOP = -2 mm Hg
· InterstitialHP = 25 mm Hg
· InterstitialOP = 2 mm Hg
· Kf = 0.5 mL/min/mm Hg
What is the rate of water flow across the capillary wall?
Decreased viscosity,
increased velocity,
partial occlusion of a blood vessel
Factors of turbulent blood flow
a suppressed response of the baroreceptor mechanism
Normal baroreceptor mechanism responds to a decrease in arterial pressure through the vasomotor center by increasing sympathetic outflow and decreasing parasympathetic outflow; (+) sympathectomy = sympathetic component of the baroreceptor mechanism is absent
66/M, s/p sympathectomy, experiences a great fall in arterial pressure upon standing up. Explanation?
ST segment
Ventricles are completely depolarized in which portion of the ECG?
Left-to-right ventricular shunt
Pulmonary blood flow is greater than aortic blood flow in which type / direction of shunt?
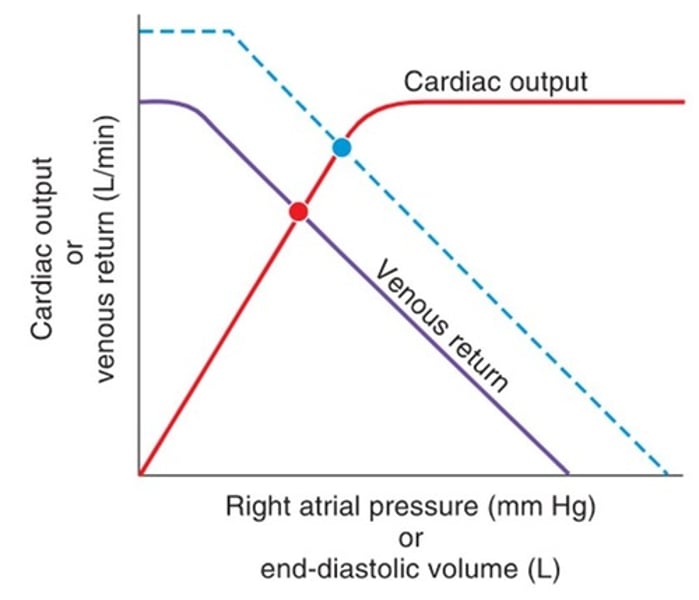
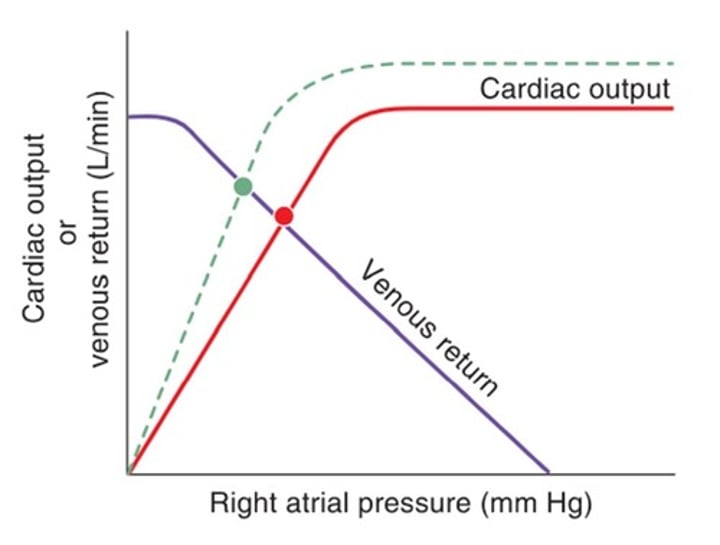
increased mean systemic filling pressure
The shift in the venous return curve to the right is consistent with an increase in blood volume and, as a consequence, mean systemic filling pressure.
The change indicated by the dashed lines on the cardiac output/venous return curves shows
decreased conduction through the AV node
this pattern indicates that ONLY EVERY OTHER P WAVE is conducted through the AV node to the ventricle.
2 P waves preceding each QRS complex. Interpretation?
Decreased firing rate of the carotid sinus nerve
Decrease parasympathetic outflow
Compensatory change in the carotid sinus during acute decrease in arterial blood pressure
increased venous pressure
Edema occurs when more fluid is filtered out of the capillaries than can be returned to the circulation by the lymphatics.
Tendency for edema to occur will be increased by _____ venous pressure
the aortic valve closes before the pulmonic valve
Rationale for inspiratory split of the second heart sound
Increase in local metabolites on skeletal muscle arterioles
Causes vasodilation
Rationale for decrease in total peripheral resistance during exercise
an increase in arterial pressure
Increase in arteriolar resistance, without a change in any other component. Effect on arterial pressure?
6.25 L/min;
CO = 500ml/min / (0.24mlO2/mL - 0.16mL O2/mL)
Fick Principle for measuring CO:
O2 consumption / O2 Pulmonary veins - O2 Pulmonary Artery
CVP: 10 mm Hg
HR: 70 beats/min
Systemic arterial 02 = 0.24 mL 0 2 /Ml
Mixed venous O2 = 0.16 mL 0 2/mL
Whole body O2 consumption: 500 mL/min
What is this patient's cardiac output?
Upstroke of the action potential in atria, ventricles and Purkinje fibers is the result of fast inward Na+ current.
Upstroke in SA node is due to inward Ca2+ current.
Result of an inward Na+ current
increased contractility
An upward shift of the cardiac output curve is consistent with an increase in myocardial contractility; for any right atrial pressure (sarcomere length), the force of contraction is increased.
Dashed line in the figure illustrates the effect of
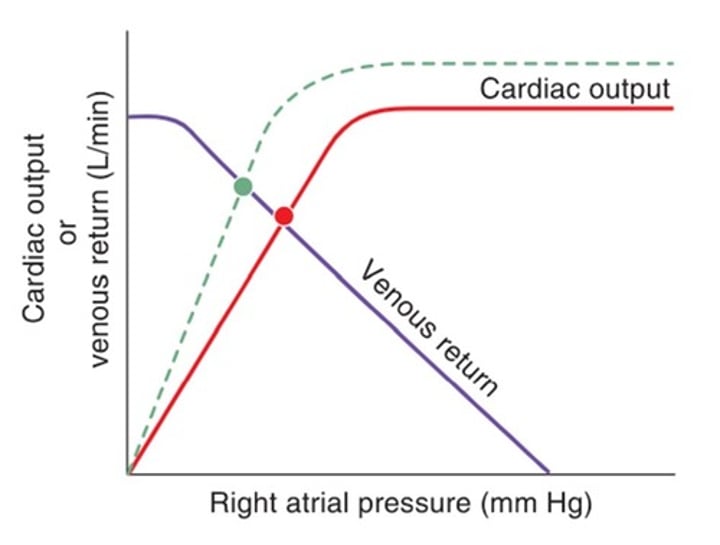
end-diastolic volume
End-diastolic volume and right atrial pressure are related and can be used interchangeably
x-axis in the figure could have been labeled
they have the greatest resistance
the greater the resistance is, the greater the decrease in arterial pressure
Rationale for why the greatest pressure decrease occurs across the arterioles
determined by stroke volume
Pulse pressure is the difference between the highest and lowest arterial pressure; reflects the volume ejected by the left ventricle
Pulse pressure is determined by what cardiac parameter
an increase in Na+ conductance
What conductance is increased in phase 4 depolarization of SA node?
Alpha-1 receptor
Receptor responsible for the increased splanchnic vascular resistance
Reduced ventricular ejection
Aortic pressure reaches its HIGHEST level immediately after the rapid ejection of blood during the left ventricular systole. This highest level actually COINCIDES with the beginning of the reduced ventricular ejection phase.
During which phase of the cardiac cycle is aortic pressure highest?
Calcium
Myocardial contractility is best correlated with what intracellular concentration
Vasodilation
Effect of histamine on arterioles
Brain
Blood flow to the brain is autoregulated by carbon dioxide.
Increase PCO2 will cause cerebral vasodilation, decrease PCO2 will cause cerebral vasoconstriction
Carbon dioxide regulates blood flow in which organ?
100%
CO of the left and right sides of the heart are equal
Cardiac output of the right side of the heart is what percentage of the cardiac outpute of the left side?
allow sufficient time for filling of the ventricles
Rationale for relatively slow conduction through the AV node
skin
Blood flow to which organ is controlled primarily by the sympathetic nervous system?
Decreased TPR
Although increased sympathetic outflow to the blood vessels might be expected to increase TPR, it does not because there is an overriding vasodilation of the skeletal muscle arterioles as a result of the buildup of vasodilator metabolites (lactate, K+ adenosine)
Effect on total peripheral resistance during exercise
Beta-1 receptor
72/W, being treated with propranolol. Blockade of which receptor is responsible for the decrease in cardiac output?
Isovolumetric ventricular relaxation
ventricular volume is at its lowest value while the ventricles is relaxed (diastole), just before ventricular filling begins
Ventricular volume is lowest in which phase of the cardiac cycle?
Increased size of the heart
Myocardial O2 consumption is determined by the amount of tension developed by the heart.
Heart size that causes an increase in myocardial O2 consumption
Glucose
O2, CO2, and CO are lipophilic, they cross primarily by diffusion through endothelial cell membranes.
Crosses capillary walls primarily through water-filled clefts between the endothelial cells;
Glucose, O2, CO2, OR CO
Decreased venous return.
Diarrhea causes loss of ECF volume, which already decreases arterial pressure that then increases HR in supine.
Upon standing, blood pools in the leg decreasing venous return and FURTHER decreasing arterial pressure and FURTHER activating the baroreceptors and FURTHER increasing HR on standing.
24/W with severe diarrhea;
· Supine BP = 90/60 mmHg
· Supine HR = 100 beats/min
· Standing HR = 120beats/min
What causes further increase in heart rate upon standing?
Left renal artery stenosis
right renal artery is non-stenotic since it is able to detect the increase in blood pressure, decreasing its renin secretion.
60/M, BP of 185/130 mmHg, increase in plasma renin activity, plasma aldosterone level, and left renal vein renin level. His right renal vein renin level is decreased.
Cause (diagnosis) of the hypertension?
Phase 4
Phase 4 is the resting membrane potential. Because the conductance K+ is highest, the membrane potential approaches the equilibrium potential for K+
Phase where membrane potential is closest to the K+ equilibrium potential
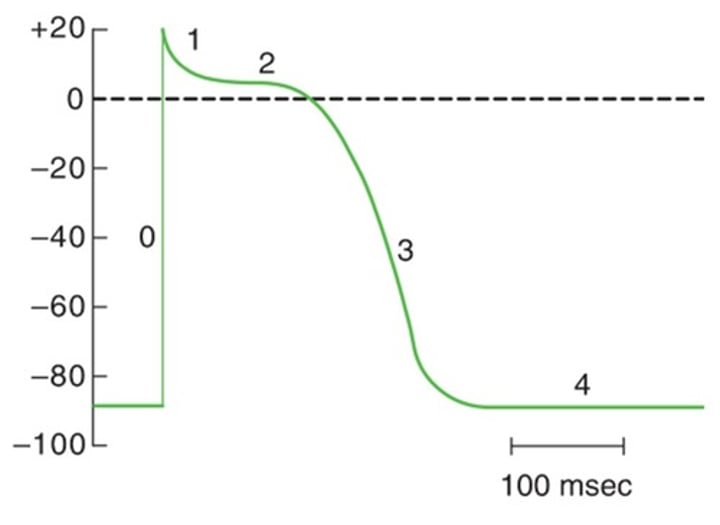
Phase 2
During this phase, the conductance to Ca2+ increases transiently. Ca2+ that enters the cell during the plateau is the trigger that releases more Ca2+ from the sarcoplasmic reticulum (SR) for the contraction.
Phase where calcium conductance is highest
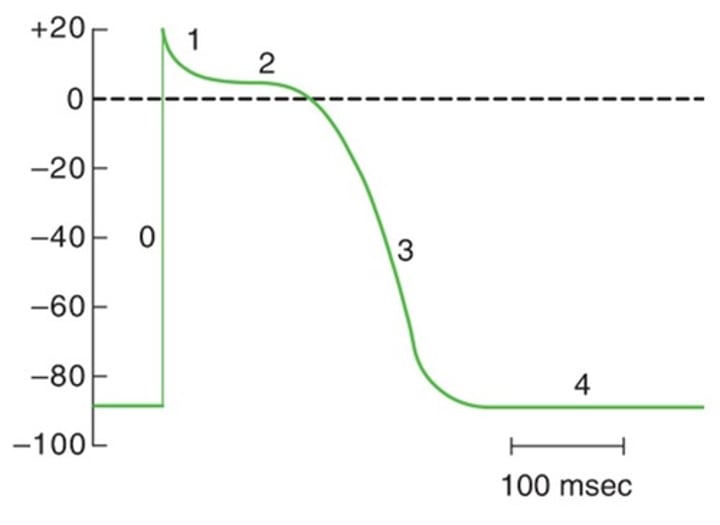
Phase 4
Phase 4 is electrical diastole.
Phase where ventricular action potential coincides with diastole
Decreases heart rate
Propanolol effect on heart rate
Muscarinic receptor (Parasympathetic)
Receptor that mediates slowing of the heart
Acetylcholine (Parasympathetic)
Neurotransmitter with negative inotropic effect on the heart
Gap junctions
Allow for the spread of action potentials between myocardial cells
Aldosterone
Angiotensin II, ADH and Aldosterone increases after decreased renal perfusion, of all these, only aldosterone has a direct function of increasing renal Na+ reabsorption.
released after a hemorrhage and causes an increase in renal Na+ reabsorption
Rapid Ventricular Filling
Blood rapidly flows from atrium to ventricles when the ventricular pressure is less than the atrial pressure
According to BRS, Isovolumetric ventricular relaxation
The mitral valve opens when left atrial pressure becomes HIGHER than left ventricular pressure. This occurs when the left ventricular pressure is at its lowest - when the ventricle is relaxed.
Cardiac cycle phase where mitral valve opens
92 mL; EDV = SV/EF
· CO = SV x HR; thus, SV = CO / HR
· SV = 3.5L/min x 95beats/min = 36.8mL
· EDV = SV/EF
· EDV = 36.8mL / 0.4
ejection fraction = 0.4
heart rate = 95 beats/min
cardiac output = 3.5 L/min
What is the patient's end-diastolic volume?
decreased blood volume, decreased preload, decreased cardiac output
38/W, with vomiting and diarrhea, light-headed upon standing. Explanation?
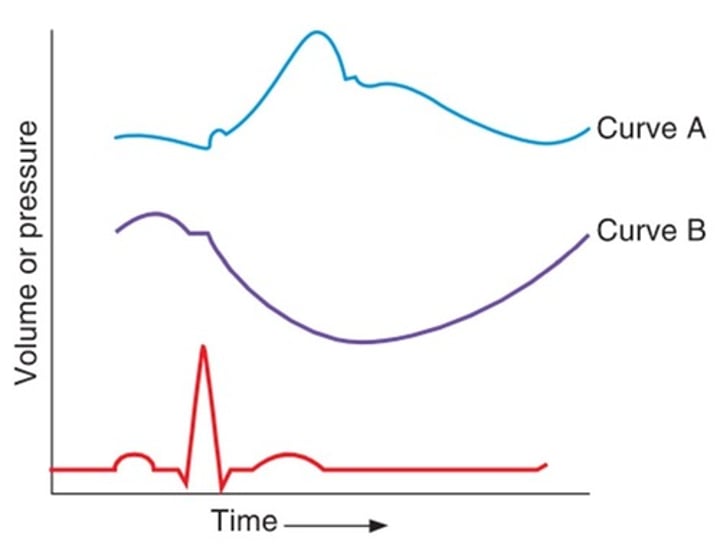
Aortic pressure
Aortic pressure increases steeply after QRS, as blood is ejected from the ventricles. After reaching peak pressure, aortic pressure decreases as blood runs off into the arteries. The characteristic dicrotic notch (dip in the aortic pressure curve) appears when the aortic valve closes.
Curve A in the figure represents
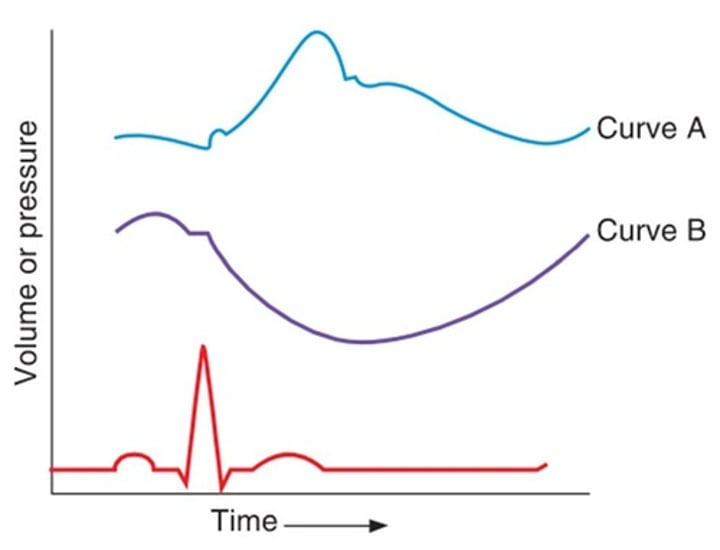
Ventricular Volume
Ventricular volume increases slightly with atrial systole (P wave), is constant during isovolumetric contraction (QRS), and then decreases dramatically after the QRS, when blood is ejected from the ventricle.
Curve B in the figure represents
CO = HR x SV = 60 beats/min x 70mL/beat = 4200mL/min
70kg healthy male with HR of 60beats/min. CO?
CO also increases
(based on Frank-Starling and Bainbridge reflex)
What happens when VR increases?
beta-1 blockers
Drugs that decreases heart rate
decrease to 1/16
BRS: 50% narrowing of left renal artery, expected change in flow?
Carotid and aortic body chemoreceptors
BRS: Hypoxemia produces hyperventilation by direct effect on the
it increases cardiac contractility
effect of digoxin
dromotropy
AV node: inotropy, chronotropy, dromotropy or lusitropy
pulmonic valve, aortic valve
Two valves that open during systole
B-Type Natriuretic Peptide
(BNP or Brain Natriuretic Peptide)
Released by Ventricular myocytes due to increased tension
1st degree AV block
AV block that does NOT require treatment
decreased arteriolar vasoconstriction (decreased arteriolar resistance), increased sodium excretion by the kidneys to the urine, decreased cardiac output
Effects of ACE-I
presence of collateral vessels
most cases of patient recovery from coronary occlusion is due to
Macrolides, etc.
Drug that can cause torsades de pointes
between Rapid ventricular ejection and reduced ventricular ejection
Aortic pressure is highest during this cardiac cycle phase
Vitamin B1 or Thiamine
(can cause CHF or wet beriberi)
Vitamin deficiency that can cause heart failure
increased Cardiac output for a given EDV
Increased contractility in the Frank-Starling diagram is demonstrated by
Actin, Tropomyosin, Troponin
Components of thin filament of cardiac muscle
V = Q/A
Where
v = velocity(cm/sec)
Q =blood flow (ml/min)
A = cross-sectional area (cm2)
Formula that relates blood flow, velocity and cross-sectional area
Stroke Volume
Volume ejected from the ventricle after each heart beat
Q = deltaP/R
What again is Ohm's Law
Cardiac Output
Based on Ohm's Law, Pulmonary vascular resistance is (Pulmonary Artery Pressure - L Atrial Pressure) over _________
R Bundle Branch Block, Pulmonary Stenosis, , Mitral Valve Regurgitation, VSD
Conditions associated with exaggeration of normal splitting (Wide Split S2)
ASD
Fixed Splitting is auscultatory hallmark of
EF = SV / EDV. CO = HR x SV
Some Important Cardio formulas
Right Atrium
Cardiac chamber to measure central venous pressure
T-wave
ECG wave indicating ventricular repolarization
Calcium Influx
Causes spike potential in SA node AP
Closure of semilunar valves
Happens during S2