Smoking
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
Smoking prevalence
Alarming prevalence - 1.3 billion smokers worldwide
Contributing to over 8 million deaths worldwide each year and significant health associated complications
Major cause of preventable morbidity and mortality in the developed world
Smoking in Australia
11.1% daily smokers aged > 18 years
20,000 deaths annually
Over $32 billion in health, social and economic costs
7.6% of the total burden of disease and injury
70% of total disease burden from lung cancer and chronic obstructive pulmonary disease (COPD)
Smoking facts
Contributing death of one-third to one-half of all lifetime users.
Kills more than AIDS, legal drugs, illegal drugs, road accidents, murder and suicide combined
Hundreds of thousands of deaths annually associated with second-hand smoke
Nicotine dependance
Mental, behavioral or neurodevelopmental disorders dur to substance use
Chronic condition (similar to diabetes and hypertension)
Characterized by remission and relapse
Hard to cure
Nicotine dependance
Classified as ‘tobacco use disorder’ in DSM-V
Presence of at least 2 of the following criteria:
Impaired control: taking more or for longer than intended. Unsuccessful efforts to stop or cut down use. Spending a great deal of time obtaining, using or recovering from use. Craving for the substance
Social impairment: failure to fulfil major obligations due to use. continued use despite problems caused or exacerbated by use. Important activities given up or reduced because of substance use
Risky use: recurrent use in hazardous situations. Continued use despite physical or psychological problems that are caused or exacerbated by substance use
Pharmacological dependance: tolerance to the effects of the substance, withdrawal symptoms when not using or using less of the substance
Pharmacokinetics of nicotine
Colorless and odorless naturally occurring alkaloid
Short half-life of 40-120 min
Whole life up to 20 hours
Nicotine is the most addictive but not the most harmful substance in a cigarette
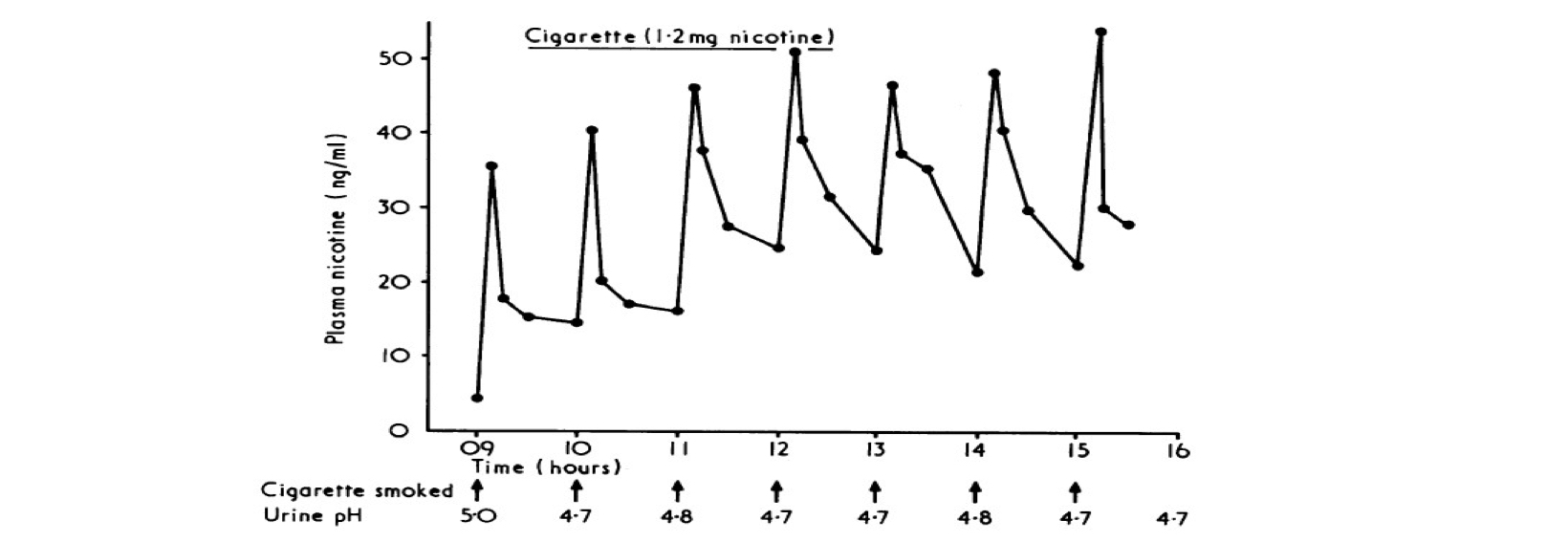
Pharmacokinetics of Nicotine
Nicotine plasma concentration range 10-80 ng/ml
Nicotine plasma concentration range 20-35 ng/ml for regular smokers
Pharmacokinetics of Nicotine
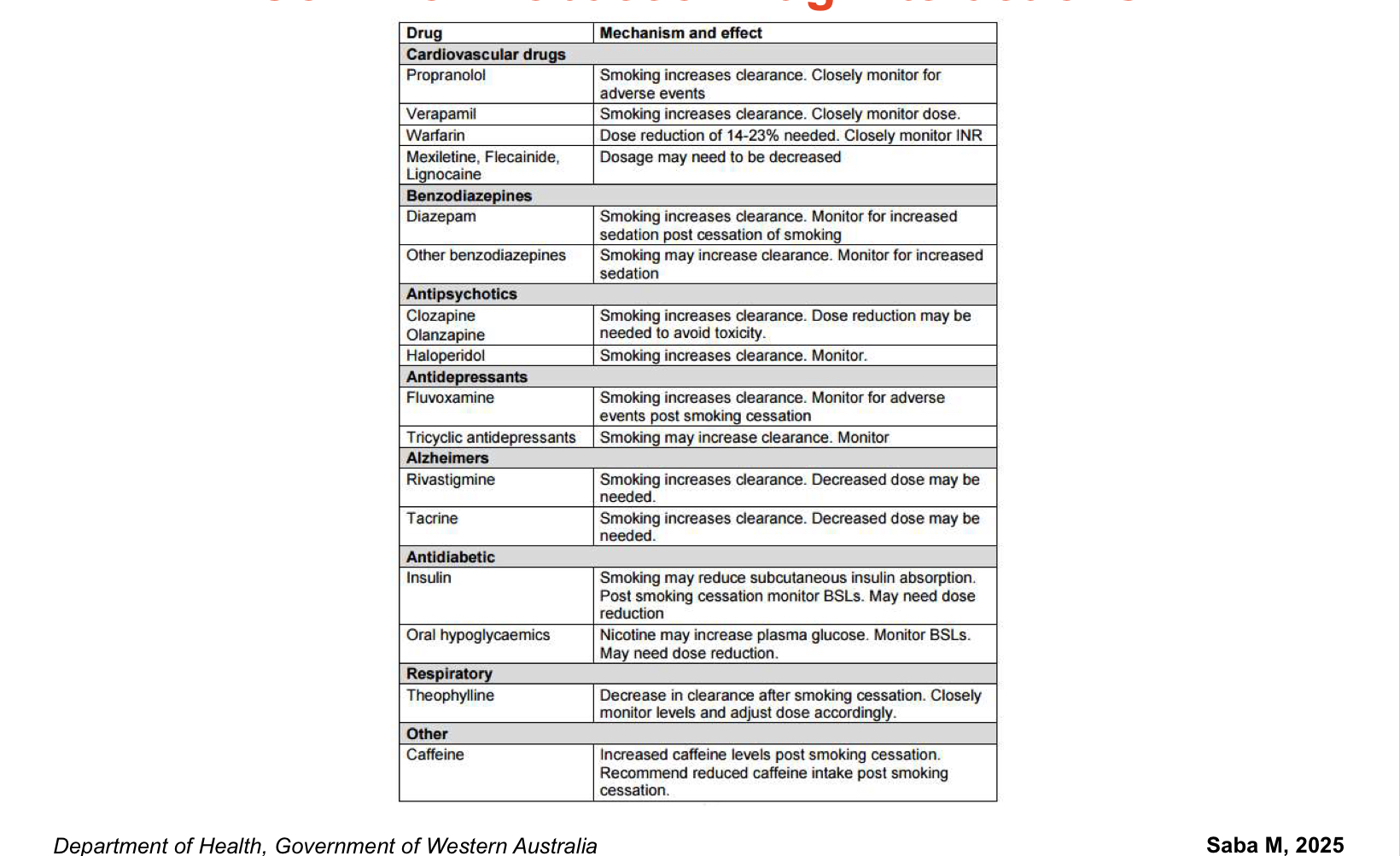
Metabolized by CYP2A6 mainly, CYP2B6, CYP2E1 and CYP1A2
Cotinine: nicotine’s major non-addictive metabolite
Induction of CYP1A2 and CYP2B6 by smoking (via chemicals in cigarette smoke such as polycyclic aromatic hydrocarbons)
Major tobacco-associated drug interactions
Common Tobacco-drug interactions
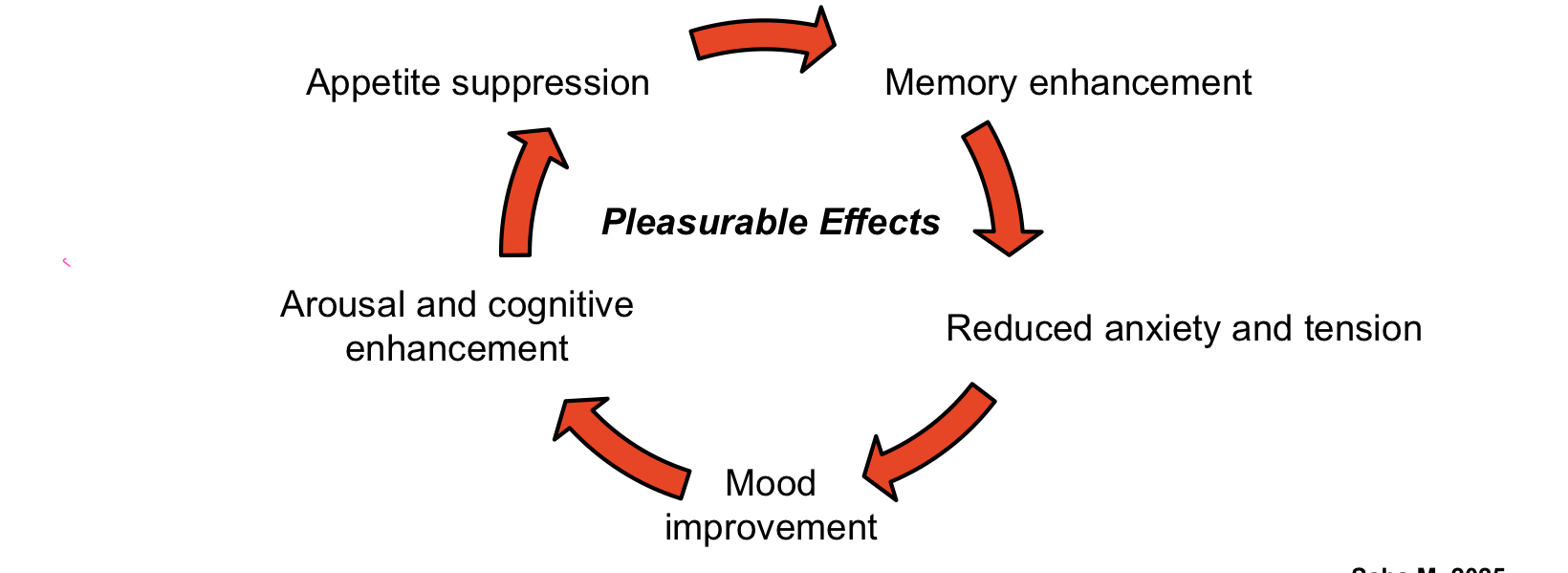
Pathophysiology of Dependance
Absorption of nicotine by the respiratory tract
Rapid absorption into the pulmonary venous circulation
Reaches brain in less than 10-20 sec
Pathophysiology of Dependance
Activation of dopaminergic receptors- DA release
Widespread neuronal activation by nicotine and dopamine
Release of rewarding neurotransmitters
Pathophysiology of Dependance
Desensitization and upregulation of receptors with chronic exposure
Tolerance
Decreased responsiveness to nicotine as body adapts to its presence
Increasing dose of nicotine required to obtain same effects
Dependance
Withdrawal symptoms upon reduction or abstinence
Strong tendency to relapse post quitting
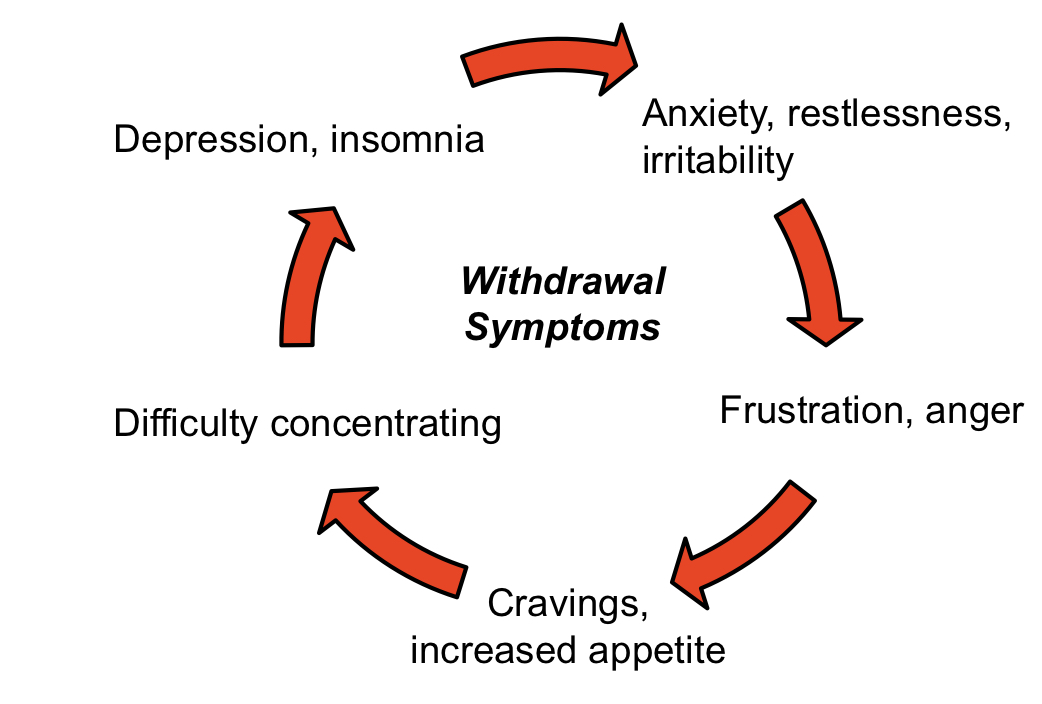
Withdrawal symptoms
Increased noradrenergic outflow secondary to deactivation of reward system
More smoking & failed quit attempts
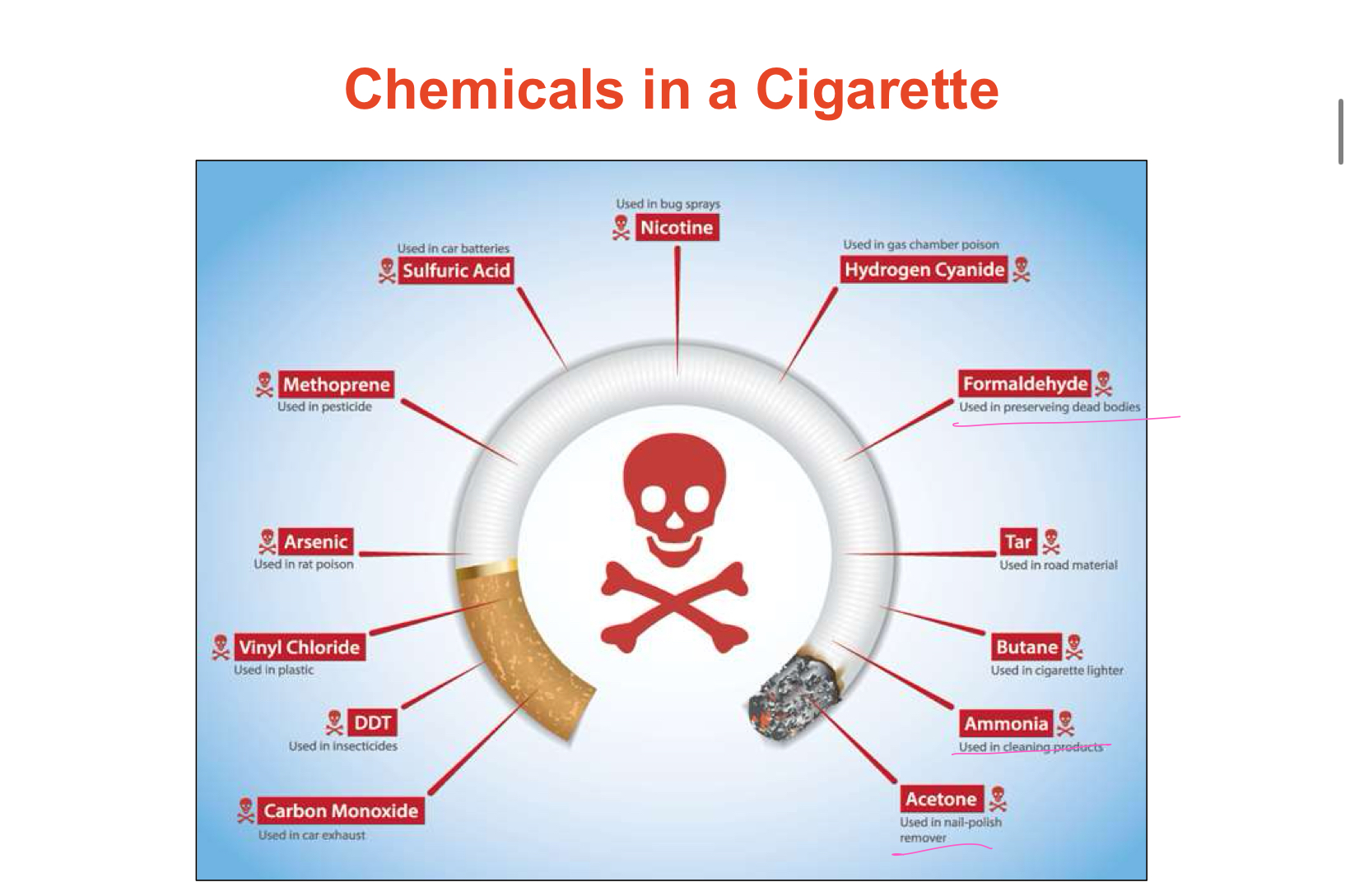
Chemicals in a cigarette
4000 toxins inhaled/cigarette smoked
>40 clinically proven carcinogens
Polycyclic aromatic hydrocarbons and Nitrosamines - DNA damage
Hundreds of additives and flavorings
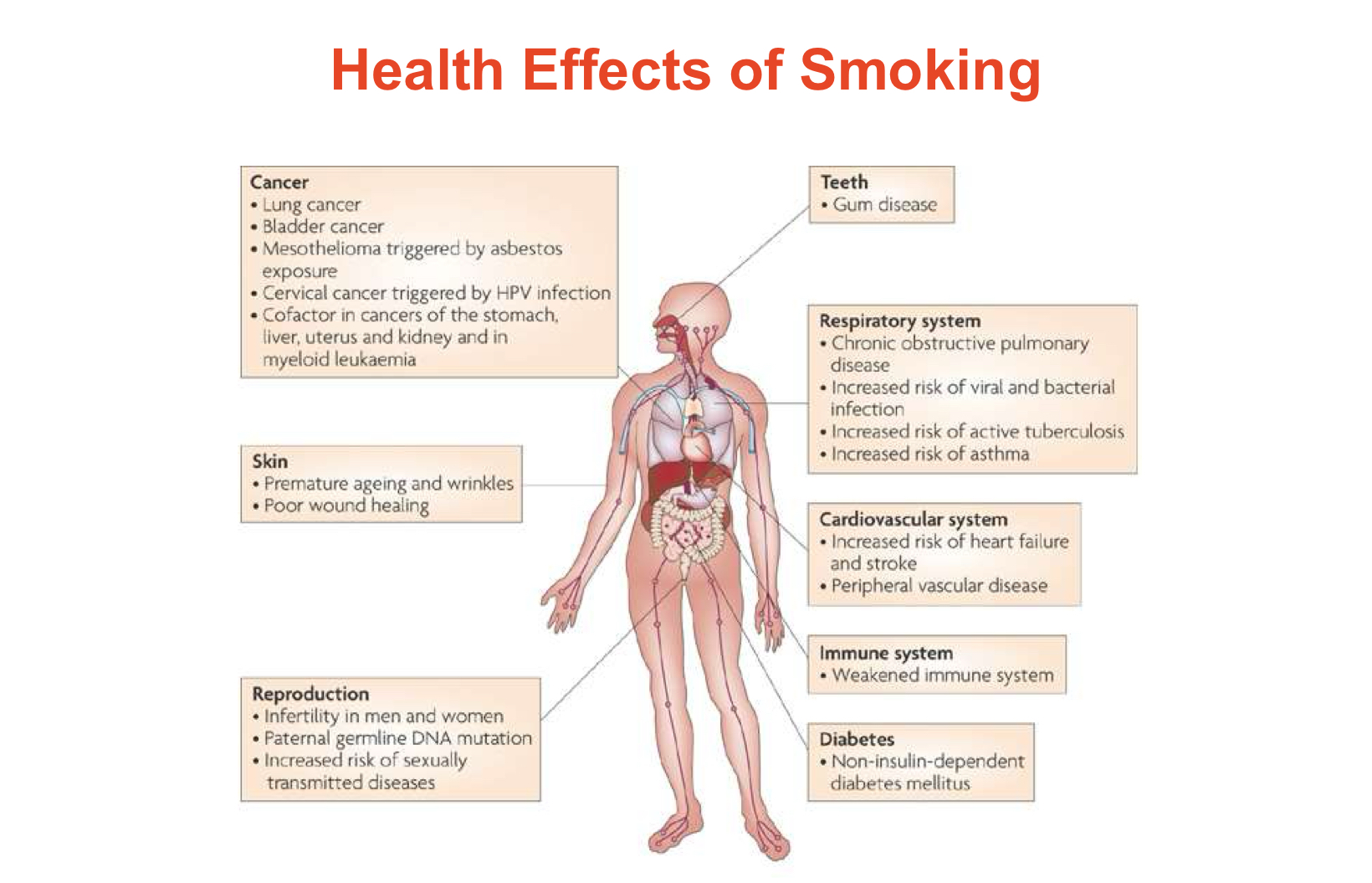
Detrimental effects on:
Vital organs
Immune system
Key body functions
Life expectancy
Health effect of smoking
Benefits of smoking
24 hours: Lungs starts to clear out mucus and other smoking debris
48 hours: Carbon monoxide is eliminated from body. The senses of taste and smell are improved
72 hours: Breathing becomes easier. Bronchial tubes start to relax. Energy levels increase
2-12 weeks: Circulation improves
3-9 months: respiratory problems improve as lung function is increased by up to 10%
1 year: Risk of heart attack decreases by half that of a continuing smoker
10 years: Risk of lung cancer decreases by half that of a continuing smoker
15 years: Risk of heart attack becomes similar to someone who has never smoked
Quitting before or during pregnancy: Risk of miscarriage, preterm delivery, low birth weight baby and sudden infant death syndrome decrease.
Smoking Cessation in Pharmacy - Role of pharmacists
Apply the 5As of quitting
Ask the patients if they use tobacco products
Advise them to quit
Assess their nicotine dependance level and their willingness to quit
Assist with pharmacotherapy and counselling
Arrange follow up to prevent relapse
Role of pharmacists: Applying the 5Rs of quitting- For patients unwilling to attempt quitting
Relevance: Why quitting is relevant to their health scenario
Risk of ongoing smoking habits
Rewards: benefits of smoking cessation
Roadblocks or impediments to quitting (withdrawal symptoms, fear of weight gain, social situations)
Repetition: most need multiple quit attempts
Role of pharmacists-Brief intervention
Applying the AAH
Ask the patients if they use tobacco products
Advise them to quit and advise that using pharmacotherapy and behavioral interventions is the most effective way
Help by offering pharmacotherapy and referral to behavioral pathways such as quilting
Assessment of Nicotine Dependance
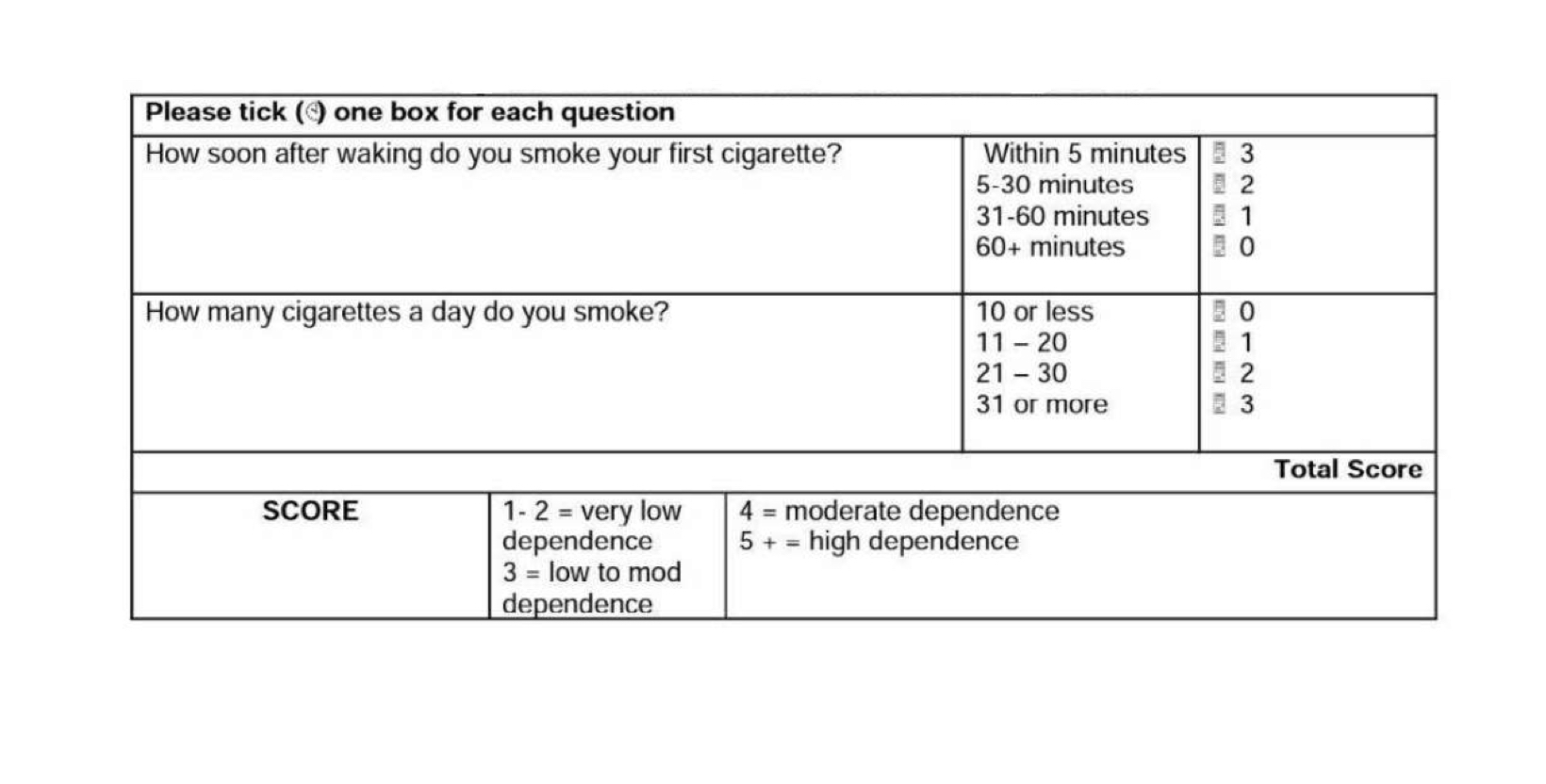
Fagerstrom test for nicotine dependance
Heaviness of smoking Index (HSI)
Expired CO levels using a CO monitor
Carboxyhemoglobin levels (COHb)
Urinary, saliva or blood cotinine levels
Fagerstrom test
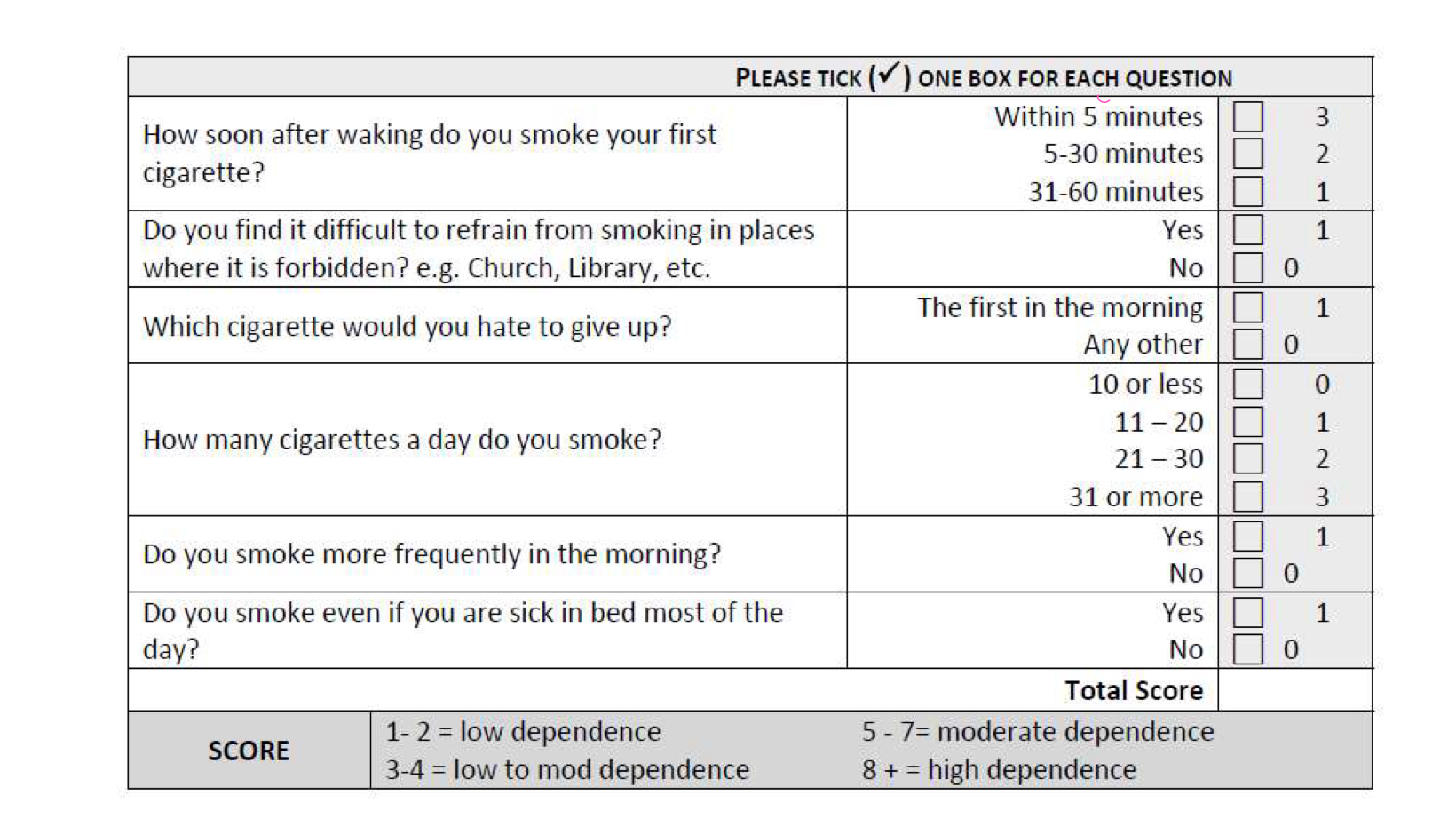
Heaviness of Smoking index
it’s not about the number of cigarette but the criteria
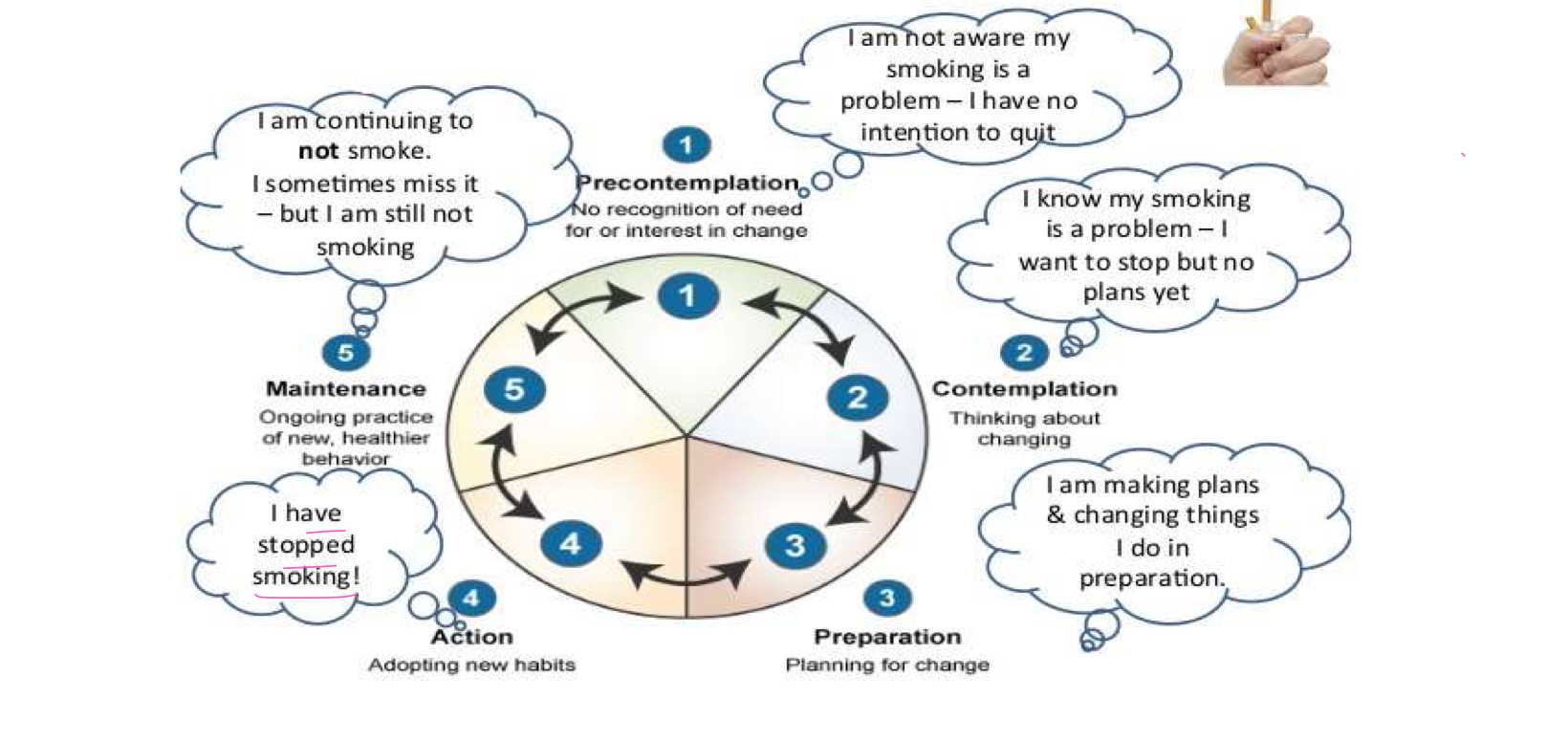
Assessment of willingness to change
Stages of change model
Pharmacological interventions
Nicotine replacement therapy (NRT)
Gums
Lozenges
Transdermal patch
Quick Mist mouth spray
Inhalator (being discontinued)
Nasal spray (not available in Australia)
Varenicline
Bupropion
Others: Cytisine
When you would you recommend applying the patch as it has a side effect of vivid dreams?
at night because it’s a slow-release formulation, it’s peak will be in the morning. the smoker will be awake and won’t experience these side effects
Nicotine Replacement Therapy
Equal efficacy of all forms of NRT
Nicotine delivery effects (in decreasing order)
Cigarette
Spray
Inhalator
Lozenge/Mini Lozenge/Gum
Patch
Smoking while on NRT is NOT contraindicated
Instructions for use - GUM
Chew 1 piece of gum slowly, until flavors become strong or a slight peppery tingling sensation is felt
Park between the cheek and gum
Chew again when flavor fades
Repeat until there is no more tingling for about 30 minutes
Instructions for use - Lozenge
Place lozenge between the cheek and gum, suck slowly until taste is strong
Stop sucking until taste fades, resting the lozenge against the cheek
Continue to suck again when taste fades
Move lozenge occasionally from side to side
Repeat until lozenge has completely dissolved
The whole process should take 20-30 minutes for lozenges and 10-13 minutes for mini lozenges
Instruction for use - Mouth spray
Point the spray nozzle towards the open mouth, holding it as close as possible
Press the top of the dispenser to release one spray into the mouth, avoiding the lips
For best results, avoid swallowing for a few seconds after spraying
Instructions for use- Inhalator
Insert cartridge into mouthpiece
Take a shallow puff every 2 seconds or take 4 deep puffs every minute
Continue for up to 20 minutes
Replace cartridge
Instructions for use - Patch
Apply the path in the morning or bedtime
Remove before bedtime if applied in the morning or remove in the morning if applied at bedtime (16 hours) or replace the next day (24 hours)
Patches should be applied to clean hairless skin on chest or upper arm
Rotate site each day
Do not cut patches in half
Swimming and bathing are allowed 1-hour post-application
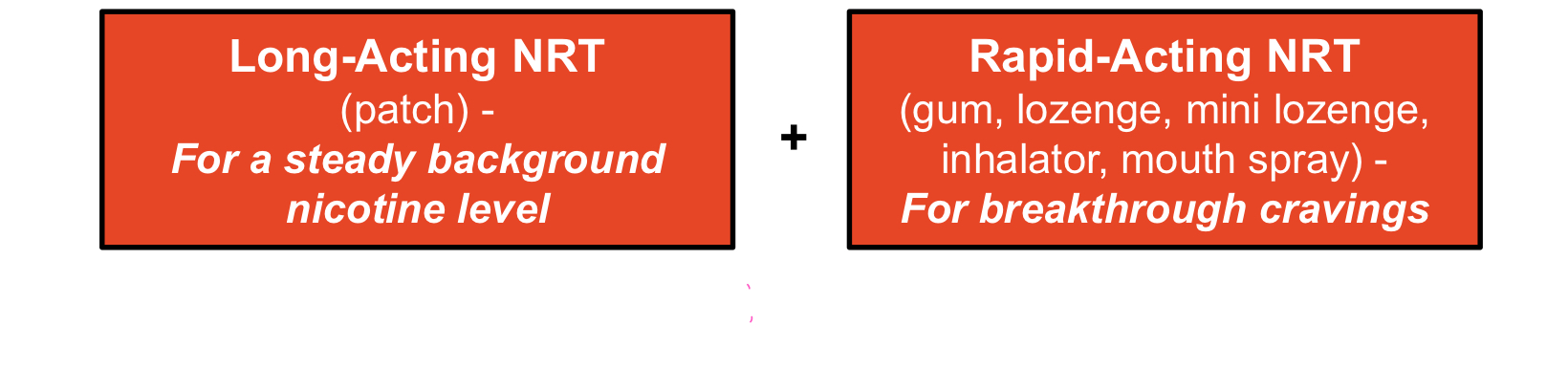
Nicotine replacement therapy
Combination therapy more effective than monotherapy
Double successful quit rates with combinational NRT
Establishes safety
First line pharmacotherapy = Varenicline
Varenicline
Dosage form:
Prescription only
0.5 mg (white) & 1 mg (blue) oral tablets per pack
Day 1-3: 0.5 mg daily
Day 4-7: 0.5 mg twice daily
Day 8 - week 12: 1 mg twice daily
Benefits:
Partial agonist acting centrally on a4b2 nicotine receptors, simulating dopamine release, thus reducing cravings and withdrawal symptoms
Antagonist preventing stimulation of receptors by nicotine, thus decreasing the pleasurable effects achieved from smoking and the risk of full relapse after temporary lapse
3-fold increase in odds of successful long-term quitting as compared to pharmacologically unassisted attempts
Adverse effects:
Mild to moderate nausea in 30% of patients, generally diminishing with time
Headache
Insomnia
Vivid dreams
Reports of serious neuropsychiatric events including depression and suicidal thoughts in some patients.
Precautions / contraindications:
Cautions in patients with underlying psychiatric illnesses - Monitor closely
Dose adjustment in severe renal impairment
Not recommended in pregnancy, breastfeeding and in smokers under the age of 18 due the lack of conclusive evidence
Contraindicated in hypersensitivity to any ingredient
Comment:
Recommended 12-week course of therapy for increased chances of success
No significant increase in CV adverse effects
Equally effective to combination NRT
Available on PBS
Bupropion
Dosage form:
Prescription only
150 mg tablets
150 mg for 3 days
150 mg BD for the remaining 53 days (7.5 weeks)
Benefits:
Selective dopamine/norepinephrine reuptake inhibitor, thus reducing cravings and nicotine withdrawal symptoms
Nicotinic receptor antagonist
Double the success rates of quitting at 6 months as compared to placebo
Efficacious in patients with depression, cardiac and respiratory diseases
Adverse effects:
Insomnia
Headache
Nausea
Dry mouth
Dizziness
Anxiety
Precautions / contraindications:
Seizure/epilepsy
Head injury
Brain tumors
Past/current history of anorexia / bulimia nervosa
pregnancy and lactation
Patients under 18 years of age
Concomitant or recent use within the last weeks of MOA inhibitors
Severe hepatic diseases
End-stage renal disease
Acute withdrawal from benzodiazepines or alcohol
Hypersensitivity
Comments:
Less frequently prescribed antidepressants for smoking cessation
Highest success rates when prescribed with NRT - monitor for blood pressure
Recommended therapy for 8-12 weeks
Available on the PBS
Cytisine
Inexpensive plant derived alkaloid
Partial nicotinic receptor agonist (a4b2 subunit)
Approved and used in Central and Eastern Europe and Central Asia for several decades
1.5 mg tablets used over 25 days (titration method)
Varenicline derived from Cytisine (analogues)
Established effectiveness for promoting smoking cessation
Cytisine at least as effective as varenicline in supporting abstinence rates at 6 months
Common side effects: GI problems, headaches, irritability, nausea, constipation, difficulty sleeping, tachycardia
Contraindicated in arterial hypertension and advanced atherosclerosis
TGA interim decision creates a Schedule 3 entry (i.e., a pharmacist-only medicine) for cytisine for divided oral and oro-mucosal preparations with a maximum of 9 mg as a smoking cessation aid for adults, and a Schedule 4 entry (i.e., prescription only) for all other preparations of Cytisine
There are currently no TGA approved products on the market containing cytisine
Pharmacotherapy Combinations
Combinations therapy:
Two forms of NRT
Patch and gum/lozenge/mouth spray
Varenicline and NRT
Bupropion and NRT
Bupropion and patch
Varenicline and Bupropion
Nicotine vaping products in smoking cessation
There are currently no nicotine vaping products approved by the TGA and registered in Australian Register of Therapeutic Goods (ARTG)
Pharmacotherapeutic considerations
Clinical eligibility
Past experiences and outcomes
Patient preferences / convenience
Cost
Compliance and adherence complications
Non-pharmacological Interventions
Avoid triggers
Changing routines / shifting to reinforcing alternatives
Adequate rest and relaxation
Exercise
Healthy diet
Avoiding secondhand smoke
Summary
Smoking cessation interventions, provided by healthcare professionals can significantly increase quit rates
Evidence based pharmacotherapy represents the cornerstone of smoking cessation interventions
Clinical eligibility, previous therapy, patient preference, convenience and cost are essential criteria for guiding the choice pharmacotherapy