Urinary System
1/76
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
77 Terms
Urinary System Functions
removal of wastes from blood
and toxins/medications
formation/concentration of urine
storage of urine
excretion of urine
regulation of homeostasis
electrolytes, blood pressure, erythrocyte levels, H2O
4 Homeostatic Functions of Urinary System
regulates blood volume and blood pressure
regulates plasma ion concentrations
helps stabilize blood pH
conserves valuable nutrients
Regulates Blood Volume and Blood Pressure
by adjusting volume of water lost in urine
releases renin
releases erythropoietin (increases O2 in blood)
Regulates Plasma Ion Concentrations
sodium, potassium. and chloride ions (by controlling quantities lost in urine)
calcium ion levels (through synthesis of calcitriol (vit D))
Helps Stabilize Blood pH
by controlling loss of hydrogen ions and bicarbonate ions in urine
Conserves Valuable Nutrients
by preventing excretion while excreting organic waste products
Parts of Urinary System
kidneys (2)
ureters (2)*
urinary bladder (1)*
urethra (1)*
*part of urinary tract
Location of the kidneys? Peritoneum?
kidneys are retroperitoneal (behind the peritoneum)
peritoneum = double layer membrane that surrounds most abdominal organs
Kidneys are held in place by:
the overlying peritoneum
contact with adjacent organs
supporting connective tissues
fibers capsule, perinephric fat capsule, renal fascia
all three layers connected by collagen fibers and anchored to peritoneum and deep fascia posteriorly
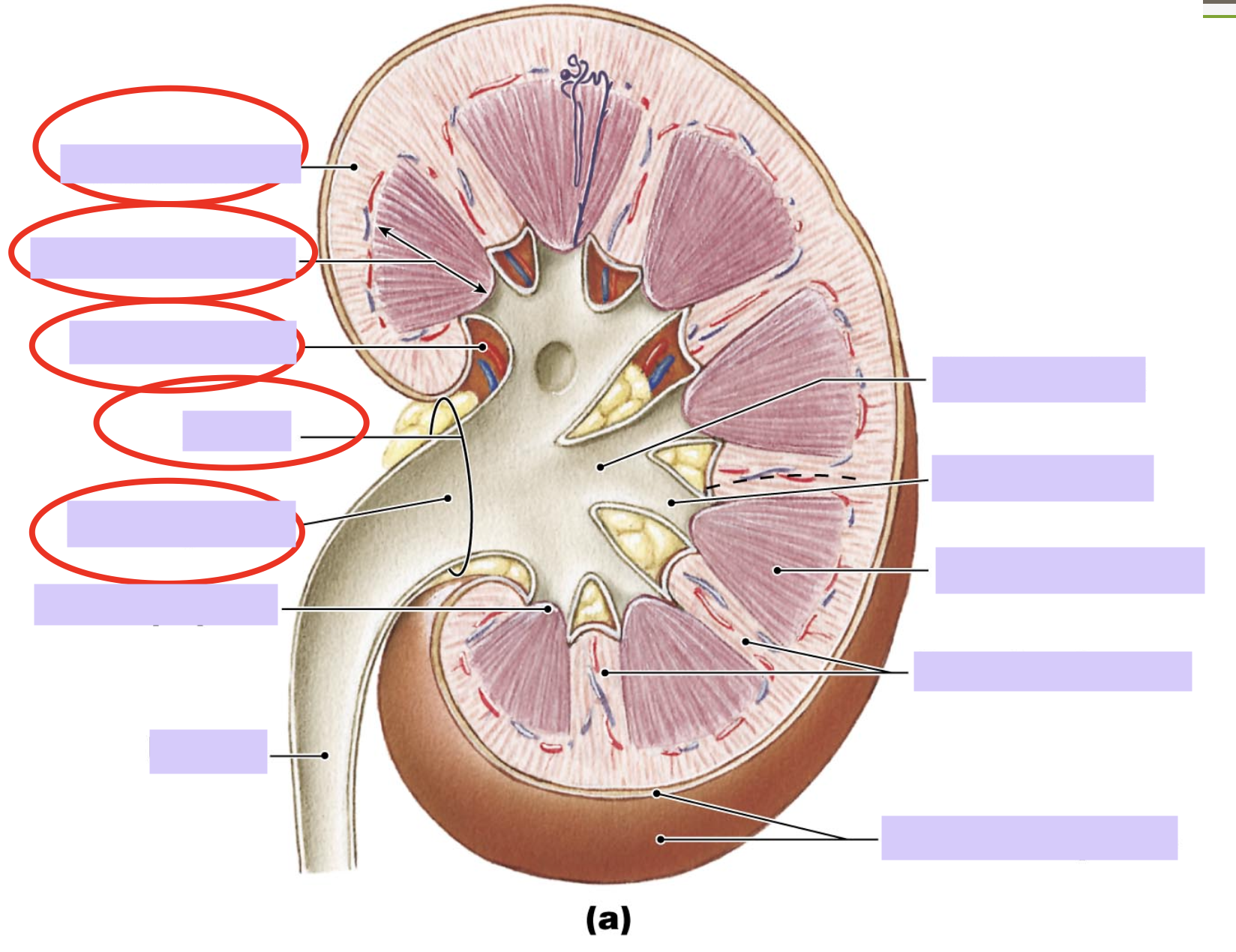
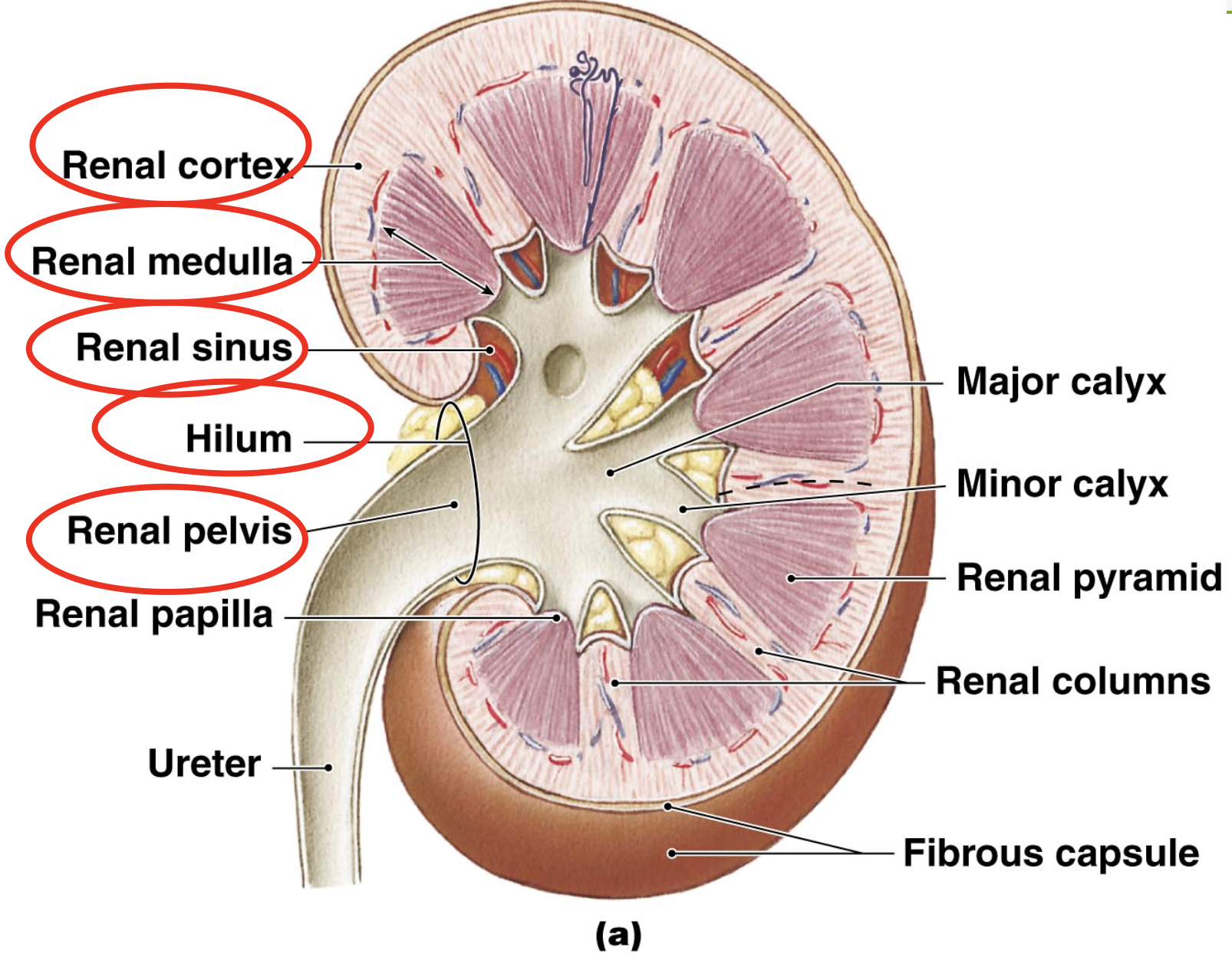
Parts of Kidneys
hilum- medial depression, entry/exit point for renal artery/vein.nerve and ureters
renal sinus- space/cavity within medial kidney, contains renal pelvis
cortex- area closest to renal capsule laterally
medulla- inner layer (medial to cortex)
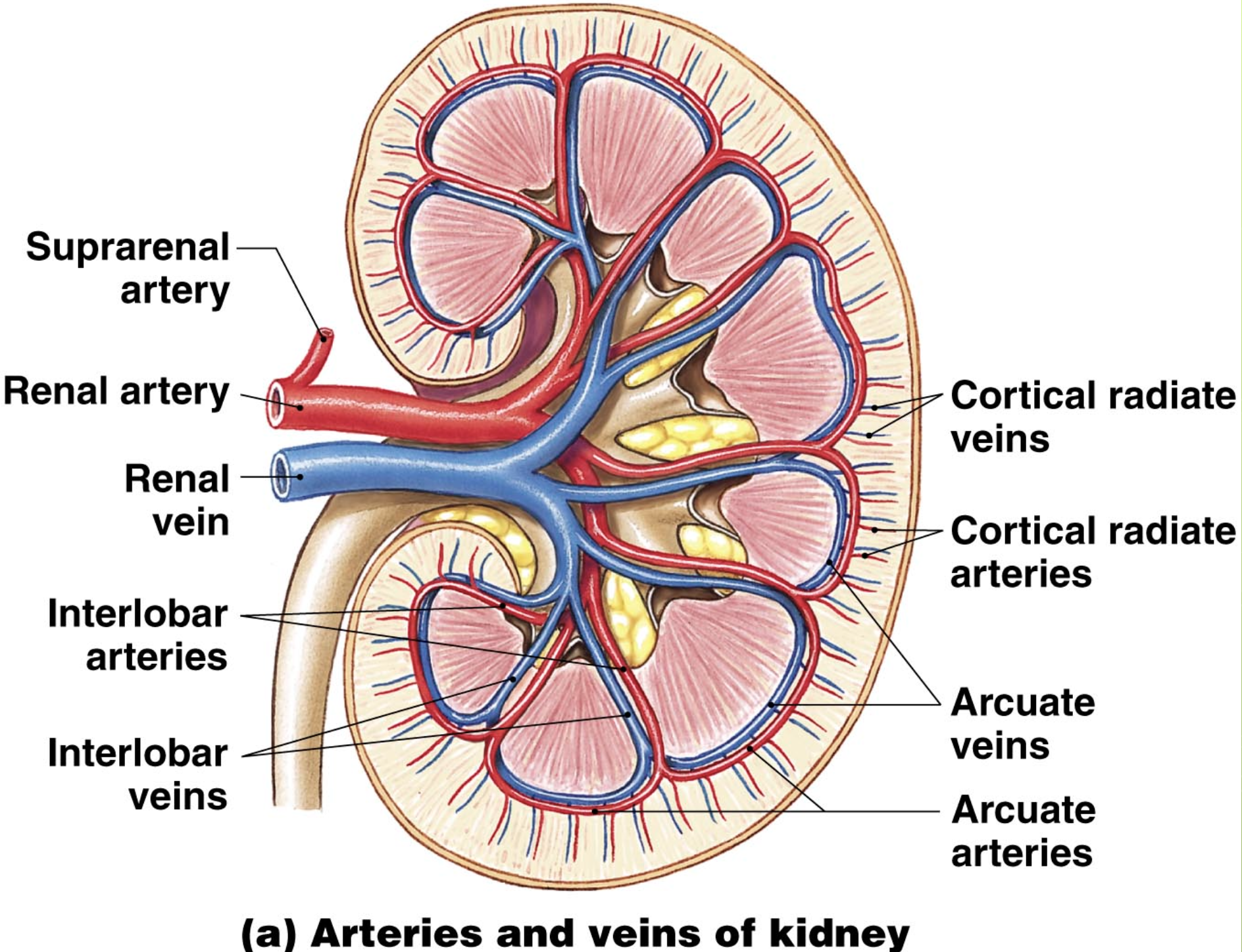
Blood Flow Through Kidneys
kidneys receive 20% to 35% to total cardiac output
1200mL of blood flows through kidneys each minute
kidney receives blood through renal artery
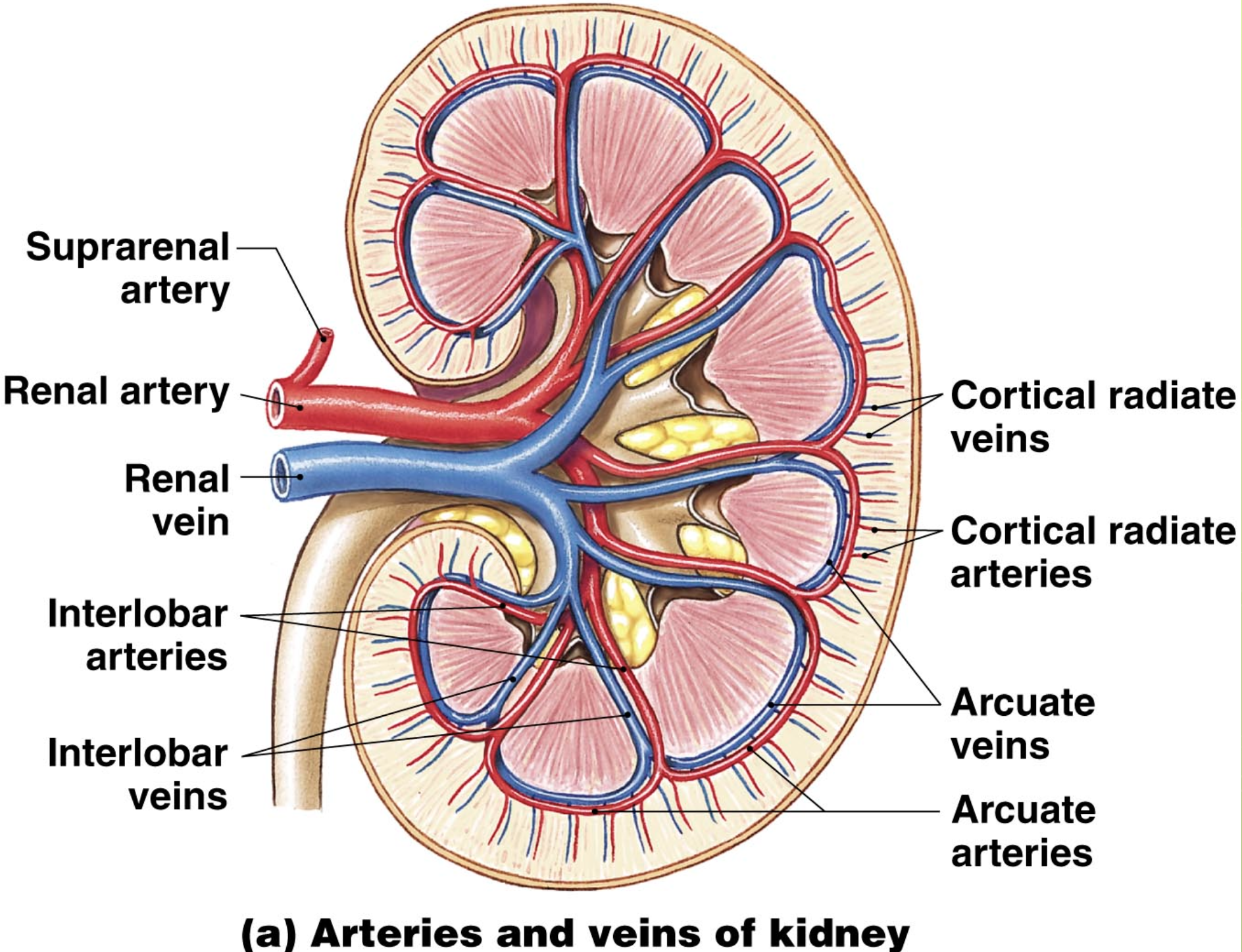
Artery blood flow in kidneys
renal artery enters kidney at hilum and branches as it flows toward the cortex
segmental arteries- in renal sinus
interlobar arteries- travel through renal columns
arcuate arteries
cortical radiate arteries
afferent arterioles
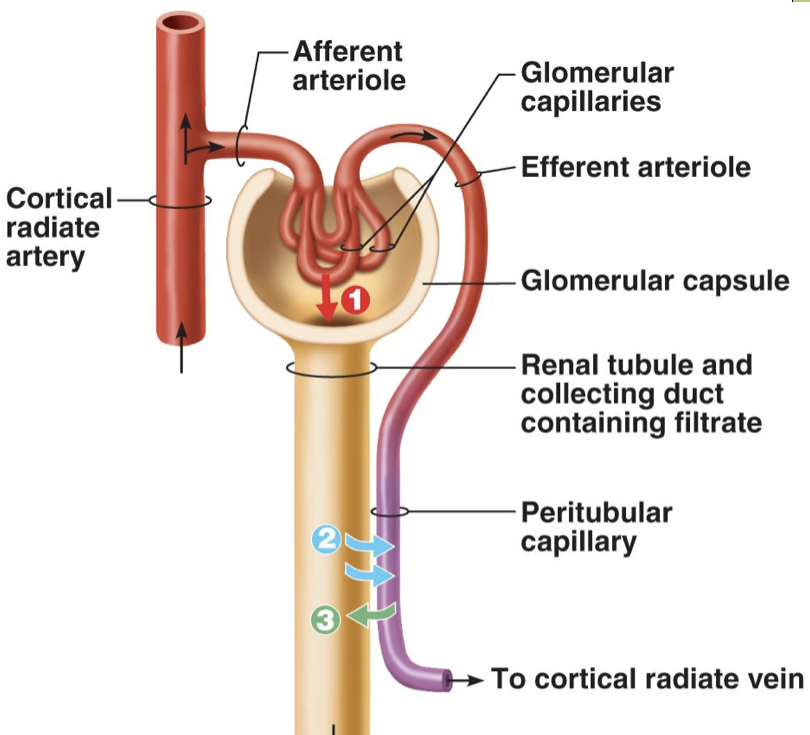
Afferent arterioles
enter glomerular capsule and form a capillary bed called a glomerulus
blood leaves glomerulus in efferent arteriole vessels then forms peritubular capillaries and (sometimes) vasa recta
Vein blood flow through kidneys
particular capillaries converge to form:
cortical radiate veins, arcuate veins, interlobar veins, renal vein
NO segmental veins
arcuate arteries and veins form boundary b/w cortex and medulla in kidneys
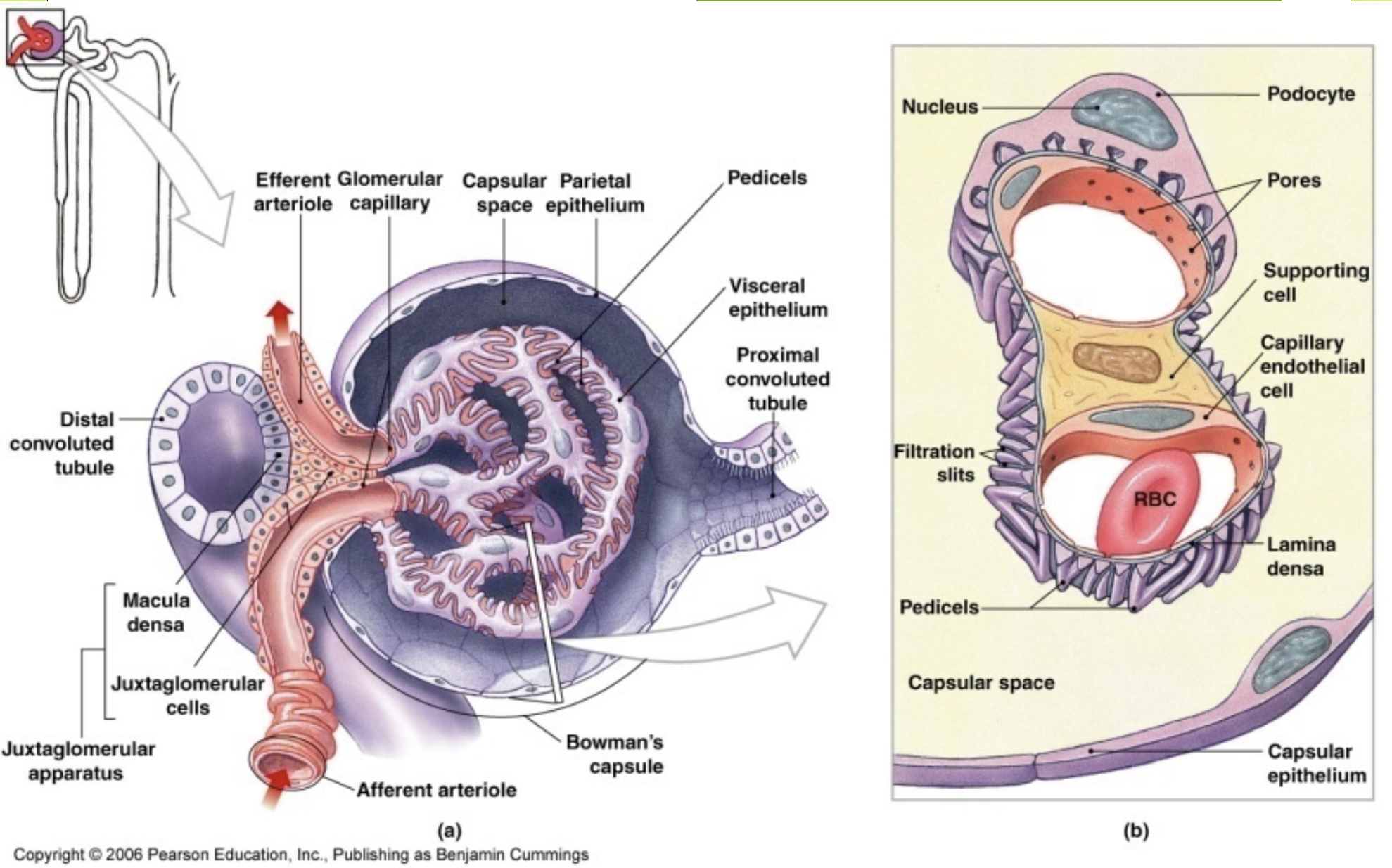
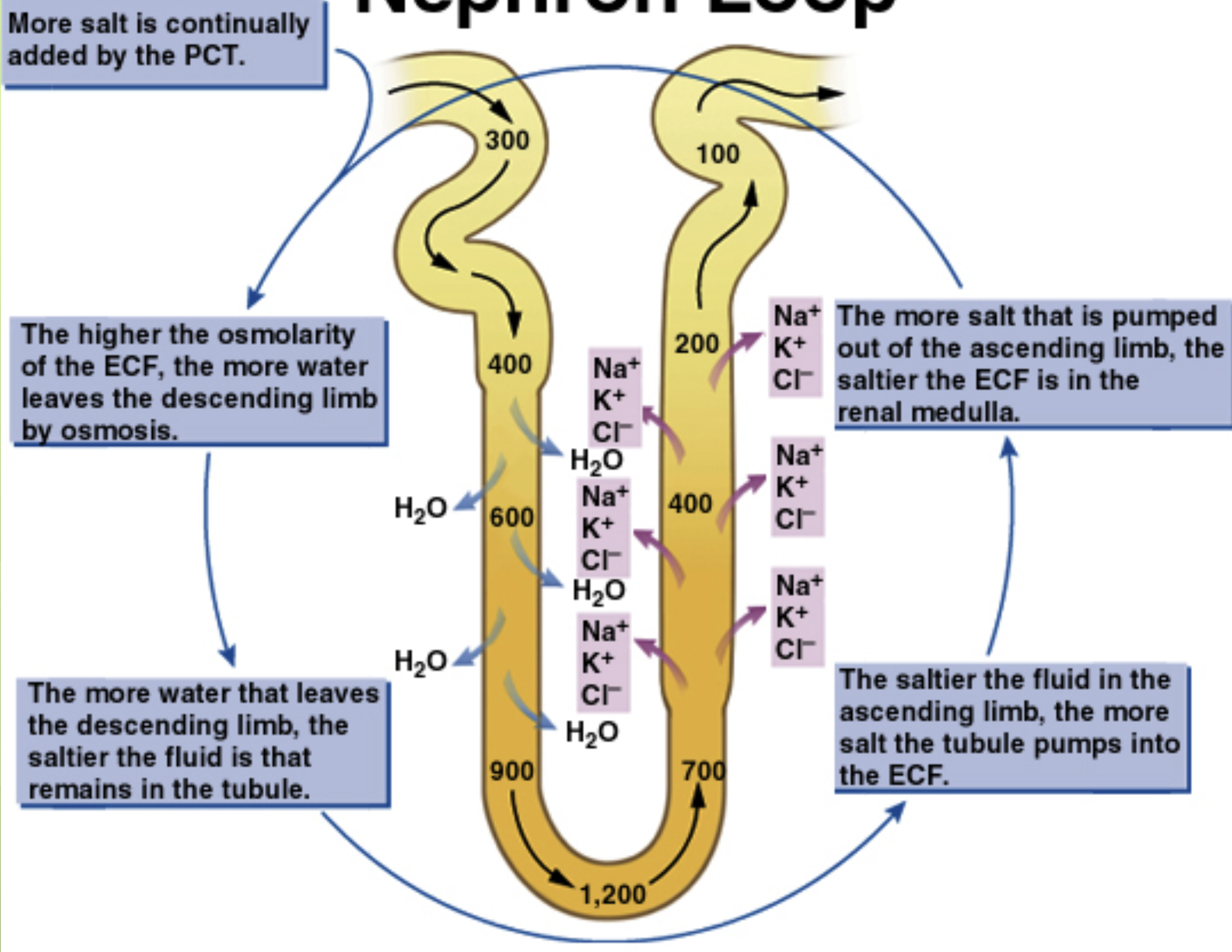
Renal Corpuscle
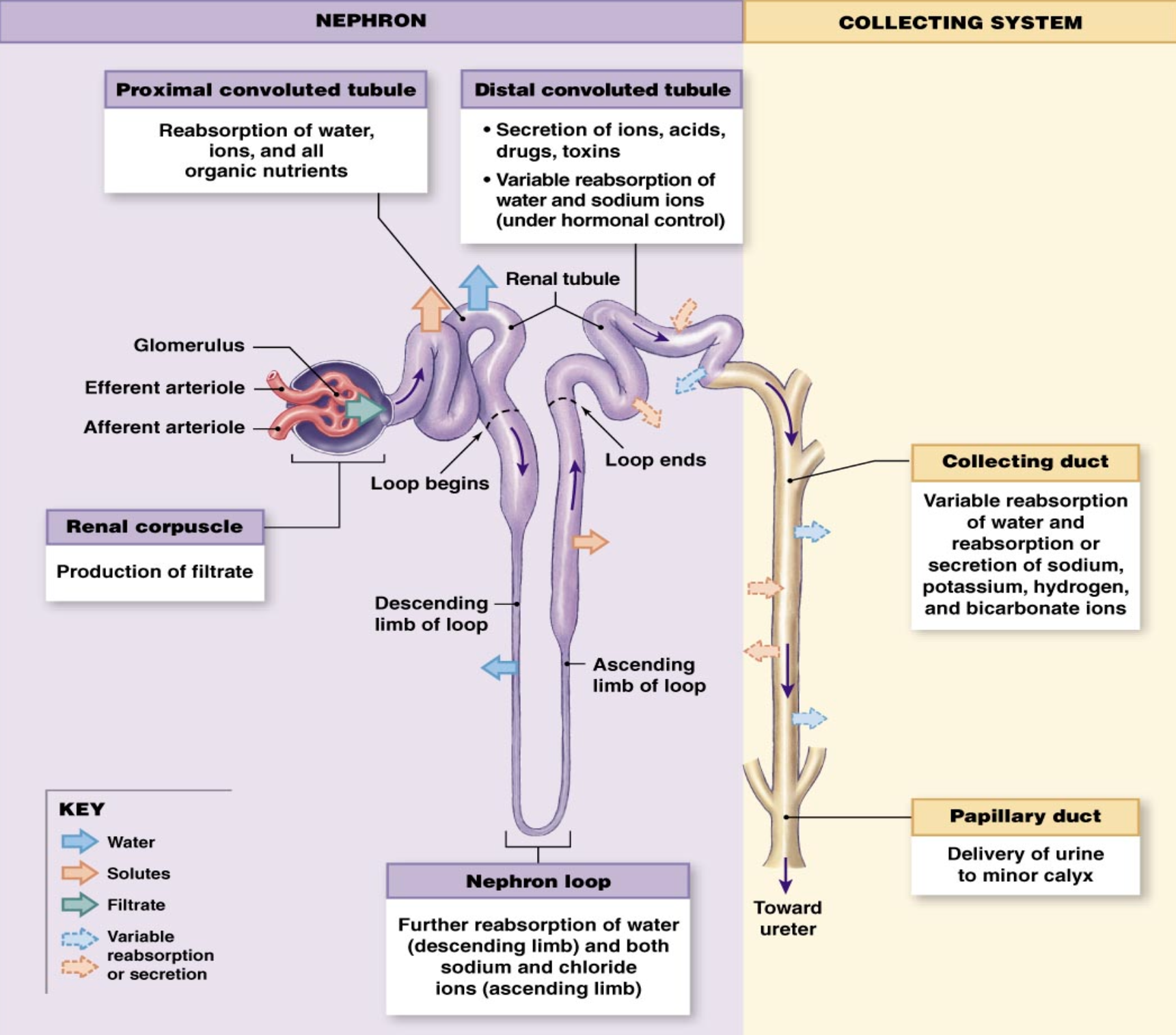
The Nephron? Made up of?
basic functional unit of kidneys
where blood is filtered and the fluid removed is concentrated into urine to almost urine
Made up of:
renal corpuscle- glomerulus and glomerular capsule
PCT- proximal convoluted tubule
nephron loop
DCT- distal convoluted tubule
The Nephron
2 types of nephrons
cortical nephron (85%)
juxtamedullary nephron
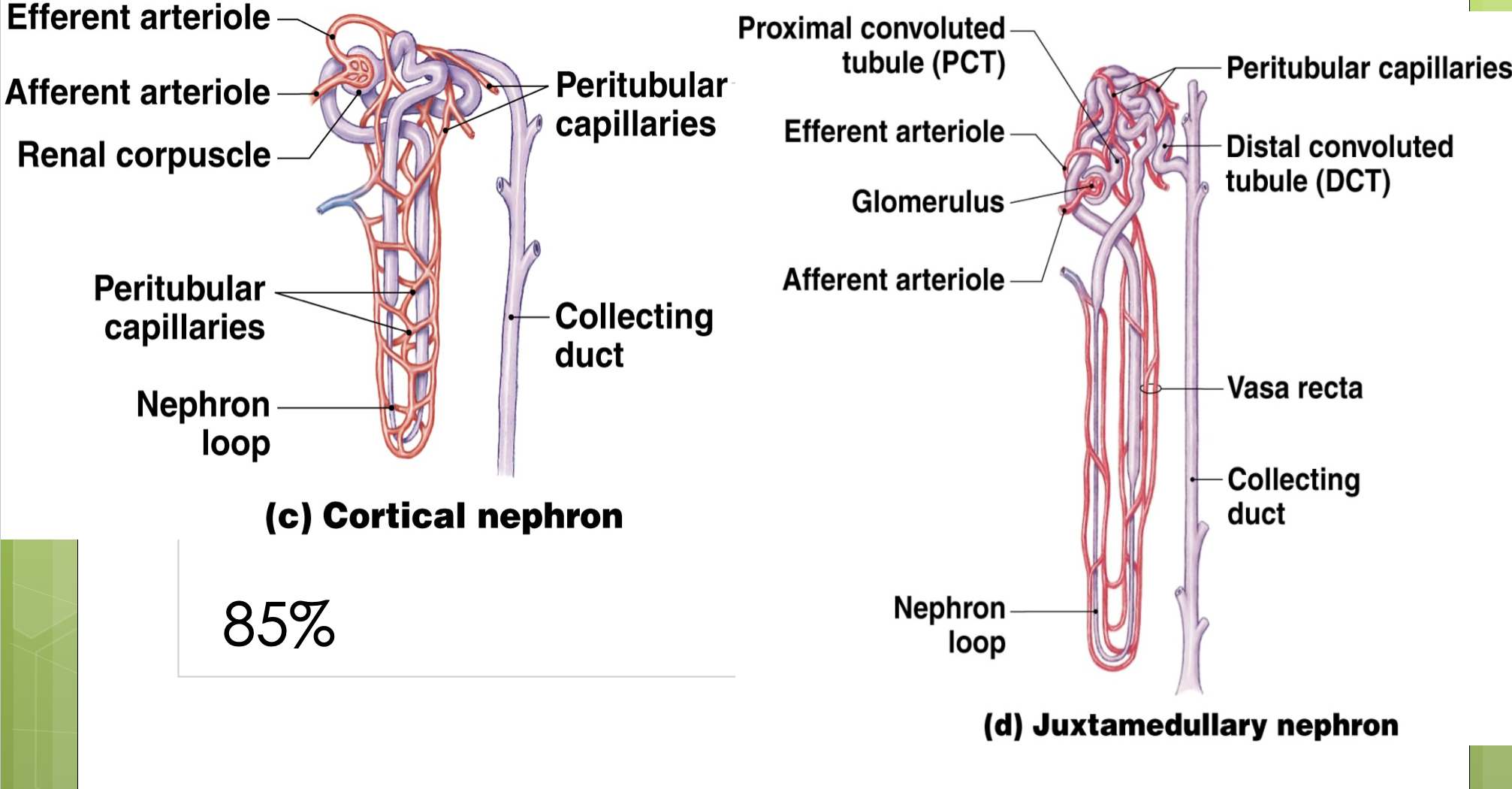
What are Juxtamedullary Nephrons?
have long nephron loops
reach far into renal medulla where solute concentration is high in peritubular fluid
these nephrons are important in concentrating our urine
Urine formation (7 steps)
blood enters “leaky” glomerulus
fluid and some solutes leave blood
filtrate is caught by glomerular capsule and enters PCT
as filtrate flows through PCT, Tehran loop and DCT, water and some solutes are reabsorbed back into blood. some substances are secreted into nephron
filtrate flows into collected duct - some final changes occur
by the time filtrate leaves collecting duct, it can be called urine
urine passes through papilla into minor calyx to major calyx to renal pelvis to ureter to urinary bladder
What is being filtered out?
metabolic waste products/nitrogenous wastes
urea- AA breakdown
creatinine- muscle contraction/creatine phosphate breakdown
uric acid- DNA/RNA breakdown
ammonia- AA breakdown
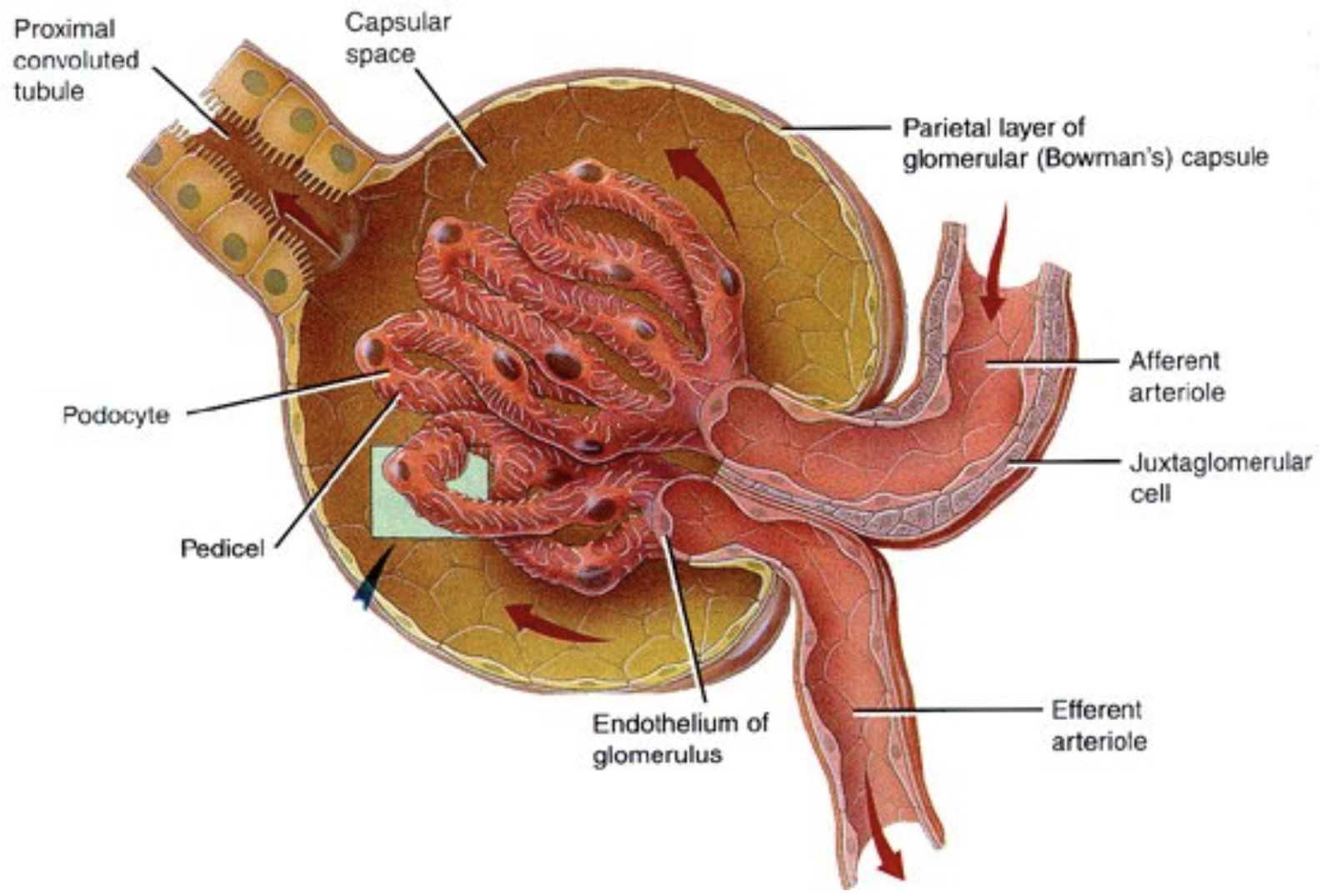
Renal Corpuscle Structure
glomerular capillaries
glomerular capsule
podocytes
mesangial cells
Glomerular capillaries
single layer of endothelial cells plus basement membrane (dense layer)
Glomerular Capsule
made up of simple squamous epithelium (capsular epithelium)
capsular space separates capillaries from glomerular capsule
Podocytes
cells that wrap around glomerular capillaries
Mesangial Cells
cells that lie between capillaries and help regulate capillary blood flow
Renal Corpuscle - The Filtration Membrane
glomerular capillaries
dense layer
filtration slits in podocytes
Only small solutes get through to enter capsular space and PCT
What 3 forces are at work in the renal corpuscle?
Glomerular Hydrostatic Pressure (GHP)
blood pressure in glomerular capillaries
Capsular Hydrostatic Pressure (CsHP)
pressure of filtrate in capsular space
Blood Colloid Osmotic Pressure (BCOP)
force of solutes in blood that draws water back into glomerular capillaries
Where is GHP high? Why? CsHP?
GHP is higher in glomerular capillaries than other capillary beds - 50mm HG vs 35 mm Hg
bc the efferent arteriole is smaller in diameter than afferent arteriole
CsHP is about 15mm HG
this pressure of filtrate being pushed into PCT
Opposes GHP
How do you calculate Net Hydrostatic Pressure (NHP)?
CsHP - GHP = NHP
How to calculate Net Filtration Pressure (NFP_
NHP - BCOP = NFP
How many liters of filtrate do kidneys produce a day? What % is reabsorbed? How much urine is produced in 24 hours?
180 Liters of filtrate per day
99% is reabsorbed by nephron and collecting ducts
1.8 L of urine per 24 hours
What is Glomerular Filtration Rate (GFR)?
the amount of filtrate the kidneys produce in one minute (approx. 125 mL/min)
What does rate of filtration depend on? What does an increase and decrease in pressure do?
depends on BP entering glomerulus
Increase= increased filtrate
decrease= decreased filtrate
What would happen to filtration if there was a small drop in pressure? Why is this bad?
small drop in pressure would eliminate filtration
with our filtration we lose ability to eliminate wastes and maintain pH and blood volumes
Regulation of GFR
auto regulation
accomplished by myogenic mechanisms
a drop in systemic BP= contraction of efferent arteriole
a rise in systemic BP = constriction of afferent arteriole
What hormones regulate GFR?
renin-angiotensin system
natriuretic peptides
Renin-angiotensin system
renin secretion from juxtaglomerular complex
drop in BP
nervous stimulation
decline in osmotic concentration of filtrate in DCT
Natriuretic peptides
secreted by heart in response to high blood volume
causes vasodilation of afferent arterioles
causes vasoconstriction of efferent arterioles
causes a decrease in Na+ (and water) reabsorption at nephron
What is Juxtaglomerular Complex made up of?
made up of cells of the macula dense and juxtaglomerular cells
What does the macula dense do? What do the juxtaglomerular cells do?
macula densa= stimulate juxtaglomerular cells in response to a drop in Na+ levels in filtrate
juxtaglomerular cells= secrete renin in response to a decline in BP in afferent arteriole, nervous stimulation, or when stimulated by cells of macula dense
What do renin release do?
renin release concerts angiotensinogen to angiotensin I
Angiotensin I
is cleaved into angiotensin II in the lungs by the enzyme angiotensin converting enzyme (ACE)
Angiotensin II
causes constriction of efferent arteriole, aldosterone release, thirst, ADH release, increase heart rate and vasoconstriction in periphery
Erythropoietin
released by the juxtaglomerular complex
released in response to low blood O2 levels
stimulates red bone marrow to increase RBC production
Autonomic Regulation
regulates GFR
sympathetic nervous system stimulation causes vasoconstriction in afferent arteriole
this decreases GFR and filtrate production during sympathetic activation
during fight or flight response
during strenuous exercise
Reabsorption
certain substance are reabsorbed (remove) from the filtrate into the interstitial fluid of kidneys
Secretion
certain substances are added to the filtrate from the interstitial fluid of the kidneys
Where is filtrate? What is peritubular fluid?
filtrate is contained in the nephron
peritubular fluid is the extracellular fluid outside the nephorn
peritubular fluid contents are taken up by peritubular capillaries and vasa recta
Peritubular Fluid Concentration
has vastly differing solute concentrations depending on where in the renal medulla you look
near cortex= 300mOsm/L, deep in medulla= 1200mOsm/L
Proximal Convoluted Tubule (PCT), What is reabsorbed? What is filtered?
cells forming wall of PCT have microvilli to increase surface area
filtrate here is similar to plasma without proteins
the PCT reabsorbs 60-70% of filtrate produced
reabsorption of glucose, AAs, ions
reabsorption of water by osmosis
secretion of H+
all reabsorption into peritubular fluid
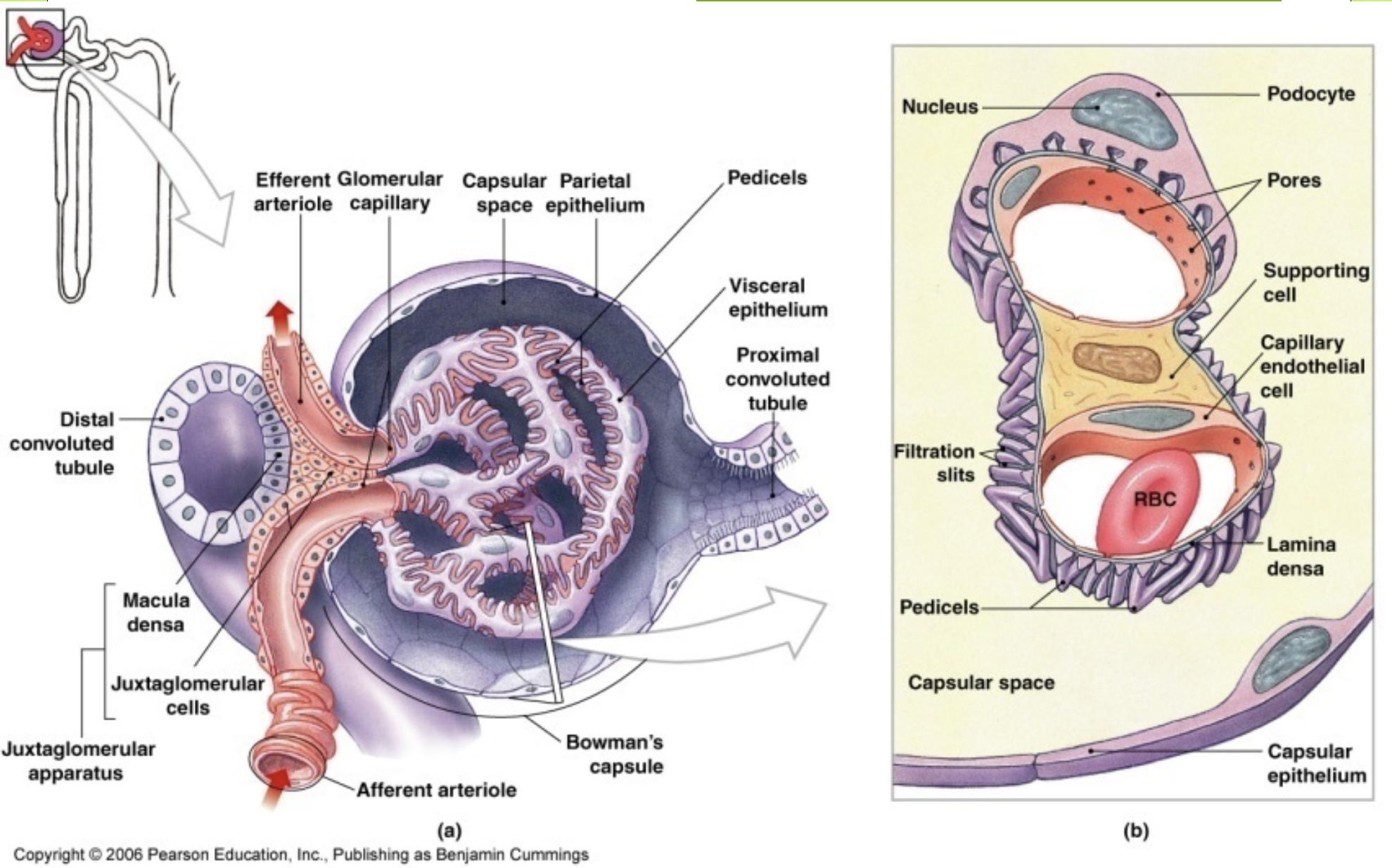
Nephron Loop (Loop of Henle)
the “loop” reabsorbs 50% of water that is left in filtrate and 66% of Na+ and Cl-
Descending limb and ascending limb have differing permeabilities
(thin) descending limb is permeable to water, but not silutes
(thick) ascending limb is not permeable to water or solutes, but has active transport mechanisms for removal of Na+ and Cl- from filtrate
Ascending Limb (thick)
cells of thick ascending limb actively transport Na+, K+ and Cl- out of filtrate into cell at apical surface
cells then actively transport Cl- and K+ out basal surface into peritubular fluid
cells then also use Na+/K+ ATPase pump to return K+ into cells and pump Na+ out into peritubular fluid
K+ then diffuses back into filtrate through passive channels
Different permeabilities of descending vs. ascending limbs
helps create osmotic gradient in medulla
facilitates reabsorption of water and solutes
Countercurrent Multiplication
between ascending and descending limbs of loop
permits passive reabsorption of water from tubular fluid
picture drawn in notebook
Countercurrent Multiplication
Distal Convoluted Tubule
15-20% of original filtrate reaches DCT
Reabsorption of Na+ and Cl- through active transport
reabsorption of water
secretes K+ and H+ from peritubular fluid into filtrate
What control is DCT reabsorption under?
under hormonal control
aldosterone increases Na+ reabsorption
ADH increases water reabsorption
effects of aldosterone and ADH are opposed by natriuretic peptides
Collecting Duct (what is reabsorbed?)
reabsorption also regulated by ADH and aldosterone
aldosterone- more Na+ reabsoprtion
ADH- more water reabosprtion
both opposed by natriuretic peptides
Reaborbs HCO3- and H+
urea is also reabsorbed
Anti-diuretic Hormone
The DCT and collecting duct are impermeable to water except in the presence of ADH
stimulates water channels to be produced and embedded in the apical surface of the DCT and collecting duct cells
water is then reabsorbed into peritubular fluid
facultative water reabsorption
this mechanism reabsorbs about 26L per day
diabetes insipidus
Peritubular capillaries and Vasa recta
take up peritubular fluid and carry away both water and solutes and returns them to the circulation
Normal Urine
clear/light yellow
sterile (no bacteria)
volume: 700mL - 2000mL per day
pH= 6.0
protein= none (unless after intense workout for short period)
blood= none (unless after intense workout for short period)
glucose= none (unless w/ diabetes mellitus)
Ureters
muscular tubes that extend from the kidneys to the urinary bladder
peristaltic contractions occur about every 30 seconds to move urine along toward bladder
3 tissue layers of Ureters
inner transitional epithelium
middle smooth muscle layer
superficial connective tissue
Urinary Bladder
located w/in pelvic cavity - posterior to pubic symphysis
“boat-shaped”
Where do ureters enter bladder? Urethra?
ureters enter bladder on posterior/inferior portion
urethra exits bladder inferior to ureter openings
urinary trigone
4 tissue layers of urinary bladder
inner transitional epithelium (mucosa)
submucosa
muscular layer (detrusor muscle)
superficial connective tissue layer
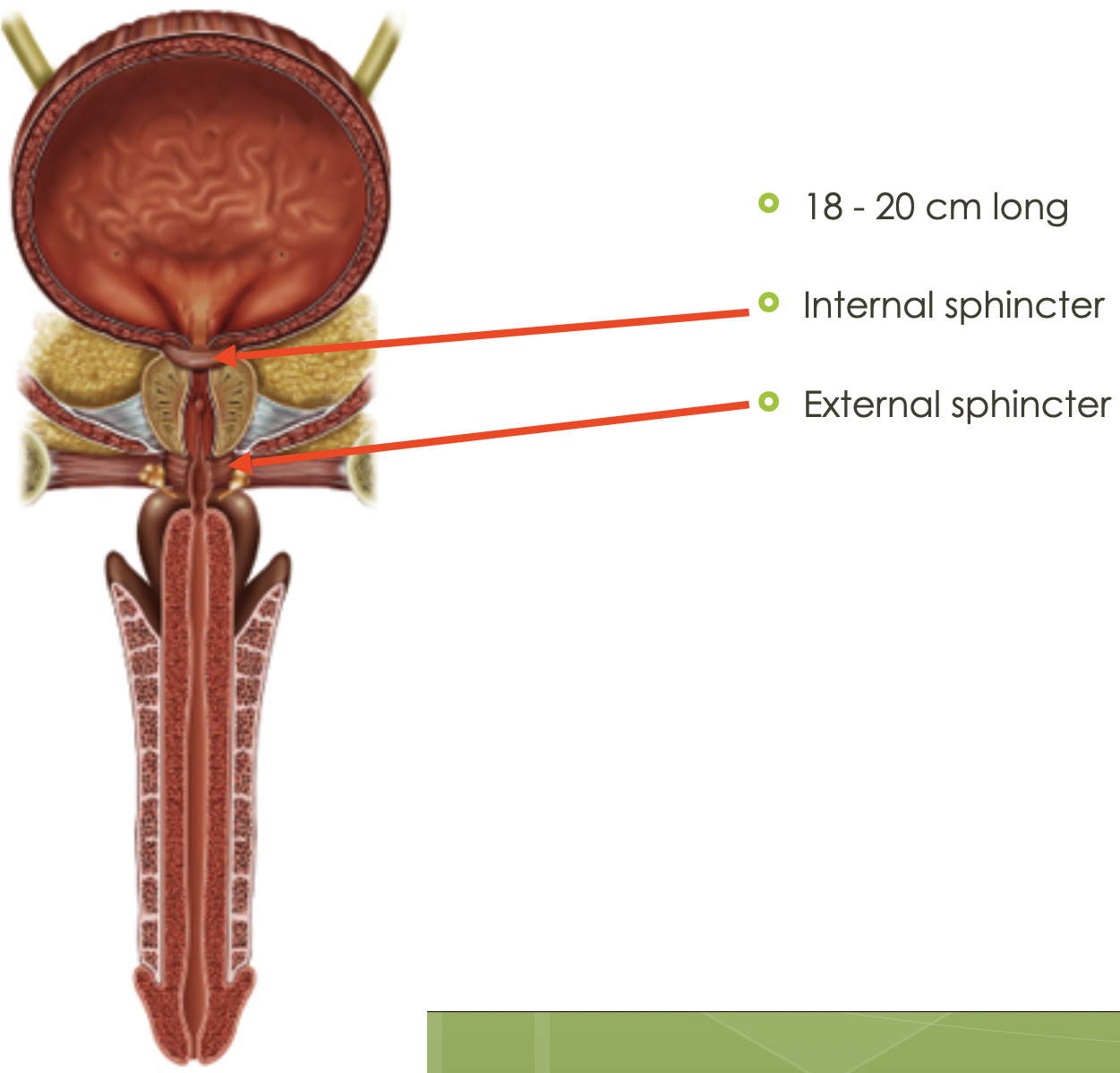
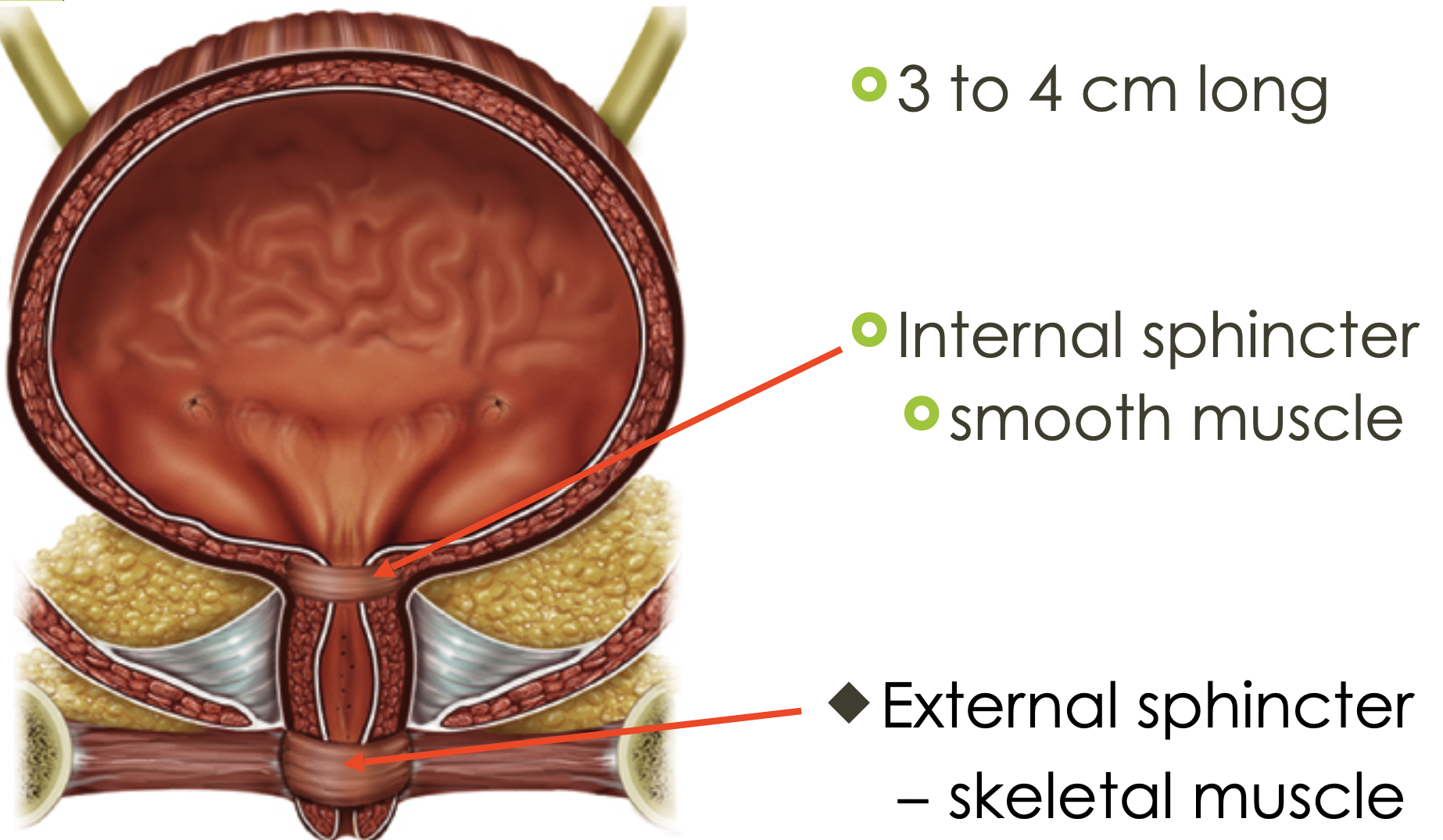
Urethra (What is it? what does it do? how long?)
tubular structure that extends from urinary bladder to exterior
transports urge from bladder to exterior
tissue lining urethra varies from transitional epithelium near bladder to stratified squamous epithelium near external environment
18-20cm long in males and 3-5cm long in females
What is where the urethra exits the bladder?
a circular band of of smooth muscle called
where urethra passes through pelvic floor musculature, there is a circular band of skeletal muscle called: external urethral sphincter
provide voluntary control over discharge of urine
Male Bladder and Urethra
Female Bladder and Urethra
Voiding/Urination
stretch receptors in the wall of the urinary bladder are bladder are stimulated
neuron signals are sent through pelvic nerves into spinal cord where motor neurons controlling the detrusor muscle are stimulated
urination involves conscious relaxation of external urethral sphincter, which causes relaxation of internal urethral sphincter
Incontinence
inability to control urination
damage to urethral sphincters
damage to pelvic nerves
damage to central nervous system
UTI
bacterial infection of urinary bladder (lower UTI) OR bladder and ureters and renal pelvis (upper UTI)
prevention through hydration and proper hygiene (front to back)
more common in females
symptoms
frequency (feel like you have to go to the bathroom all the time), pain with urination, flank pain, fever
Kidney Stones
mineral deposits that form in urine in the kidneys
painful as they pass through ureters
calcium oxalate (80%)
prevention through hydration, cannot form in dilute urine