Rehabilitation Robotics
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
57 Terms
Major factors causing disabilities world-wide
Neonatal Nutrition >> Premature Births >> Cerebral Palsy, Autism, Down Syndrome, etc.
High Blood Pressure >> Strokes
HIV >> Dementia, Strokes
COVID-19 >> Chronic fatigue, Cognitive Impairment
Therapy Robots
Treat neurological disorders such as stroke and cerebral palsy
Function to automate and deliver autonomous or semi-autonomous therapy for the arm (or leg or joint)
Function to assess the level of disability and impairment remaining in a limb, arm, or leg
Outcome >>> reducing motor impairment, increasing function, and driving brain re-organization
Typically function in clinics or supervised settings

Assistive Robots = Service Robots in Rehabilitation/Medical Settings
Replace other functions or activities, or things (e.g., surveillance robots)
Replace a lost limb (e.g., prosthetics)
Replace the function of a paralyzed limb and do tasks instead of the limb (e.g., a wheelchair robot)

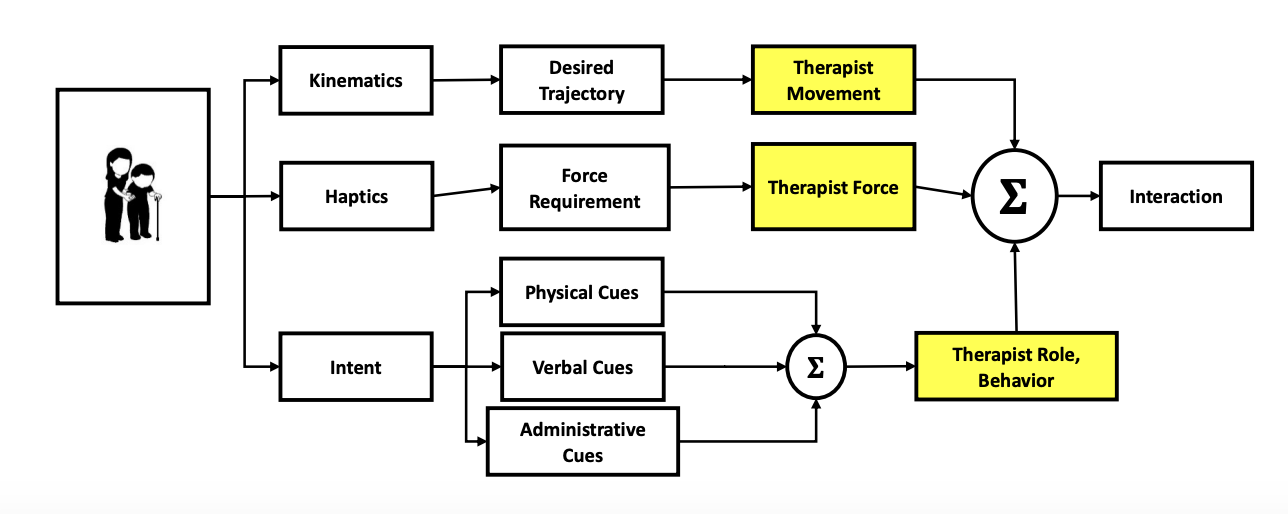
Observing Human-Human
patients w/ therapists
study of therapist movement gives us info on
—> how we model the kinematics of those movements
—> how we develop desired trajectories
look at the forces of interaction that therapists exert on their patients
—> how much force should the robot exert?
look at the therapist's role and behavior
—> understand the physical cues, verbal cues, and administrative cues they are using
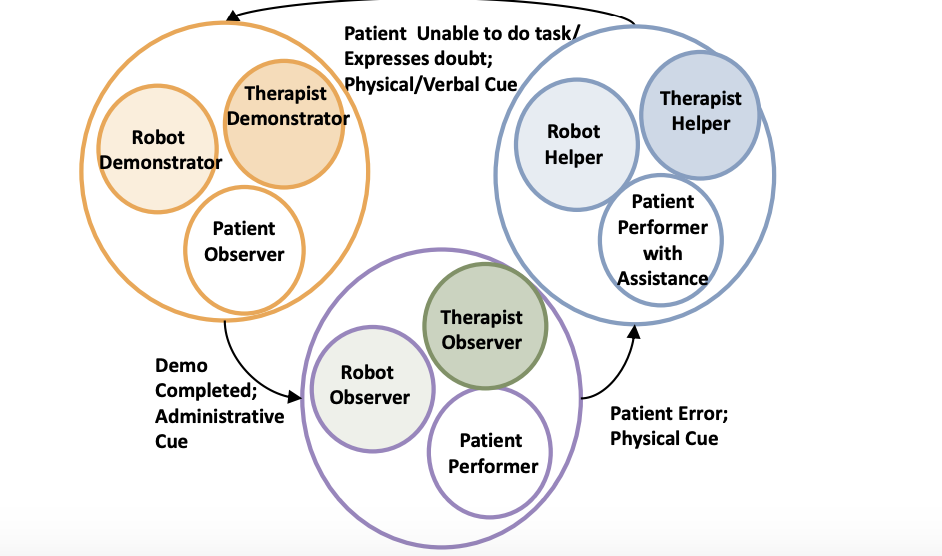
Capturing Roles and Cues
encode therapist activity to understand what behavior, rules, and scenarios we might see in a typical therapy session between the therapist and the patient
Multimedia Video Analysis Software: MVTA
8 Videos Coded independently by 2 therapists
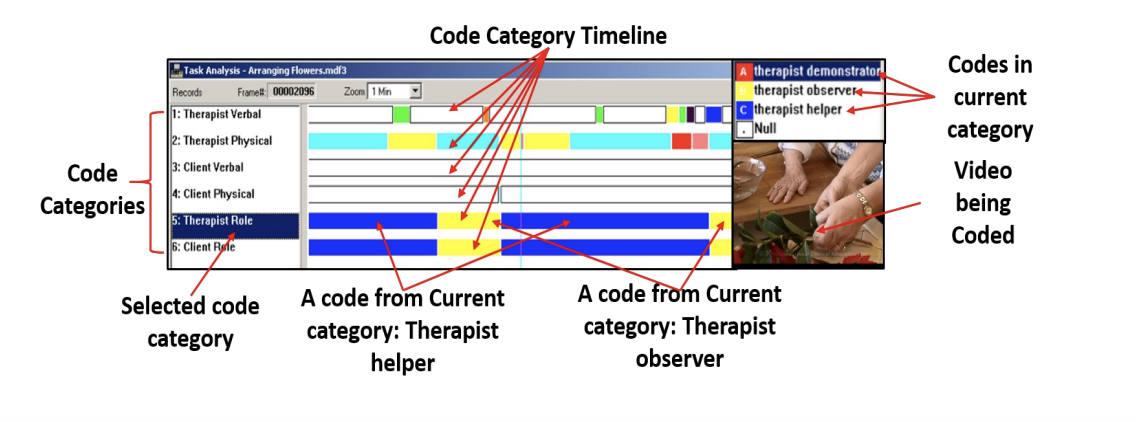
Patient-Therapist Dyads
therapist took on 3 behaviors
demonstrators (while the patient observed the action)
observer (while the patient becomes the performer)
helper (patient is performing, but now with the therapist’s assistance)
at the patient’s request/or if they observe something
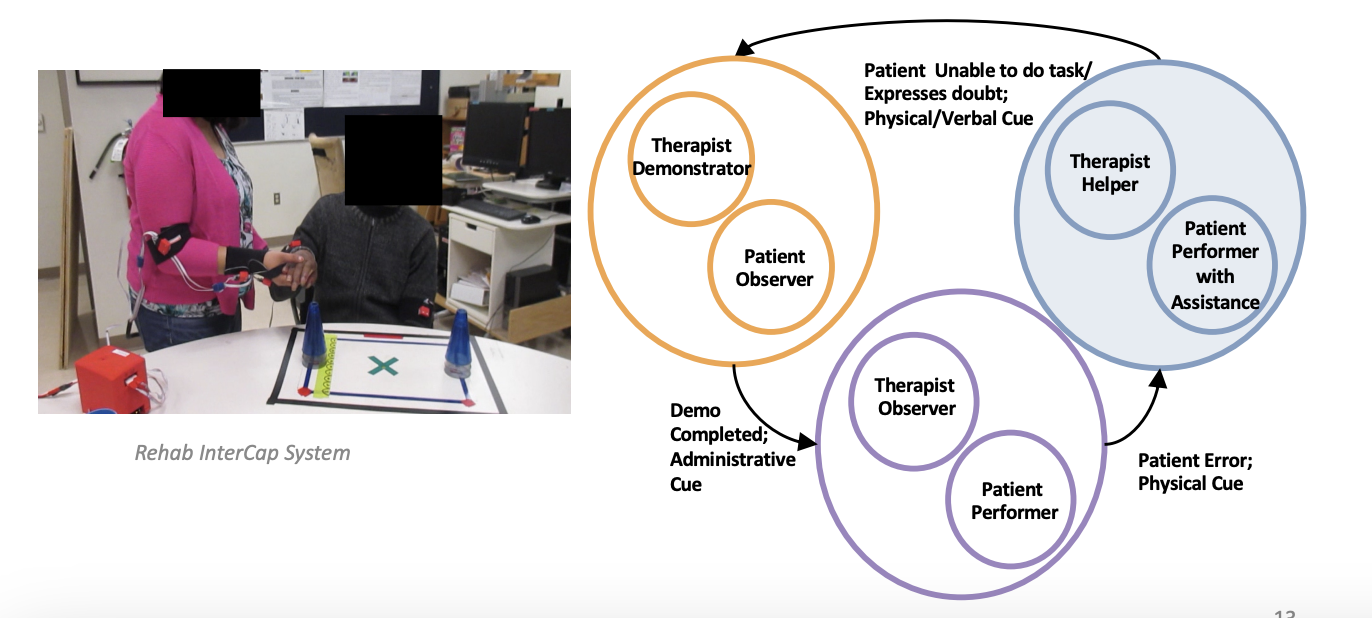
Therapist >> Robot
Ideally, the robot should take on three roles as demonstrator, observer, and helper, and co-act with the patient
Helper role is often seen in hands-on effector THERAPY ROBOTS (e.g., ADLER, Theradrive)
Demonstrator and Observer Roles are often found in ASSISTIVE ROBOTS or SERVICE ROBOTS (e.g., Nao)
i.e., look at patients performing tasks —> provide feedback —> monitor
Fluid transitioning from contact to non-contact with a patient is not often done due to huge safety concerns about soft and hard impacts


Helper role example
permanently attached to the person

TeleMonitoring/TeleTherapy: Rehabilitation Tasks
two rehabilitation tasks:
magazine stacking
and free movement of the stroke-affected limb
example of a robot that is in the social role of observing
patient is wearing a sensor
robot’s role is to
observe/monitor the patient to see if they are complying with the task and
get information about the level of impairment as they move on
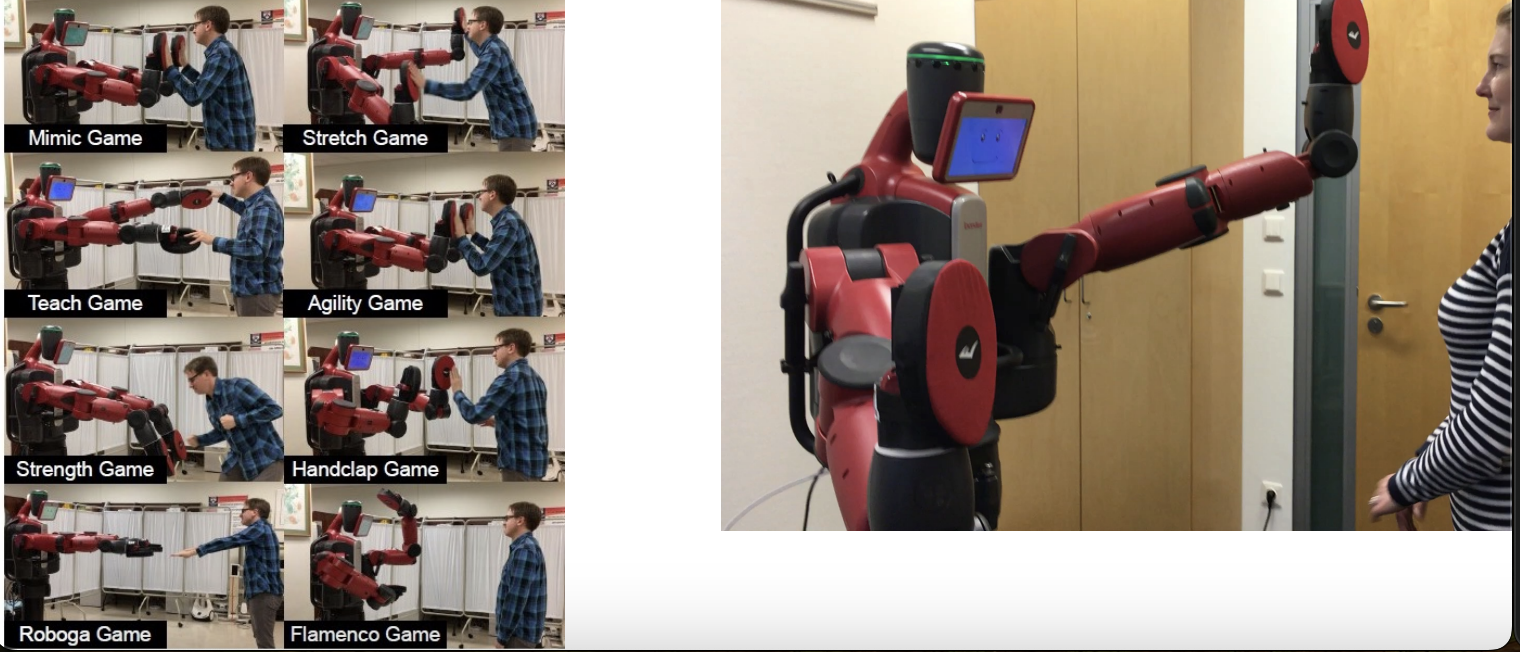
Baxter: Elder Exercise
Demonstrator/Observer roles >>
using camera systems and sensora
as the robot tries to get the person to interact with it, it can know whether the person interacted or not
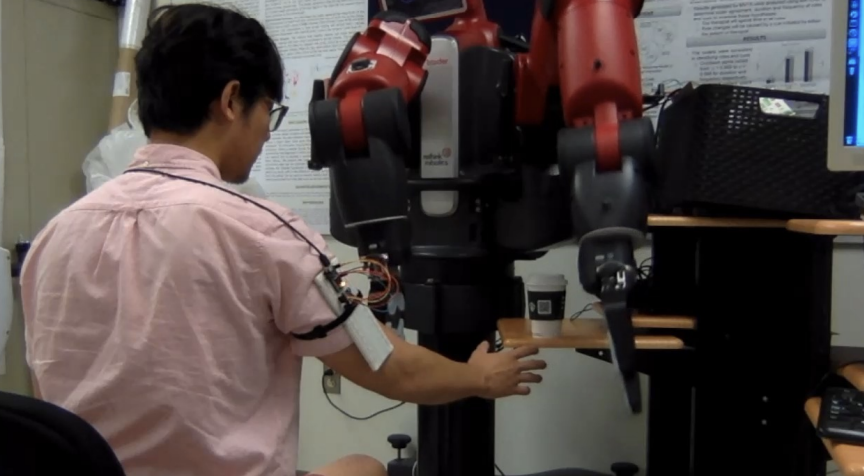
BAXTER: Therapy Assistant
Observer/Helper roles >>
sensory on the patient’s arm
monitoring the velocity of the movement of the patient’s arm
if there is an indication that the person is not acting within some prescribed bounds, the robot will come in and act

social robot on top of a telepresence platform
Demonstrator/Observer role >>
camera allows the the robot to observe the actions of the patient that it’s interacting with —> social robot can demonstrate activities that the patient can then comply with
Goal: Robot shares control with the therapist
philosophy: robots, whether they’re a therapy robot or a social robot, should act together w/ the therapist
sharing of control
therapist should program the robot in an appropriate way for their patient
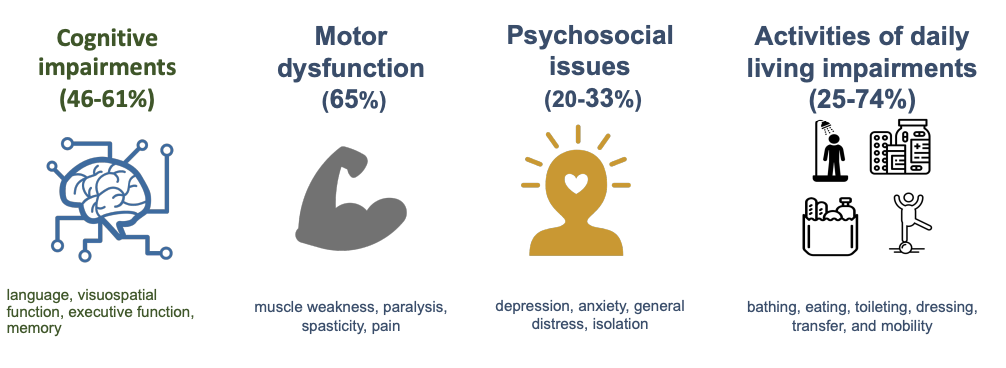
Long-term impairments persist after stroke
Cognitive impairments (46-61%)
language, visuospatial function, executive function, memory
Motor dysfunction (65%)
muscle weakness, paralysis, spasticity, pain
Psychosocial issues (20-33%)
depression, anxiety, general distress, isolation
Activities of daily living impairments (25-74%)
bathing, eating, toileting, dressing, transfer, and mobility
Upper Arm Impairment
Spasticity
Muscle Weakness
Impaired Interlimb and Intralimb Coordination
Reduced Joint Range of Motion
Impaired Posture
Increased Trunk Compensation
Inability to perform isolated arm movement
Flexor or Extensor Synergy
Upper Arm Stroke Rehabilitation
Practice Weight-Bearing
Practice Real Activities
Practice Moving Joints
Sensory Facilitation
Ex: Specific Techniques
Constraint Induced Therapy

Design Choices for RAT (Robot Assisted Therapy system)
figure out what these things should be; variables
what controls should you use?
how do you motivate a patient?
how do you customize it so that it’s different for individuals?
what type of feedback?
how will we make it learn?
what type of task?
==> must be useful in increasing engagement, allow for intense therapy, result in neuroplasticity, and carry over into the world
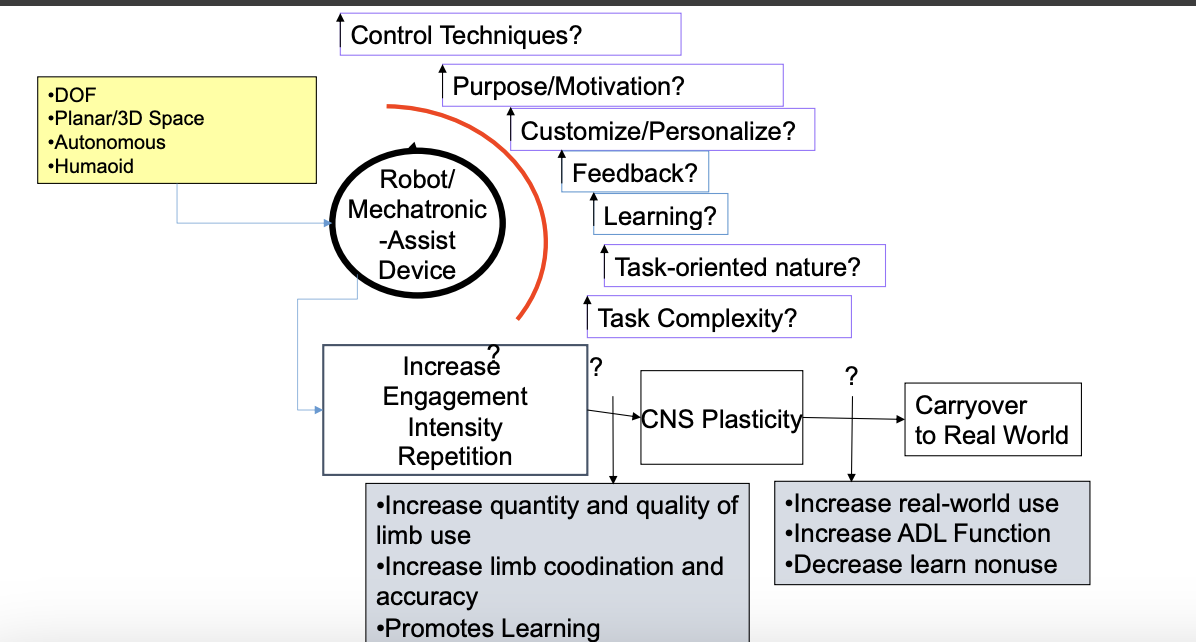
Mechanical Device and Sensors
Exoskeletons
End-effector
Single joint (e.g., only acting across the elbow)
Multiple joints (e.g., acting across the shoulder and the elbow)
Degrees of Freedom (i.e., the # of motors that they may have; the # of independent movements in the system that they may have)
Planar
3D
Pneumatic, etc.
(advantages to) Therapy Robots: Upper Limb
Automate traditional therapy treatments
Enable semi-autonomous training
once you program them, you can have them go
Provide consistent, repeatable, intensive training
can stress your patients a little bit more in terms of repetition; e.g., doing 1000 reps
Provide objective measures of recovery
quantitative ways of knowing that what you’re doing works

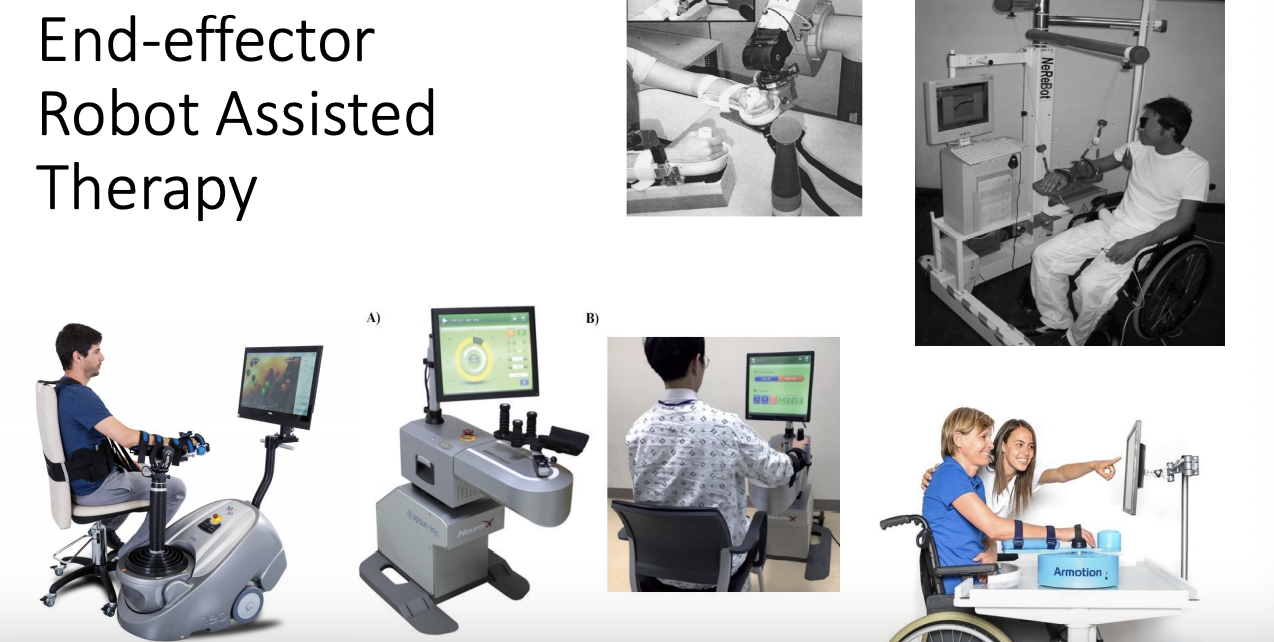
End-effector Robot Assisted Therapy
attached towards the forearm/wrist complex
can come in different configurations to support the UE (e.g., joystick)
usually connected to some type of gaming activity
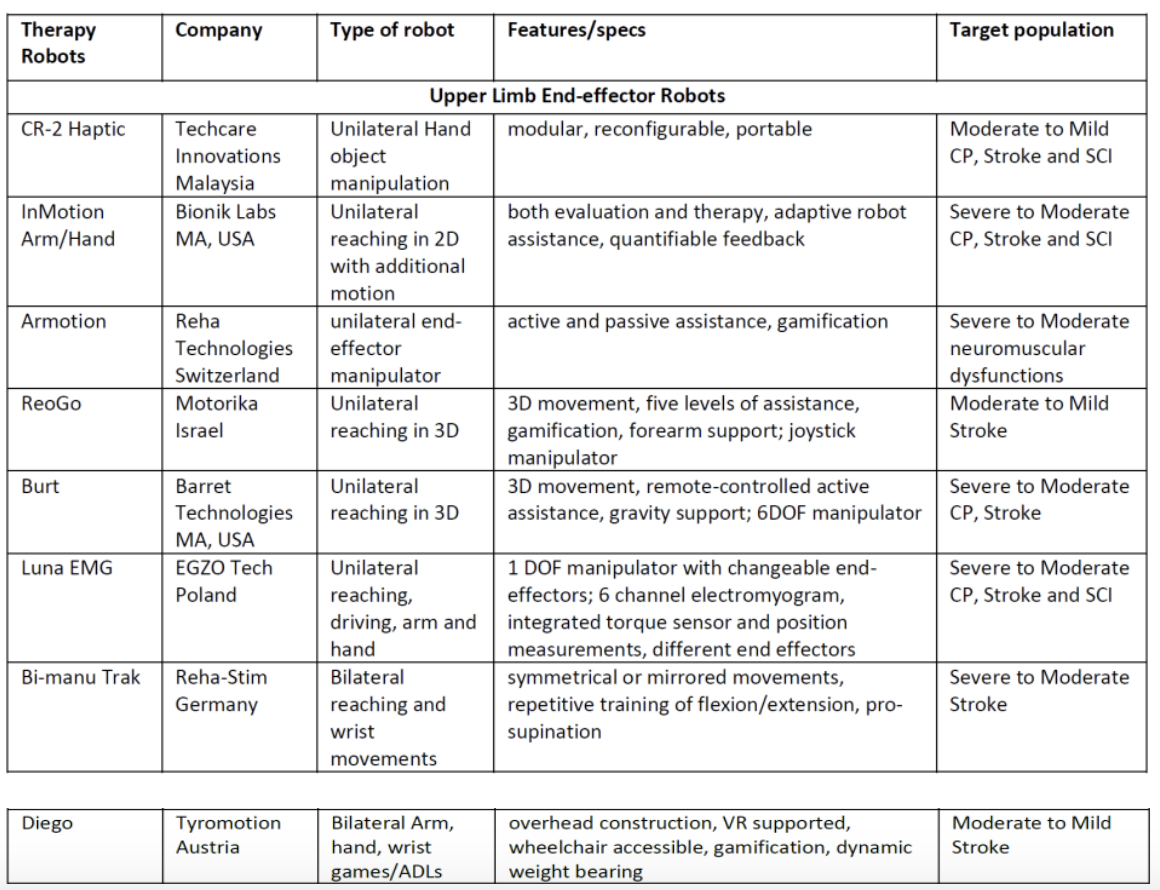
Example List of End-Effector Therapy Robots
Cost of these robots varies from $3K (CR-2 Haptic) to $275k (G-EO)
ExoskeletonsRobot Assisted Therapy
covering the upper arm in its entirety
often are not just attached to the wrist; also attached at the elbow
trying to move individual joints

Example list of some popular exoskeletons that exist that you can purchase out of the market
RUPERT IV
one of the earliest examples of exoskeletons; early designs were very heavy and bulky (but the premise of these were very encouraging)
Device encourages the retaining of the coordination of real-life activities
Three main links to support Shoulder, Elbow, and Wrist Movements Robot
RUPERT IV utilizes pneumatic McKibben artificial muscle actuators
The power supply and the control system are located in the backpack part of the robot
Myomo
less bulky exoskeletons that people can take home

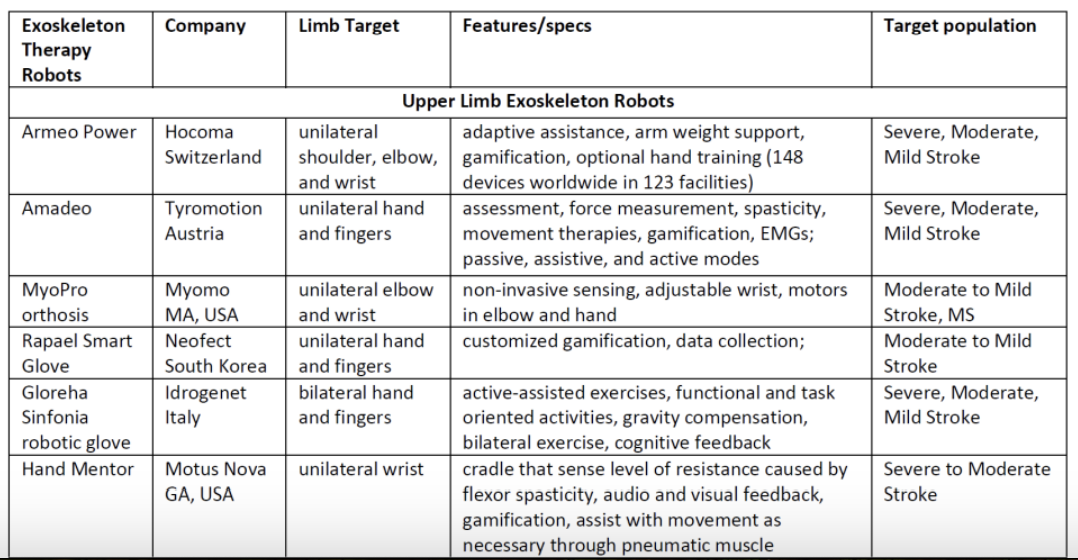
MIT-MANUS/InMotion
2D - HELPER ROBOT= designed to focus on exercise in the plane (mostly upper extremity- elbow/shoulder activities)
SCARA Manipulator
2 Degrees of Freedom (Planar robot)
Backdrivable
Low Inertia
you don’t feel a lot of resistance when you’re moving it
Reaching practice
Point-to-Point Tracking
Impedance Control
we can craft how it feels: the mass, the spring, the damping experience as you use the robot
gaming environment used to develop a training modality (a particular exercise)
as you move around the dashed lines, you are mainly exercising the elbow
as you move along the closer dashed lines, you are mainly exercising the shoulder
as you move along the solid lines, you are doing more inter-limb and coordinated type reaching
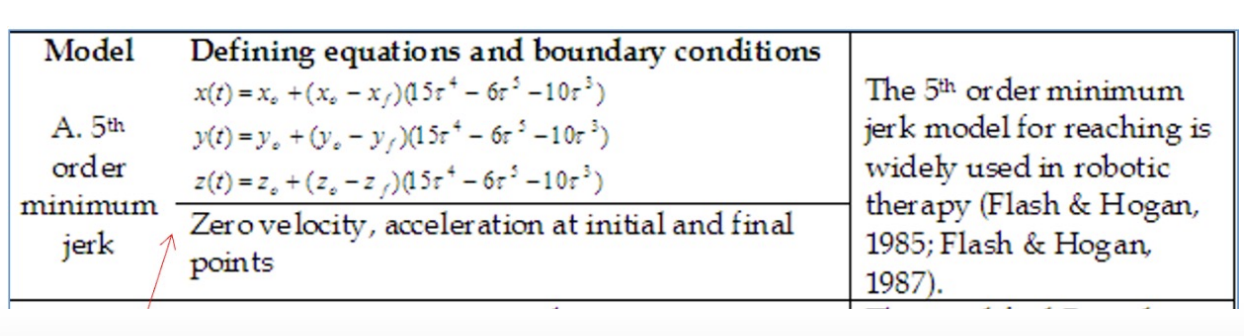
Minimum Jerk Model
model that allows us to command and create trajectories
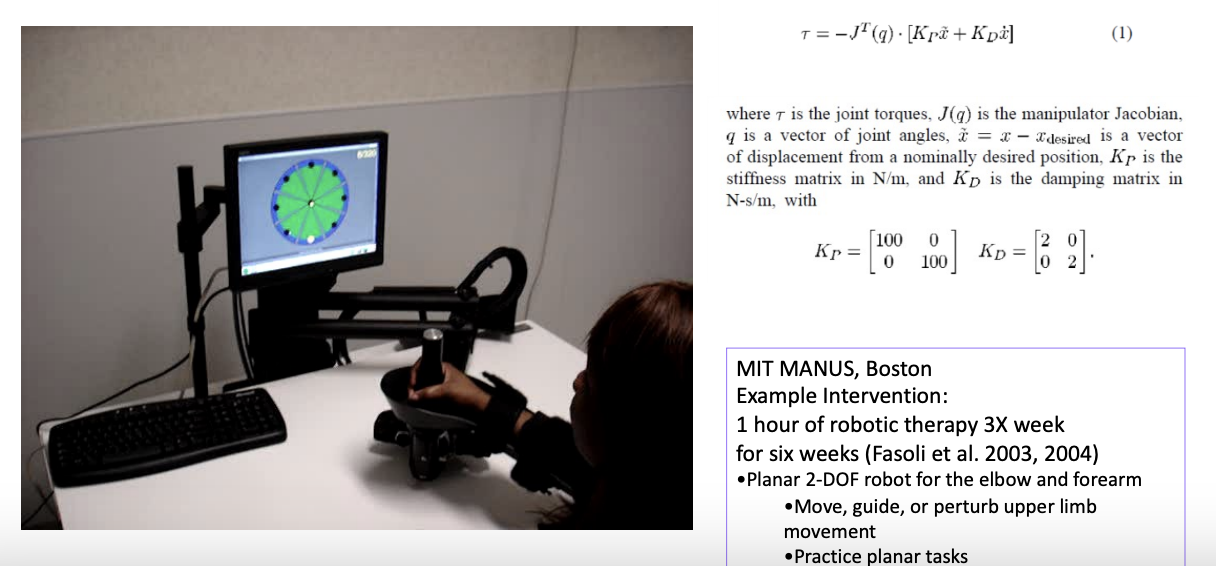
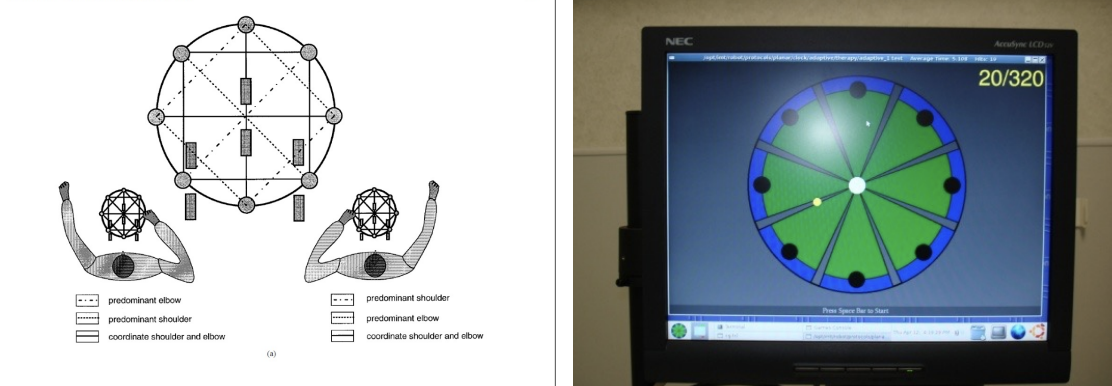
example of someone using the MIT MANUS (end-effector robot, as it is attached to the end-effector)
there is a target that is appearing on the screen
the person is asked to move to those targets
how do we control the experience at the robot?
controlling the stiffness and the damping experience at the robot
patient is severely impaired —> robot should be stronger and stiffer, so that the person is guided along the path
patient is a lot milder in terms of their presentation —> robot should give little help, so that the person is doing it themselves; or, provide resistance/increase damping, so that the person has a more challenging experience
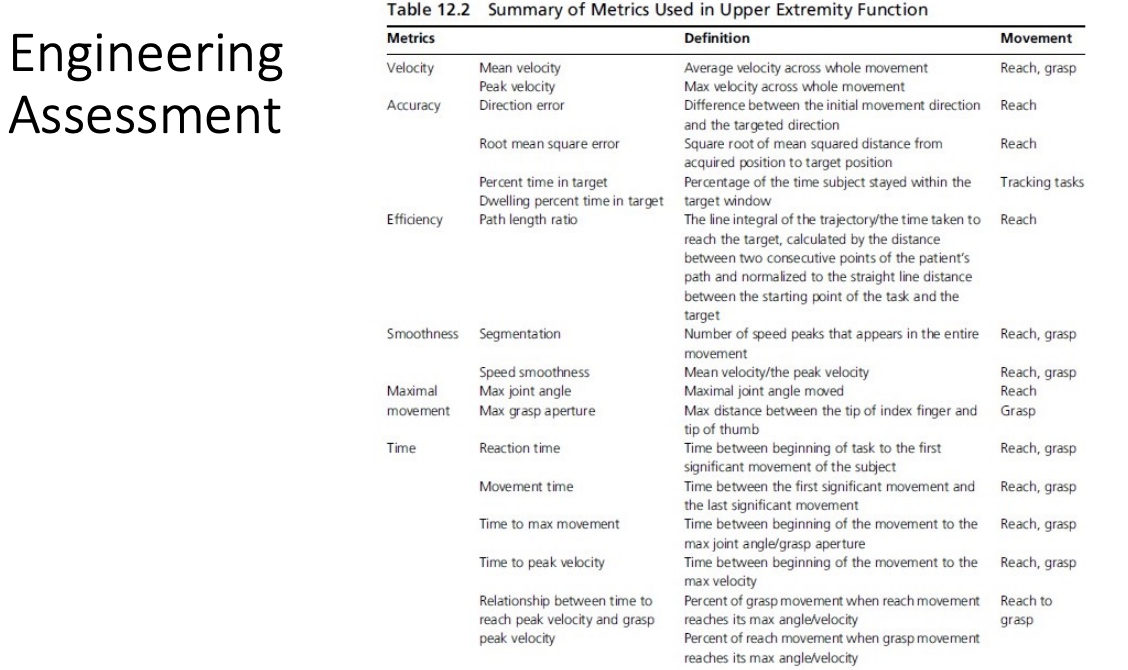
Examples of the measures that can be extracted from the actions that the patients are doing with the robot; can have quantitative info about…
velocity
acuracy
efficiency
smoothness
time
***these measures have been shown to be sensitive to reduction in impairment
InMotion Therapy Robot
designed to have 1 therapist set up the system and work with the patient; advantages:
can allow lots of repetition
therapist can wander off if they need to (e.g., to look at another patient)

Robot-Assisted Therapy (RAT) VA Clinical Trial Results
clinical trial that compared robot therapy to non-robot therapy in 2 ways: standard therapy and intensive therapy; looked at moderate-severe functioning stroke survivors with UE impairment
Robot Therapy:
36, 1-hour, high-intensity therapy with the In Motion robot (MIT-Manus paradigm with horizontal, vertical, wrist, and hand modules)
***findings: did not improve significantly more than non-robot control groups, BUT it got better as time goes on
***findings: cost of robot therapy was comparable to non-robot therapies, and the price is not too bad!
Non-Robot Therapy:
Standard Therapy and Intensive (same dosage)
Subjects:
Moderate to severe functioning stroke survivors with upper limb impairment for at least 6 months and with lesions due to single and multiple strokes
Robot therapy did not improve significantly more than non-robot control groups of usual care or intensive therapy, but had a modest improvement over 36 weeks
The cost of robot therapy was comparable to the non-robot therapies (12 weeks: $9,977 RT versus $8,269 Non RT, and 36 weeks: $15,562 RT versus $15,605 and $14,343 for non RT)
***could be good in environments that don’t have a lot of clinicians, but a lot of patients that need help; robots could help deliver therapy
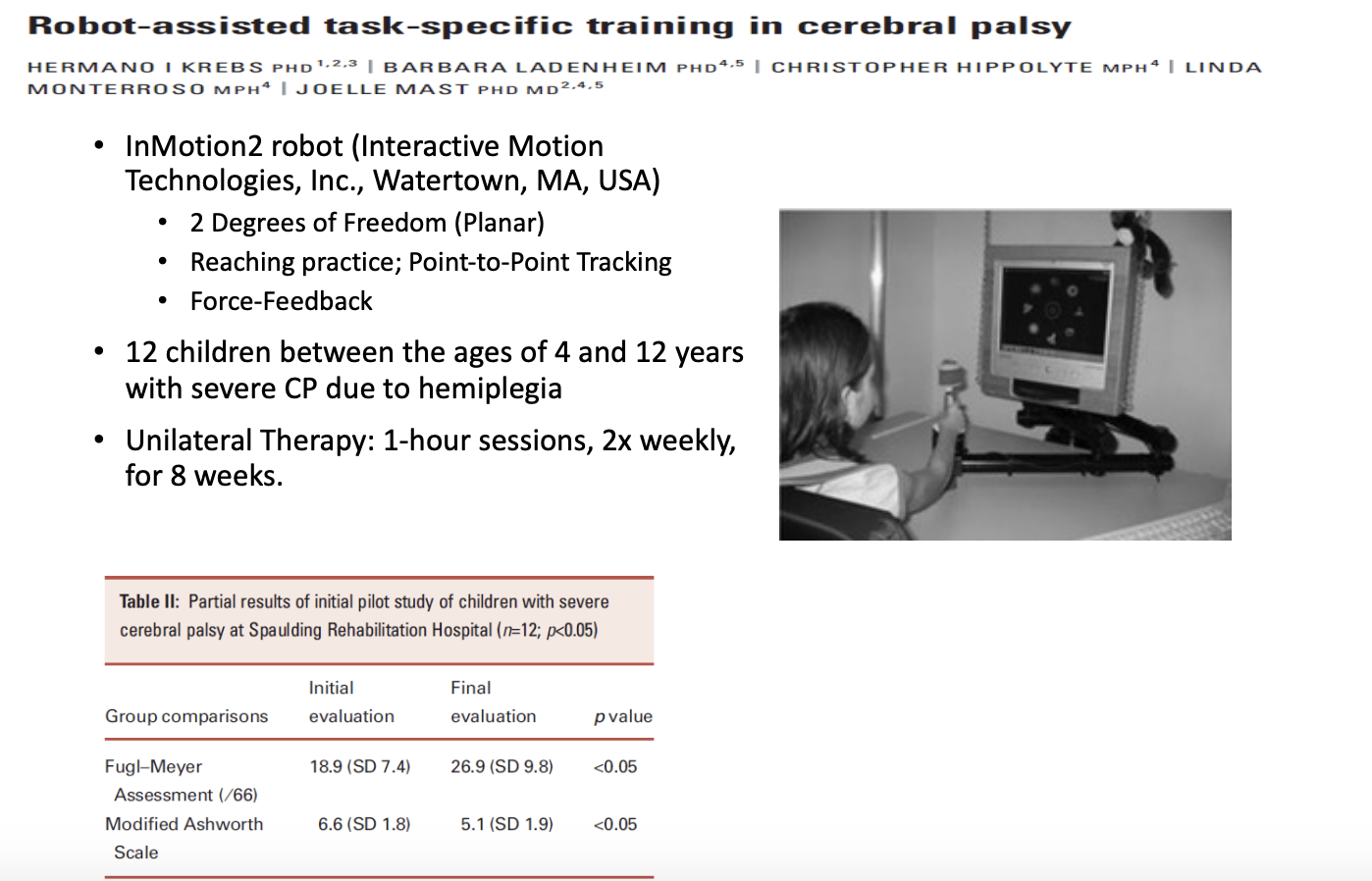
image
systems have also been used for kids w/ cerebral palsy; similar results
ADLER
3D (3 degrees of freedom)- Example
HELPER ROBOT
robot with motions in 3-dimensional space, so that you can move in and out of the plane; designed for people to practice a task in their workspace, but also were connected to the robot with their hands free, so that they can interact with objects within the environment
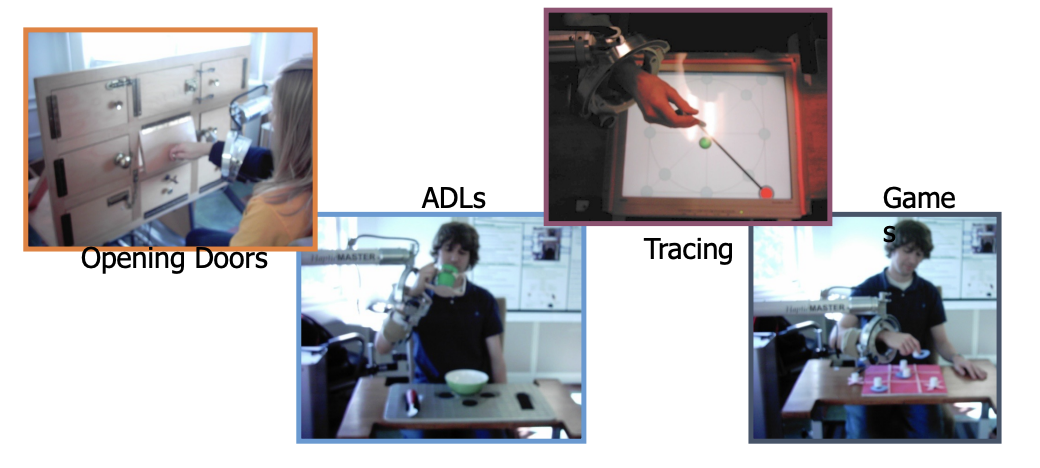
idea is to be more task-oriented
Task-Oriented Robot Assisted Therapy
Design robots to support real tasks/ADLs practice
Design to maintain engagement/motivation
Design is patient-centered
Design is integrated with the clinical environment
Design control strategies that promote effective and adaptive therapy
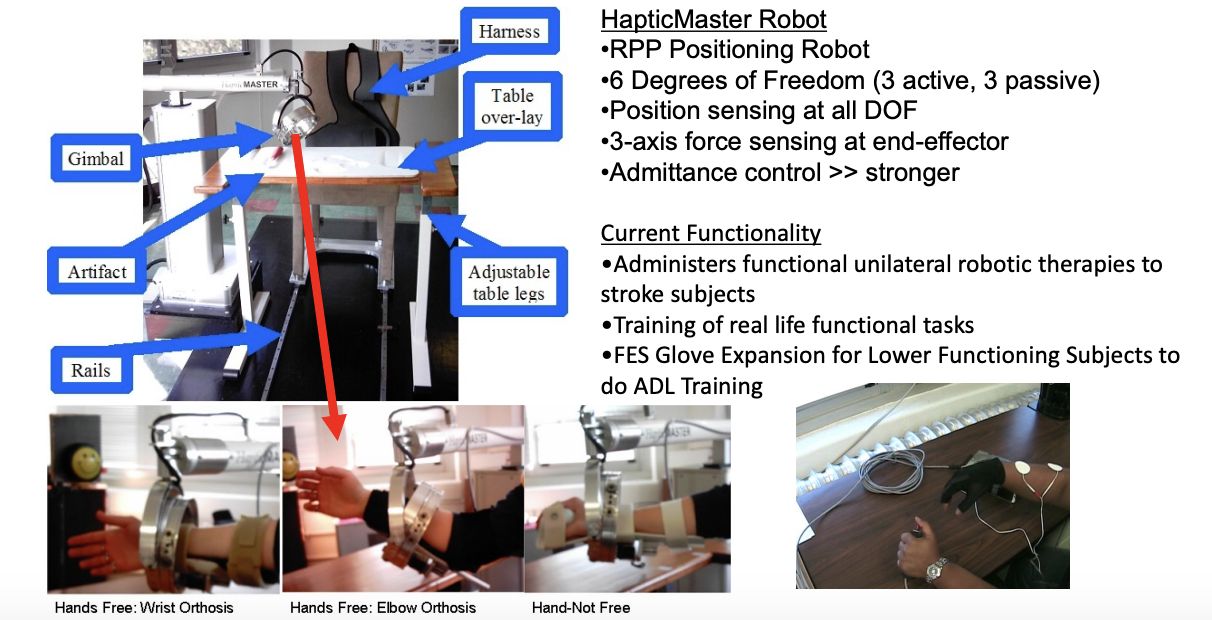
ADLER: Activities Daily Living Exercise Robot
built on a desktop-type environment, and the different end effectors allowed the hand to be free
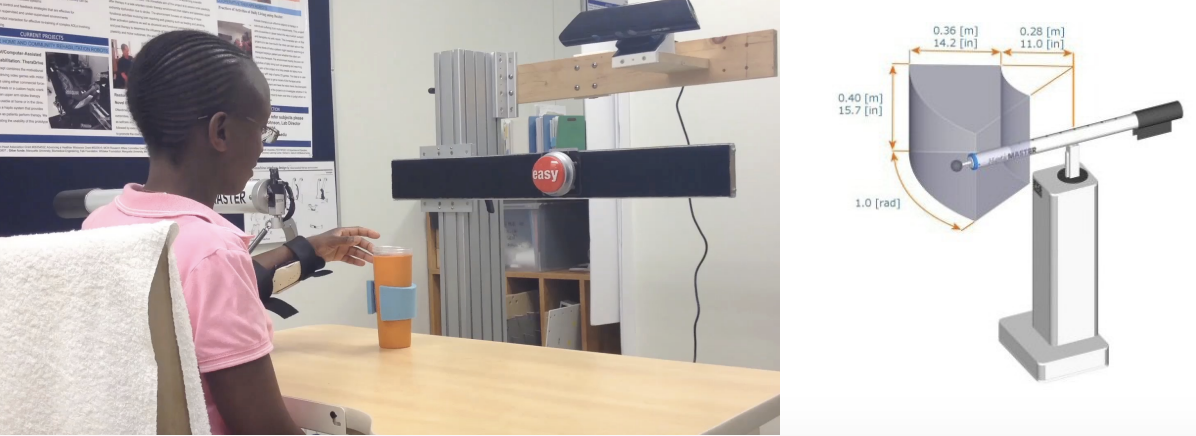
HapticMaster Robot
RPP Positioning Robot
6 Degrees of Freedom (3 active, 3 passive)
Position sensing at all DOF
3-axis force sensing at the end-effector
Admittance control >> stronger
Current Functionality
Administers functional unilateral robotic therapies to stroke subjects
Training of real-life functional tasks
FES Glove Expansion for Lower Functioning Subjects to do ADL Training
e.g., opening/closing activities for those who had a more impaired hand
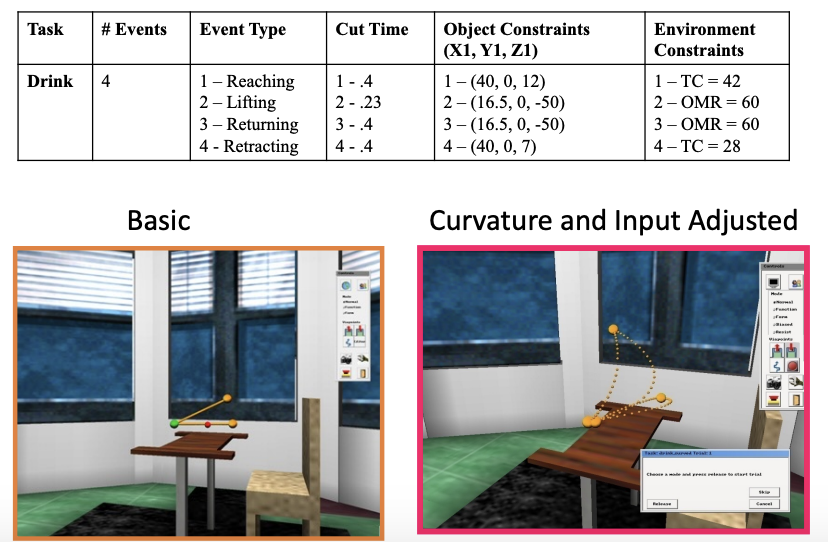
ADLER: Task Examples (3DOF Example)
Use real tasks that reflect ADLs
Adaptable to many motivating and engaging task environments
Supervisory Structure
software that allowed therapists to design programs ahead of time and implement them, so that the robot could actually complete the task
HERALD Software
HapticAPI programming environment
Crystal Space v0.98
PC-based Environment
The GUI shows a one-to-one mapping of the environment and the trajectory
Programming Activities
On the fly, using start, end, and multiple via points to define the task
By uploading data from a file with real or pre-defined trajectories
Various models of task trajectories are programmed
Moves the subject in Training modes

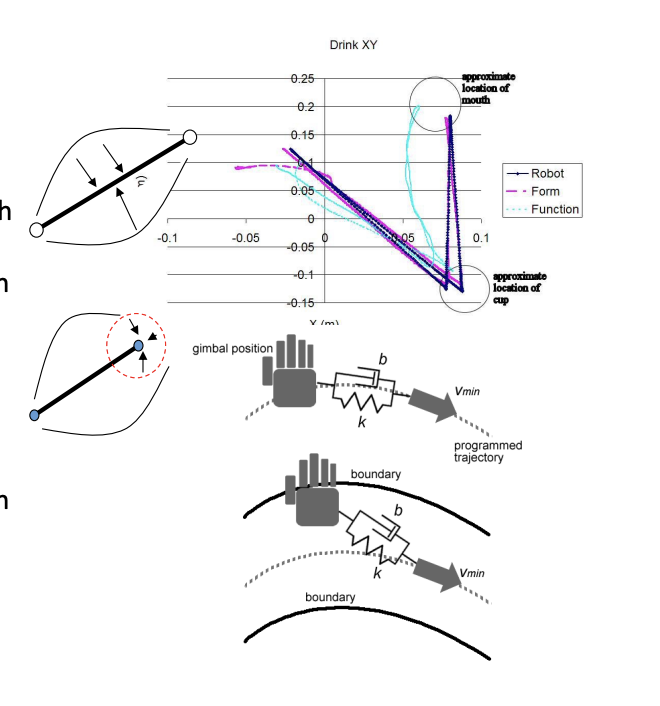
Trajectory Planning for Reaching
to map different trajectories (e.g., reach to the cup; bring cup to mouth), had to develop different types of models (versions of the minimum jerk paradigm- the original model)
modified ways to incorporate real tasks
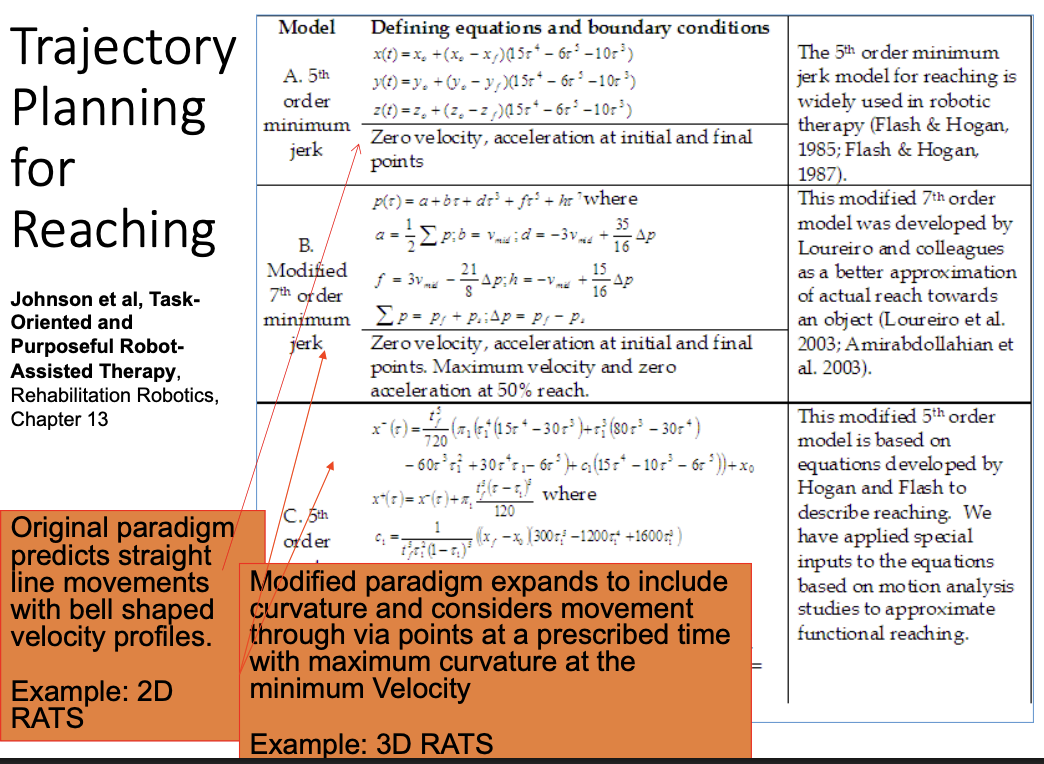
Trajectory Planning ADLER (3D)
Example of projection planning for a real task within the environment
Reaching Training
Current Training Strategies
Form (Guiding Forces); for people who are very impaired
Actively follow a desired path
supports movement along the path, so there would be reinforcement of movement
Experience forces if they deviate
Graded resistance along the path
goal: tracking the original movement of the robot
Function (Minimal Guiding Forces) (New); for people who are less impaired
Aim for the target point
supports target reaching
Permitted to deviate
Attracted to the target
Graded resistance along the path
goal: get to the target
Resist
Normal (No forces): Evaluation mode
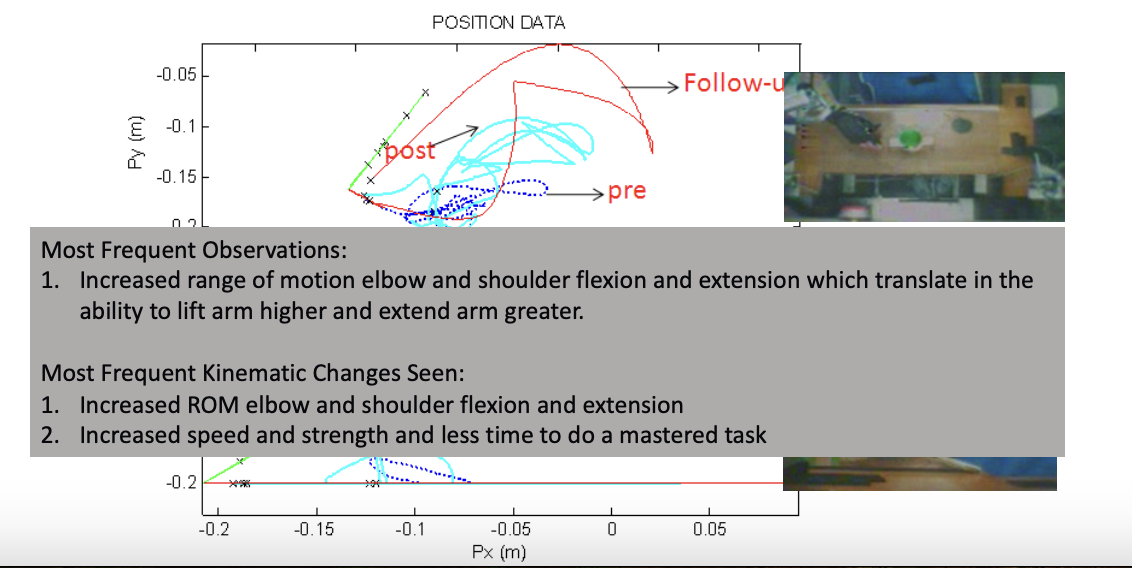
Observed Kinematic Changes
tested Adler with patients; after 4 weeks of interacting with the system, 3x/week for ~1hr
== system can promote recovery and reduction in impairment for a drinking task (i.e., as a result of the treatment, the person was able to move across the table + move out of the plane a little bit better)
Most Frequent Observations:
1. Increased range of motion of the elbow and shoulder flexion and extension, which translates into the ability to lift the arm higher and extend the arm further
Most Frequent Kinematic Changes Seen:
1. Increased ROM of the elbow and shoulder flexion and extension
2. Increased speed and strength, and less time to do a mastered task
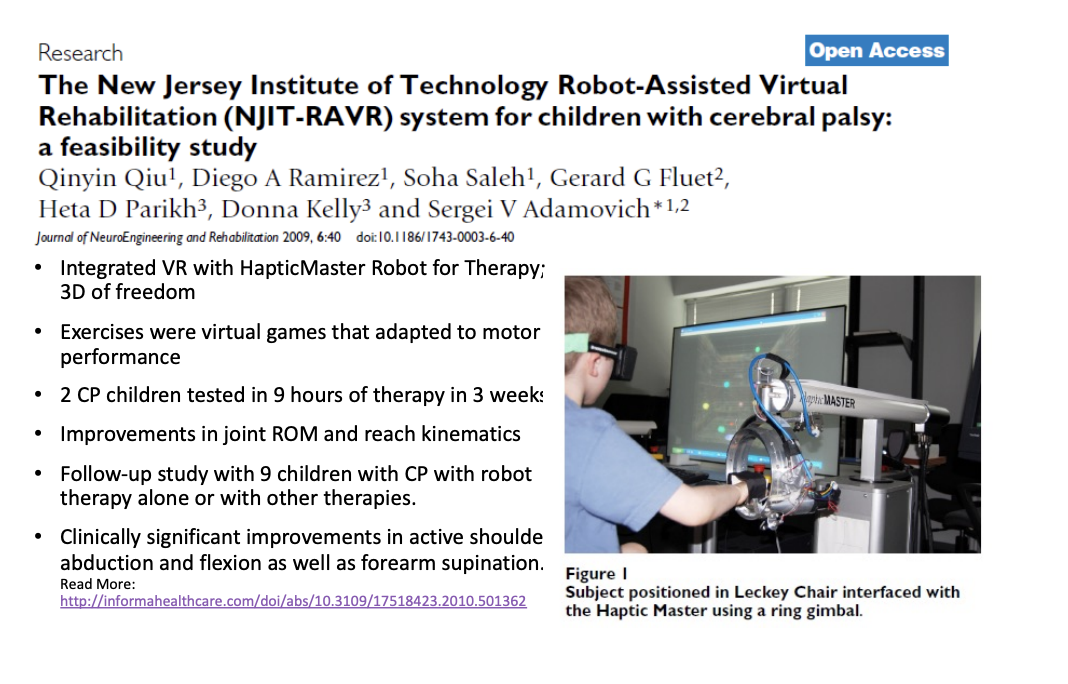
also saw that the system was useful for children in a more VR-type environment
Integrated VR with HapticMaster Robot for Therapy; 3D of freedom
Exercises were virtual games that adapted to motor performance
2 CP children tested in 9 hours of therapy in 3 weeks
Improvements in joint ROM and reach kinematics
Follow-up study with 9 children with CP with robot therapy alone or with other therapies
Clinically significant improvements in active shoulder abduction and flexion as well as forearm supination.
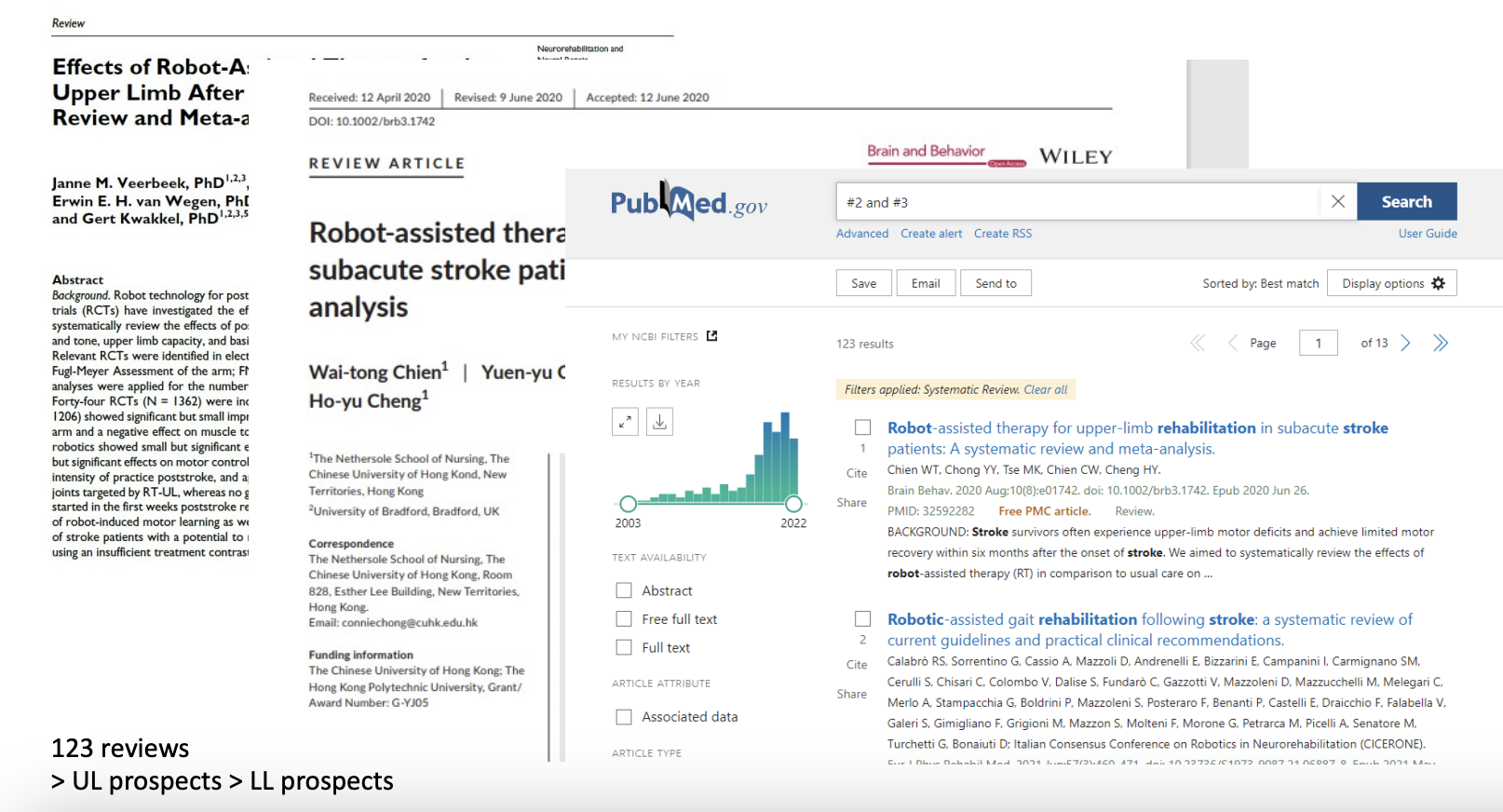
reviews + pros of rehabilitation robotics
original reviews
upper limb robot therapy is able to reduce motor impairment
pros of rehabilitation robotics
As effective as high-intensity physical therapy
Repeatable
Adaptive
Enable semi-autonomous training
Provide consistent training
Provide objective measures of recovery
Reduce Impairment
Increase Activity
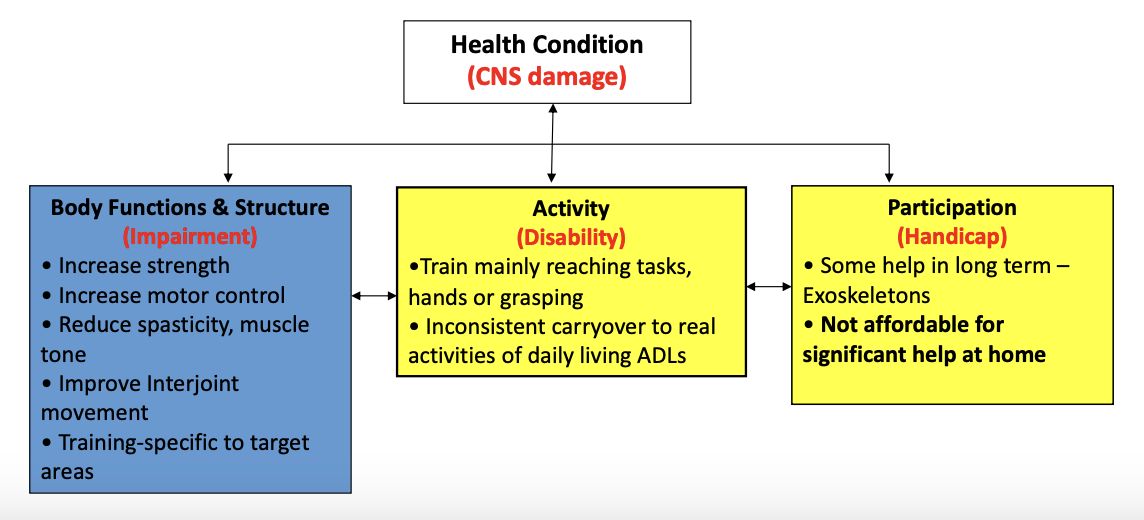
Key Findings: Robot Assisted Therapy by ICF
Health Condition (CNS damage)
Body Functions & Structure (Impairment)
Increase strength
Increase motor control
Reduce spasticity, muscle tone
Improve Interjoint movement
Training specific to target areas
Activity (Disability)
•Train mainly reaching tasks, hands or grasping
Inconsistent carryover to real activities of daily living ADLs, but still have effects overall
Participation (Handicap)
Some help in the long term – Exoskeletons
Not affordable for significant help at home
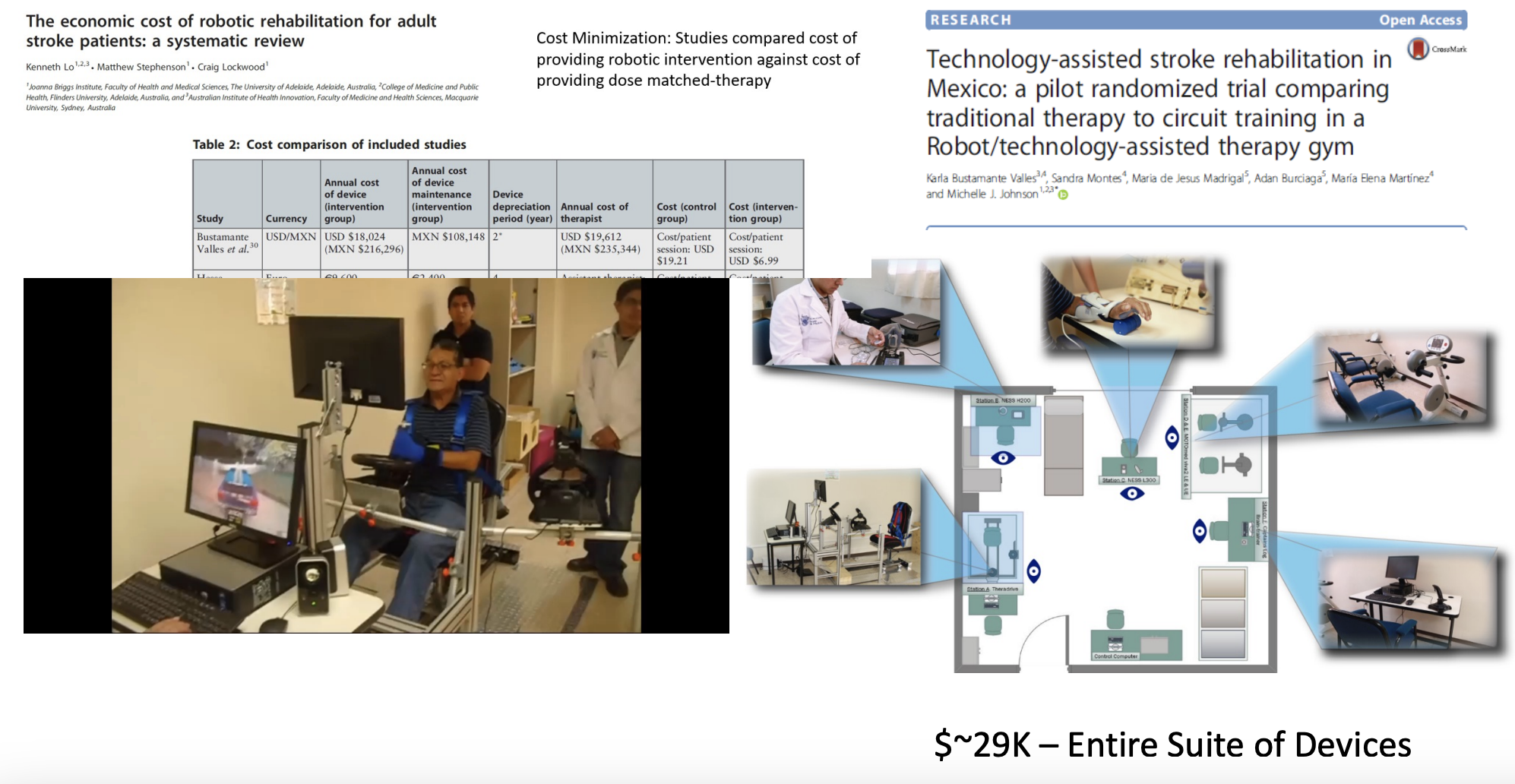
The economic cost of robotic rehabilitation for adult stroke patients: a systematic review
Cost Minimization: Studies compared the cost of providing robotic intervention against the cost of providing dose matched-therapy
robots are favorable in terms of their outcomes as compared with the standard of care
in general, robots are worth pursuing
Rehabilitation Robotics Market
growing market!
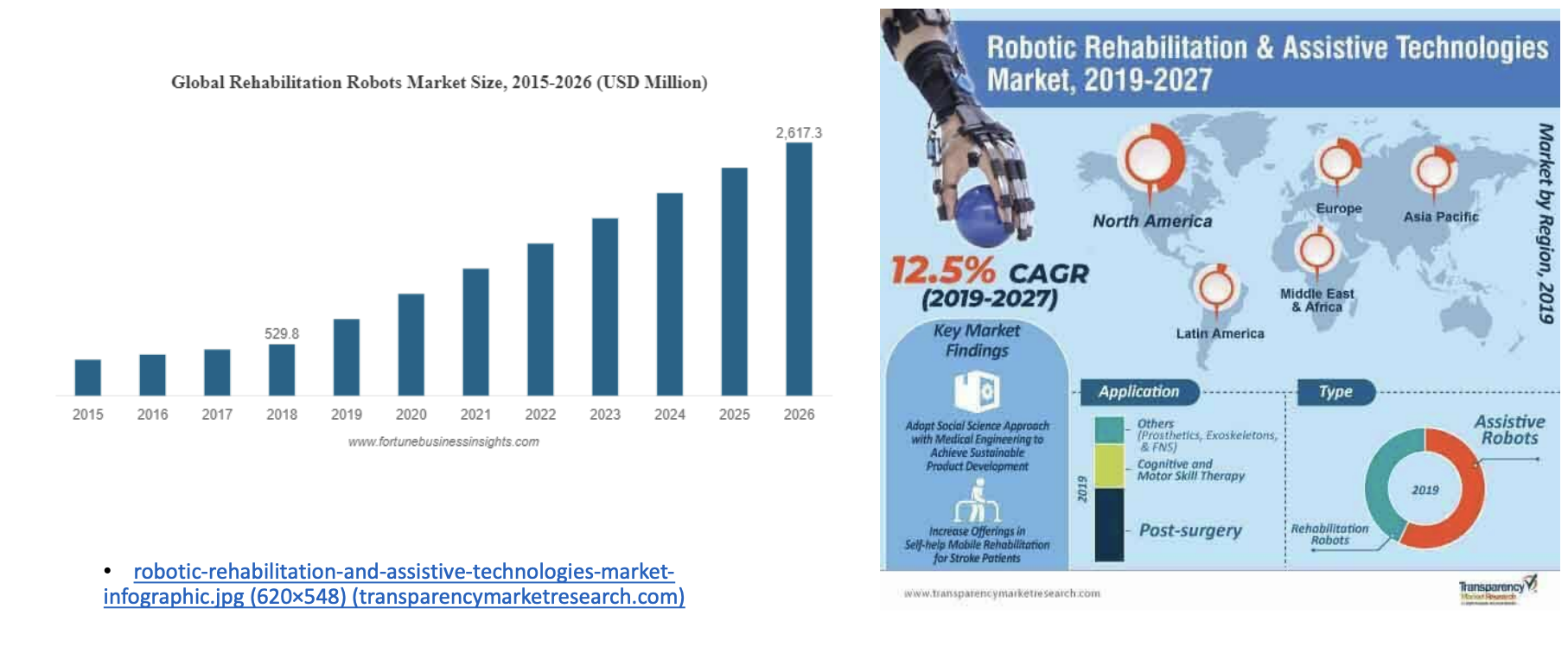
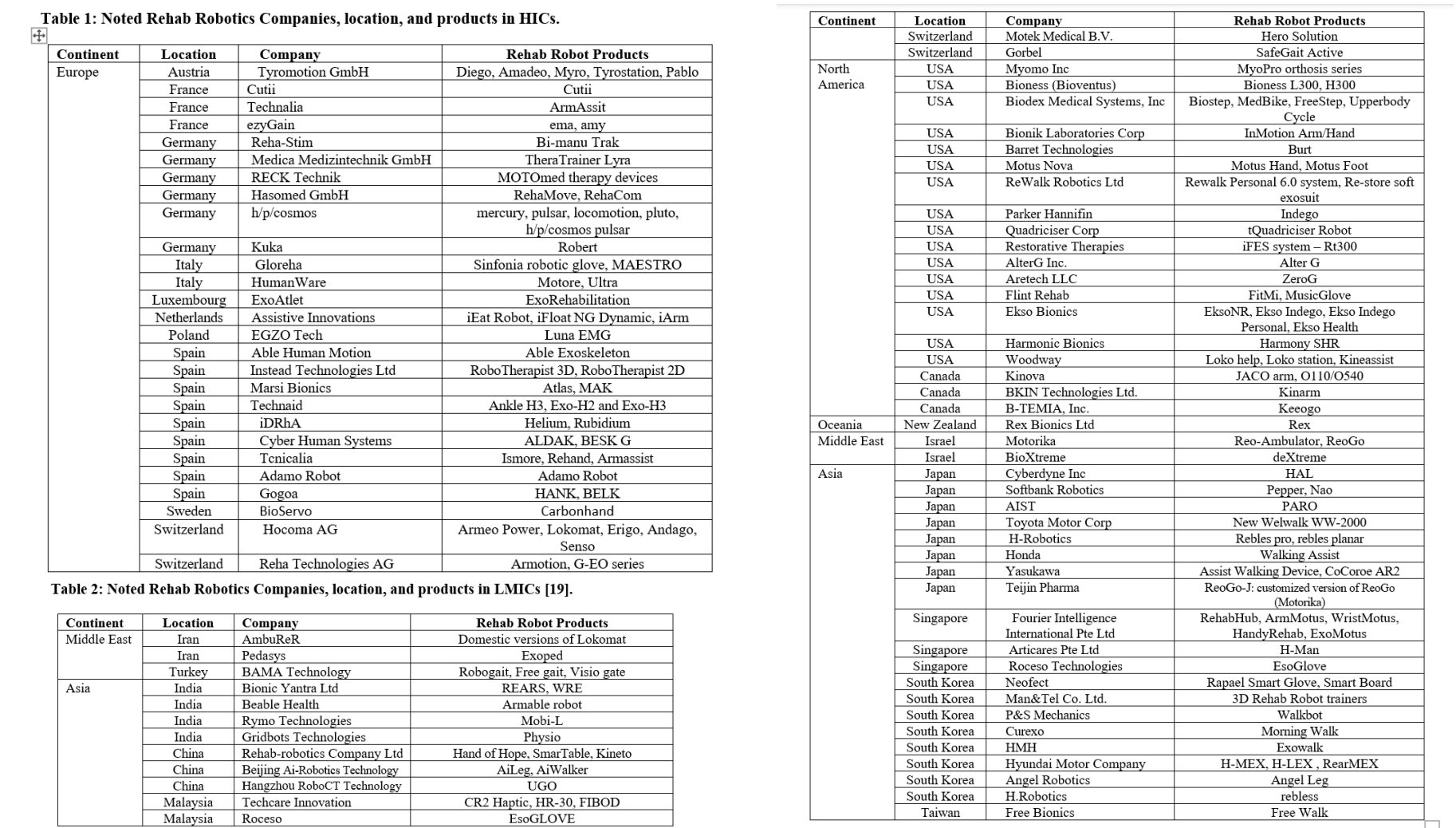
Rehabilitation Robots for Neurorehabilitation in High-, Low-, and Middle-Income Countries Current Practice, Barriers, and Future Directions
growing number of companies in Europe, North America, and Asia- high-income countries; much less in South America and Africa
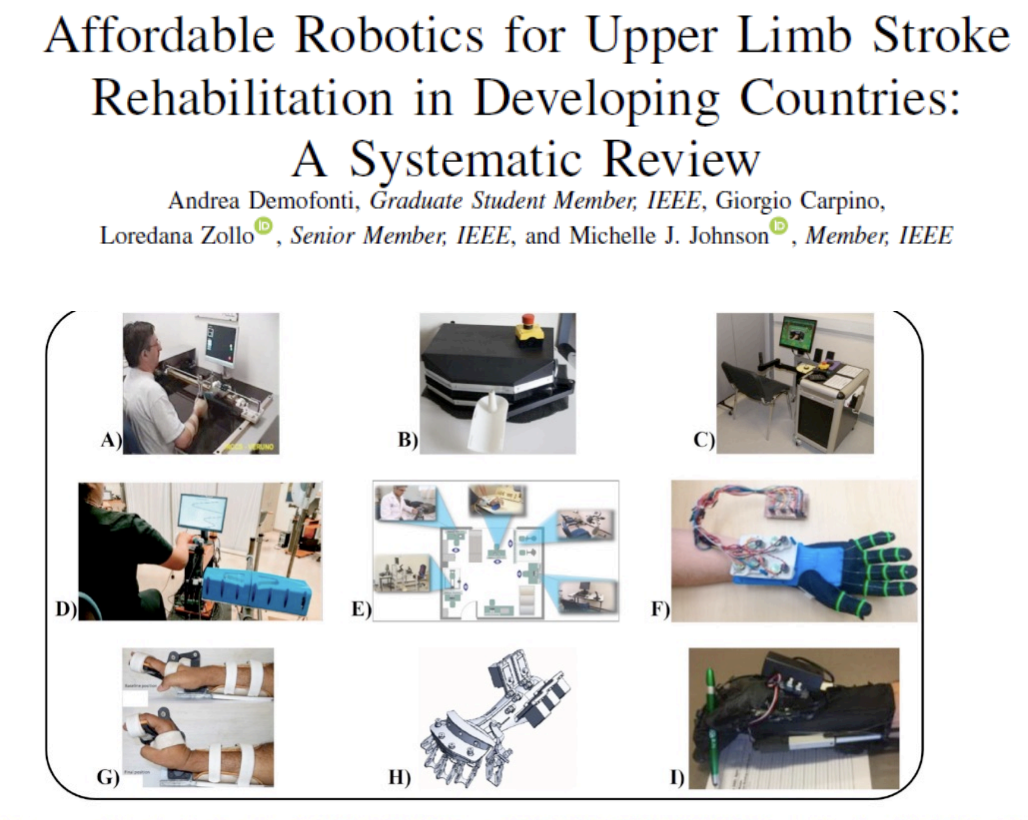
Problem with current systems for LMICs
design issues:
Mechanical complexity
Huge sizes and masses
High Costs
REHABILITATION 2030- a call for action
there is a global need for rehabilitation and the availability of services
World Health Organization passed a law saying that all their member countries should prioritize rehabilitation
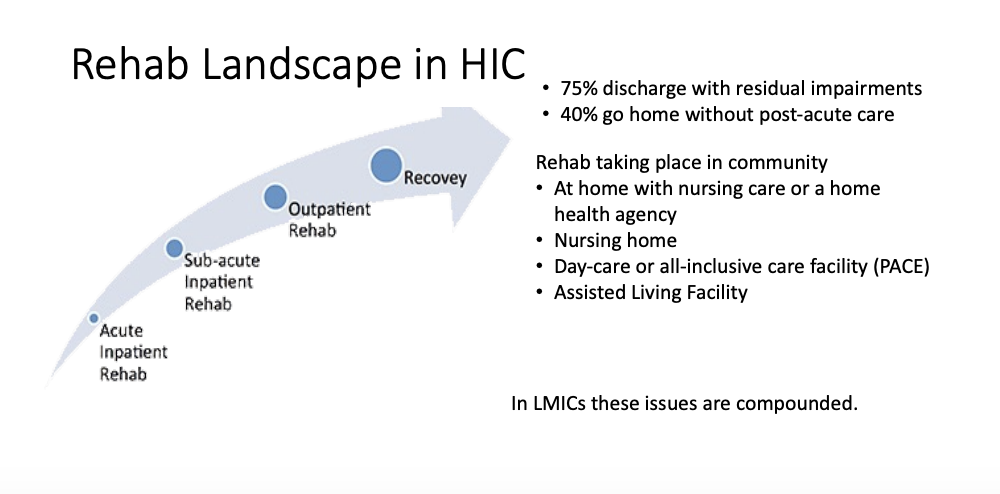
Rehab Landscape in HIC (high-income countries)
even in HIC, rehabilitation is increasingly occurring outside of a hospital environment in acute care
75% discharge with residual impairments
40% go home without post-acute care
Rehab taking place in the community
At home with nursing care or a home health agency
Nursing home
Day-care or all-inclusive care facility (PACE)
Assisted Living Facility
In LMICs (low and middle income countries), these issues are compounded
Rehabilitation in Low and Middle Income Countries
Rehabilitation is often an afterthought, and the focus is on disease cure
Rehabilitation access is low (below WHO guidelines)
Rehabilitation care is not as specialized, and many are not trained to deliver it
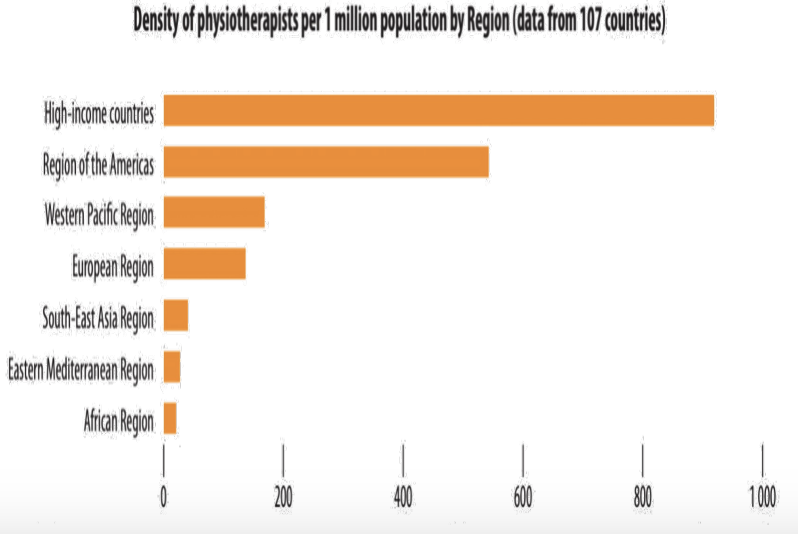
Skilled therapists and physiatrists are often not available in large numbers inside or outside of cities;
Low doctor-patient ratios, e.g., in Malawi 1:88,000
Low therapist-patient ratios, e.g., in Botswana – a hospital ~15:800 beds
Rehabilitation technology is not available or is not of the same quality
Some Key Guidelines
Rehabilitation Robots In LMICs Must Be Affordable
Rehabilitation Robots In LMICs Must Be Multipurpose
Rehabilitation Robots In LMICs Must Be Effective
Rehabilitation Robots In Low-Resource Settings Must Promote Community-based Rehabilitation
Rehabilitation Robots In LMICs Must Be Appropriate
Sustaining Rehabilitation Robots In LMICs Depends On Capacity Building
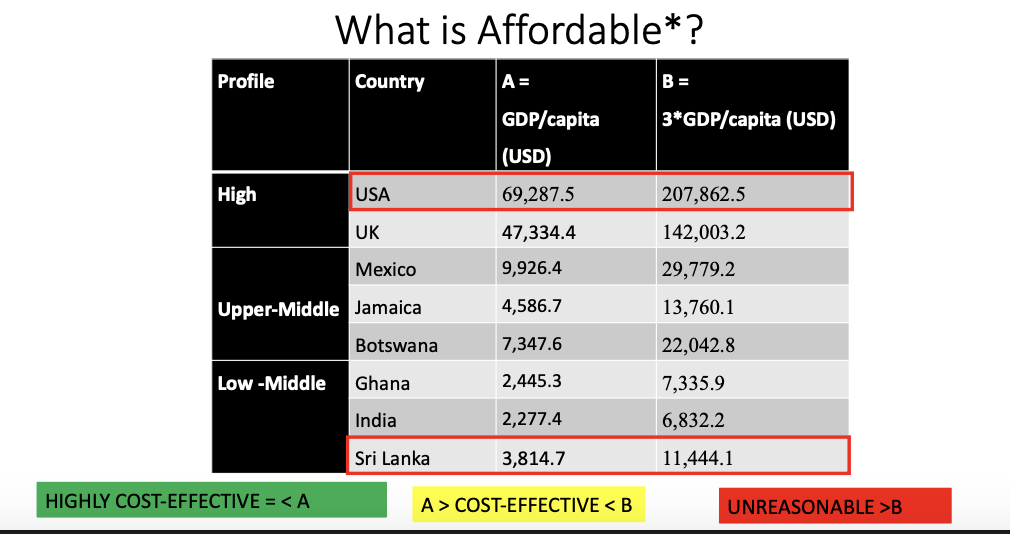
Affordability
“Robots are not affordable … but despite their high cost … a likely advantage is that automated interventions like robotic therapies require minimal input from rehabilitation professionals in terms of time and efforts.”
affordability, noun= the extent to which something is affordable, as measured by its cost relative to the amount that the purchaser can pay
Potential strategies to reduce cost and be multipurpose?
Use low-cost robotics/mechatronic systems
Use cheaper materials – 3D printing/soft robots/found objects
Use a system of low-cost robot units that can reconfigure
Use multiple-use systems
Use local manufacturing and resources
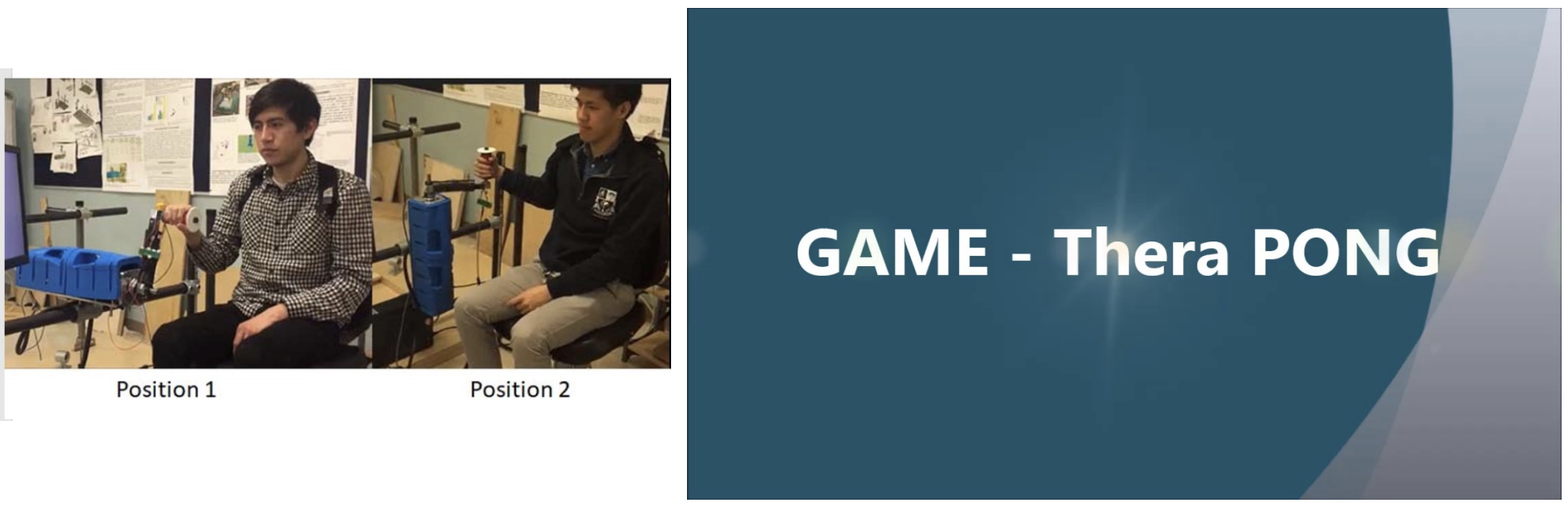
Mexican Theradrive
a low-cost training system
6-station training gym that had robotic and technology assistant systems in the gym
ran a study confronting the standard of care vs people participating in the gym
== saw that it was cost-effective; able to maximize the impact of the therapies without diminishing the outcomes of therapies
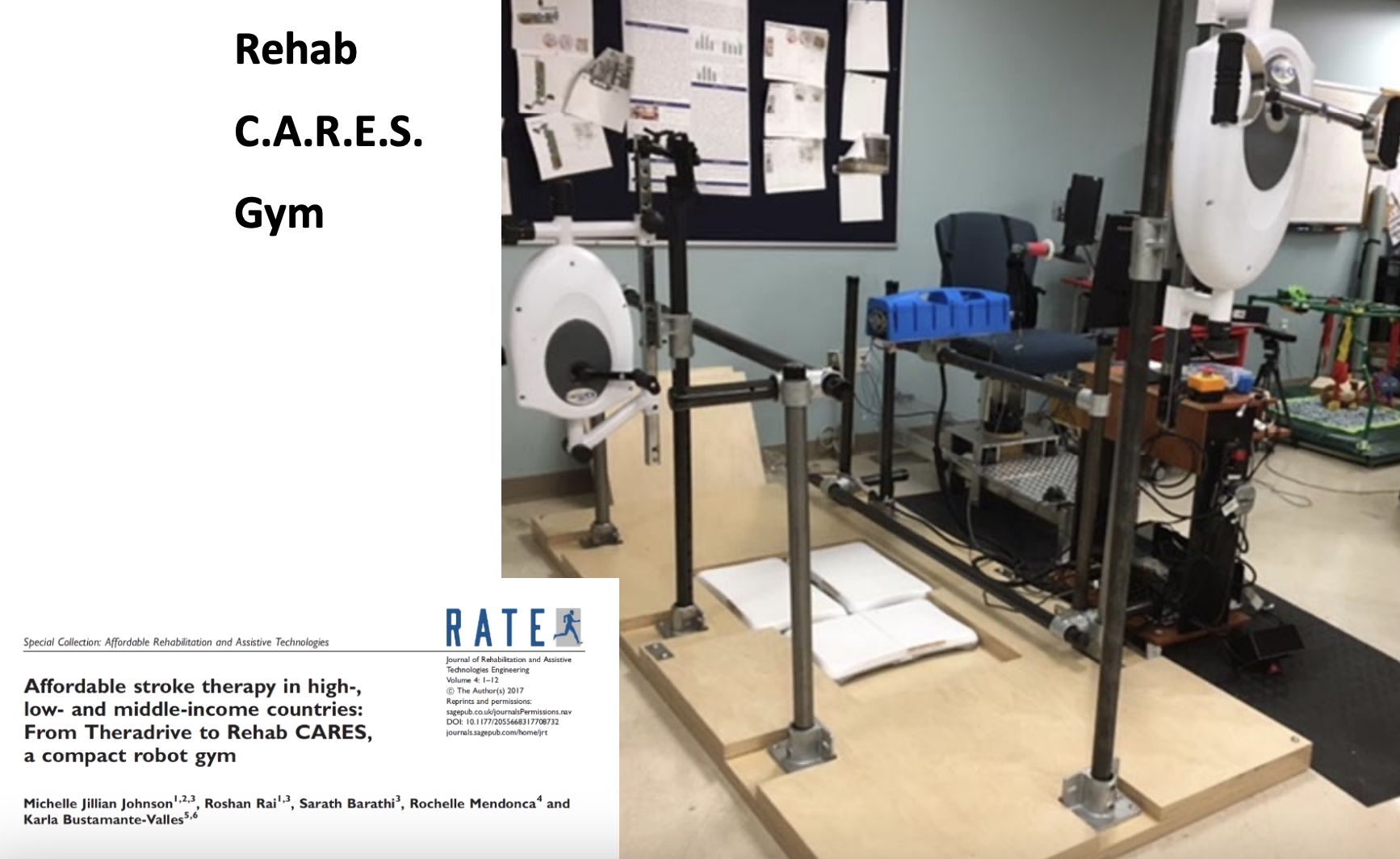
Rehab C.A.R.E.S. Gym
community based scenario of multiple robots together that could then be placed in different areas
Haptic Theradrive (TD-3)
also developed a new robot that was stronger and able to support people with more severe impairment