NM701 - Module 5 - AUB (abnormal uterine bleeding) and Pelvic Pain
1/112
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
113 Terms
Common causes of anovulation include:
PATHOLOGIC:
thyroid/pituitary disorders - (if too little or too much)
hyperprolactinemia
iatrogenic (radiation/meds)
PCOS - (one of the hallmarks of PCOS is oligo-ovulation)--- that may stretch out into long enough time periods that we call it anovulation)
PHYSIOLOGIC:
pregnancy (most common)
lacation
perimenarche (immature HPO axis)
perimenopause (not as sensitive to FSH and cycles space out)
low/high BMI
excessive exercise
Estrogen levels will
increase the thickness of the endometrium
high estrogen = heaviest bleeding
Explain why excessive uterine bleeding may be a sign of endometrial hyperplasia or cancer
Although rare, long periods of anovulation in the presence of unopposed estrogen can predispose to developing endometrial cancer.
Hyperplasia can mutate the cells of the lining that can become cancerous.
hyperplasia or cancer always a possible cause of heavy or irregular uterine bleeding, especially when a woman has been anovulatory for a long time
What methods can rule out endometrial cancer?
Start with TVUS and move to biopsy only if imaging findings are suspicious.
A thin endometrium on TVUS can rule out endometrial cancer (less invasive)
Timing of the ultrasound is important to avoid false positives
Age of onset for endometriosis
adolescent to early adulthood
Age of onset for PCOS, adenomyosis, PMS, endometrial hyperplasia
middle to late reproductive years
Age of onset for ovarian/breast cancer
post menopausal
Intense itching of the vulva may be associated with:
lichen sclerosis, yeast vaginitis, contact dermatitis
What is the origin of most chronic pelvic pain?
About 2/3 of chronic pelvic pain has a GI or GU origin
other causes:
abortion
ectopic
PID
ovarian pain
adrenal tension
fibroids
dyspareunia
endometriosis
What are the most encountered diagnoses in gynecologic care?
amenorrhea
abnormal uterine bleeding
hyper androgenic disorders
Amenorrhea
NO pd x 3mos OR
6mos if cycles are irregular
this and anovulation can occur when estrogen is present or absent
How can we effectively rule out endometrial hyperplasia or cancer?
via TVUS and if they endometrial lining is less than 4mm thick
endometrial sampling is indicated if lining is large
**for many perimenopausal women, lining will be thick UNLESS ORDERED WITHIN THE FIRST 5 DAYS OF THE PD**
dysmennorhea
painful menstrual cramps
primary in young people is normal with high prostaglandins
Anovulation in a rich environment means the body gets stuck in
LACK OF PROGESTERONE - the luteal phase leading to hyperplasia and random painless disorganized bleeding
causes of Intermenstrual periods
fragile or inflamed tissue on the cervix, vagina or higher in the reproductive tract
cervical polyps
cervical cx
STI's
ectropion
irregularly sloughing hyperplastic endometrium
When does intermenstrual bleeding occur?
either with regular or irregular periods
Causes of prolonged bleeding
pelvic pathology
endometriosis
hypo androgenic disroders
A change in the TIMING of the period is caused by
a hormonal change such as:
GNRH
release patterns of FSH, LH
no progesterone
Examples:
Thyroid disorder
PCOS
endometrial hyperplasia
A change in the BLEEDING is caused by
a structural or systemic change (mostly structural)
Leiomyomas (Fibroids)
adenomyosis
Examples:
polyps (spotting)
blood dyscrasias
rarely von willebrands disease
NO BLEEDING (amenorrhea) can be caused by
EITHER hormonal or structural changes
Ex:
Outflow obstruction
elevated prolactin
pregnancy
F. is a 24-year-old woman who reports that her last period was 5 months ago. Her periods have always been irregular, with 7-8 periods per year. She is sexually active and uses condoms for contraception. F. has never been pregnant. She has had screening Paps since age 21 and both have been normal. F's prior medical history is uncomplicated. Her past surgical history includes repair of an ankle ligament in high school. She is training for a marathon and has intentionally lost 15 pounds in the last few months.
Review of systems:
increasing acne and hair growth on her chin
more frequent headaches, some with nausea and vomiting.
Based on F's history, the clinician can safely conclude that F has:
secondary ammenorrhea
Based on F's history and review of systems, EXPECTED history and exam findings would be:
hirsutism
acanthosis nigricans
lack of PMS
dysmenorrhea
What lab tests are necessary in someone with secondary amenorrhea?
Pregnancy test (always R/O first!)
TSH
Prolactin
Which is true regarding making a diagnosis of polycystic ovary syndrome (PCOS)
oligo-ovulation and clinical signs of hyperandrogenism
According to the Rotterdam criteria, these 2 criteria are sufficient for diagnosis once other conditions are excluded.
*DIAGNOSIS OF EXCLUSION*
with PCOS, what is true about a progestogen test?
likely to bleed after the PCT because her estrogen levels are adequate to develop an endometrium
with PCOS considering differential diagnosis?
Pituitary tumors or dysfunction are possible considering bleeding pattern and symptoms.
If lab testing confirms PCOS, management should include:
incorporating reproductive life goals in the plan.
What is true regarding using combined oral contraceptives (COCs) to manage PCOS?
COCs raise sex hormone binding globulin because they are administered orally, which may help bind free androgens and reduce new hair growth.
COCs typically improve acne as well.
B. is a 46-year-old woman who presents with "period problems." She reports that her periods have been getting progressively heavier for about 3 years, but it's getting to the point now that she has a hard time leaving the house the first 3 days of her period because they are so heavy. Her periods are generally regular, with a 26-day cycle length. Her husband had a vasectomy 10 years ago. She had three normal vaginal deliveries without pregnancy or birth complications. Surgical history includes only an appendectomy at age 25. B. is a 1 pack per day smoker. A review of systems is significant for headaches, recent constipation, and dry skin. Her BMI is 31.
___________________________________________________
Possible differential diagnoses for B currently include:
anemia
AUB-E
perimenopause
abnormal bleeding patterns are associated with
a large, tender uterus
Which diagnsotic tests to order if you think the patient has prolactinemia?
An endometrial biopsy or transvaginal ultrasound early in the cycle to evaluate the endometrium.
Yes, endometrial hyperplasia and endometrial cancer are don't-miss-it diagnoses. This woman's endometrium must be evaluated in some way because she is experiencing progressively worsening heavy menstrual bleeding
If a patient is dx with AUB, a safe option is
MONOPHASIC birth control
B asks about a hysterectomy to address her heavy menstrual bleeding. An appropriate response from the clinician is:
Hysterectomy does work to solve this problem, but there are significant risks from surgery.
Most people find their heavy bleeding is adequately controlled by a Mirena IUD.
What may commonly cause secondary amenorrhea?
prolonged anovulation with low or no estrogen
prolonged anovulation with normal or high estrogen
secondary amenorrhea
no period for 3 mos in women with previously normal periods AND for nine months in women with previous oligomenorrhea (infrequent periods, more than 35 days)
In one pathway to secondary amenorrhea, a pituitary tumor causes
PROLACTIN to rise which suppresses
GNRH, resulting in very low levels of
ESTROGEN
Prolactin may increase because of:
frequent breast stimulation
breastfeeding
prolactinoma (bening pituitary tumor)
medications (such as mood stabiliziers)
What are causes of secondary amenorrhea?
PREGNANCY
asherman syndrome
cervical stenosis
contraception
thyroid issue
pituitary tumor
PCOS
cns/hypothalmic disorders (anorexia, chronic disease, stress, athleticism)
obesity
prolactinoma
menopause
ovarian insufficiency
causes of primary amenorrhea
pregnancy, imperforate hymen, gonadal dysgenesis (turner's syndrome), HPO axis abnormalities (anorexia, bulimia, weight loss, excessive exercise), FSH greater than 40
what is the hormonal state for PCOS and obesity?
normal to high estrogen
What is the hormonal state for menopause and ovarian insufficiency?
HIGH FSH/LH with LOW estrogen
What is the hormonal state for chronic disease, anorexia and prolactinoma?
LOW estrogen
Expected Progestogen challenge test results for galactorrhea,
prolactinemia, ovarian insufficiency
NO bleed due to insufficient estrogen (negative)
Expected Progestogen challenge test results for PCOS and obesity
WITHDRAWAL BLEED (positive)
ss of adenomyosis
Enlarged uterus on bimanual exam
Usually in older women
Caused by endometrial tissue implanted in the myometrium
SS of endometriosis
Uterus may be fixed to pelvis or other structures
pelvic pain, dysmenorrhea, dyspareneuia, abnormal bleeding
SS of both Endometriosis OR adenomyosis
Tender uterus on bimanual exam
what type of woman is more likely to have adenomyosis?
40+ who is multip
HX of miscarriage, curettage, endometrial resection, csection or tamoxifen use
previously normal menses
no pelvic pain until recently
what type of woman is more likely to have endometriosis?
dysmenorrhea, painful defecation, and infertility
most common cause of anovulation
pregnancy
What are differential diagnosis for heavy bleeding?
endometriosis
adenomyosis
hyperplasia
perimenopause
fibroids (if they have SS - leiomyomatas)
polyps
PID
adhesions
what is the hallmark of endometriosis?
Cyclical pelvic pain worse at 1 to 2 days before menses and WITH PERIODS
may or may not involve bleeding changes
may progress to pain in between periods
pain with intercourse
what some less common causes of AUB?
copper IUD
miscarriage
What does ACOG recommend if 45 and up with AUB or risk factors?
must ensure its not hyperplasia prior to treating
do a pelvic US or endometrial biopsy
risk factors for hyperplasia
AUB
postmenopausal bleeding
most common causes of amenorrhea in general?
pregnancy
menopause
PCOS
fibroids (leiomyomas)
most commonly have NO SX
can cause pain
benign estrogen-dependent uterine muscle tumors --> menorrhagia (heavy period) most common presentation
Surgical Indications = cause anemia, severe pelvic pain, uterine size > 12 wks, urinary symptoms, growth after menopause, recurrent miscarriage or infertility, rapid increase in size
-- Complications = recurrence in 50%, adhesions
waht is the first line tx for AUB-E?
LNG - IUD
IUD will assist with long term bleeding but to stop acute bleeding, estrogen therapy or tranexamic acid is used
what medication is helpful for adenomysis and dysmenorrhea?
NSAIDS
helpful when pain severe and medication resistant because they reduce pain by reducing prostaglandins
Adenomyosis
benign invasive growth of the myometrium that may cause heavy, painful menstrual bleeding
What are all the risks for unopposed estrogen/endometrial hyperplasia?
PCOS,
obesity,
estrogen therapy w/o progesterone
lynch syndrome (hereditary nonpolyposis colorectal cancer (HNPCC) - high risk for colon cancer and endo cancer
What does the PCT require?
requires estrogen to be present (and the outflow tract has to be patent) for there to be a withdrawal bleed.
SS of uterine fibroid
enlarged uterus, asymmterical, painless, usually associated with AUB
SS of adenomyosis
benign invasive growth of the myometrium that may cause heavy, painful menstrual bleeding
ENLARGED uterus, symmetrical, moderate tenderness, increases menses
SS of cervical polyps
bright red PAINLESS bleeding after sex
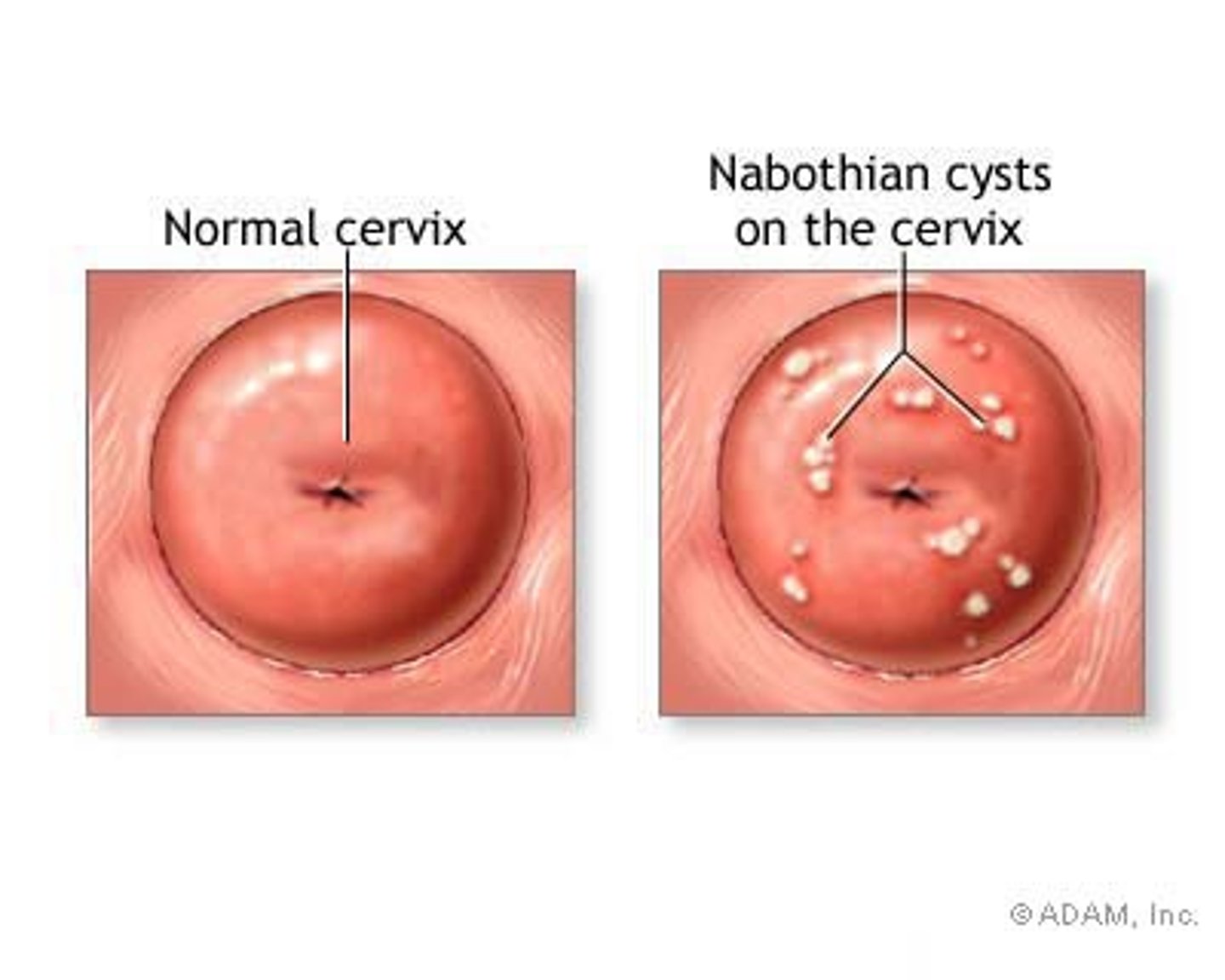
SS of nabothian cysts
white, firm, painless nodules visible on cervix
differential diagnosis for secondary amennorhea
hypothyroidism
hyperprolactinemia
outflow tract obstruction and hyperandrogenic chronic anovulation.
Regularity of periods by age
18- 29 and 42+ = 9 days or less
30-41 = 7 days or less
AUB-PALM
related to structural abnormalities
AUB - COEIN
UNrelated to structural abnormalities
What physiologic processes explain why irregular menses are common during adolescence and perimenopause?
due to life cycle changes
in first 2 yrs of pd and 3 yrs before menopause
Consider the differences between evaluating and managing a YOUNG person's abnormal uterine bleeding and an OLDER person's abnormal uterine bleeding. How is the investigation different? Why? What are the special concerns of a perimenopausal person with AUB
Adolescence- don’t require as much, if any, investigation, if during the first 2 years of menses
1. Assess for eating disorders, iron/folic acid deficiency anemia
2. Assess for sexual function, need for BC
3. Pelvic exam only if specific indication
·Perimenopausal- incidence of AUB increases within 3 years of menopause
1. Associated w/ menopause or ovulatory s/s: PMS, dyspareunia or irregular bleeding
2.Provide education r/t health risks: diet/exercise for osteoporosis, quit smoking, etc.
3. r/o endometrial hyperplasia/endometrial cancer (45yo+)
What conditions cause heavy, irregular and/or intermenstrual bleeding?
If childbearing age w/ previously normal cycle -
most likely cause is a complication of pregnancy → rule that out, then begin down PALM-COEIN:
- Polyps (bleed easy)
- Adenomyosis – menorrhagia (abnormal heavy bleeding during menstruation)
- Leiomyoma-fibroids- if submucosal- then interfere with endometrium and is more likely to cause AUB
-Malignancy/hyperplasia - postmenopausal bleeding
-Coagulopathy - heavy, usually first sign in teen yrs of bleeding disorder
-Ovulatory dysfunction
-Heavy - secondary to high/sustained unopposed estrogen
-PCOS - estrogen-related breakthrough bleeding
-Endocrine - thyroid, pituitary, increased prolactin
-Heavy & irregular - POPs, progestin-only contraception
-Irregular - post-menarche or perimenopausal
-Heavy and often prolonged - pelvic pathology
-Uterine fibroids/leiomyomas
-Adenomyosis
- Endometrial polyps
-Heavy and intermenstrual - endometrial is often predictable and cyclical and can also be intermenstrual or prolonged
- Intermenstrual - chlamydia
-Irregular - gonorrhea and endometritis or iatrogenic often characterized by breakthrough bleeding
What are likely and unlikely causes of different types of AUB:
New-onset vs. long-standing bleeding abnormalities
1. Regular: structural or systemic cause e.g.: fibroids, polyps (spotting), blood dyscrasias
2. Irregular: Hormonal change/cause e.g. thyroid problems, PCOS, endometrial hyperplasia (UNLIKELY)
3. Amenorrhea: either- outflow tract obstruction, elevated prolactin, pregnancy
1. Irregular and/or regular:
1. Ovulatory dysfunction
2. Fibroids- heavy, clots, “pelvic fullness” (UNLIKELY)
Describe the assessment (history, physical examination, and diagnostic testing) and management options for individuals presenting with abnormal uterine bleeding. Include patient education.
1.HX: a detailed menstrual hx
2. PE:
General PE for signs of systemic illness such as fever, ecchymoses, enlarged thyroid, or evidence of
hyperandrogenism (hirsutism, acne, clitoromegaly, or male pattern baldness.
Acanthosis nigricans (darkening of the skin in folds and creases) may be seen in people with PCOS
3. DX TESTING:
A pelvic examination is essential for a person of any age who is (or has been) sexually active or has abdominal pain, anemia, or bleeding that results in hemodynamic instability.
A pelvic examination is most likely not necessary if the patient is an adolescent who is not sexually active, recent menarche, and normal hematocrit.
A pelvic examination is helpful for identifying normal genital anatomy, outflow tract patency, and if estrogen depletion is present.
4. Labs and dx:
2. Pregnancy test
3. CBC if indicated or if anemia is suspected
4. Thyroid-stimulating hormone (TSH), especially if thyroid abnormality is suspected
5. Prolactin level if they have headaches, has galactorrhea and/or peripheral vision changes
6. Pap test
AUB-C
Coagulopathies
13% of ppl with AUB present with a clotting disorder
von willebrand is the most common
TX: referral
Anovulatory cycles are characterized by:
lack of PROGESTERONE in the LUTEAL phase that leads to an unstable, excessively vascular endometrium
One of the most concerning causes of AUB is endometrial hyperplasia, a precursor to endometrial cancer. How may endometrial hyperplasia present clinically? How (and in whom) should we rule it out?
Clinical presentation: *most common s/s of endometrial cancer is AUB and postmenopausal bleeding
-Should r/o: If a person is experiencing AUB-O (ovulatory dysfunction) and 45+, endometrial biopsy and pelvic sonography are recommended OR if they are
younger than age 45 (35-45) and have a history of unopposed estrogen exposure, failed medical management (and neg preg test), and persistent AUB, - anendometrial biopsy should be performed
*Transvaginal ultrasound (TVUS) of the endometrial thickness can effectively rule out endometrial hyperplasia in postmenopausal women; if the thickness of the endometrial lining or "stripe" on ultrasound is less than 4 mm, it's extremely unlikely that the woman has hyperplasia.
What medications or therapies are used to treat heavy or prolonged menstrual bleeding (for example, tranexamic acid and CHC)? What are their contraindications? What do patients need to know about how to use them
1. Estrogen (ACUTE)
Contraindicated: hx of thrombosis or other coagulopathies
-progesterone needs to be taken after COCs - monophasic
-if flow does not stop w/in 48 hours of tx- return for evaluation
-use antiemetic since high estrogen cancause nausea
2. POP,CHC, IUD, Cyclic MPA, NSAIDS, Tranexamic acid (CHRONIC/LONG TERM)
-Contraindicated: pregnancy, ulcers (nsaids), blood clots (TXA), fibroid (IUD)
3. GnRH agonists - used when awaiting surgery for HMB
NOT FOR LONG TERM BLEEDING due to S/E and its expensive
4. estrogen/progesterone (ACUTE PROLONGED BLEEDING)
5. NSAIDS - used ideally for IDIOPATHIC HMB
6. TXA - 2nd line option for NONHORMONAL use
effective in combination with von willebrand disease
VTE CONCERN
S/E rare but include nausea and leg cramps
management goals for HMB
normalize bleeding
correct anemia
prevent cancer
restore quality of life
progesterone vs estrogen in resolving acute bleeding
progestogens are not as effective as estrogen in stopping acute bleeding but they are effective long term AFTER acute bleeding has been resolved
How can the levonorgestrel IUD be used for women with AUB?
After acute bleeding is under control, may initiate levonorgestrel IUD for long-term txt, causes chronic anovulation.
What other treatments are available for individuals diagnosed with AUB-E?
1. COCs, progestin therapy (depo, Nexplanon, mini pill), if testing shows anemia d/t
bleeding, iron therapy is recommended2. If medical therapy fails- surgical options: d&c, endometrial ablation, uterine artery
embolization, hysterectomy3. AUB-E dx of exclusion
How can COCs be used to stop prolonged or heavy bleeding?
1. monophasic COC admin 3x/daily should result in the ↓ of bleeding w/in 24 (up tp 48) hours.
2. COC is typically tapered to 2x/daily for 2 days, then 1 pill daily for 21 days of active pills followed by 7 days of placebo pills or no pills.
3. An alternative to the 21/7 cycle is an extended regimen of 84 days of monophasic COC followed by a 7 day pill-free interval.
4. When the bleeding stops, 2.5 mg of conjugated equine estrogen (Premarin) can be admin daily, followed by the addition of 10 mg of medroxyprogesterone acetate (Provera) during the last 10 days of therapy to initiate withdrawal bleeding.
Know the difference between primary amenorrhea & secondary amenorrhea
Primary amenorrhea is the failure to begin menses by age 16-but has normal secondary sexual characteristics. Any girl who has not reached menarche by age 15 or
who has not had a menses within 3 years of menarche should be evaluated
Secondary amenorrhea is defined as 3 months without a period with previously normal periods
AND for nine months in women with previous oligomenorrhea (infrequent periods, more than 35 days
What are the special assessment and diagnostic concerns of each type of amenorrhea including INITIAL WORKUP?
For Primary Amenorrhea
Initial workup:
1. No period by 15 - maybe no uterus or intact hymen, no ovaries, no vagina
2B.IF Secondary sex characteristics are present-
U/S first (see if they have a uterus), preg test as
indicated, refer to endocrinology
2A.If no secondary sex characteristics- HPOA is not working, =
draw an FSH/LH and refer
For Secondary Amenorrhea
1. May be caused by outflow tract obstruction, surgery on endometrium (ashmans syndrome)
or hormonal problem interfering with HPO axis at ANY LEVEL:
more cmmmon prolactinemia and tsh
less common hpo issue
NORMAL/HIGH estrogen w/ PROLONGED unopposed
exposure (this is VERY BAD)
1A.check TSH and prolactin first
1B.If normal, order a PCT
If normal prolactin but ABNORMAL TSH = thyroid disease
If normal TSH but ABNORMAL prolactin = refer to determine
Describe the assessment (history, physical examination, and diagnostic testing) and management options for women presenting with amenorrhea. Include patient education
1. History - lifestyle, exercise, meds, drug use, eating habits, s/s eating disorders, family hx of anatomic or genetic abnormalities.
- Other symptoms r/t differential
-Pregnancy - breast tenderness, nausea, vomiting
-Prolactinoma - headaches, visual field defects
-Thyroid problems - dry skin, constipation, etc.
2. Primary
-Physical exam - focus on
-Identifying maturation of secondary sex - tanner staging
-Establishing outflow tract patency - any bleeding from vagina
-Outflow tract abnormalities d/t abnormal development are rare - still consider
-If cervix not visible or vagina not patent → imperforate hymen-Obstructed bimanual exam → referral and f/u for possible vaginal septum or blind pouch
3. Secondary - check TSH and prolactin - if normal → PCT
4. Lab tests
1. Estrogen production - reliable measure of ovarian function
2. Serum estradiol: >40 = functioning ovaries, low may = ovarian failure or hypothalamic
amenorrhea
3. Progestogen challenge test
4. Endometrial thickness measurement
5. Serum FSH concentration - indirect measurement, lower level = normal function
6. If these tests = ovaries are producing estrogen and FSH normal = dx of chronic
anovulation
7. Serum prolactin -for dx of hyperprolactinemia w/ amenorrhea
8. Hyperprolactinemia
9. Serum prolactin
1. Not always w/ galactorrhea (nipple discharge)
10. Some meds can → elevated level (antidepressants, opiates, CCBs, and estrogens),
ask about meds
11. If w/ amenorrhea - more evaluation needed to r/o pituitary tumors and hypothalamic
mass lesions
5. Tx of choice is dopamine agonist
6. PCT +, no galactorrhea, and prolactin level normal = possibility of pituitary tumors
ruled out =dx is anovulation
1. Tx - progestogen for first 10 days each month or CHC
2. Evaluate for PCOS
7. Anovulation - management necessary, if not treated
What particular information does a progestin challenge test provide? What conditions would cause a person to be amenorrheic and then have a positive or negative progestin challenge test? (For instance: an amenorrheic woman has a NEGATIVE PCT but does not have an outflow tract problem…what can we deduce about the probable estrogen level?)
1. PCT+ (positive) 1. Withdrawal bleeding = functioning ovaries b/c bleeding only occurs if sufficient circulating estrogen is present *ANY amount of bleeding is a POSITIVE result*
-Withdrawal bleeding should occur w/in 7-10 days after d/c of progesterone and if outflow tract is patent
-Positive tests with: PCOS, Obesity
-A positive progestin challenge test: if their lack of menstruation is due to anovulation (lack of ovulation), meaning their body is producing sufficient estrogen but not releasing an egg
2. PCT - (negative)
1. Minimal/no estrogen → no endometrium → no flow
-Negative tests with: galactorrhea (milk unrelated to preg), prolactinemia, ovarian insufficiency
A negative progestin challenge test would indicate a problem with the uterine lining or outflow tract, like Asherman's syndrome, where the endometrium isn't adequately estrogenized, usually due to low estrogen levels from conditions like hypothalamic amenorrhea or premature ovarian failure
What conditions cause clinical hyperandrogenism?
PCOS-most common
Adrenal hyperplasia/tumor
Hyperthecosis
Androgen producing tumors
What are the clinical manifestations and health consequences of hyperandrogenic disorders? How will you tell these disorders apart in practice?
Clinical manifestations:
Gradual onset with slow progression
Symptoms such as- acne, alopecia, hirsutism, maybe over wt/obese (50%), “apple-shaped”, insulin resistance, polycystic ovaries, menstrual irregularity (HALLMARK feature) can lead to amenorrhea and/or prolonged anovulatory bleeding, difficulty achieving pregnancy is common
Tell apart: history, PE, and labs
i.e. negative TSH/Prolactin, higher free testosterone with s/s of hirsutism- PCOS (r/o all other causes)
What are the health consequences of hyperandrogenic disorders?
*Dyslipidemia- may result in metabolic syndrome (lipid level, fasting glucose for labs)
*Metabolic syndrome
*CVD
How do the cycles with hyper androgenic disorders differ from normal menstrual cycles?
Irregularity is a hallmark feature of PCOS-
Oligomenorrhea (infrequent periods) - most common presentation of overt menstrual dysfunction - cycle length 35-199 days
Amenorrhea - cycle >199 days
More significant endocrinopathies including more severe hyperandrogenemia, ↑ serum LH and cortisol and incidence of hyperinsulinemia
Polymenorrhea (frequent periods) - more rarely, may be iron def. anemia
Bleeding generally unpredictable. Can be heavy
Regular menses can occur w/ oligo-anovulation → subclinical menstrual dysfunction w/ regular menses but chronic anovulation
Either type may have unpredictable menses before bleeding d/t lack of premenstrual s/s = clinical indication of anovulation
What are the assessment, diagnostic, management considerations, and special risks faced by individuals with hyperandrogenic disorders?
1. Assess:
1. age of onset (Tanner stages, etc)
2. menstrual pattern, preg hx, miscarriage
3. obesity, hirsutism, seborrhea, acne, alopecia
4. complete medication hx
5. s/s of hirsutism and virilization- libido, muscle bulk, voice deepening, breast atrophy,
clitoromegaly
6. polydipsia or polyuria (glucose intolerance)
7. s/s hyperprolactinemia/pit tumor (galactorrhea, visual disturbances, HA)
8. s/s cushing syndrome (striae, mood chages, easy bruising or wt gain)
9. CVD and metabolic risk factors (smoking, hx HTN, dislipidemia, DM, CVD)
10. Fam hx
2. PE:
1. ht, wt, BMI, obesity degree, distribution of body fat (wt circumference of >35*)
2. VS esp BP
3. Skin- hirsutism, acne, alopecia, acanthosis
4. Thyroid
5. Breast (galactorrhea)
6. Cushings (moon face, hump)
7. Pelvic-clitoris, bimanual for uterine size, ovaries, and mass presence
3. Labs:
1. prolactin (mild elevations of prolactin are common in women with PCOS, may also identify women with prolactinoma-extremely rare)
2. TSH
3. lipids
4. 2-h OGTT
5. Progesterone days 20-24 of menstrual cycle
6. Serum 17-OHP- low-levels r/o congenital adrenal hyperplasia
7. Imaging: pelvic US, TVUS
endometrial biopsy (d/t risk of hyperplasia w/ unchecked estrogen), avoid routine adrenal
imaging
Special risks: endometrial cancer, metabolic syndrome, higher rate of CVD
How will you assess and diagnose PCOS?
Dx of EXCLUSION;
Rotterdam Criteria: must have 2/3 of following with no other cause identified:
1. Irregular menses (d/t irregular ovulation)
2. Multiple cysts in the ovaries (d/t unruptured dominant follicle)
3. Clinical hyperandrogenism (hirsutism, acne, alopecia, virilization)
FIRST LINE management for PCOS.
1.lifestyle modifications- weight loss, and exercise, metformin, hirsutism management- hair removal in women with PCOS who are not trying to conceive
COC is the best medical maintenance therapy to treat menstrual disorders and manage symptoms
progestin may be used for endometrial protection
letrozole should be considered as 1st line therapy compared with clomiphene
What red flags indicate the need for immediate referral in hyperandrogenic individuals?
Virilization: enlarged clitoris, deepening voice, increase in muscle mass, breast atrophy, increased aggression/libido -RED FLAG if they happen SUDDENLY.
Virilizing tumors: sudden onset of advanced PCOS symptoms concerning for adrenal or ovarian tumors
*should see endocrinologist immediately- virilization effects can be permanent
What should the assessment (history, physical examination, and diagnostic testing) of an individual with vulvar skin changes include?
Hx:
1. OLDCARTS
2. Prior self or prescribed txt and their outcomes
3. Concomitant systemic changes (ie lymphadenopathy of skin, perianal or oral mucosal disease)
4. Ask about all products used on the vulva and vagina
5. Increased risk of malignancy should be considered when women report a prior hx of high-risk HPV or close fam hx of skin malignancies
2. PE:
1. Conduct a thorough exam of vulva, beginning with keratinized skin areas (inguinal folds, mons
pubis, and labia majora), followed by partially keratinized (labia minora, clitoral hood, and posterior fourchette)
2. Palpation for lymphadenopathy
3. inspection of scalp, eyes, nasal mucosa, and oral mucosa
4. Examination of the skin folds
5. Spec exam to identify involvement of vaginal mucosa
3. Dx: 1. Selective testing may aid dx- ex: tests for candida, STIs, microscopy for scabies or vaginal
pathogens
2. Microscopy in all women with symptoms
3. Biopsy with any atypical, nonresponsive findings
How is lichen sclerosis managed?
lichen sclerosis: chronic mucocutaneous disorder that is characterized by inflammation, epithelial thinning, and depigmentation, and dermal changes-often include agglutination of labia minora, can be progressive or relapsing and remitting.
Most often genital, occasionally identified in other body areas, including trunk neck, forearms, axillae, and under the breasts, most often occurring on tissue that has undergone trauma
Dull, nonspecific vulvar irritation, whereas progressive disease often manifests with severe pruritus, burning, and associated dyspareunia; perianal symptoms, including pruritus ani, painful defecation, and anal fissures may also occur
Goals of tx: s/s relief, reversal of agglutination, prevention of further architectural distortion w/ loss of function, and prevention of potential malignant changes
First line tx - high or very high potency topical steroid ointment - clobetasol propionate 0.05%; 3 month tapered dosing common
Yearly vulvar exam
Atypical or nonresponsive to tx - referral to specialist

How would you recognize and manage Cervical polyps?
Cervical polyps:
may be single or multiple, usually <3cm in diameter
lobular/pear-shaped, stalk arises from cervical canal and size varies
1. Often asymptomatic and incidentally dx
2. postcoital or intermenstrual bleeding
Management:
1. SDM- observation (education to report irregular or postcoital bleeding) or removal for histology (indications are symptoms such as irregular or postcoital bleeding, increased discharge, larger than 3cm, necrotic, friable, irregular
color)
2. if stalk is clearly visible, removal is simple and in office. GRab polyp, clamp and apply pressure for 3-5 minutes, twist forceps to remove polyp. May bleed-can cauterize

How would you recognize and manage Nabothian cysts?
small white/yellow raised areas
retention cysts of endocervical glands are a normal variation
leave them alone - harmless