Clinical Skills: Local Anesthesia and Laceration Repair
1/80
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
81 Terms
Local Anesthesia
Blocks the conduction of nerve impulses
Effects are reversible and nonspecific
Can act on sensory nerves, temperature sensation, pain, touch, pressure, and motor
Most common forms of local anesthesia
topical, direct infiltration, regional blocks
Why anesthesia burns
Anesthetic solution are acidic
Once injected the pH normalizes
Buffer with bicarbonate- limits shelf-life, degrades epinephrine
Epinephrine decreases pH which makes burning worse
Epinephrine is included in anesthesia for
Decreases blood flow
Reduces systemic absorptions
Shortens onset
Extends duration of action
Doubles the duration of anesthesia with Lidocaine
Limited system absorptions allows for greater amounts to be used without a fear of toxic potential
Reasons why epinephrine should not be included in anesthesia
Decreases blood flow
Not be used for regions of the body supplied by a single vascular source
May cause necrosis
Regions of the body that can be affected by necrosis from epinephrine
Fingers, nose, penis, and toes
pinna of the ear can also be affected
Anesthetic in infection
Anesthetic solutions work best at physiologic pH
They are less effective in infected tissues than in healthy tissues
This is due to the infected tissue's metabolic acidosis from the infection, which decreases the tissue pH
Maximum amount of anesthetic calculation
dose (mg/kg) x (weight in kg/10) x (1/concentration of local anesthetic) = mL lidocaine
Maximal dose for lidocaine without epinephrine
3 mg/kg
Maximal dose for lidocaine with epinephrine
7 mg/kg
Anesthesia toxicity is due to
decreased clearance
Decreased hepatic blood flow and reduced enzyme function
Anesthesia toxicity patient considerations
those undergoing general anesthesia, taking propranolol, have congestive heart failure, cirrhosis, or hypothermia
Maximum dose of lidocaine for most average patients
30 cc of 1% Lidocaine
Topical anesthetic agents
benzocaine and lidocaine
Injectable anesthetic agents
lidocaine, bupivacaine
Local anesthetia indications
Elimination of pain with therapeutic modalities
Repair lacerations and minor surgery
Incision and drainage of abscesses
Removal of lesions, biopsies, nail removal
Contraindications to local anesthesia
True allergy
Severe liver disease
Severe renal disease
Severely unstable blood pressure
Untreated hyperthyroidism
Severe CAD
Epinephrine in local blocks
Narrow angle glaucoma
Anesthesia complications
Vasovagal reaction of patient due to injection fear
Local anesthesia complications
Not common
Bruising, edema, prolonged nerve damage
Systemic anesthesia complications
Hypotension, bradycardia, CNS depression, stimulation
How to prepare the patient for anesthesia injection
Talk to the patient
Reassure the patient
Have the patient supine
Engage in conversation to distract
Encourage them to take deep breaths
Reassure them through the procedure
May need conscious sedation for anxious patients or children
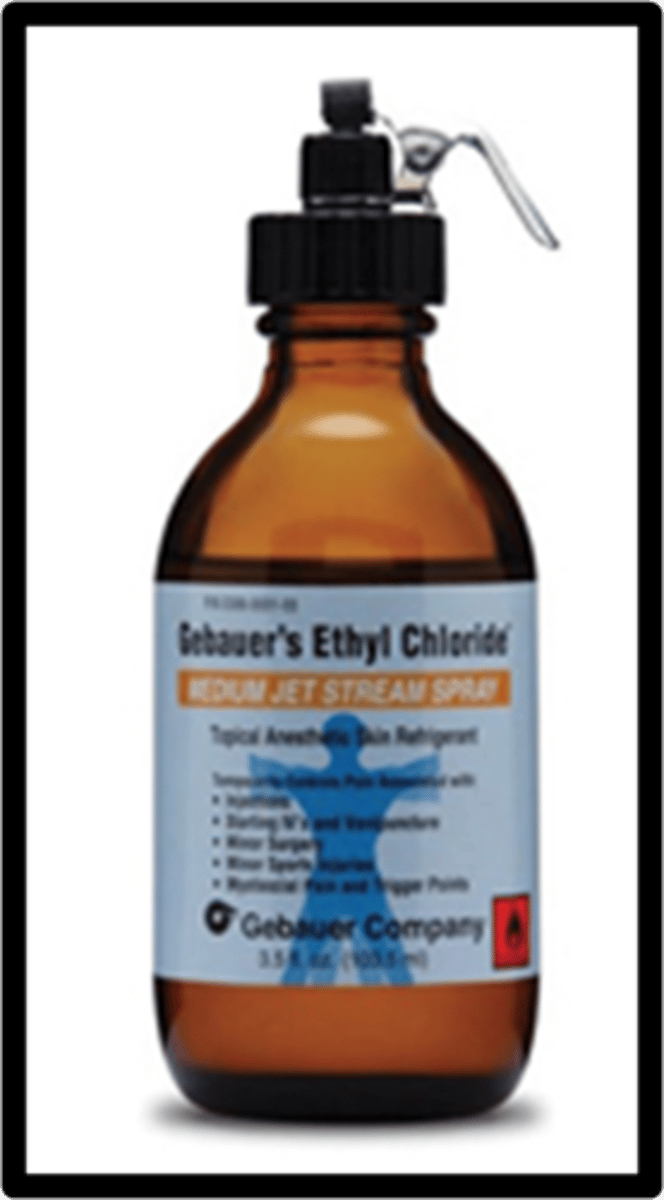
Cryo-anesthetics
Provide short period of decreased pain sensation
Ice, ethyl chloride, trichloromonofluoromethane,
Can use before an injection
Use for curettage of superficial lesion
Can burn if sprayed on skin too long
Topical anesthetics
Apply topically to mucous membrane or skin/wound
Best for highly vascular sites (face and scalp)
Takes approx. 15-20 minutes
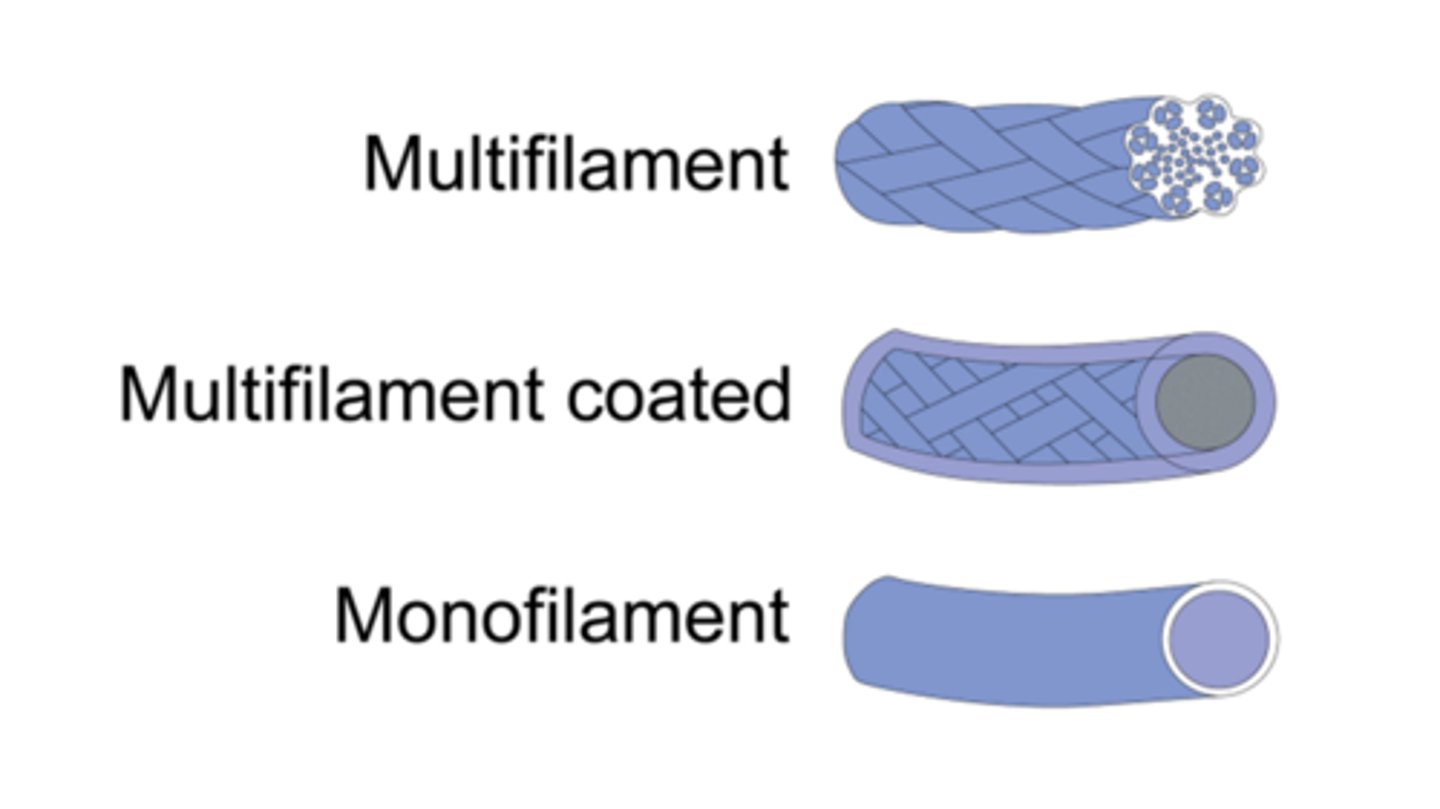
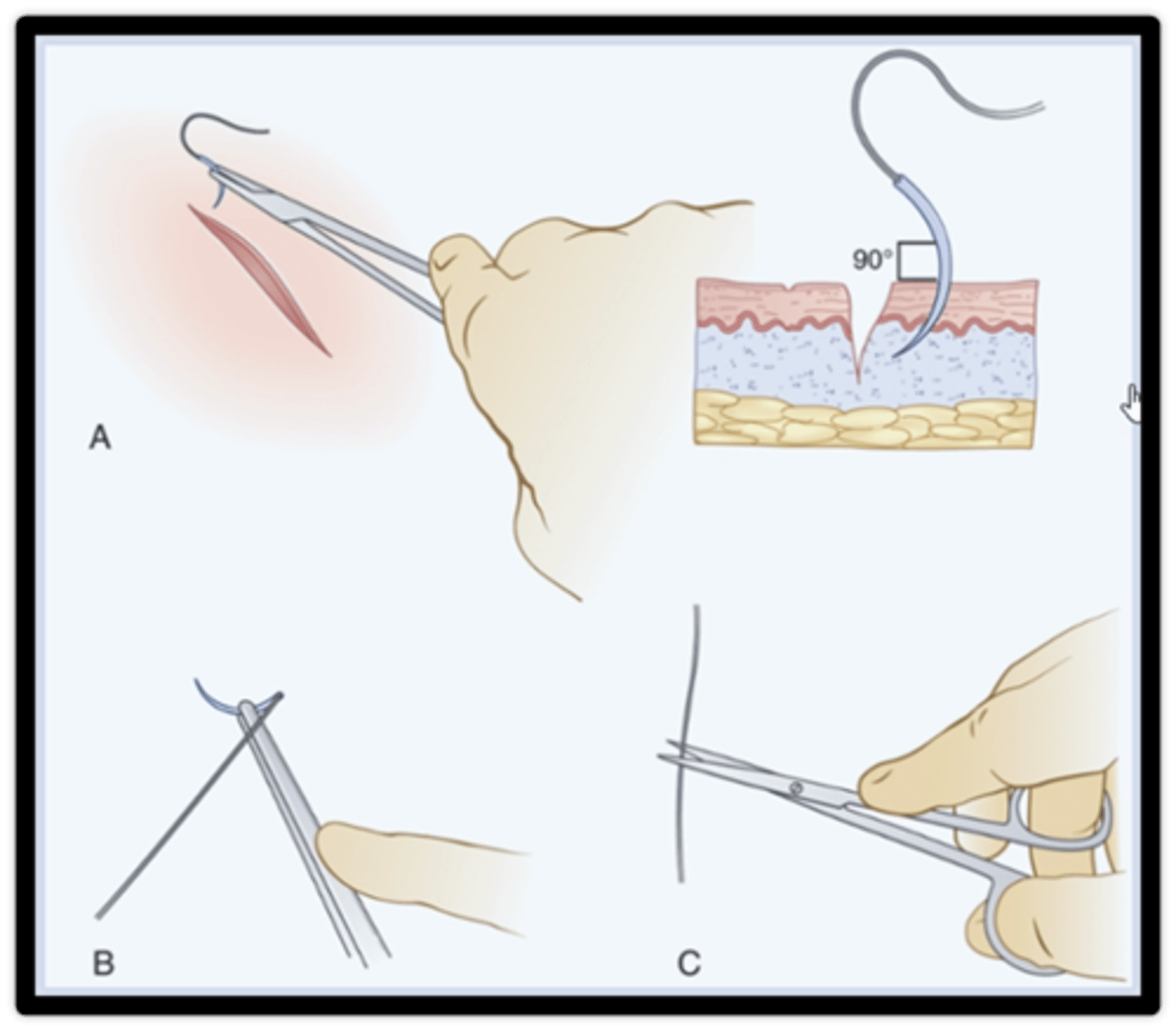
Injection anesthesia
injected into the wound or surrounding tissue
use small 27-g needle
slowly inject
burns

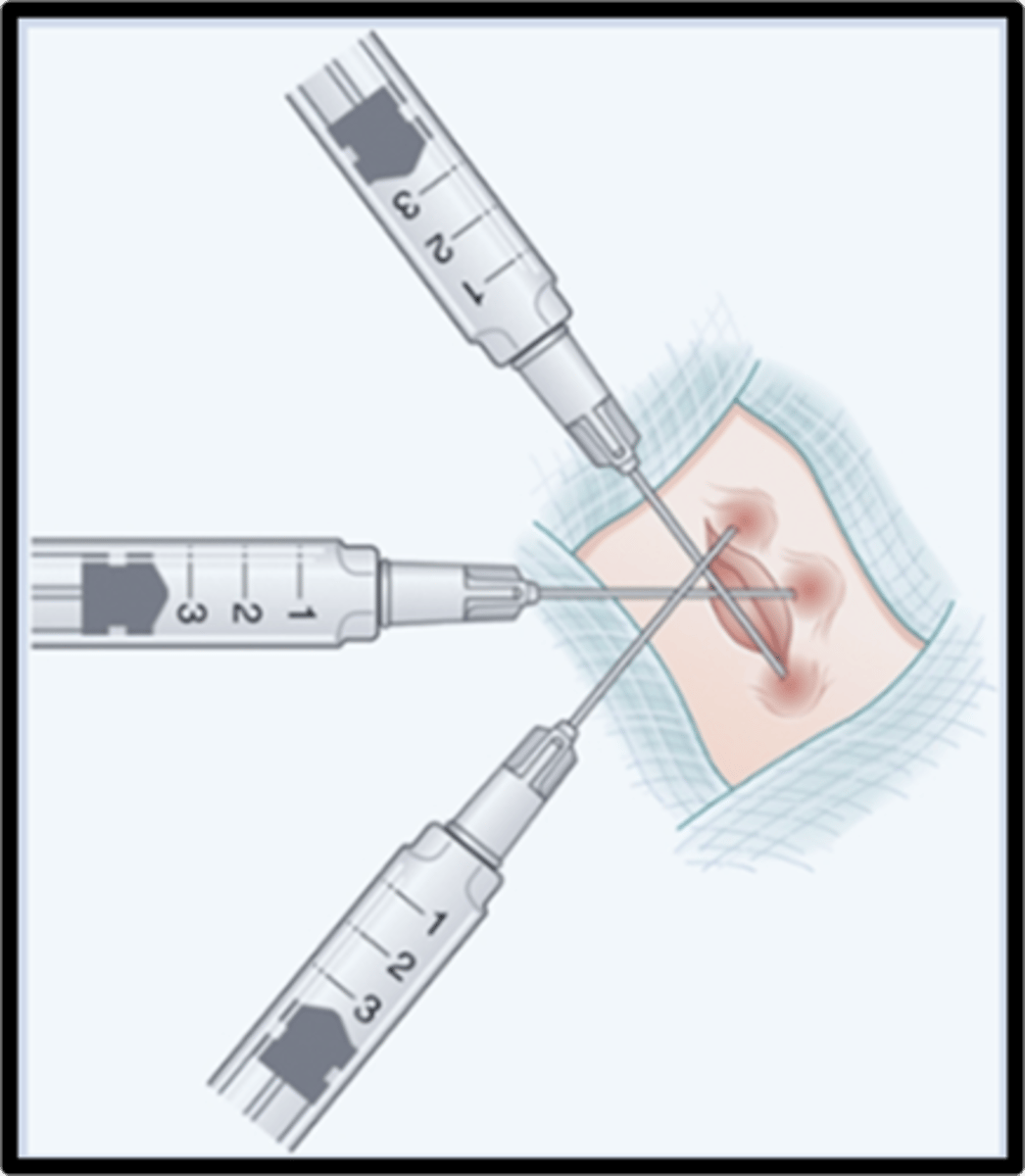
Direct infiltration of wound
1.Enter from inside the wound
2.Start on side where innervation originates
3.Aspirate to ensure not in vessel
4.Inject then withdraw
5.Move the needle around the wound repeating
6.Repeat until all edges of the wound are anesthetized
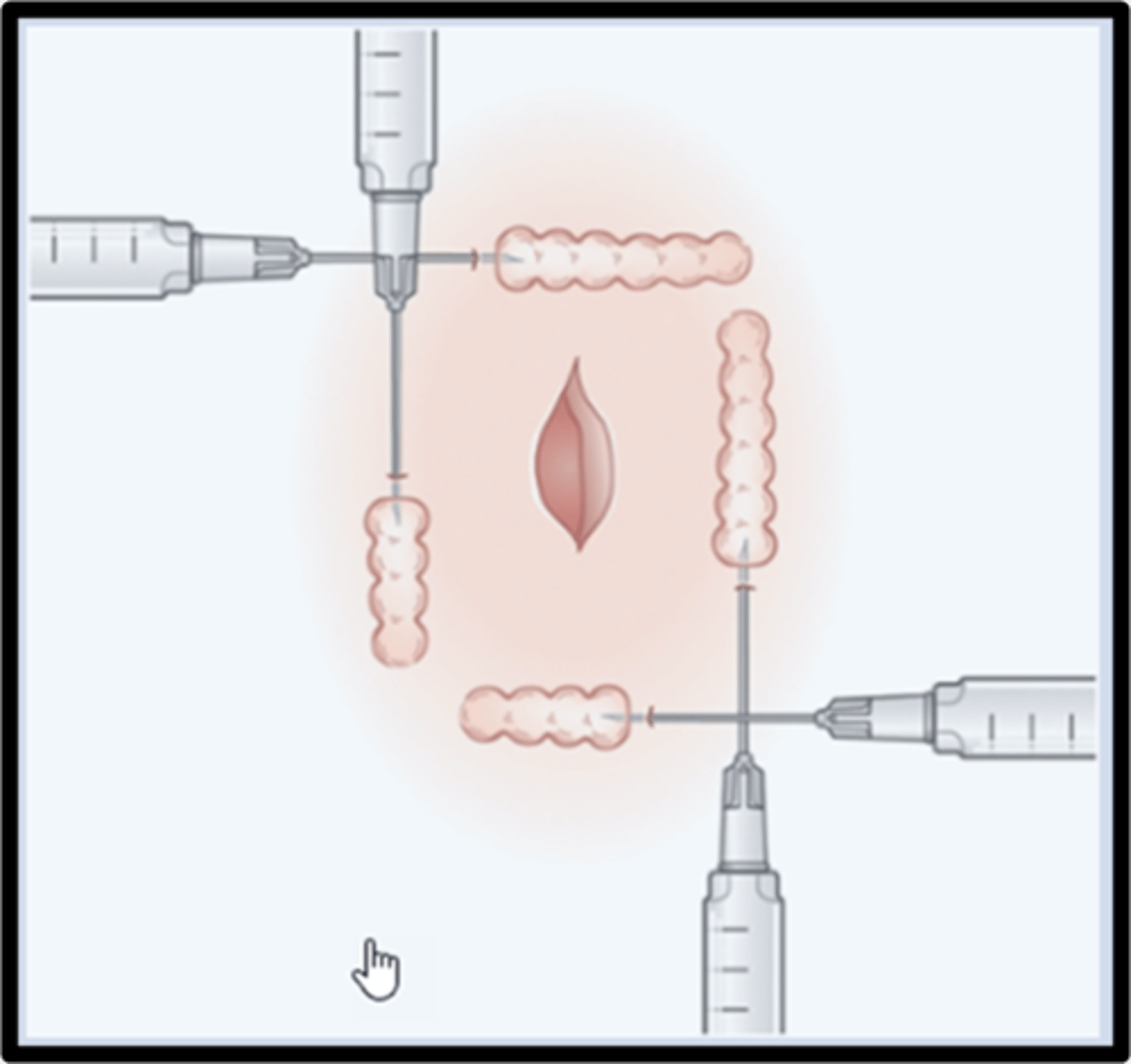
Field block
Use when larger laceration and grossly contaminated wound
Use a 25 - 27-g needle, 11/4 to 2 inch needle
Insert needle and run parallel to the skin up to the hub
Slowly inject as you pull back
Repeat 3 additional times until you have squared the field
Digital block
Recommended for procedures distal to the mid-proximal phalanx of the digit
Nail avulsion, paronychial drainage, repair of lac of digit
Lidocaine 1% w/o epi
Digital block: dorsal injection
1.Inject just distal to the web space in the middle of the digit. (lateral and medial sides)
2.After aspirating, inject 0.1 mL of anesthetic locally into the epidermis
3.Advance the needle to the bone, withdraw slightly, and then move dorsally, where 0.5 mL of anesthetic is injected after aspiration
4.Withdraw the needle again to the midline, advance to bone, and move ventrally, where another 0.5 to 1 mL of anesthetic is injected after aspiration
5.Withdraw the needle and repeat the whole procedure on the other side of the digit
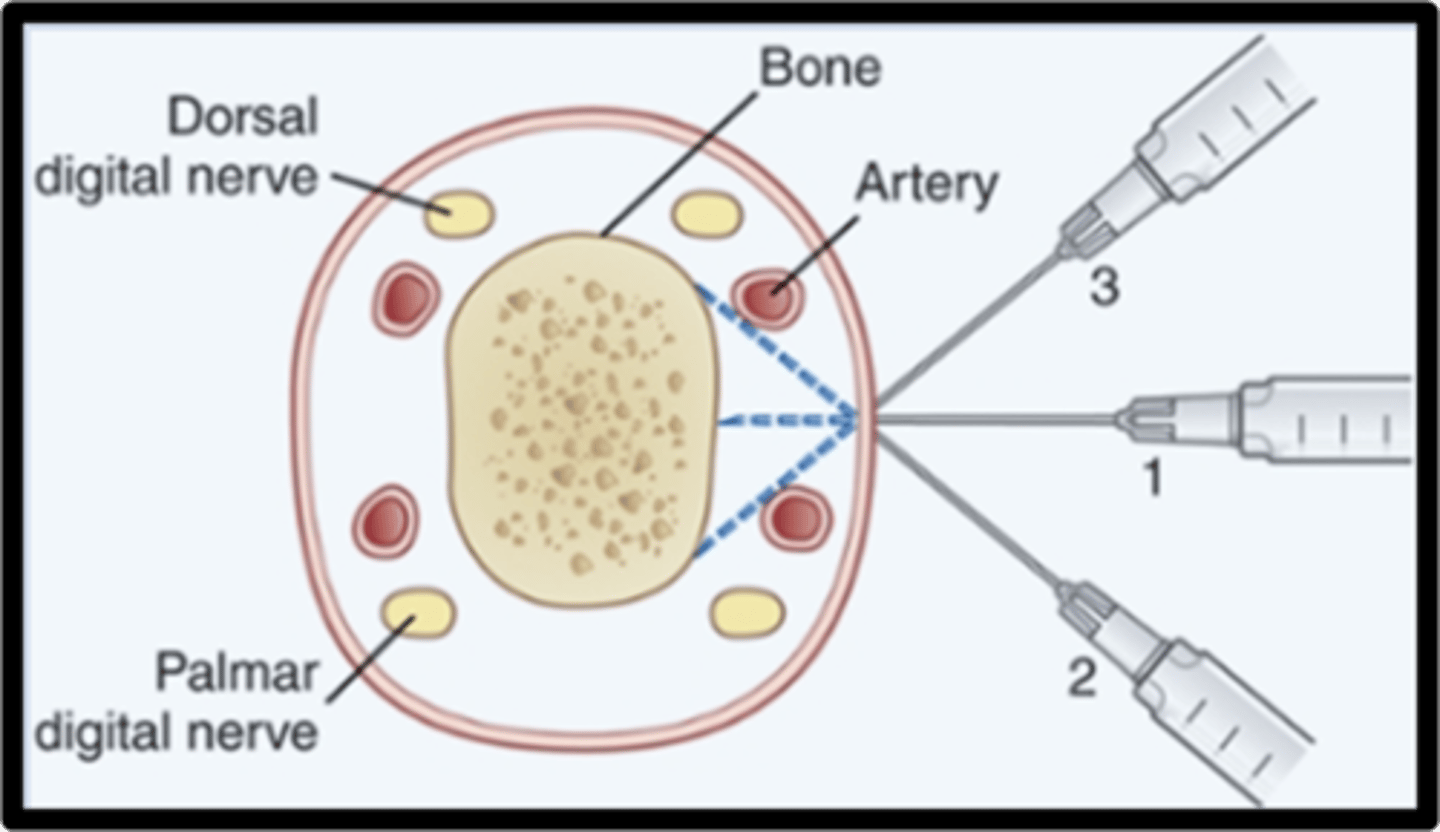
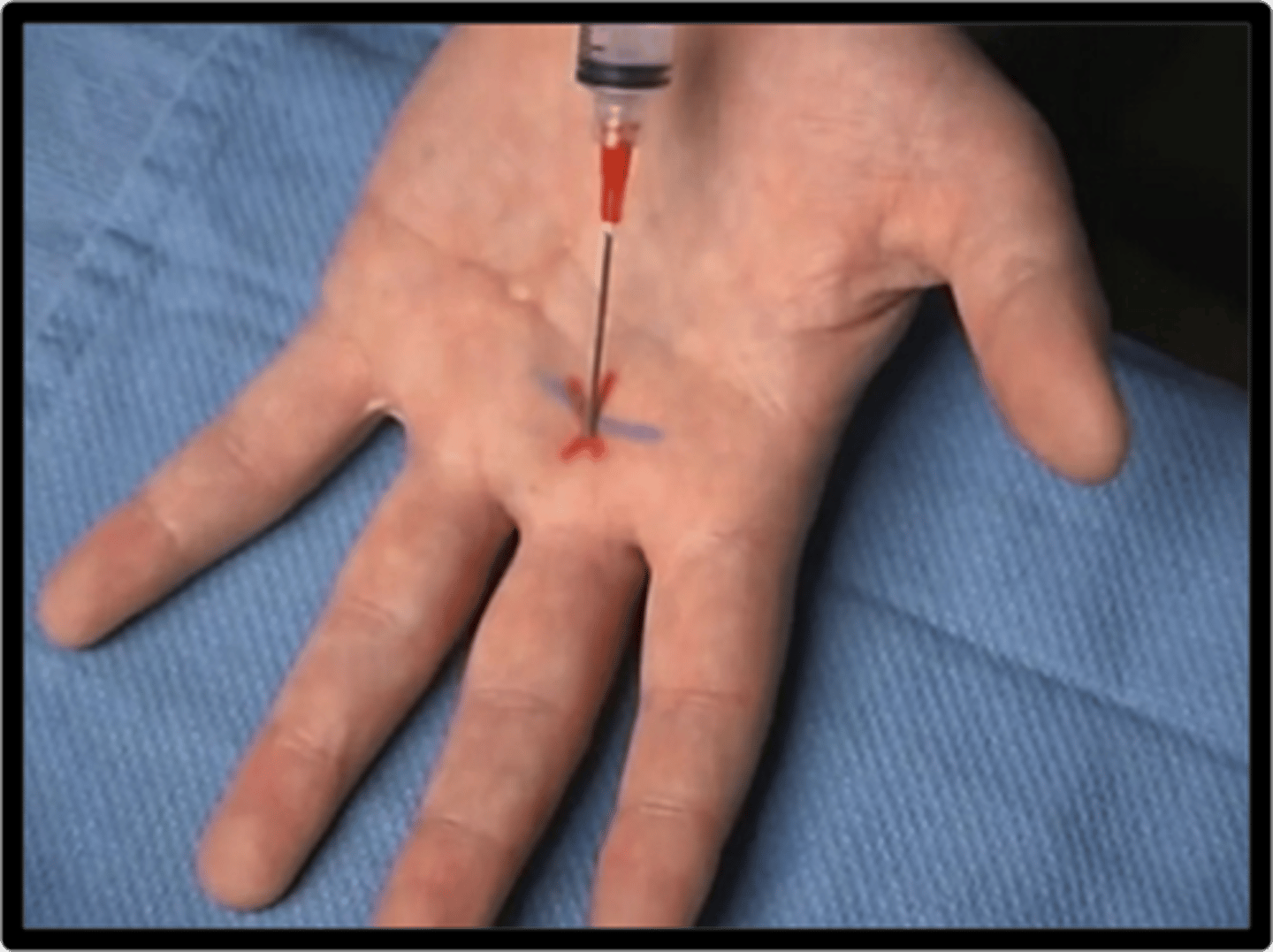
Digital block: palmar inject
1.Hand placed in supinated position
2.Needle is introduced distal to the distal crease of the palm lined up with midline of the digit
3.After aspiration, inject 1 to 2 mL of anesthetic
Wound closure considerations
Reapproximate wound edges to facilitate wound healing and reduce the likelihood of infection
Timeframe for wounds to be closed within
18 hours of injury
Wound closure indications
time required for wound healing
likelihood of infection
amount of scar tissue
Repair loss of structure and/or function
Improve cosmetic appearance
Wound closure contraindications
Contaminated wounds
Presence of foreign bodies
Tendon, nerve, and/or artery involvement
Potential complications of wound closure
Infection
Scarring, including keloid formation
Loss of function and structure
Loss of a cosmetically desirable appearance
Wound dehiscence
Tetanus
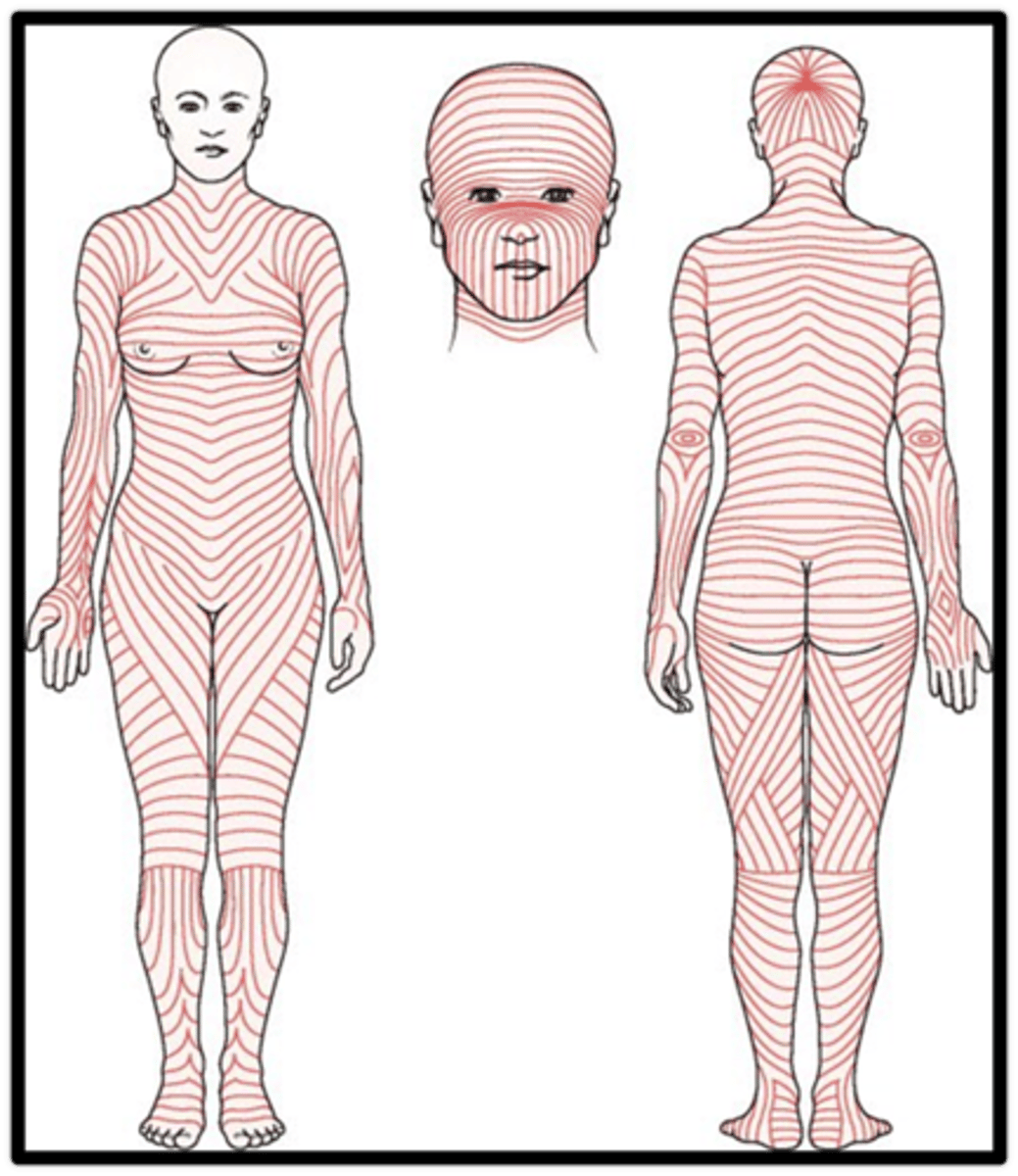
Langer line
Lacerations that run parallel to these lines naturally reapproximate the skin edges
Lacerations that run at right angles to the tension lines tend to gape apart
Clean wounds
Incisions made during a surgical procedure in which aseptic techniques were followed, without involvement of the gastrointestinal, respiratory, or genitourinary tract; likelihood of infection is less than 2% and warrants routine primary closure
Clean-contaminated wounds
Similar to clean wounds, except that the gastrointestinal, respiratory, or genitourinary tract is involved
Contaminated wounds
Similar to clean and clean-contaminated, except there is gross spillage (e.g., bile, stool); traumatic wounds fall into this category
Infected wounds
Established infection before wound is made (e.g., incision and drainage of an abscess) or heavily contaminated wounds (e.g., gross spillage of stool)
Wound closure classification: primary intention
All layers are closed
Best chance for minimal scarring
Usually performed in clean and clean-contaminated wounds
Wound closure classification: secondary intention
The deep layers are closed, whereas superficial layers are left open to granulate on their own from the inside out
Often leaves a wide scar and requires frequent wound care, consisting of irrigation and assorted types of packing and dressings
Prolonged process
Reasons for use include excessive tissue loss and infection
Used for infected and contaminated wounds
Wound closure classification: third intention or delayed primary intention
The deep layers may be closed primarily, whereas the superficial layers are left open until reassessment on day 4 or 5 after initial closure, at which time the wound is inspected for signs of infection
If it looks clean and has begun to granulate, it is irrigated and closed
If it looks as if it may be infected, it is left open to heal by secondary intention
These wounds often arise initially from contaminated wounds
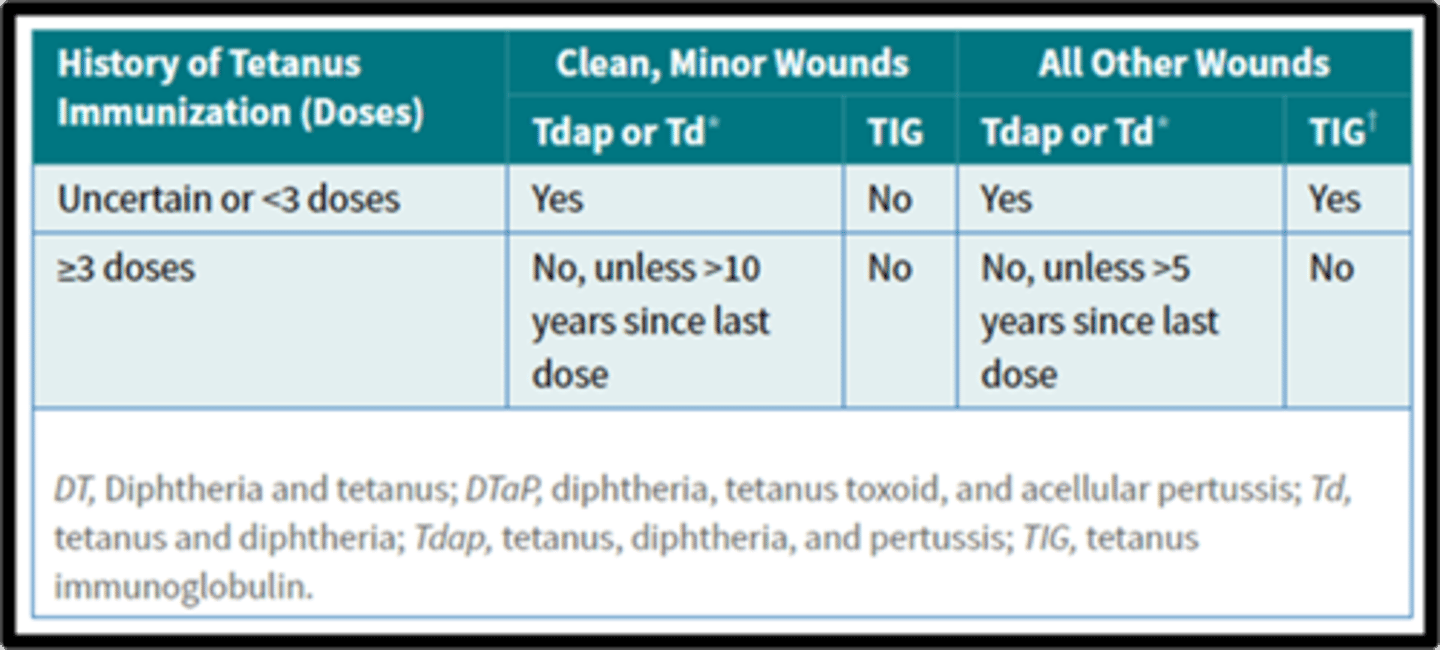
Patient preparation for wound closure
History
Physical Exam
Tetanus Vaccination History
Absorbable suture types
Gut, Monocryl, Vicryl
Absorbable suture absorption time is affected by
Material
Location of suture
Patient factors
Absorbable sutures are commonly used for
Deep tissue and tissues that heal rapidly
Small bowel anastomosis
Urinary or biliary tracts
Tying off small vessels near the skin
Closing of skin
Nonabsorbable suture types
silk, nylon, polypropylene
Nonabsorbable sutures are used to provide
long-term tissue support
Remain walled off by the body's inflammatory processes
Nonabsorbable sutures are used for
tissues that heal slowly
Fascia
Tendons
Closure of abdominal wall
Vascular anastomoses
Monofilament suture types
nylon and polypropylene
Monofilament sutures
Passes through tissue more easily than does braided suture. Disadvantage- has less tensile strength than a multifilament suture
Multifilament suture types
silk and ethibond
Multifilament sutures
Better flexibility, Disadvantage would be that it may harbor organisms more easily within the braid
Suture size
denoted by the number of zeros, and increases in number as the diameter of the suture decreases
Example 7-0 is smaller than 1-0
Natural suture material
made of natural fibers (e.g. silk or catgut). They are less frequently used, as they tend to provoke a greater tissue reaction
Natural suture materials commonly used for
securing surgical drains
Synthetic suture materials
comprised of man-made materials (e.g. PDS or nylon). They tend to be more predictable than natural sutures, particularly in their loss of tensile strength and absorption
Monofilament suture
a single stranded filament suture (e.g. nylon, PDS*, or prolene). They have a lower infection risk but also have poor knot security and ease of handling
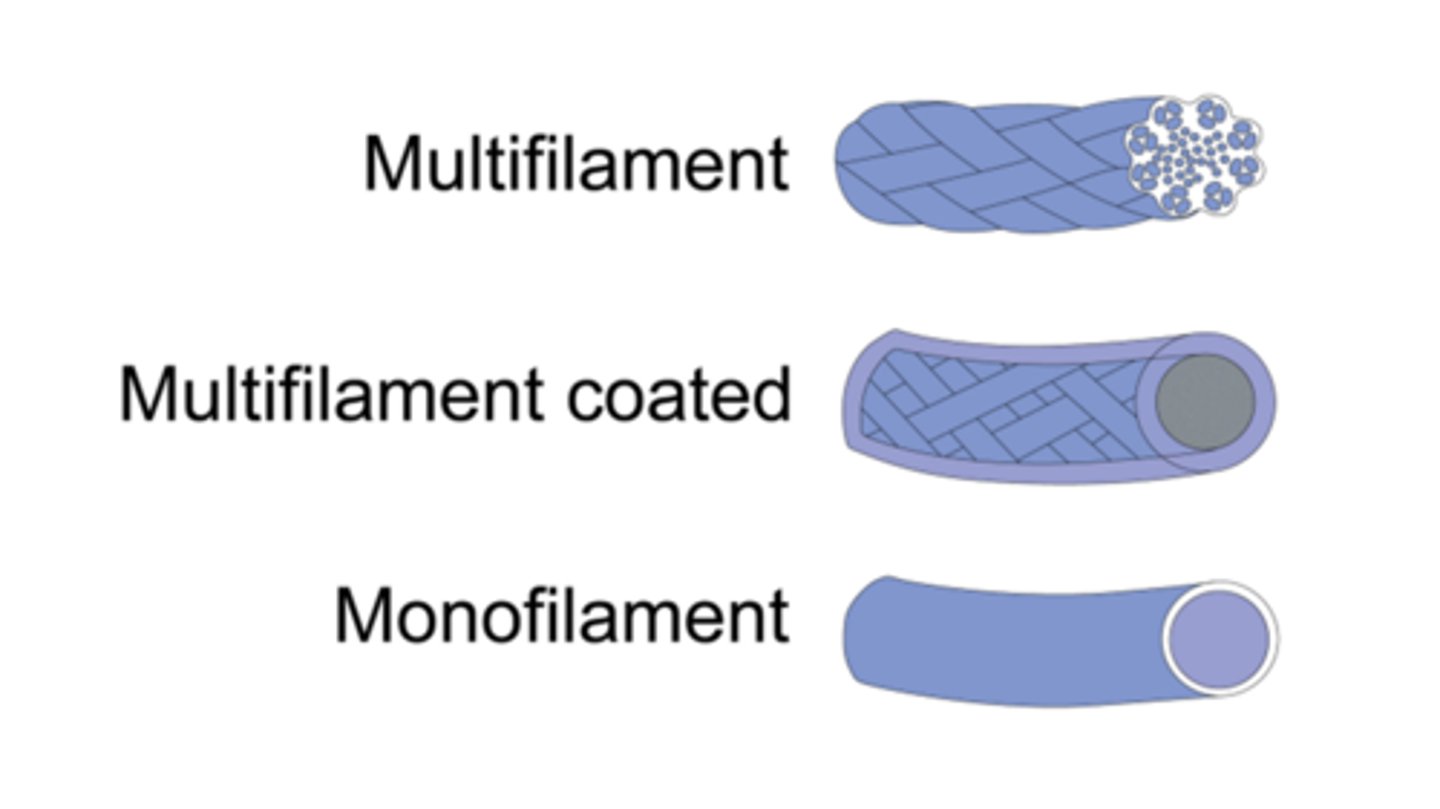
Multifilament suture or braided suture
made of several filaments that are twisted together (e.g. braided silk or vicryl). They handle easier and hold their shape for good knot security, yet can harbor infections
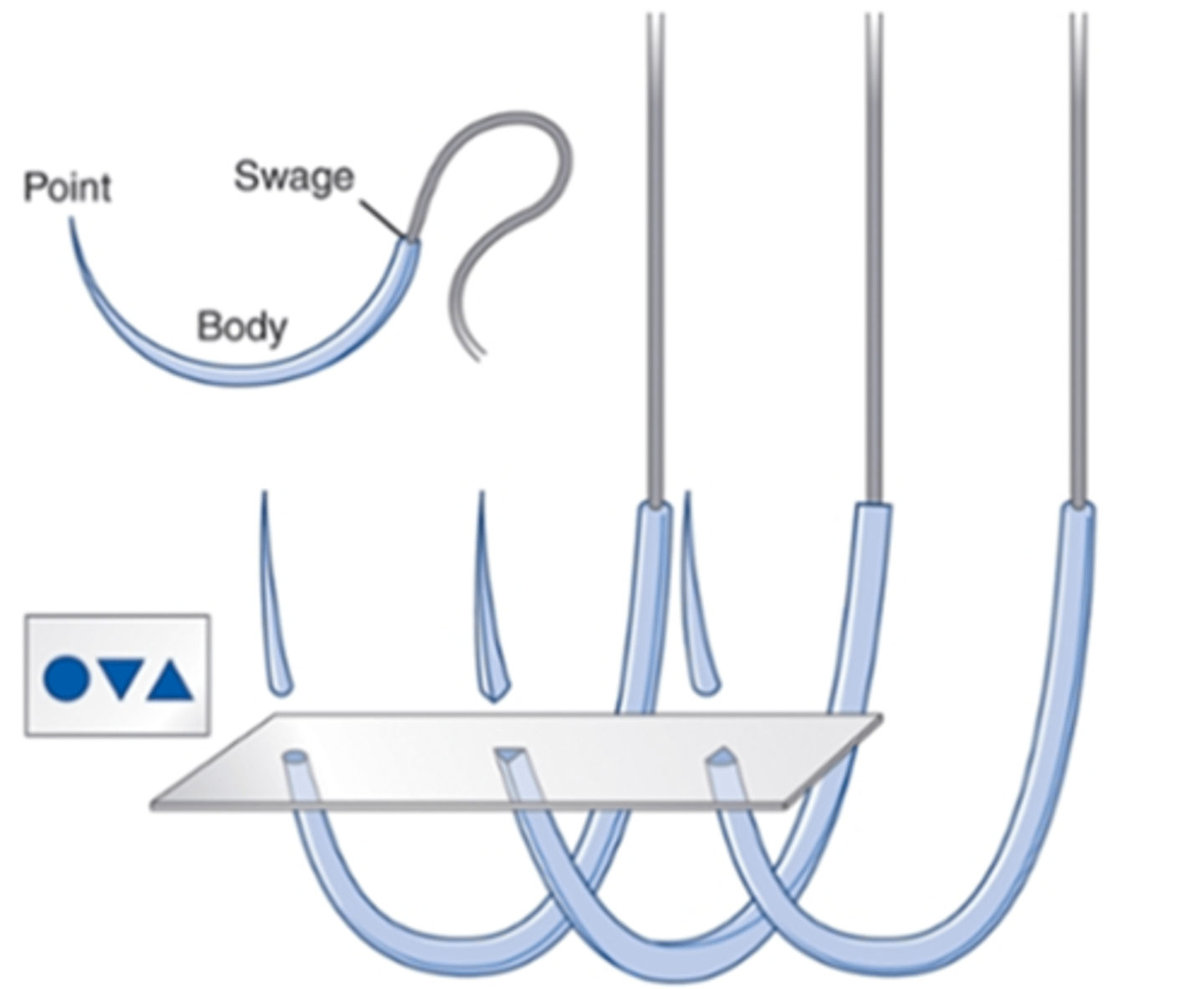
Ideal suture needle
Rigid enough to resist distortion
Flexible enough to bend before breaking
Slim as possible to minimize trauma
Sharp enough to penetrate tissue with minimal resistance
Stable within a needle holder to permit accurate placement
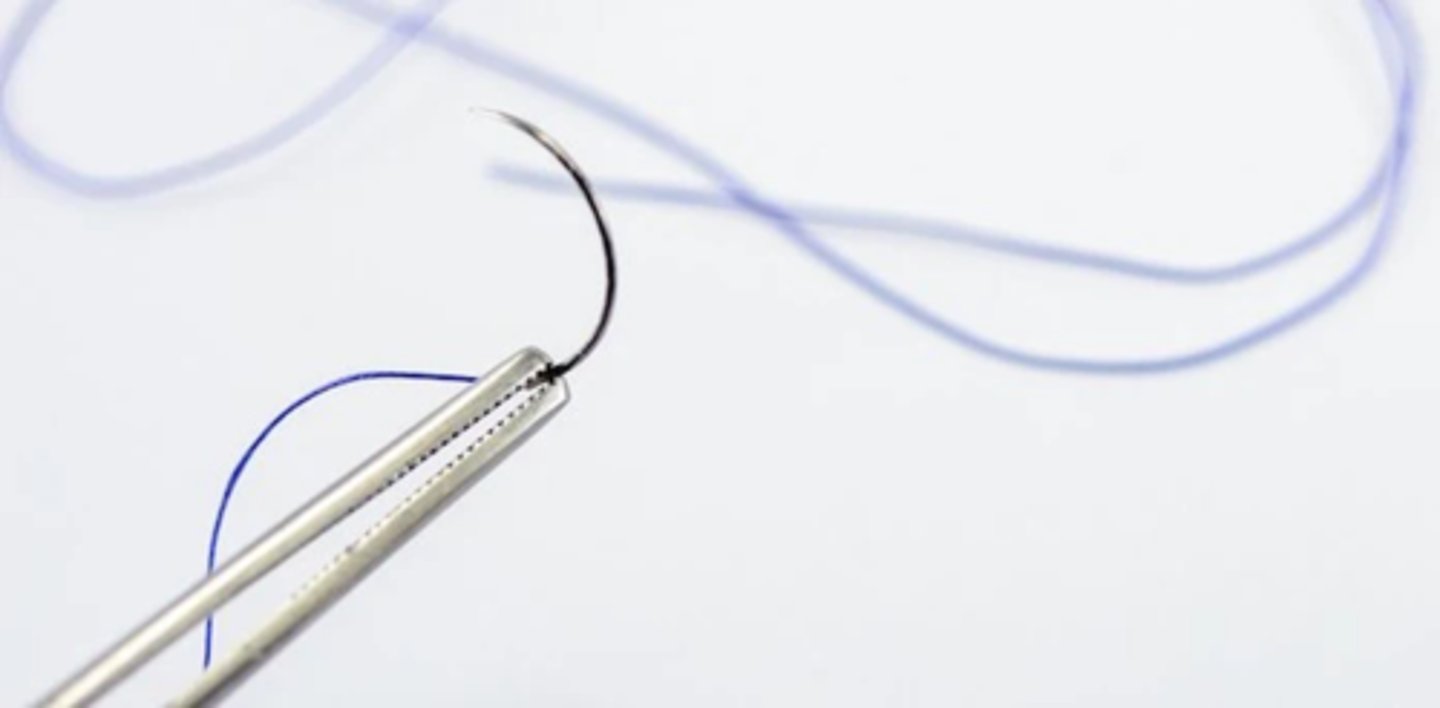
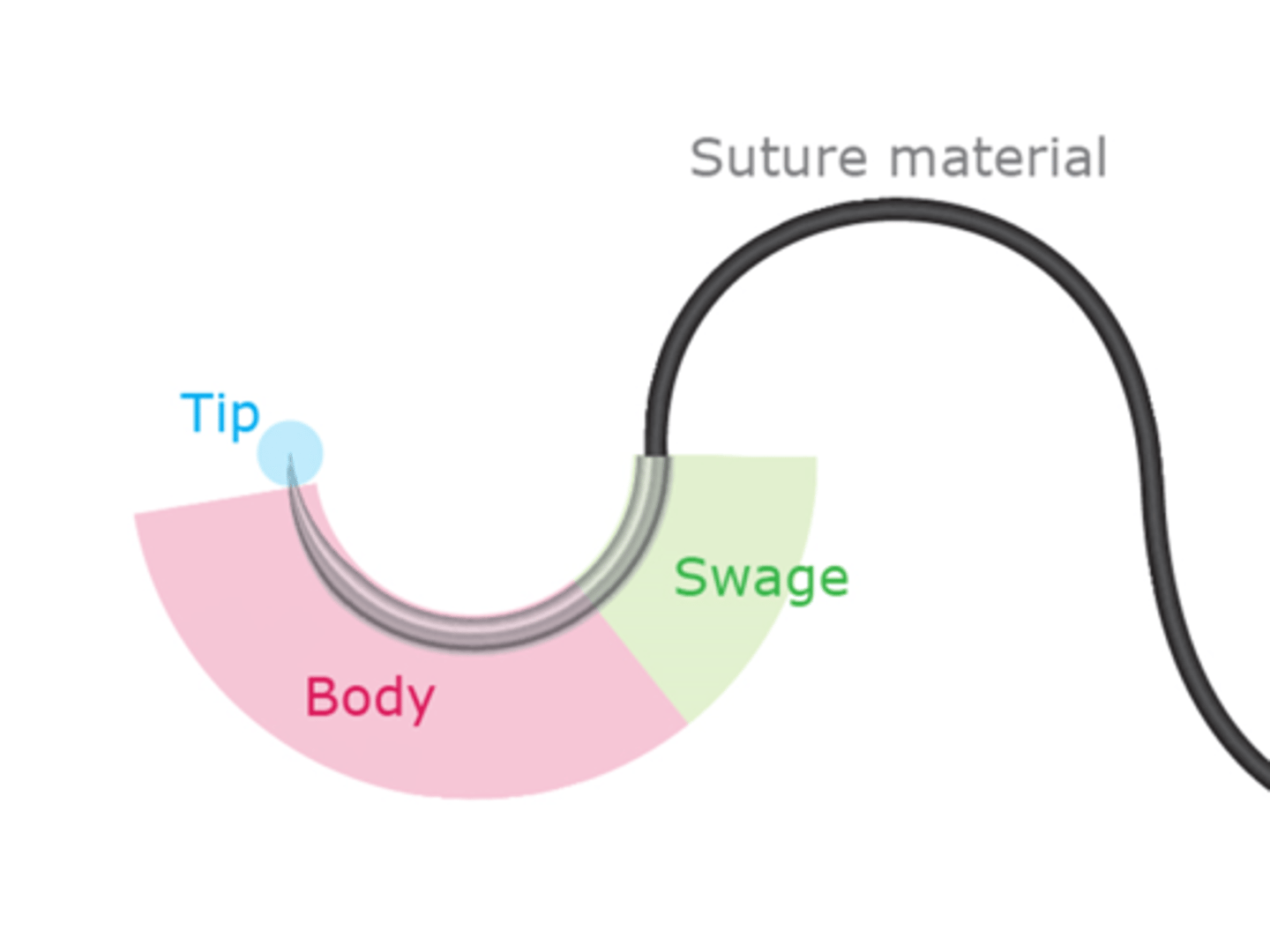
Parts of a suture needle: swage
connects the needle to the suture
Parts of a suture needle: body or shaft
the region grasped by the needle holder
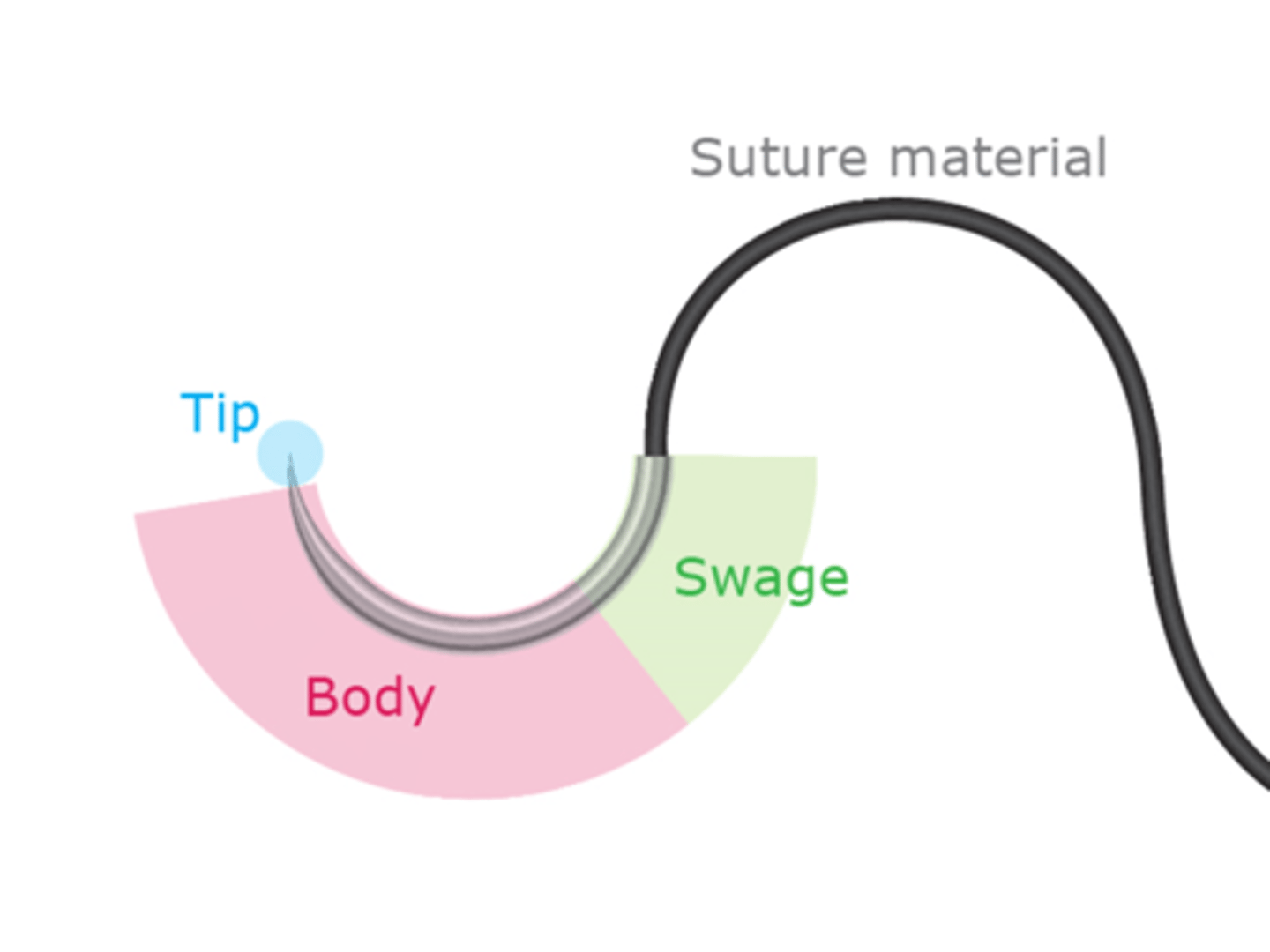
Parts of a suture needle: point
pierce the tissue
Suture needle body types: round (taper)
Friable tissue such as liver and kidney
Dilates rather than cuts
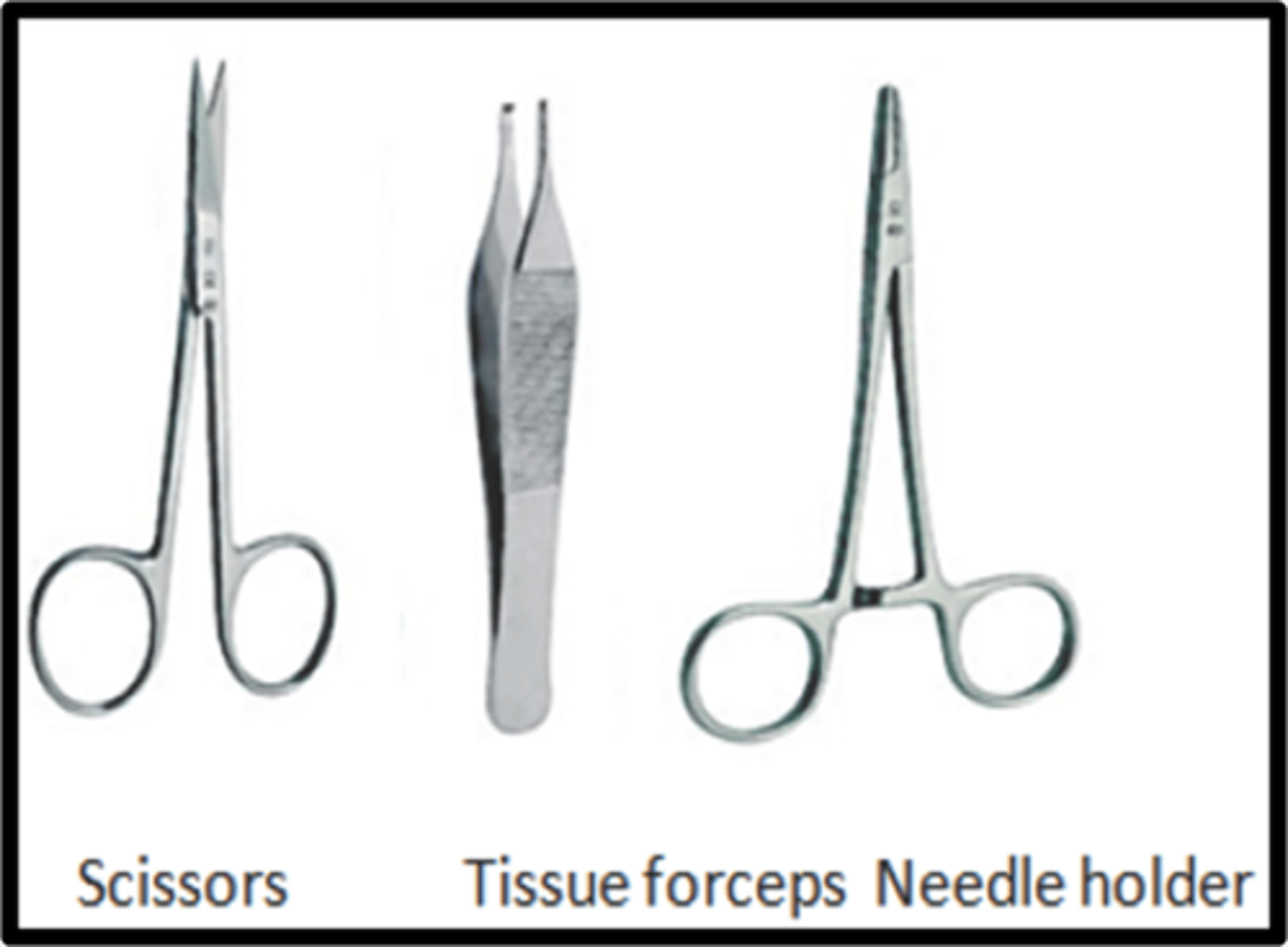
Suture needle body types: reverse cutting
Reverse cutting needles have a cutting surface on the convex edge
Cuts rather than dilates
Ideal for tough tissue such as tendon or subcuticular sutures
Reduced risk of cutting through tissue
Ideal for skin
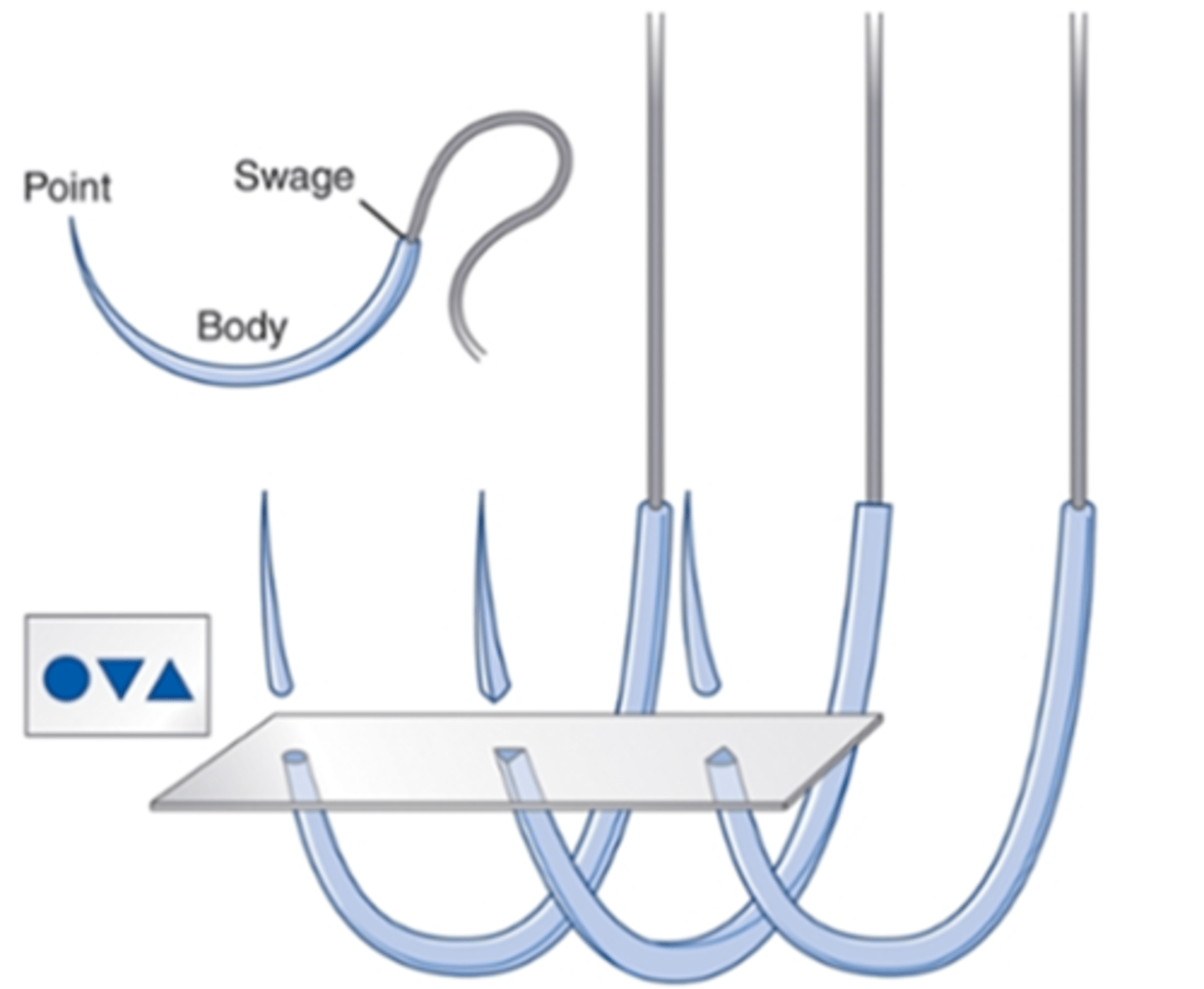
Suture needle body types: cutting
Triangular in shape
3 cutting edges to penetrate tough tissue such as the skin and sternum
Have a cutting surface on the concave edge
Cuts rather than dilates
Creates weakness allowing suture tear out
Suture needle point types: sharp
Pierce and spread tissues with minimal cutting
Used in areas where leakage must be prevented
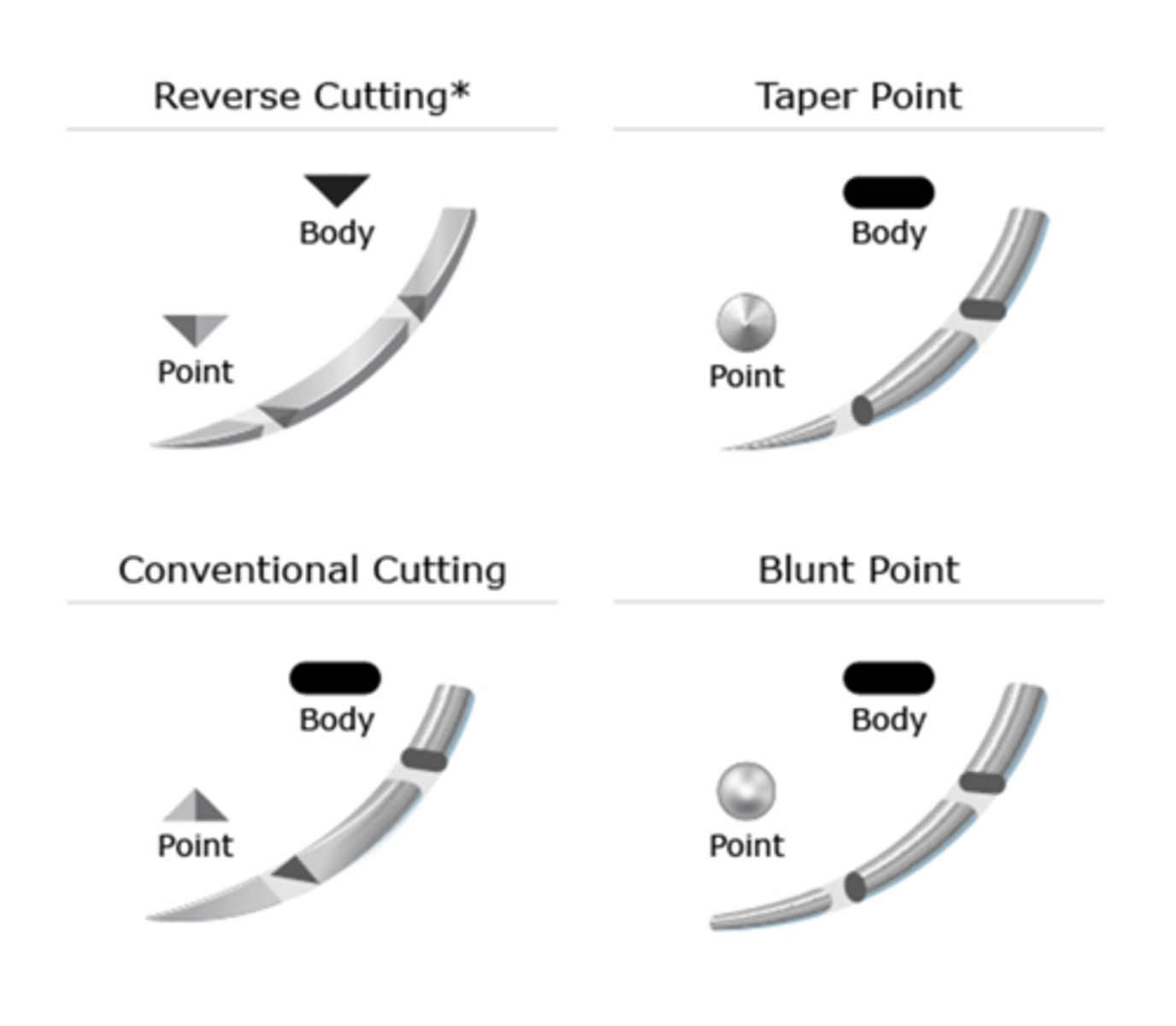
Suture needle point types: blunt
Used for abdominal wall closure, and in friable tissue,
Can potentially reduce the risk of blood-borne virus infection from needlestick injuries
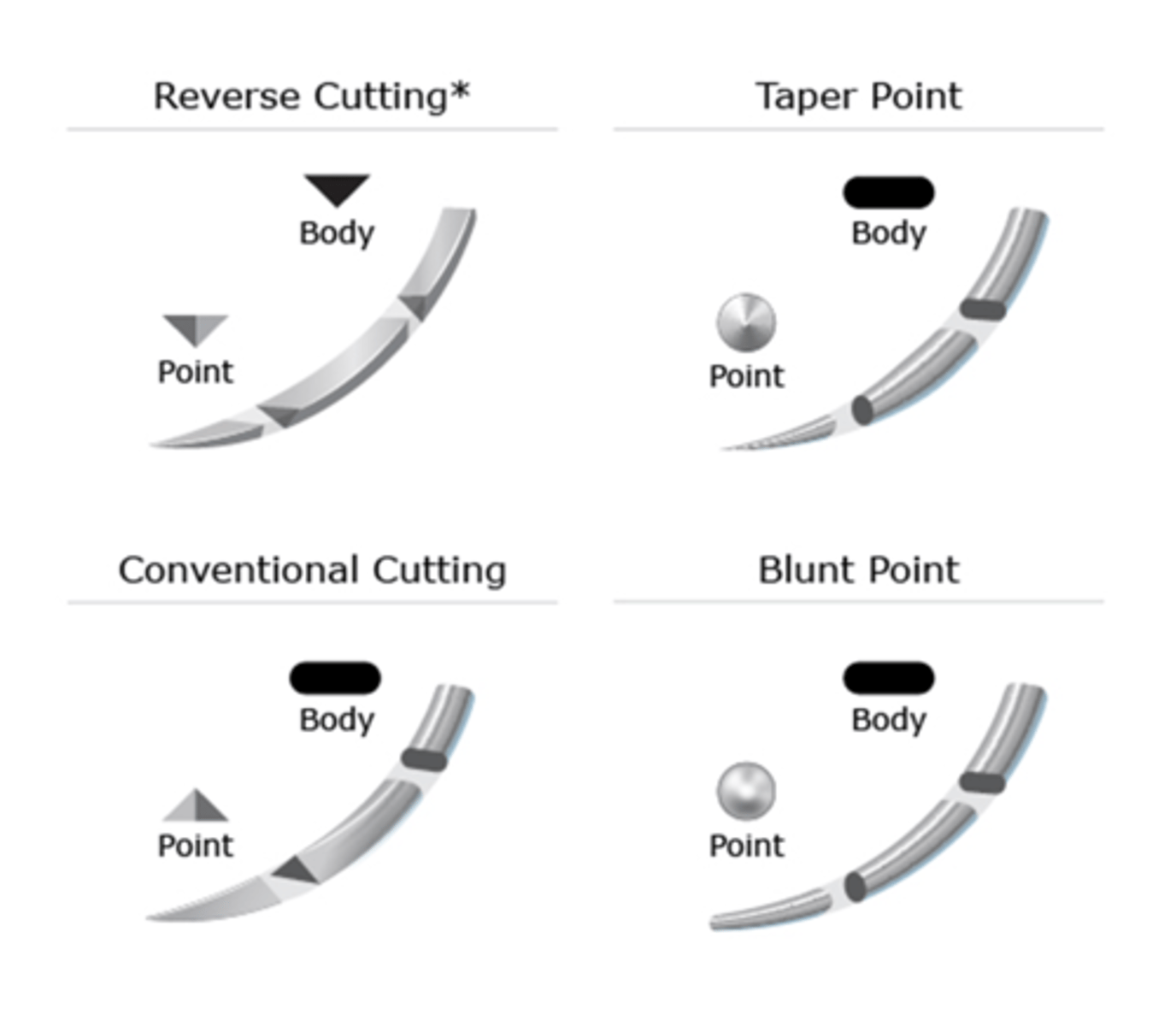
Needle shape
vary in their curvature
Are described as the proportion of a circle completed
Most common needle curvatures used
¼, ⅜, ½, and ⅝
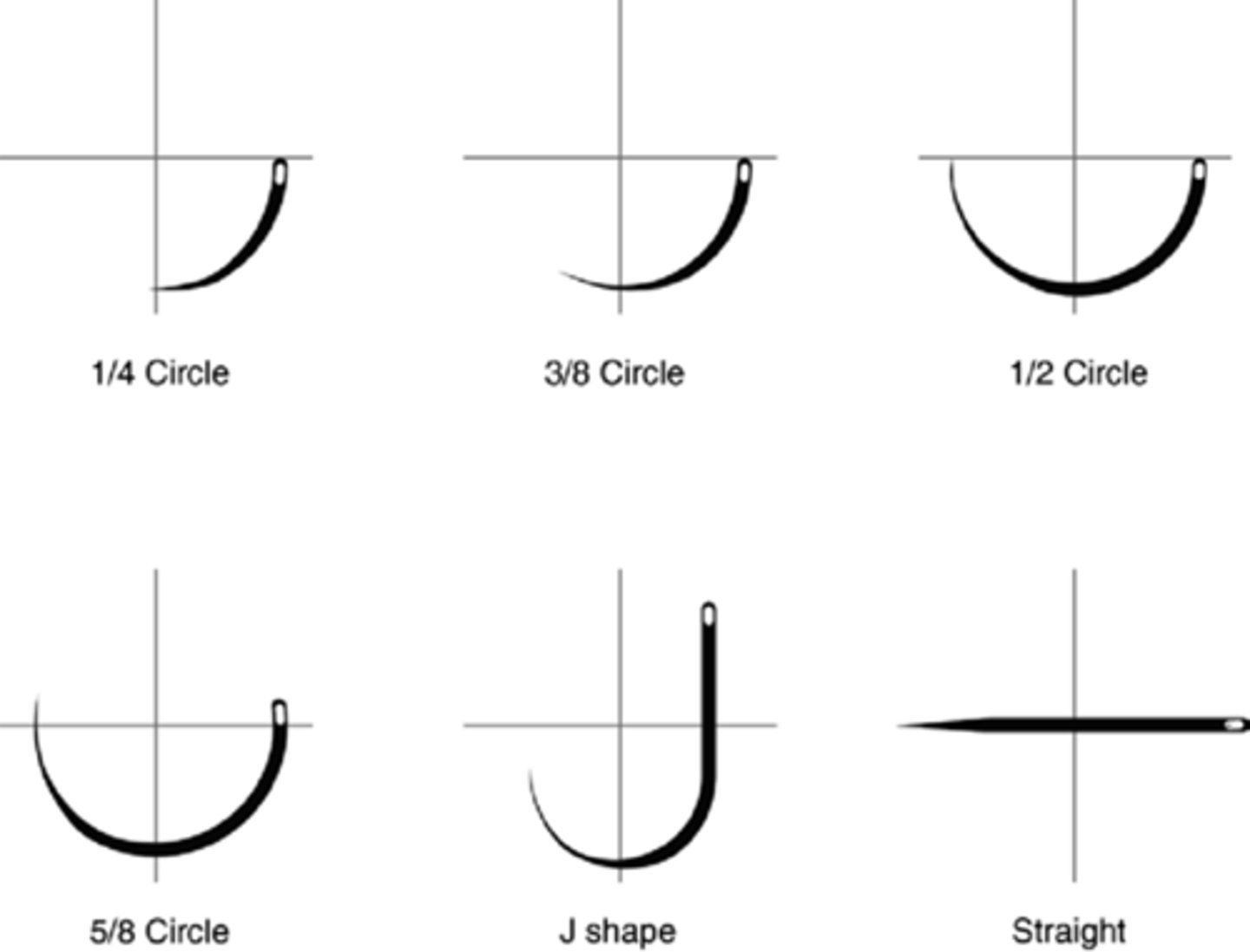
Instruments used for laceration repair
Scissors, tissue forceps, needle holder
Proper positions for laceration repair
Suture considerations: hairy region
Trim surrounding hair
Cutting the suture tails longer than usual
Use blue suture
Never shave an eyebrow
Suture considerations: lining up edges
Line up the hair and skin borders exactly to avoid misalignment
Align the vermilion border of the lips
Tattoos
If an incision has to be made, it is important to recognize and follow the natural skin tension lines
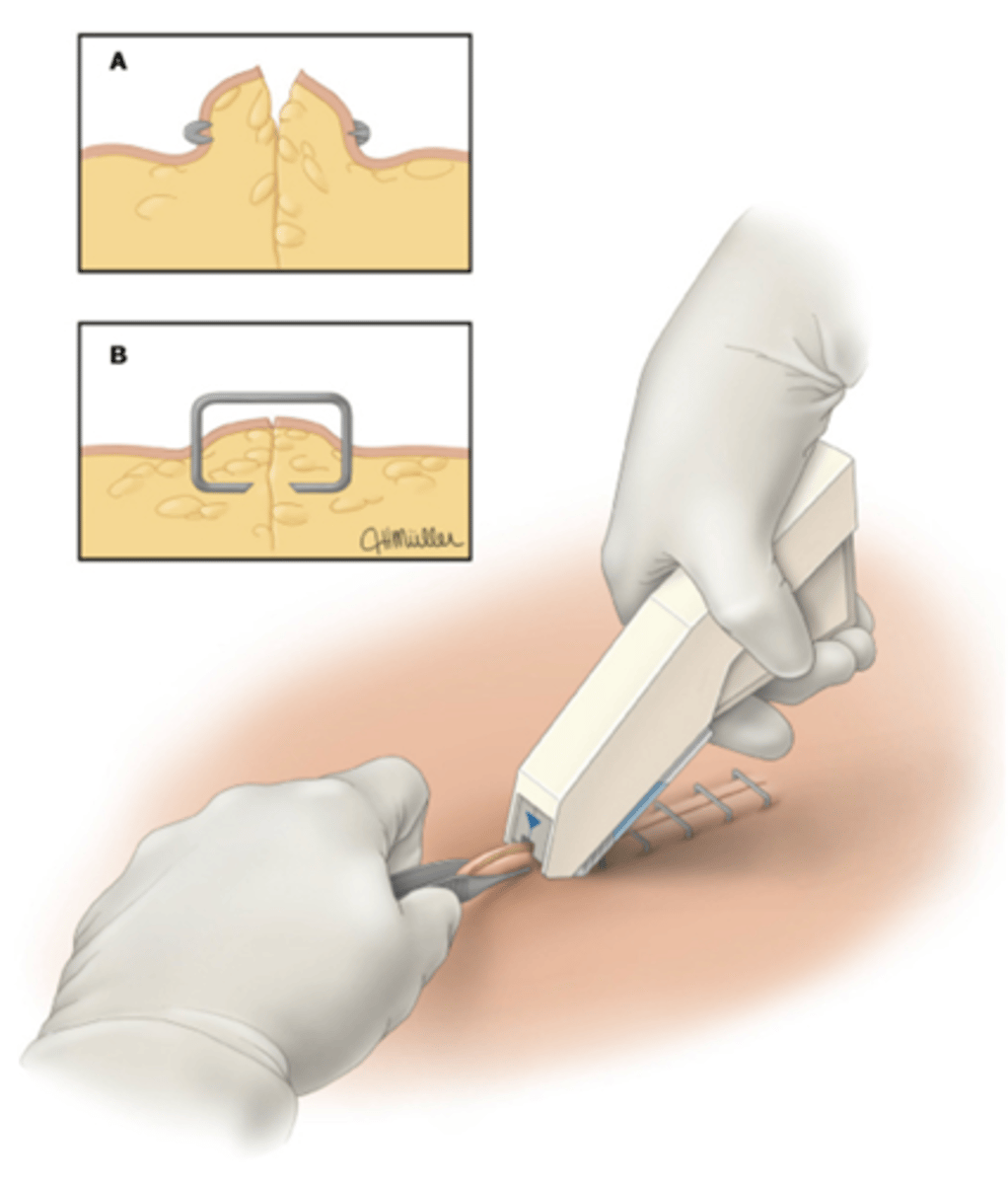
Staples
useful for long, linear lacerations of the scalp, trunk, and extremities because they can be applied quickly with the same ultimate cosmetic result as suture
How to apply staples
1.Use an assistant to evert the tissue edges of the laceration
2.Place staples over the approximated wound and firmly squeeze the trigger to deliver each staple
Follow up care after a laceration repair
Keep wound dry and clean
Elevate
Cold compress for 48 hours
Describe signs of infection
Wound check twice a day for signs of infection
Activity restriction
Pain medication
Return to clinic
Antibiotic considerations for wounds
Wounds > 12 hours old at initial presentation, especially those of the hands
Human or animal bites, including those caused by the patient's teeth
Crush wounds
Heavily contaminated wounds
Avascular areas, such as the cartilage of the ear
Joint spaces, tendon, or bone
Severe paronychia and felons
Wounds in patients with a history of valvular heart disease
Immunosuppressed patients
Antibiotic treatment for bite wounds
Augmentin - amoxicillin/clavulanate
Antibiotic treatment for MRSA
Clindamycin
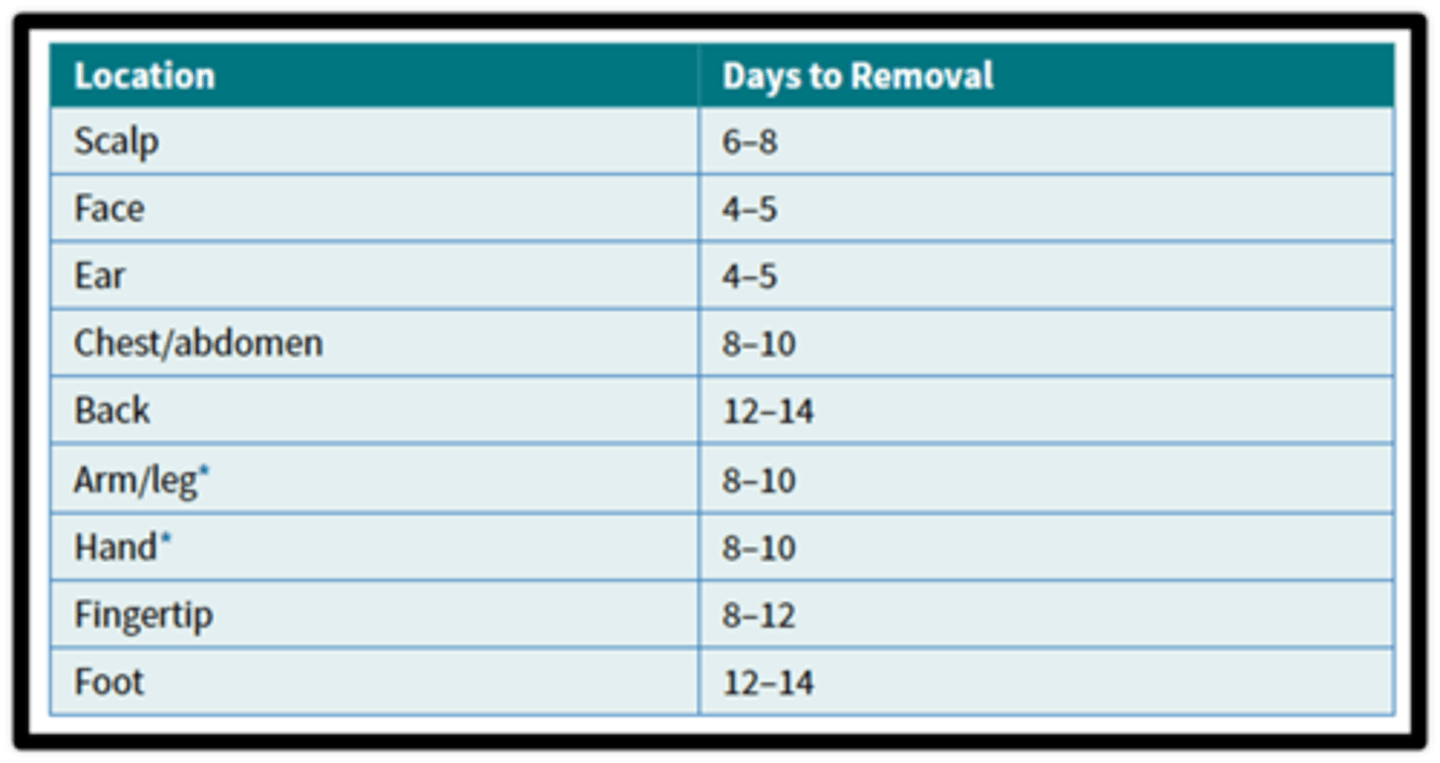
Suture removal: days until removal