High-Yield Neuroanatomy and Stroke Management
1/560
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
561 Terms
Stroke risk factors
The two most important risk factors for stroke (cerebral infarction) on USMLE are hypertension and atrial fibrillation.
Hypertension (HTN)
A strong systolic impulse pounds the carotid arteries, leading to endothelial damage and increased development of atherosclerotic plaques (carotid stenosis), which then launch off to the brain/eye.
Atrial fibrillation (AF)
Results in turbulence and stasis, leading to left atrial mural thrombus, which launches off.
Hypertension prevalence
Hypertension is most common in the population for causing stroke.
Blood pressure control
Blood pressure control is more important than smoking cessation for decreasing stroke risk.
AF vs HTN in stroke
If the USMLE Q gives you a patient who has both AF and HTN, they want AF as the most important risk factor.
Carotid stenosis
Occurs from HTN, where an atheromatous plaque has launched off.
Circle of Willis
A network of arteries at the base of the brain that supplies blood to the brain.
ACA stroke
Anterior cerebral artery stroke leads to motor/sensory abnormalities of contralateral leg.
MCA stroke
Middle cerebral artery stroke leads to motor/sensory abnormalities of contralateral arm + face.
Dominant MCA stroke
Usually left MCA stroke can lead to Wernicke or Broca aphasia.
Non-dominant MCA stroke
Usually right MCA stroke can cause hemispatial neglect (inability to draw clockface).
PCA stroke
Posterior cerebral artery stroke leads to contralateral homonymous hemianopsia with macular sparing.
Prosopagnosia
Inability to recognize faces, associated with PCA stroke.
Lateral medullary syndrome
Also known as Wallenberg syndrome, the answer for dysphagia + ipsilateral Horner syndrome after a stroke.
PICA stroke
Causes dysphagia and is associated with lateral medullary syndrome.
Horner syndrome
Ipsilateral miosis, partial ptosis, anhidrosis, can be caused by Pancoast tumor or lateral medullary syndrome.
Medial medullary syndrome
The answer for ipsilateral tongue deviation after a stroke.
Lateral pontine syndrome
The answer for ipsilateral Bell's palsy after a stroke.
AICA stroke
Causes lateral pontine syndrome, which is associated with Bell's palsy.
Weber syndrome
Midbrain stroke that results in ipsilateral CN III palsy (down and out eye) + contralateral spastic hemiparesis.
Locked-in syndrome
Basilar artery stroke that results in inability to move entire body except for eyes.
Gerstmann syndrome
Stroke of angular gyrus of parietal lobe.
Tetrad
1) agraphia (inability to write); 2) acalculia (cannot do math); 3) finger agnosia (can't identify fingers); 4) left-right disassociation (cannot differentiate between left and right sides of body).
Hemiballismus
Stroke of subthalamic nucleus causing 'ballistic' flailing of contralateral arm and/or leg.
Lenticulostriate strokes
Strokes affecting small lenticulostriate arteries deep within the brain, often leading to lacunar infarcts.
Lacunar infarcts
Ischemia within small vessels leading to necrosis and reabsorption of tissue, resulting in tiny cavities called lacunae.
Charcot-Bouchard microaneurysms
Tiny (<1mm) aneurysms that form within lenticulostriate arteries that can bleed and cause hemorrhagic strokes.
Liquefactive necrosis
The answer for necrosis of nervous system tissue.
Red neurons
Strong eosinophilic (pink) staining seen acutely with ischemic infarction of the CNS.
Microglia
Resident macrophages of the CNS that phagocytose necrotic brain/spinal tissue.
Astrocytes
Glial cells that proliferate and become a glial scar (gliosis) in the CNS.
Wallerian degeneration
Degradation of an axon/myelin sheath distal to the site of injury, with regrowth occurring at a maximum of 1mm/day.
Optic nerve
Considered an extension of the CNS and myelinated by oligodendrocytes; degeneration results in permanent blindness.
Vertebrobasilar insufficiency
Condition related to blood flow issues in the vertebral artery affecting brain perfusion.
Subclavian steal syndrome
Condition caused by narrowing/stenosis of the proximal subclavian artery leading to lower pressure in the vertebral artery.
Dizziness
A potential neuro finding in subclavian steal syndrome due to backflow of blood in the vertebral artery.
Blood pressure difference
A sign of subclavian steal syndrome, where blood pressure is different between the two arms.
Pure motor hemiparesis
A specific syndrome that can manifest from lacunar infarcts.
Pure sensory stroke
Another specific syndrome that can manifest from lacunar infarcts.
Ataxic hemiparesis
A specific syndrome that can manifest from lacunar infarcts.
HTN
Hypertension can cause lipohyalinosis leading to lacunar infarcts.
Lipohyalinosis
A fancy term for microatheroma formation in small lenticulostriate arteries.
CNS
Central Nervous System, where astrocytes and microglia play crucial roles.
PNS
Peripheral Nervous System, where Schwann cells can regenerate myelin.
Oligodendrocytes
Cells in the CNS that do not effectively regenerate myelin post-injury.
CN VII
Cranial nerve associated with Bell's palsy, which has better regenerative potential compared to the optic nerve.
Blood pressure difference between arms
Indicates potential aortic dissection or subclavian steal syndrome.
CT or MR angiography
Next best step in diagnosis for conditions related to blood pressure differences.
Vertebral artery stenosis
Presents with unexplained dizziness without blood pressure differences between arms, caused by atherosclerosis.
Vertebrobasilar insufficiency
A broader term for patients with either subclavian steal syndrome or vertebral artery stenosis.
Vertebral artery dissection
A false lumen in a vertebral artery that can lead to stroke due to clot formation.
Heparin for vertebral artery dissection
Recommended treatment for patients who have experienced posterior stroke due to vertebral artery dissection.
Wernicke aphasia
Fluent aphasia characterized by nonsensical speech and impaired comprehension, caused by L-sided MCA infarct.
Broca aphasia
Non-fluent aphasia with telegraphic speech and normal comprehension, caused by L-sided MCA infarct.
Conductive aphasia
Impaired repetition due to stroke of the arcuate fasciculus connecting Wernicke and Broca areas.
Global aphasia
Combination of Broca and Wernicke aphasias with impaired repetition, caused by stroke affecting Broca, Wernicke areas, and arcuate fasciculus.
Transcortical sensory aphasia
Similar presentation to Wernicke's aphasia but with intact repetition.
Transcortical motor aphasia
Similar presentation to Broca's aphasia but with intact repetition.
Ischemic stroke diagnosis
Non-contrast CT of the head is done to differentiate between ischemic and hemorrhagic stroke.
tPA administration
Given for ischemic stroke within 4.5 hours of symptom onset if no contraindications are present.
4.5-hour window for tPA
Refers to the time since the patient was last confirmed normal before stroke symptoms appeared.
Aspirin for ischemic stroke
Recommended if the 4.5-hour window has elapsed after stroke onset.
185/110
Blood pressure control for tPA: BP should be below ___before administering tPA.
Hemorrhagic stroke treatment
Do not give tPA; first step is to lower blood pressure.
Labetalol, nicardipine, hydralazine
Medications used to lower blood pressure in hemorrhagic stroke.
hemorrhagic
Non-contrast CT findings: Blood appears as bright (hyperdense) areas on CT in cases of __stroke.
Contrast CT
Used for diagnosing conditions like brain abscess and malignancy, not for suspected bleeds.
Stroke of arcuate fasciculus
Leads to conductive aphasia due to impaired repetition.
Frontal lobe stroke
Causes Broca's aphasia.
Temporal lobe stroke
Causes Wernicke's aphasia.
Systolic BP reduction
Reduce BP rapidly to systolic <140 mm Hg.
Anticoagulation reversal
Reverse anticoagulation if the patient is on it (i.e., FFP for patients on warfarin).
Cerebral edema
Correction of hypernatremia too quickly with hypotonic saline can cause cerebral edema.
Central pontine myelinolysis
Correcting hyponatremia too quickly with hypertonic saline causes central pontine myelinolysis.
Osmotic demyelination
Can be described as 'osmotic demyelination.'
Locked-in syndrome
Central pontine myelinolysis causes locked-in syndrome.
Hypercalcemic crisis
Refers to cognitive dysfunction / a delirium-like state in the setting of severe hypercalcemia, often due to malignancy or primary hyperparathyroidism.
Delirium
USMLE wants you to know that high calcium, as well as any sodium disturbance, can cause ___
Treatment for hypercalcemia
First step on USMLE for Tx of hypercalcemia is normal saline.
Bisphosphonate therapy
After normal saline, USMLE wants bisphosphonate therapy (I've seen pamidronate listed on NBME).
Pseudotumor cerebri
Term that refers to increased intracranial pressure in the setting of no clear structural cause.
Papilledema
Q can mention papilledema (optic disc swelling) or absent venous pulsations on fundoscopy (another increased ICP buzzy finding).
Reye syndrome
Cerebral edema and hepatotoxicity seen with administration of aspirin to children (and sometimes adolescents) during a viral infection.
Beta-oxidation impairment
Thought to be due to impairment of beta-oxidation, but USMLE doesn't care.
Diffuse axonal injury
Deceleration injury (e.g., car accident) followed by severe cognitive and/or motor/sensory dysfunction.
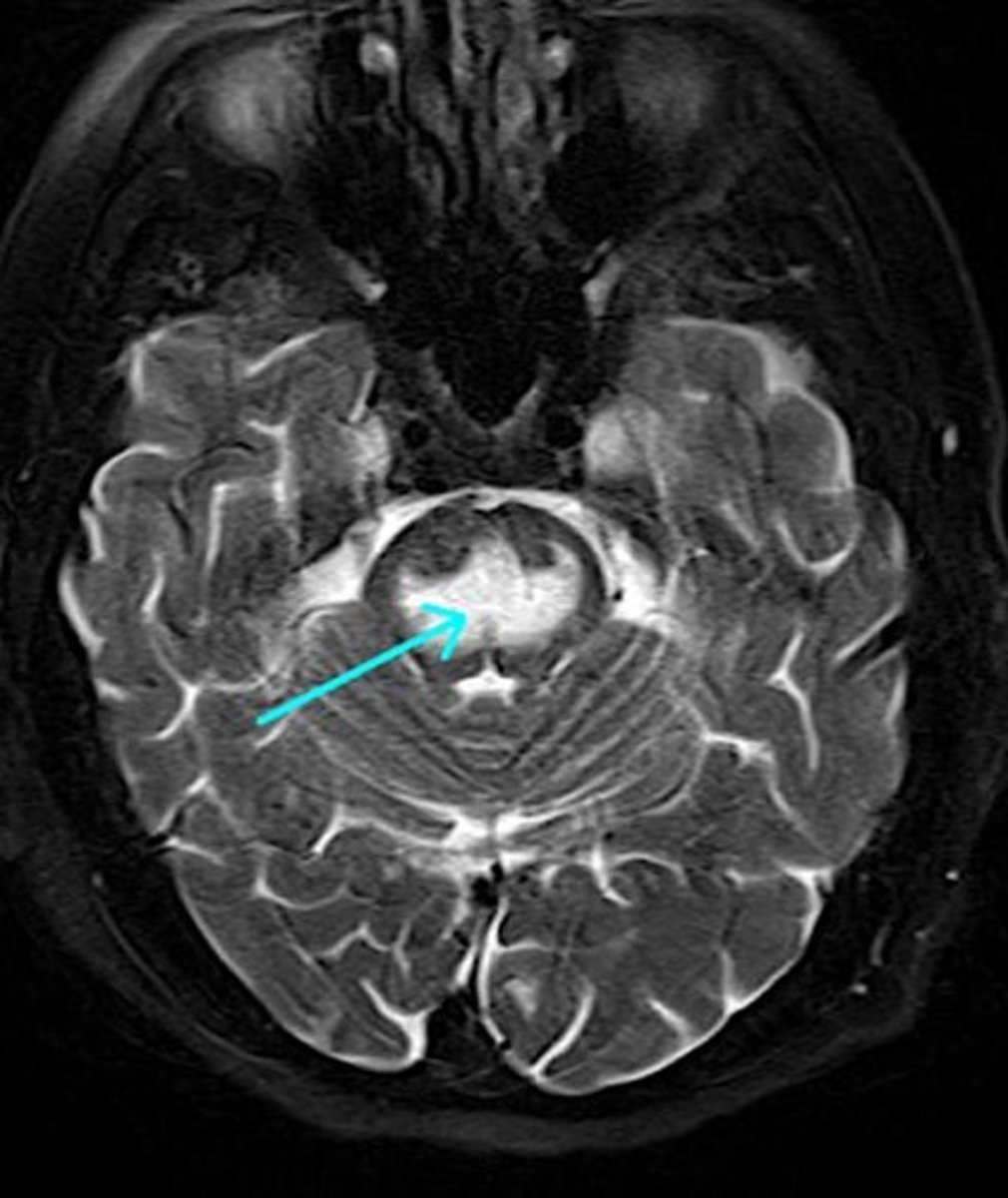
MRI findings in diffuse axonal injury
USMLE can show MRI showing scattered hyperintense (white) lesions.
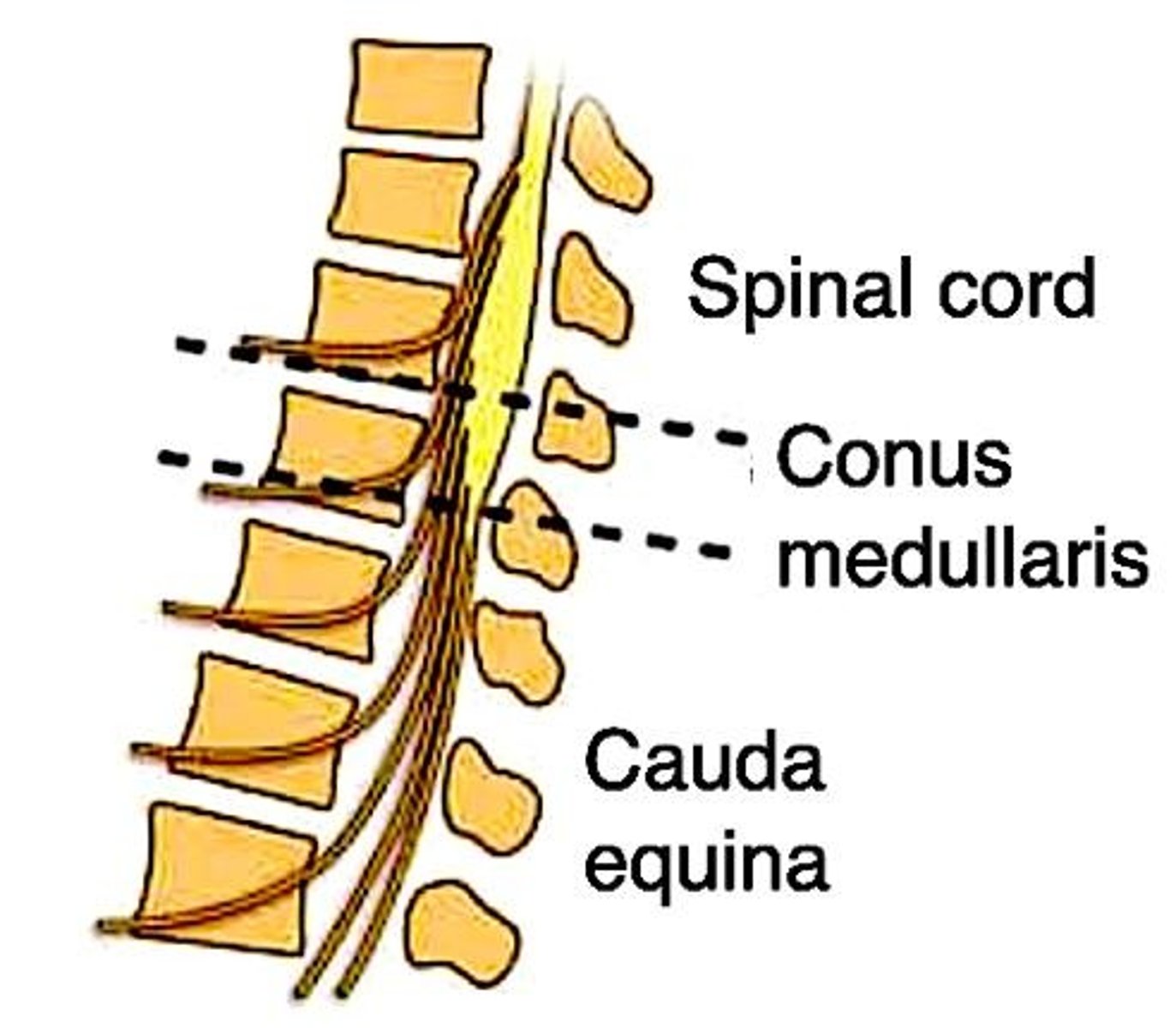
Spinothalamic tract
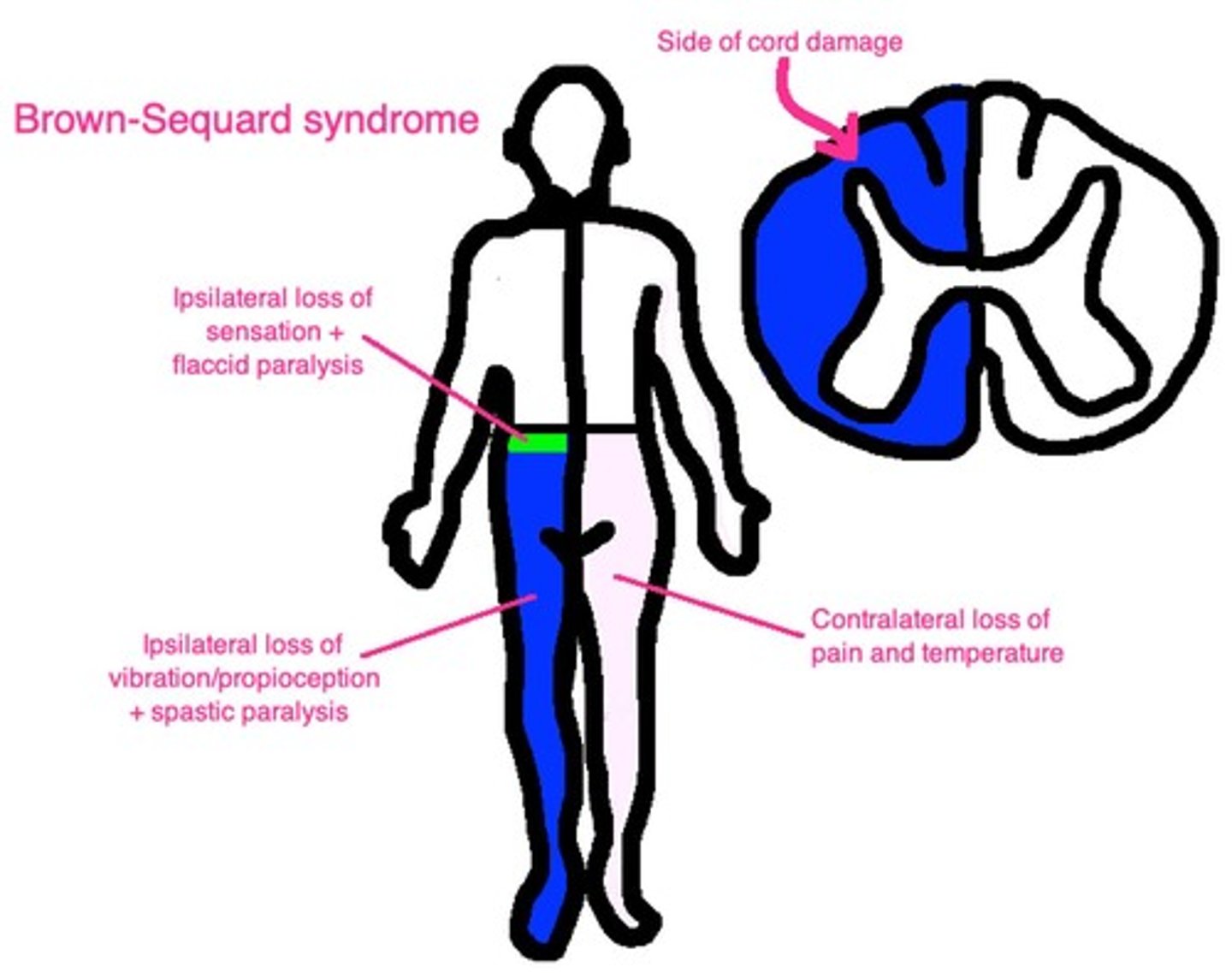
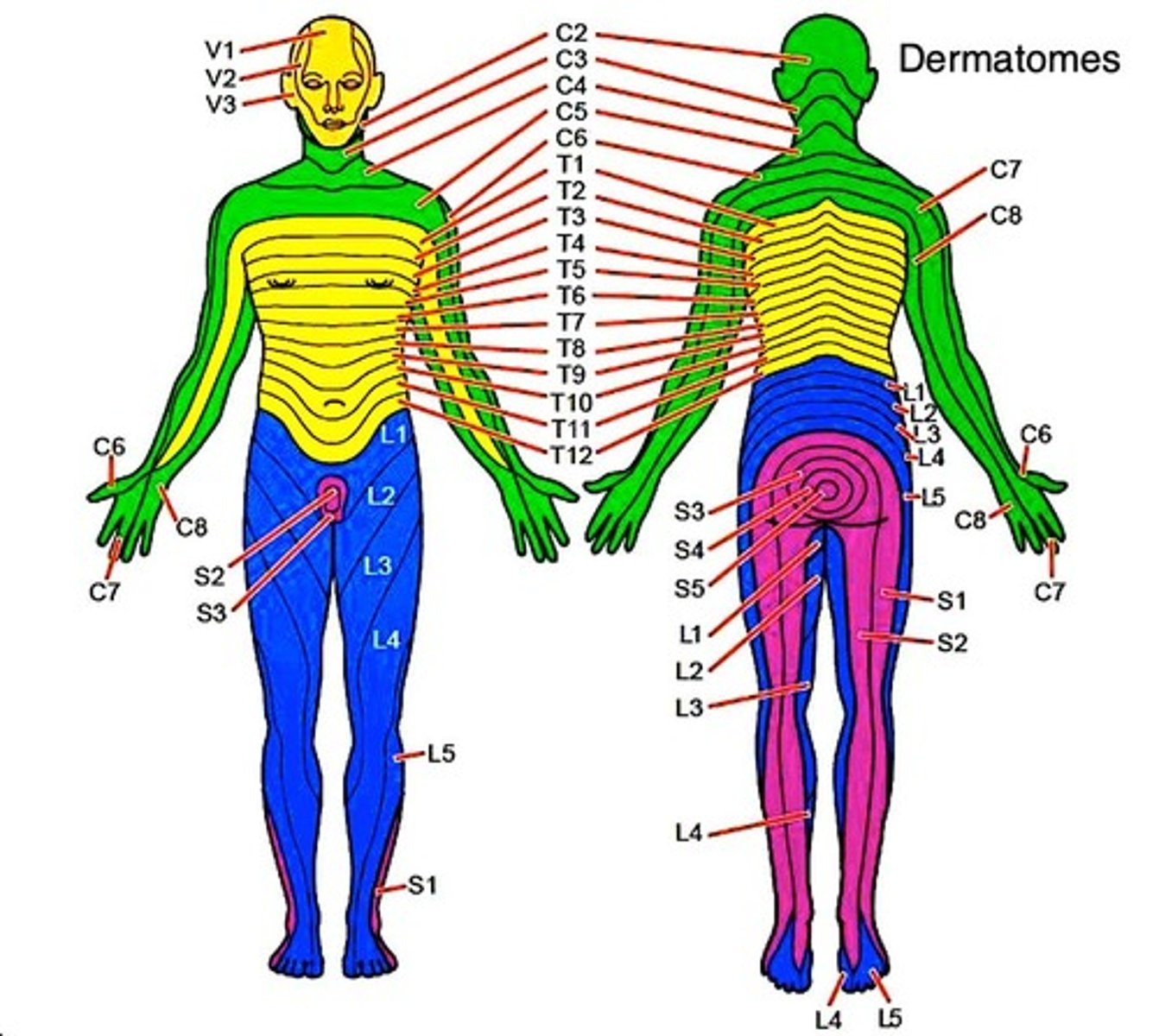
Pain and temperature sensation from contralateral body.
Decussation point
Cross-over (decussation) point is in spinal cord, meaning if, e.g., the left spinothalamic tract is damaged, we lose pain and temperature on the right side of the body below the lesion.
Corticospinal tract
Motor function from ipsilateral body.
Dorsal columns
Carry vibration + proprioception from ipsilateral body.
Tabes dorsalis
Dorsal column lesion caused by neurosyphilis.
Romberg test
If the dorsal columns are disrupted, patient will have (+) ___ which is where he/she falls over when standing with eyes closed.
Upper motor neuron findings
Lesion of the corticospinal tract presents as hyperreflexia, hypertonia, clonus, Babinski sign.
Lower motor neuron findings
Lesion involving the motor neuron from the anterior horn until the muscle itself presents as hyporeflexia, hypotonia/flaccidity, fasciculations.
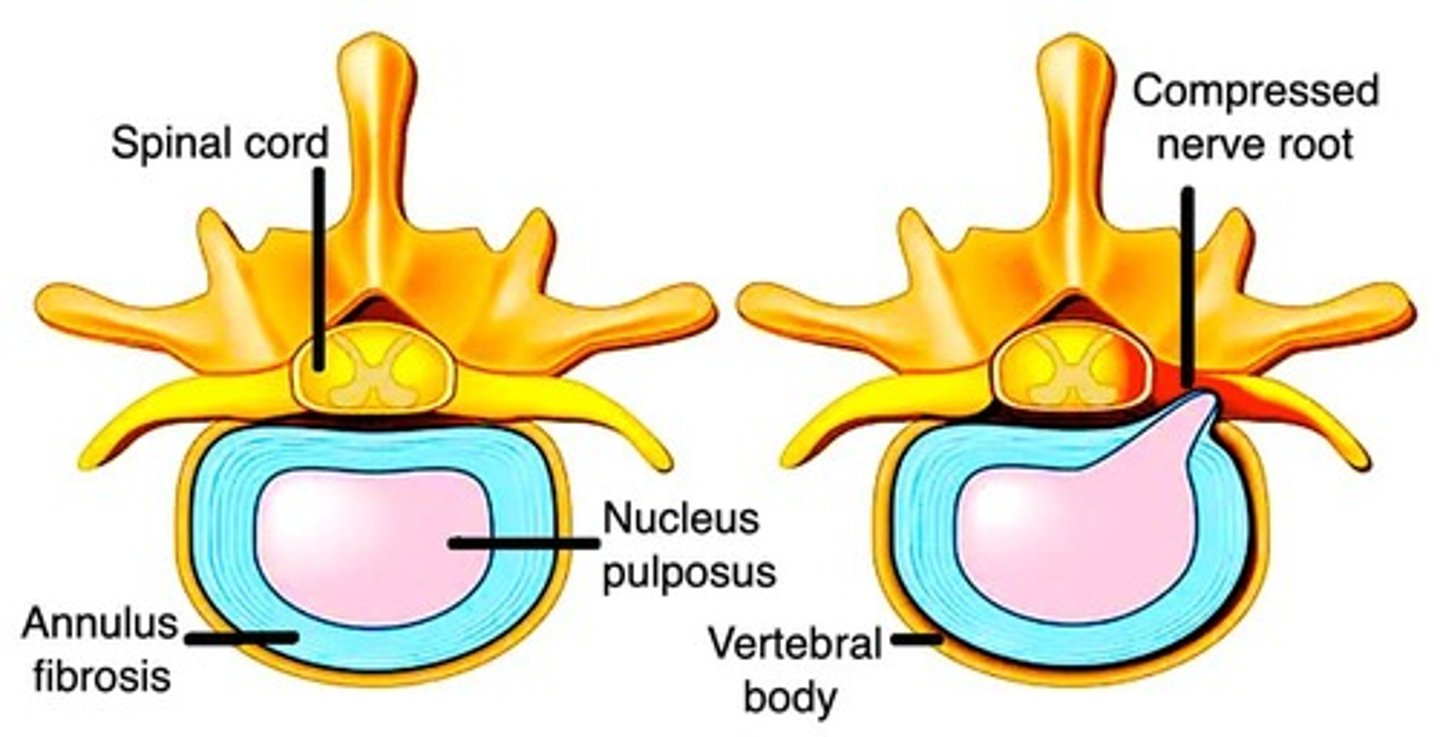
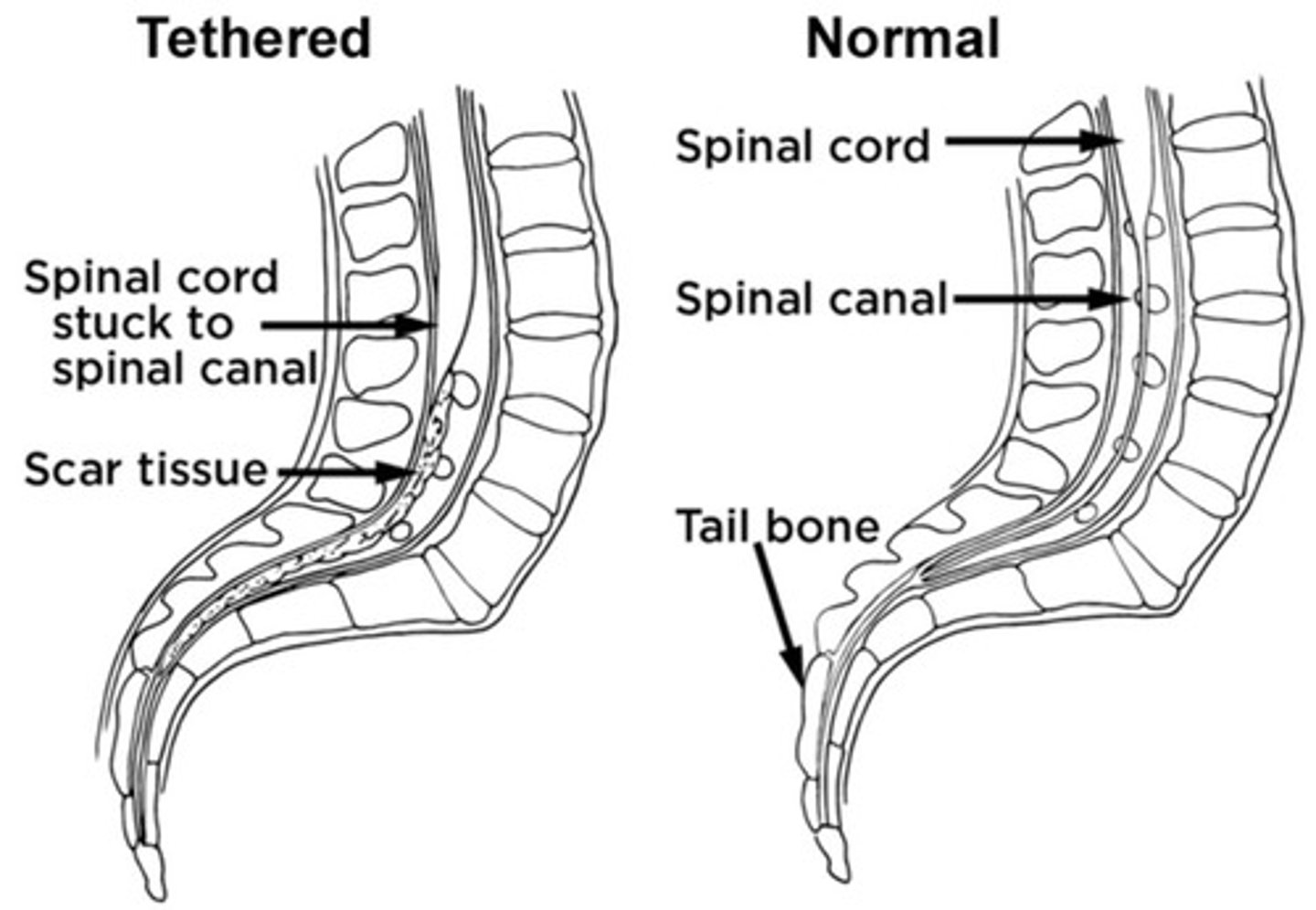
Syringomyelia
9/10 Qs will give bilateral loss of pain and temperature due to lesion of anterior white commissure (decussation point for spinothalamic tract).
Corticospinal Tract Involvement
Maybe 1/3 of Qs will also involve corticospinal tract, where you'll see some impaired motor function in addition to the bilateral loss of pain/temperature.
Impaired Motor Function
1/10 Qs will not mention pain/temperature loss but instead just give impaired motor function, where it sounds nothing like syringomyelia, but you're forced to eliminate to get there (on a 2CK Neuro CMS form).
Brown-Sequard Syndrome
Ipsilateral loss of vibration + proprioception (dorsal columns).
Brown-Sequard Syndrome
Ipsilateral loss of motor function (corticospinal tract).