patho 1. cell death & injury 2
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
86 Terms
What are the 4 main mechanisms under intracellular accumulations
1. Inadequate removal of normal substance
2. Accumulation of an endogenous substance
3. Failure to degrade a metabolite
4. Deposition and accumulation of abnormal exogenous substance
What is the cause of intracellular accumulations
metabolic derangements
Intracellular accumulations can be reversible (T or F)
TRUE. It can be reversible if controlled or stopped
In inherited storage diseases intracellular accumulation can cause cellular injury, and if progressive, sometimes leading to cell death
(T or F).
TRUE. It causes cell injury in storage diseases.
What are the three major lipid classes that can accumulate in cells?
Triglycerides, cholesterol/chol esters, phospholipids
What is steatosis and where is it most often seen?
Abnormal triglyceride accumulation — liver
Name two common causes of fatty change in the liver.
Alcohol abuse, nonalcoholic fatty liver disease
Which condition involves cholesterol-laden macrophages in skin and tendons?
Xanthomas
What are foam cells in gallbladder lamina propria
Cholesterolosis
What usually appear as Rounded eosinophilic droplets, vacuoles, aggregates?
Protein intracellular accumulation
Rounded eosinophilic droplets, vacuoles, aggregates
Reabsorption droplets
Large eosinophilic ER inclusions in plasma cells actively producing immunoglobulins are called what?
Russell bodies
Which protein accumulation is associated with α1-antitrypsin deficiency?
Misfolded proteins
Which abnormal protein accumulation can deposit intra/extracellularly and disrupt function?
Amyloidosis
This intracellular accumulation pertains to an alteration within cells or extracellular space that gives a glassy, pink appearance on H&E
Hyaline change
What protein accumulation is included in intracellular hyaline change?
Reabsorption droplets and Russell bodies
Patients with long-standing hypertension and diabetes suffer from hyalinized _________, especially in the kidney
Arterioles
Extracellular hyaline found in old scars contain what type of fibers?
Collagenous fibers
True or False: Hyaline change is a general term
TRUE
What intracellular accumulation occurs in patients with abnormalities in either glucose or glycogen metabolism?
Glycogen
What do glycogen masses appear as within the cytoplasm?
Clear vacuoles
What staining method is used to identify glycogen?
Best carmine/ Periodic acid-Schiff stain
Glycogen may accumulate in the pancreas, specifically in what type of cells?
Beta cells of the islets of Langerhans
True or False: Defects in glycogen synthesis or breakdown can result to cell injury and death
TRUE
This is defined as the abnormal tissue deposition of calcium salts, together with smaller amounts of iron, magnesium, and other mineral salts?
pathologic calcification
How are the deposits described in the gross appearance of a pathologic calcification?
they are described as gritty deposits
What material are commonly deposited in pathologic calcification?
deposition of calcium salts are commonly seen
True or False. When looking at a pathologic calcification microscopically, you can observe eosinophilic, amorphous granular or clumped appearance?
False. It should be basophilic
True or False. White clumps are seen grossly when examining a specimen with pathologic calcification?
True.
Where is dystrophic calcification commonly seen?
They are commonly seen in dying or necrotic tissues.
How is Dystrophic calcification different from metastatic calcification?
dystrophic calcifications occur despite having normal serum levels of calcium
What type of bone may form at the focus of calcification?
Heterotrophic bone
Identify the given structure.
Psammoma bodies
Identify the given structure.
Asbestos bodies
Type of pathologic calcification resulting from hypercalcemia
Metastatic Calcification
True or False. Increased secretion of Parathyroid (PTH) prevent metastatic calcification
FALSE. Increased PTH is a known principal cause of metastatic calcification.
True or False. Hypercalcemia SOLELY affects the progression of metastatic calcification,
FALSE. It can also accentuate dystrophic calcification
Identify the deposit pointed on the fingers by the blue arrows.
Calcium
Microscopic findings of this sample specimen can be found in what pathologic cellular alteration.
Metastatic Calcification
True or False. Cellular aging is the progressive decline in biochemical function and viability caused by genetic abnormalities and the accumulation of cellular and molecular damage from exposure to endogenous influences.
FALSE
What is one of the strongest independent risk factors for many chronic diseases?
Age
What are two key processes that can counteract cellular aging?
DNA Repair and Protein Homeostasis
What are the effects of defective protein homeostasis on cells?
Increase of damaged proteins and decreased cell functions.
What two factors in nutrient sensing contributes to altered transcription?
decrease in Insulin/IGF signaling and decrease in TOR Altered sirtuins
True or False. Werner Syndrome a is genetic disorder associated with premature or accelerated aging due to DNA repair defects.
TRUE
True or False. All DNA damage is repaired by DNA repair
enzymes.
FALSE
What can happen to DNA damage that is not repaired as cells age?
It persists and accumulates over time
What can result from defects in genes responsible for DNA replication and repair?
Premature/Accelerated aging
Give an example of syndromes caused by defects in DNA repair mechanism.
Werner Syndrome, Bloom syndrome, ataxia-telangiectasia
What is the name of the non-dividing state that cells enter after a fixed number of divisions?
Replicative senescence
It is the progressive shortening of telomeres during replication.
Telomere attrition
True or False. Shortening of telomeres is associated with the premature development of diseases.
TRUE
What are the two mechanisms that underlie cellular senescence?
Telomere attrition and Activation of Tumor Suppressor Genes
This protein is encoded by CDKN2A gene to protect cells from uncontrolled mitogenic signals and pushes cells along the senescence pathway.
p16/INK4a
How does defective protein homeostasis affect our cells?
Impairs cell survival, replication, function, and can trigger apoptosis
A common example of a disease linked with defective protein homeostasis
Alzheimer's
How does IGF-1 influence the cells?
Mimics insulin, promotes anabolic state as well as cell growth and replication
Sirtuins and their role/s
NAD-dependent protein deacetylases that help cells adapt to stress, promote longevity, and regulate metabolism
3 Effects of Sirtuins that can promote longevity
Inhibition of metabolic activity, reducing apoptosis, stimulating protein folding, counteracting free radicals, and increasing insulin sensitivity.
How does caloric restriction affect the IGF-1 pathway?
Decreases IGF-1 signaling, lowering cell growth and metabolism, which is linked to a longer life span
What is the connection between dysregulated nutrient sensing and aging?
Overactive growth-promoting pathways (like IGF-1) and reduced stress-adaptation mechanisms (like sirtuins) accelerate aging and age-related diseases.
How does caloric restriction affect the Sirtuins?
It increases their activity, improving stress adaptation and activating DNA repair enzymes.
What are endogenous pigments?
Pigments synthesized within the body itself.
What is another name for Lipofuscin?
Lipchrome
What type of pigment is Lipofuscin?
A wear-and-tear pigment
Is Lipofuscin soluble or insoluble?
Insoluble
Describe the appearance of Lipofuscin.
Yellow-brown, finely granular cytoplasmic pigment
In what type of cells is Lipofuscin present?
Cells undergoing slow, regressive changes (e.g., liver, heart of aging patients)
Describe the appearance of melanin.
Brown-black pigment
What produces melanin?
Melanocytes and melanin-producing tumors
Give examples of melanin-producing tumors.
Pigmented intradermal nevus or melanomas
Describe the appearance of hemosiderin.
Golden, yellow-to-brown, granular, or crystalline pigment
What is hemosiderin derived from?
Hemoglobin
What is hemosiderin's role in iron storage?
One of the major storage forms of iron
What does hemosiderin represent?
Aggregates of ferritin micelles
Where may small amounts of hemosiderin be seen?
Within mononuclear phagocytes in the marrow
When is hemosiderin found in excess?
In tissue hemorrhage (e.g., bruises; changes from red/blue → green-blue → golden-yellow)
What is hemosiderosis?
Systemic iron overload
What are the causes of hemosiderosis?
1. Increased iron absorption due to inborn error of metabolism (hemochromatosis)
2. Hemolytic anemia
3. Repeated blood transfusions
What are exogenous pigments?
Pigments that come from outside the body.
What is the most common exogenous pigment?
Carbon (coal dust) — a ubiquitous air pollutant in urban areas.
What is anthracosis?
Accumulation of carbon in lung tissue and involved lymph nodes, especially in the hilar lymph nodes.
What is coal worker’s pneumoconiosis?
A lung disease caused by a fibroblastic reaction toward aggregates of carbon dust.
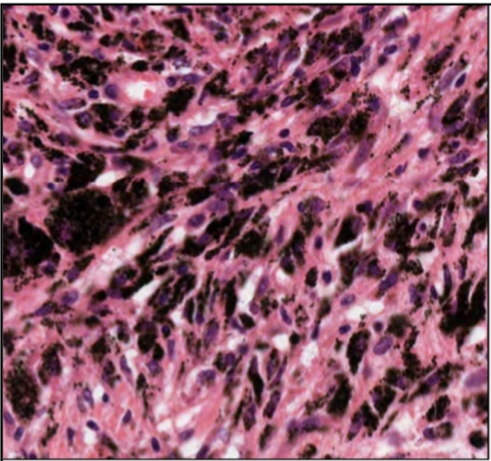
What is shown in Figure 16 of the provided material?
Accumulation of coal dust in the lungs.
What is tattooing in the context of exogenous pigments?
A form of localized, exogenous pigmentation of the skin by colored inks.
Four principal causes of metastatic calcification
Increased secretion of PTH
Resorption of bone
Vitamin D–related disorders
Renal failure