pulmonary examination
1/63
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
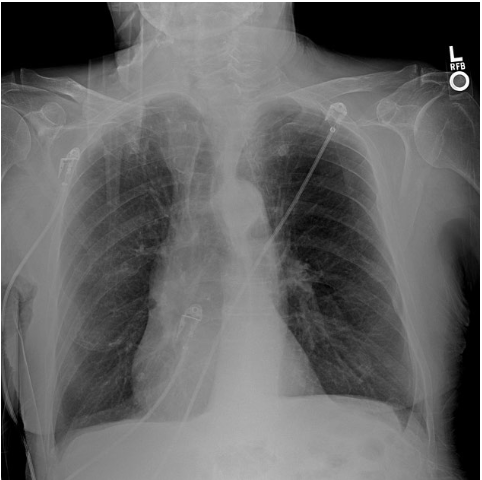
what should an xray of the lungs look like
radiolucency
radio-opaque
there is more density (looks white on the imaging)
radiolucency
appears black on the imaging (less dense)
xray of lungs with COPD
widened intercostal spaces
flattened hemidiaphragms
squared off costophrenic angles and rib angles that approach 90 degree angles
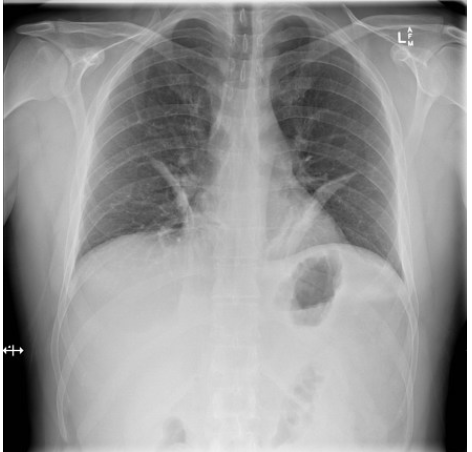
xray of lungs with atelectasis
diaphragm elevation on the collapsed side
deviation of the mediiastinum, trachea (deviated towards collapsed side
increased density of the lobe
normal FEV1 value
above 80% of the predicted value for age, gender, height and ethnicity
normal FEV1/FVC ratio in adults
above 0.7% (70%)
normal FEV1/FVC ratio in younger individuals
above 0.75-0.8%
normal FEV1/FVC ratio in people with COPD
less than 70%
forced vital capacity
the maximal volume of gas a patient can forcefully and quickly exhale
forced vital capacity technique
maximal inspiration followed by rapid and forceful expiration
forced vital capacity interpretation
generally reduced in both obstructive and resistive diseases
regulation of acids
the lungs violate acids by CO2 excretion
the kidney regulate nonvolatile acids through exctetion
the pationets ABG findings are
PH: 7.51, pCO2: 27, pO2: 146, HCO3: 24
a. respiratory acidosis
b. respiratory alkalosis
c. metabolic acidosis
d. metabolic alkalosis
B. Respiratory alkalosis
the patients ABG findings are
PH: 7.2, pCO2: 40, PaO2: 60, HCO3: 1
a. respiratory acidosis
b. respiratory alkalosis
c. metabolic acidosis
d. metabolic alkalosis
C metabolic acidosis
what regulates major blood base (bicarbonate)
kidneys
normal blood pH
7.4
pH value that indicates acidosis
less than 7.4
2 mechanisms of acidosis
metabolic acidosis (decreased HCO3)
respiratory acidosis (increased PcCO2)
pH value that indicates alkalosis
pH above 7.4
2 mechanisms of alkalosis
metabolic alkalosis: increased HCO3
respiratory alkalosis: decreased PaCO2
normal PaCO2 value
40 mmHg
PaCO2 value that is considered acidic
above 40 (respiratory acidosis)
PaCO2 value that is considered alkaline
less than 40 (respiratory alkalosis)
normal HCO3 value
24 mEq/L
HCO3 value that is considered acidic
less than 24 (metabolic acidosis)
HCO3 value that is considered alkaline
above 24 (metabolic alkalosis)
causes of respiratory alkalosis
hyperventilation
causes of respiratory acidosis
respiratory depression (medications, CNS trauma), pulmonary disease (pneumonia, COPD, cystic fibrosis, asthma)
presentation of respiratory alkalosis
lightheadedness
dyspnea
parestheia
chest tightness
seziure
clinical implications of respiratory alkalosis
monitor vital signs
breathing pattern
respiratory status
presentation of respiratory acidosis
anxiety
confusion
fatigue/lethargy
tachypnea
coma
seizure
clinical implications of respiratory acidosis
monitor vital signs
breathing pattern
respiratory status
causes of metabolic alkalosis
sodium bicarbonate overdose
prolonged vomiting
nasogastric drainage
cystic fibrosis
causes of metabolic acidosis
diabetes
shock
renal failure
interstitial fistula
presentation of metabolic acidosis
dyspnea
fatigue
nausea/vomiting
tachyarrhythmias
hypotension
presentation of metabolic alkalosis
confusion
delirium
dysrhythmias
hypotension
muscle cramping
clinical implications of metabolic alkalosis
monitor vital signs and cardiac rhythm throughout the physical therapy interventioin
assess + monitor for cognitive impairment due to increased risk for altered mental status
clinical implications of metabolic acidosis
monitor breathing pattern, respiratory status, vital signs, and cardiac rhythm during PT intervention
consider treating using the BORG RPE scale
normal PaO2
80-100
severity of hypoxemia
60-80 mmHg = mild hypoxemia
40-60 mmHg = moderate hypoxemia
<40 mmHg = severe hypoxemia
factors that influence hypoxemia
hemoglobin concentration
capillary blood flow
clinical implications of oxygen status assessment
hypoxemia is a key indicator of impaired oxygen delivery
requires further investigation
may necessitate intiiation or adjustment of supplemental oxygen
assessment equation for someone with supplemental oxygen
expected PaO2 = FiO2 × 500
vesicular breath sounds
soft
low pitched
except near trachea and mainstream bronchi
heard during inspiration and early expiration
bronchial breath sounds
loud
hollow/tubular sounds
high pitched
heard near trachea and mainstream bronchi (sternal notch)
bronchovesicular breath sounds
softer than bronchial breath sounds
heard near parasternal and supraclavicular and suprascapular region
at the junction of mainstream bronchi with the segmental bronchi
crackle breath sounds
discontinous popping sound
heard over the infiltrate or cough
fine crackles (atelectasis)
wheezes breath sounds
continous, low or high pitched
airway obstruction bronchospasm
stridor breath sounds
very high pitched
indicates upper airway obstruction
pleural rub breath sounds
grating sound indicates pleural information
normal respiratory rate for an adult
12-20
brown sputum color
indicates possible bleeding from awhile ago, bright red means new blood
black mucus sputum color
may indicate the presence of a fungal infection
white mucoid sputum color
signals nasal congestion
respiratory distress signs
nasal flaring
sweating
paleness
focused or enlarged pupils
mediate percussion characterized sounds
resonant
hyper resonant
dull
hyper resonant mediate percussion sound
over emphysematous lungs or pneumothorax
dull mediate percussion sound
increased tissue density or lungs with decreased air
fremitus definition
vibreation produced by voice or secretions in the airway
fremitus palpation technique
palpation with palms placed lightly on the chest wall
patient repeats a word (ex: 99) to distinguish normal and abnormal fremitus
normal fremitus findings
palpation reveals uniform vibrations throughout the entire chest wall
increased fremitus signs
increase in secretions in a specific area
decreased fremitus signs
increase in air in a particular area