Pharm Exam 1 Review
1/217
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
218 Terms
Mechanism of Action (MOA)
A term describing the effects of drugs that interact with other chemicals in the body.
pharmacodynamics
what the drug does to the body
pharmacokinetics
what the body does to the drug; absorb, distribute, metabolize, excrete
pharmacogenetics
the study of how genetic variation affects an individual's response to drugs
receptor
protein on the cell that interacts with drug
ligand
molecule that binds to a receptor
hormone
natural substance that is produced in the body and influences the way the body grows/develops
xenobiotic
substance that is foreign to the body
toxin
poison of biologic origin
toxicant
poisons of non-biologic orogin
agonist
binds to a receptor and activates it
affinity
how tightly a drug binds to a receptor
potency
amount of drug necessary to elicit a response
efficacy
drug's ability to produce the maximal desired response
full agonist
produces a full response at full receptor occupancy
partial agonist
binds to a receptor but partially activates the receptor; if you bind 100% of the receptors, you get 50% effect
antagonist
blocks the action of agonist
competitive antagonist
binds to receptors and prevents binding by other molecules; direct competition (beta-blocker)
non-competitive antagonist
Binds to the receptor with such strong affinity that the receptor is no longer available to bind with an agonist regardless of the concentration
allosteric antagonism
binds to allosteric site and prevents agonist action
chemical antagonism
binds directly to agonist
functional antagonism
indirectly inhibits physiologic actions of the agonist
reversible antagonist
disassociate from their receptor
irreversible antagonists
permanent, irreversible chemical bond with their receptors
high specificity
one type of receptor; very specific tissue/cell sites (abx)
low specificity
multiple receptors, more adverse effects (chemo)
stereochemistry
drugs can have left-handed and right-handed version
down regulation
protective response that the body produces in response to a drug so the body reduces the number of receptors; responsiveness is diminished
what would you have to do to overcome down regulation?
increase dose to retain effectiveness
up-regulation
body increases number of receptors; seen with antagonists
bioavailability
amount of a drug that reaches it site of action through a given route
which route of drug has the highest bioavailability?
IV; 100%
first pass effect
The initial metabolism in the liver of a drug absorbed from the gastrointestinal tract before the drug reaches systemic circulation through the bloodstream.
prodrug
An inactive drug dosage form that is converted to an active metabolite by various biochemical reactions once it is metabolized by the liver
Volume of distribution (Vd)
how extensively a drug distributes into the tissue as opposed to blood
IV administration
advantages: fast onset, 100% bioavailability,
disadvantages: can't take back what you give, precipitation can cause crystals, extravasation
extravasation
drug leakage from a vessel into the tissue
intraosseous administration
into the bone; used in children in emergent situations as an IV alternative
subcutaneous administration (SQ)
advantages: good for slow-release implants and self-administration, high bioavailability, slower onset
disadvantages: painful, could cause necrosis
intramuscular administration (IM)
advantages: less invasive, high bioavailability, fast onset
disadvantages: painful, limit volume (3ml), requires blood flow, obese and emaciated pts may have altered absorption, exercise/heat could affect absorption
intrathecal (IT)
BBB limit/slow absorption of drugs; injections into subarachnoid space
sublingual (SL)
advantages: bypasses liver, good for pts who cannot swallow
disadvantages: few drugs can be used SL
oral (PO) administration
advantages: most common, safest, economical
disadvantages: patient compliance, swallowing, first pass effect, food/drug interactions (ex milk)
rectal (PR) administration
advantages: alternative to PO, 50% bypass liver
disadvantages: irregular and incomplete absorption, patient compliance
inhalation (INH) administration
advantages: drug directly to the area is needed, fast
disadvantages: incorrect use
transdermal (TD) administration
advantages: controlled-release patches increase patient compliance
disadvantages: not all drugs penetrate on skin, can't be used on open wounds, used patches still contain large amount of drug (hazardous)
after how many years does a generic drug become available?
20 years
clinical phases of human testing
phase 1: 10-100 healthy volunteers to determine dose
phase 2: 50-500 patients with the disease to determine efficacy
phase 3: 1000s to further establish safety and efficacy
phase 4: post-marketing surveillance, monitors safety
effector
mechanism that is activated by receptor
second messenger
Small intracellular signaling molecule generated or released in response to an extracellular signal.
contact-dependent signaling
Cells must be in direct contact. Important during development and for some types of immune function.
paracrine signaling
effects on cells in the local vicinity of the signaling cell
synaptic signaling
very specific and very rapid delivery of highly concentrated signaling molecules, neurotransmitter released
endocrine signaling
slow, nonspecific delivery, hormones released
receptor types
enzymes, transport proteins, structural proteins
enzyme receptors
may be inhibited or activated by binding to a drug
transport protein receptors
involved in movement of chemicals across a biological membrane
structural proteins receptors
primary purpose of producing essential structural components of cells
ion channel receptors
gated by neurotransmitters; coded for a specific ion channel, channels are constructed from 5 distinct subunits
G protein-coupled receptors
most diverse and numerous cell surface receptors; one ligand can often activate more than one type of G-protein coupled receptor
Half of all known drugs work through ____.
G-protein coupled receptors
Enzyme-linked receptors
transmembrane proteins with extracellular binding domain
intracellular receptors
located intracellularly for drugs that can penetrate the membrane
second messengers
relay signals from receptor to target molecule
what are second messengers activated by?
enzymes or opening of ion channels
most common second messengers
cAMP, cGMP, Ca2+ and phosphoinositide
cAMP
generated from ATP by adenyl cyclase, targets protein kinases
cGMP
GC signals cGMP which regulates the activity of protein kinases
common use of cGMP
regulate ion channel conductance in intestinal mucosa, relaxes vascular smooth muscle, affects vasodilation in vessels
common use of cAMP
metabolization of stored energy in liver (glucagon), conservation of water by kidneys via vasopressin, calcium homeostasis of PTH, increased HR and force of contraction
Ca2+ and inositol triphosphate (IP3)
main function is to mobilize Ca2+ from storage; inc Ca2+ results in muscle cell contraction, secretion of insulin, cell division
dose-response relationship
the relationship between the drug concentrations and the responses they generate
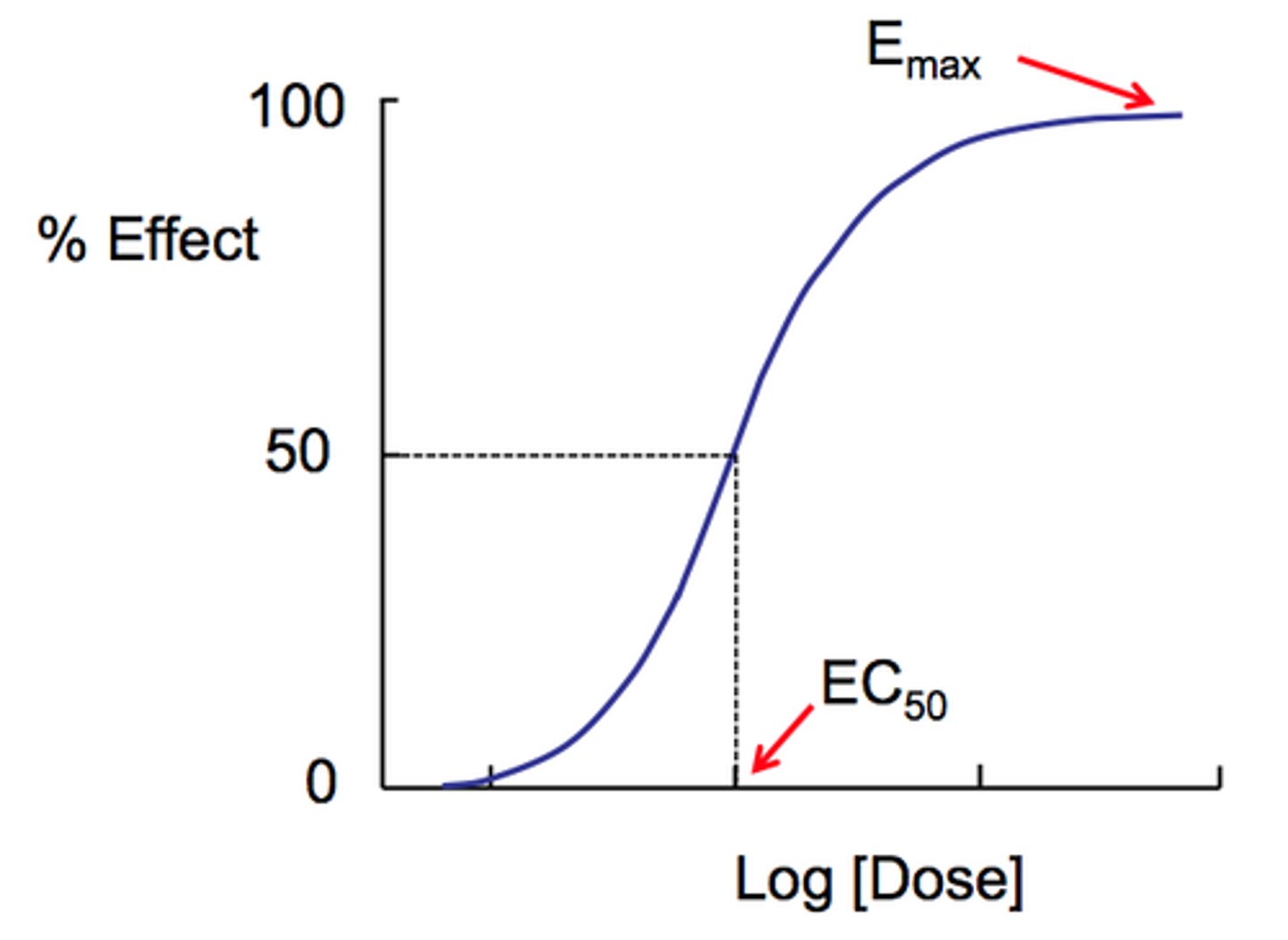
ED50
Effective dose in 50% of the population
graded response
effect of various doses on an individual
quantal response
all or none response; effect of various doses on population
as concentration of a drug increases, magnitude of its effect........
increases
Graded dose-response curve
illustrates relationship between the drug dose, receptor occupancy, and magnitude of resulting physiologic effect
maximum response
when all receptors are fully occupied
half-max response
when 50% of functional receptors are occupied
What does a low ED50 indicate?
more potent drug
Potency versus Efficacy
potency measures strength while efficacy is the effectiveness (fentanyl is more potent than morphine, but they are equally efficacious at equipotent doses; morphine is more effective than tylenol)
what does a drug with high efficacy indicate?
more therapeutically beneficial than one that is more potent
TD50
toxic dose in 50% of the population
LD50
lethal dose for 50% of the population
is a high or low therapeutic index preferred?
high; you would want to take a MUCH higher dose to reach TD50 compared to ED50
therapeutic index
the ratio between the toxic and therapeutic concentrations of a drug
TI formula
TI = TD50(or LD50)/ED50!!!!!!!!
narrow TI drugs
small dose range between what is effective and lethal
idiosyncratic drug response
drug response that is unanticipated/uncommon for the type of drug and its typical use and outcome; cannot be explained pharmacologically
Hypo-reactive or Hyper-reactive Response
intensity of effect of a given dose of drug is diminished OR increased compared to what is typically seen (ex: benedryl excitation or drowsiness)
tolerance
diminished response to a dose of a drug with continued use (opioids, stimulants, alcohol)
Tachyphylaxis
rapid decrease in response to a drug; increasing dose doesn't increase response; sometimes caused by depletion/reduction of neurotransmitter responsible for creating the drug's effect (common in amphetamines)
4 mechanisms of response that may contribute to variation in drug responsiveness
1. alteration in drug concentration that reaches receptor
2. variation in endogenous ligan concentration
3. alteration in number and function of receptors
4. changes in components of response downstream of the receptor
what causes alteration in drug concentration that reaches receptor?
pharmacokinetic factors: absorption, distribution, metabolism, excretion
other factors: age, gender, weight, disease state, genetics, change in active transport
Desensititzation
repeated or continuous admin of agonist/antagonist may lead to changes in responsiveness of receptor; receptors are still present but become desensitized to drug action (refractory period)
rebound phenomenon
body increases number of receptors in critical cells and tissues maintain homeostasis in response to a drug; if the drug is withdrawn, pt will have increased available receptors causing an exaggerated response
Beneficial and Toxic Effects Mediated by the Same Receptor-Effector Mechanism
when the intended effect of the drug also causes toxicity because of its direct intended effect (warfarin can cause too much blood thinning leading to stroke)
Beneficial and toxic effects mediated by identical receptors but in different tissues or by different effector pathways
certain drugs which are used to treat an issue in one area of the body (prednisone for COPD) can cause toxicities in other areas bc they bind to receptors elsewhere (increase glucose--> DM, fluid retention)
Beneficial and toxic effects mediated by different types of receptors
by making drugs more selective to ONE receptor, you can eliminate unintended effects and keep intended ones
Clinical sensitivity
relative to how many different receptor types a drug can interact with