Mod 2 exams
1/154
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
155 Terms
CHAPTER 18
BREASTS, AXILLAE, AND REGIONAL LYMPHATICS
SURFACE ANATOMY
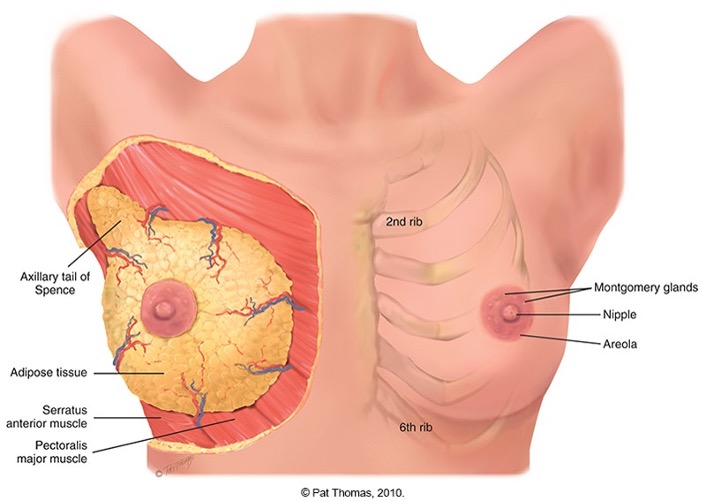
Breasts lie anterior to pectoralis major and serratus anterior muscles.
Located between second and sixth ribs, extending from medial side of sternum to midaxillary line.
Tail of Spence: Superior lateral corner projects up and laterally into axilla
Areola surrounds nipples 1-2 cm and enlarges during pregnancy.
Montgomery’s Glands: Small elevated sebaceous glands. Secrete protective lipid material during lactation
BREAST SURFACE ANATOMY
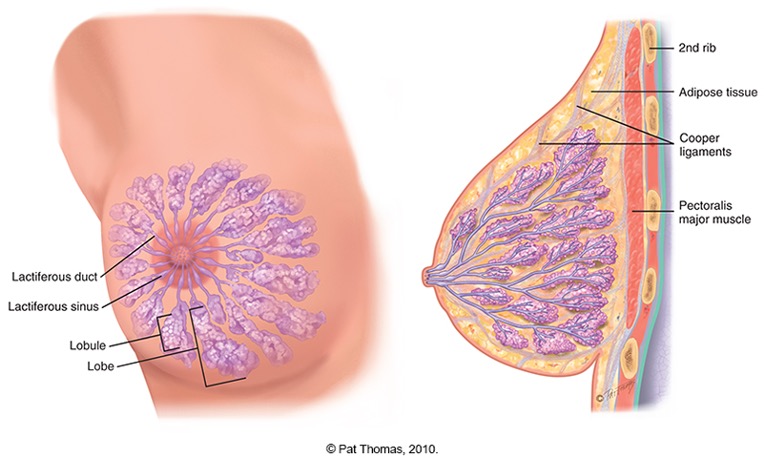
Breast is composed of:
•glandular tissue
•fibrous tissue, including suspensory ligaments.
•adipose tissue.
Glandular tissue contains 15 to 20 lobes radiating from nipple, and these are composed of lobules.
The suspensory ligament(Cooper ligament) are fibrous connective tissue extending vertically from the skin surface to attach on chest wall muscle.
The lobes are embedded in the adipose tissue. these layers of subcutaneous and retromammary fat actually provide most of the bulk of breast.
BREAST INTERNAL ANATOMY
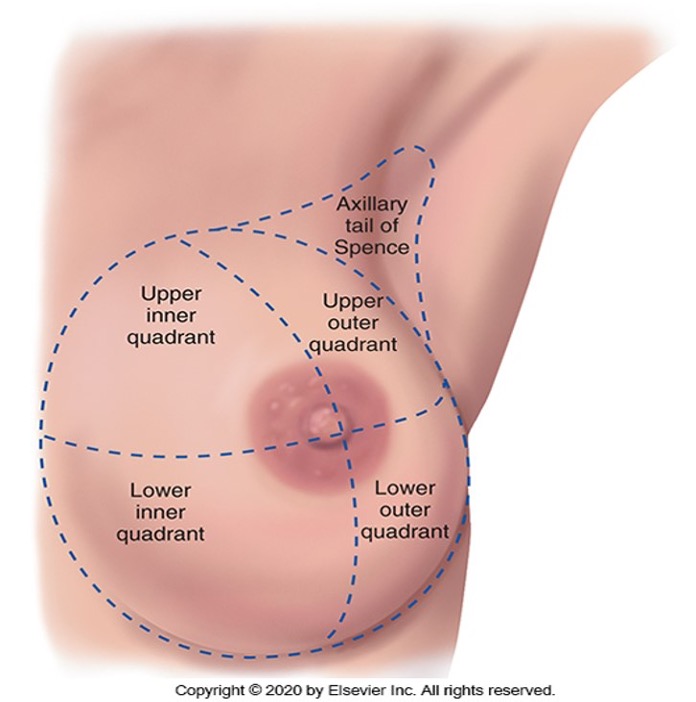
Breast may be divided into 4 quadrants.
Upper outer quadrant
Upper inner quadrant
lower outer quadrant
lower inner quadrant
Upper outer quadrant: The Tail of Spence, the cone-shaped breast tissue that projects into the axilla, is the site of most breast tumors.
REGIONAL LYMPHATICS
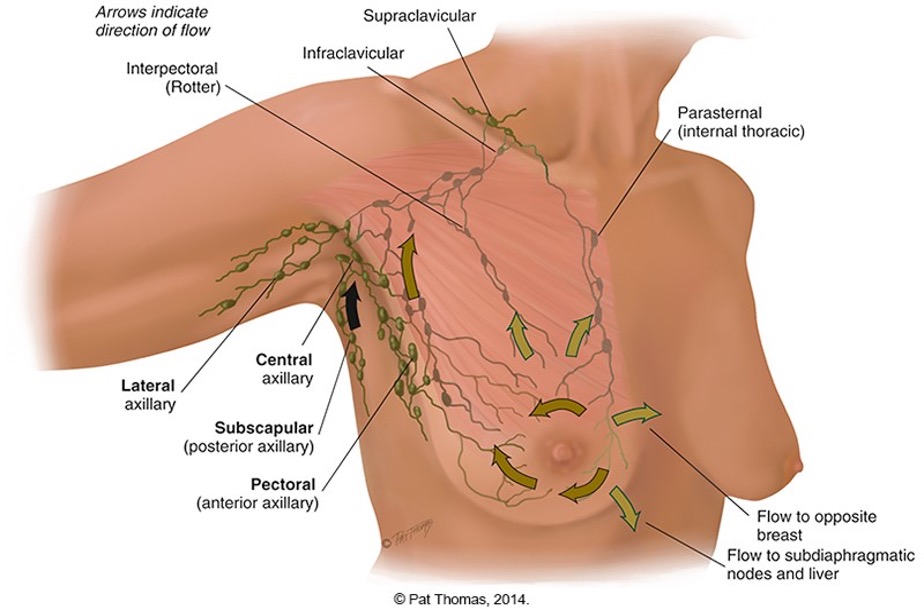
The breast has extensive drainage.
Most lymph, more than 75% drains into the lipsilateral(same side) axillary nodes.
4 group of axillary nodes are present
central axillary node- high up in the middle of the axilla over the rib and serratus anterior muscle.
pectoral- (anterior)
Subcapular-(posterior)
Lacteral- along the humerus
peau d’orange
lymphatic obstruction that produce edema, which thicken the skin and exagerates the hair follicles. the skin has pig skin or orange peel appearance- this condition suggest cancer
Supernumerary nipple
extra nipple that is visible somewhere along the track of the mammary ridge.
DEVELOPMENTAL COMPETENCE: AT BIRTH
Only Breast structure present are the lactiferous ducts within the nipple. the nipple are flat, rise above the skin, no alveoli is developed
DEVELOPMENTAL COMPETENCE: ADOLESCENT
At puberty, estrogen stimulates breast changes.
the breast enlarges as a result of fat deposition
Temporary asymmetry: Occasionally one breast may grow faster than other-tenderneess is common..
onset of breast development is between 8 and 9 for african american girl and 10 yrs for white female
Tanner 5 stages of breast growth/ maturation
Preadolescent-only a small elevated nipple
Stage 2 breast buds-the areola widens
Stage 3-the nipple is flushed with the breast surface
Stage 4- the areola and nipple form a secondary mound over the breast.
Mature breast- only the nipple protrudes
Menarche (menstruation) occurs in either stage 3 of 4 of Thelarche(breast development)
overweight girls under age 8 can develop breast bud
DEVELOPMENTAL COMPETENCE: NONPREGNANT WOMEN
breast of non pregnant women change with ebb and flow hormones during the monthly mentral cycle.
nodularity increases from midcycle to menstration
during the 3-4 days before mentration the breast feels full, tight, heavy and occasionally sore.
DEVELOPMENTAL COMPETENCE:FOR PREGNANT WOMEN
breast start to change during the 2nd month- common sign of pregnancy.
the nipple grows larger, darker and more erectile.
The areola becomes larger and darker brown as pregnancy progress.
tubercles becomes more prominent
after the 4th month colostrum may be expressed- rich in antibodies.
Mastitis
stems from an infection or stasis caused by plugged duct symptoms include: fever, redness, tenderness, swollen, hot and hard breast.
DEVELOPMENTAL COMPETENCE:
MALE BREAST
Rudimentary structure consisting of a thin disk of undeveloped tissue underlying nipple.
Gynecomastia: during adolescence, it is common for breast tissue to temporarily enlarge.
Condition is usually unilateral or bilateral and temporary.
Reassurance is necessary for adolescent male, whose attention is riveted on his body image.
occurs in adolescent age 13 or 14 yr
May reappear in aging male and may be due to testosterone deficiency.
Gynecomastia occur with use of anabolic steroids, some medication, cirrhosis, cushing syndrome, hyperthyroidism, adrenal disease, liver cirrhosis, alcohol, marijuana, antibiotic, estrogen, ACE inhibitors, TCA
early spread of cancer to the axillary lymph node is related to minimal breast tissue
CULTURE AND GENETICS:
BREAST CANCER
•Review statistics of breast cancer morbidity, mortality, and prognosis.
•Tumor supressor gene: BRCA1 and BRCA2 mutation - high risk of developing breast or ovariian cancer.
72% for BRCA1
17% for BRCA2
•Survival varies by stage when diagnosed.
•Consider family history, ethnicity, and other environmental variables- Ashkenazi jews have high risk to caucausians.
white people have greater incidence of breast cancer starting age 45, but black people have greater incidence of having cancer before age 45
•Racial disparity in survival
•Socioeconomic conditions affecting access to health care
•Screening mammography recommendations
•Review lifestyle risk factors:
alcohol drinking
weight gain
smoking
age<65
never brestfed a child
early menarche
height(tall)
late menopause(>55)
personal hx of breast cancer
no full term pregnancy
having a first degree relative with breast cancer(mother, sister, daughter)
SUBJECTIVE DATA: HISTORY
•Breast
•Pain, lump, and discharge
•Rash, swelling, trauma
•History of breast disease
•Surgery or radiation
•Medications
•Patient-centered care
•Perform breast self-examination/last mammogram
•Axilla
•Tenderness, lump, or swelling
•Rash
SUBJECTIVE DATA: PAIN
•Any pain or tenderness in breasts?
•Onset
•Pain location
•Localized or diffuse
•Is painful spot sore to touch? Do you feel a burning or pulling sensation?
•Appearance of pain cyclic?
•Any relation to menstrual cycle?
•Precipitating factors
•Brought on by strenuous activity?
•Change in activity?
•Sexual manipulation?
Symptoms
•Lump- cause by injury is caused by localized hematoma, resolves quickly.
•Discharge
•Rash
•Swelling
•Trauma: Mastalgia- occurs with trauma, inflammation, infection and benign breast disease.
•History of Breast Disease- Paget disease starts with small crust in the nipple apex and spread to the areola. Eczema or any other skin disease rarely starts at the nipple but starts at the areola pr surrounding skin.
•Surgery or Radiation
•Medications: Galatorrhea - medication can cause clear lipid discharge include; oral contraceptives,diuretics, phenorthiazides, digitalis, sterriods, methyldopa, calcuim channel blocker.
cyclic pain: Cyclic pain is common with normal breast, oral contraceptives and benign breast(fibrocystic) breast
SUBJECTIVE DATA:PATIENT-CENTERED CARESUBJECTIVE DATA:
PATIENT-CENTERED CARE
Ask about self-breast exam (SBE)
Teaching moment to review basics of examination
Review screening guidelines recommendations based on age and patient history
American Cancer Society
Begin at ages 40 to 44, screening mammography
Annual mammography from ages 45 to 54
Biennial mammography over age 55 or continuation of annual
RISK PROFILE FOR BREAST CANCER
Breast cancer is second major cause of death from cancer in women.
However, early detection and improved treatment have increased survival rates.
Review factors associated with “relative risk”
RR above 1 indicates a higher likelihood of occurrence among exposed than unexposed persons.
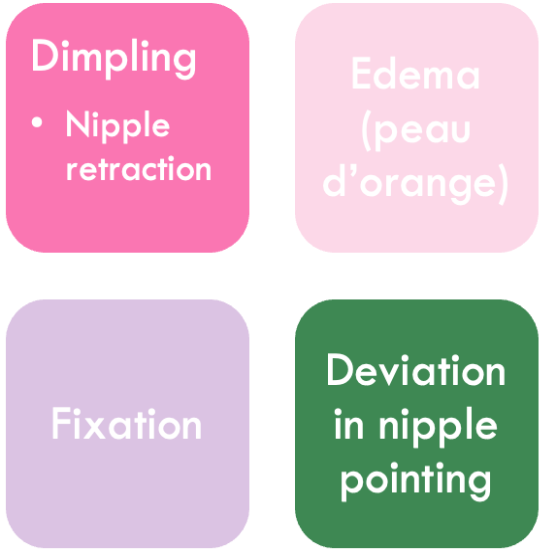
Inspection of the breast
Size: sudden increase in size of breast signifies new growth or inflammation.
Color- unilateral dilated superficial veins in nonpregnant women.
fine blue vascular network and stretch mark is present with pregnancy.
Retraction-retraction occurs with signs of fibrosis in breast tissue- breast is flatter and broader
recent nipple retraction signifies aquired disease
CHARACTERISTICS OF LUMP OR MASS
•Location
•As with clock face, describe distance in centimeters from nipple; or diagram breast in woman’s record and mark in location of lump.
•Size
•Judge in centimeters in three dimensions: width, length, and thickness.
•Shape
•State whether lump is oval, round, lobulated, or indistinct.
•Consistency
•State whether lump is soft, firm, or hard.
•Movable
•Is lump freely movable or fixed when you try to slide it over chest wall?
•Distinctness
•Is the lump singular or multiple?
•Nipple
•Is it displaced or retracted?
should be symmetrically placed on the same plane on the two breast, with deviation it indicated underlying cancer which may cause fibrosis in mammary duct.
•Skin over lump
•Is it erythematous, dimpled, retracted?
•Tenderness
•Tender to palpation?
•Lymph…
•Are regional lymph nodes palpable?
Palpating the breast an axillae
when palpating the axillae use your right hand to palpate the left axilla
move them firmly into 4 directions
down the chest wallfrom the middle to the axillae
along the anterior border of the axilla
along the posterior border
along the inner aaspect of the upper arm
(nodes are not palpable)
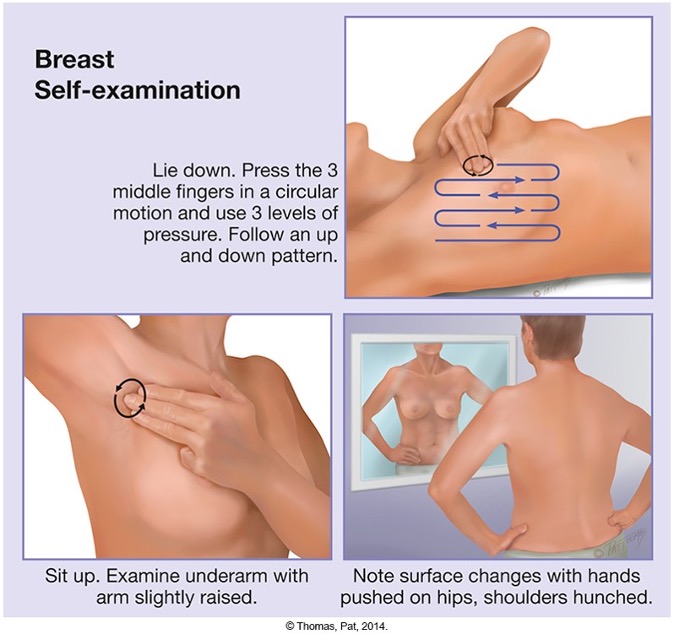
When palpating a woman’s breast assit them to a supine position with their arm raised above their head.
use pad of your 3 finger and make a gentle rotary motion on the breast.
palpate light, medium, deepin each location
vertical strip pattern identifies breast mass
start high axilla and palpate down midaxillary line just lateral to the breast down to the bra line.
in nulliparous women(women who have not given birth yet) their breast feel firm, smooth, and elastic.
in pregnant women breast feel soft and loose, in premenstral engorgement, slight enlargement, tenderness and heneraluzed nodularity is normal
in postmenenopausal women size of their breast decreases the breast seem flat and flabby due to the decrease hormones which causes atrophy of the glandular tissue in the breast.
when checcking for retraction during breast examination ask the woman to slowly lift her arms above her head and note for retraction or lag in movement
Inframmammary ridge
Common with large breast. its a firm tranverse ridge of compressed tissue in the lower quadrant. for women with large breast use a bimanual technique to palpate the breast.
physical changes associated with cancer
B-breast mass
R- retraction
E-edema
A-axillary mass
S-scaly nipple
T-tender breast
cancerous mass are solid, hard, dense and fixed to underlying tissue or skin, border is irregular and poorly delineated as cancer becomes invasive.
TEACH BREAST SELF-EXAMINATION (BSE)
best time to perform BSE is day 4-7 after the first day of the mentral cycle.
when the breast are small and least congested.
for pregnant and menopausal women they should choose a familiar date such as the 1st of every month.
ABNORMAL FINDINGS:
SIGNS OF RETRACTION AND INFLAMMATION
ABNORMAL FINDINGS:
BREAST LUMPS
Benign (Fibrocystic) breast disease- makes it hard to examine the breast, the lumpiness of the breast conceals a new lump.
Cancer
Fibroadenoma
Differentiating breast lumps:
Age
Shape, consistency, and demarcation
Number, mobility, and tenderness
Skin retraction
pattern of growth
risk to health
CHAPTER 19
THORAX & LUNGS
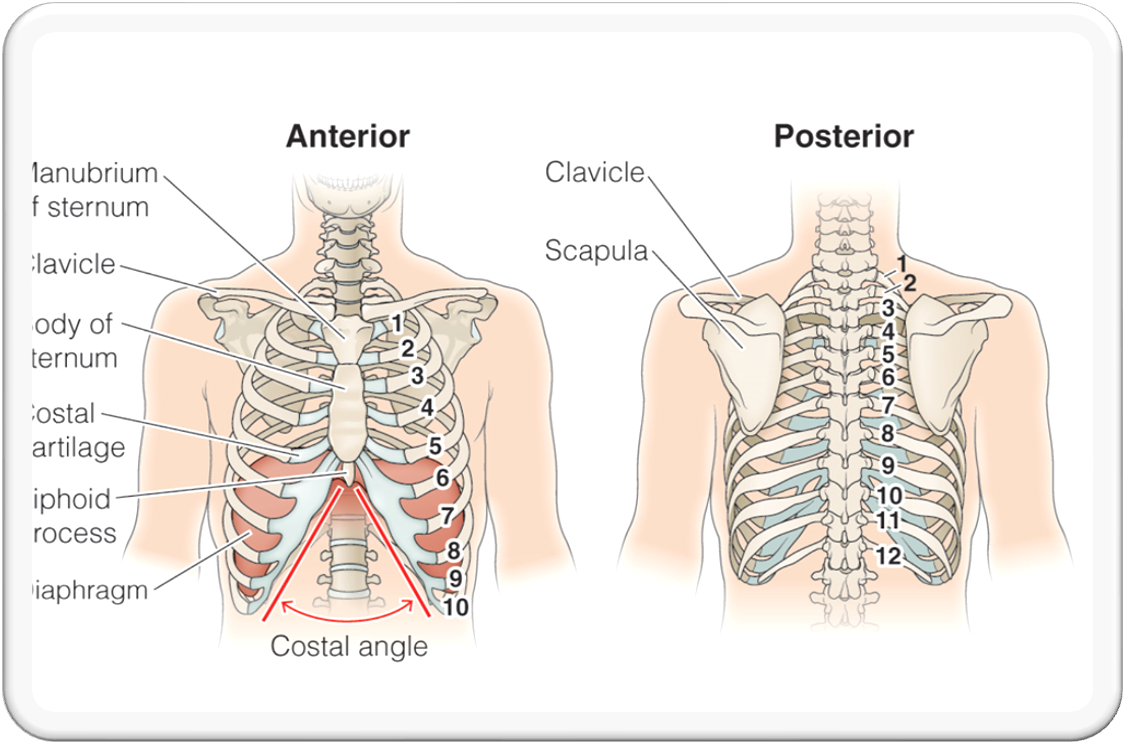
The Thoracic cage
bony structure with conial shape, its defined by sternum, 12 pairs of ribs, 12 thoracic vetebrae and diaphragm.
The coschondral junction
Is the point at which the ribs join the cartilage. they are not palpable.
ANTERIOR THORACIC
Suprasternal notch- U shapped depression above the sternum.
Sternum: the breastbone has 3 parts
the manubrium
the body and
xiphoid process
Sternal angle often called the Angle of Louis
it is articulation of the manubriium and body of the sternum and it is continuous to the 2nd rib and slides down to the second intercostal space.
Angle of Louis marks site of tracheal bifurcation into the right and left main bronchi, it corresponds with upper border atria of the heart, and lies above the fourth thoracic vetebra on the back
Costal Angle: the right and left costal margin form an angle where thy meet at the xiphoid process. usually 90 degrees or less.
usually this this angle increases when the rib cage is oveinflated such as emphysema.
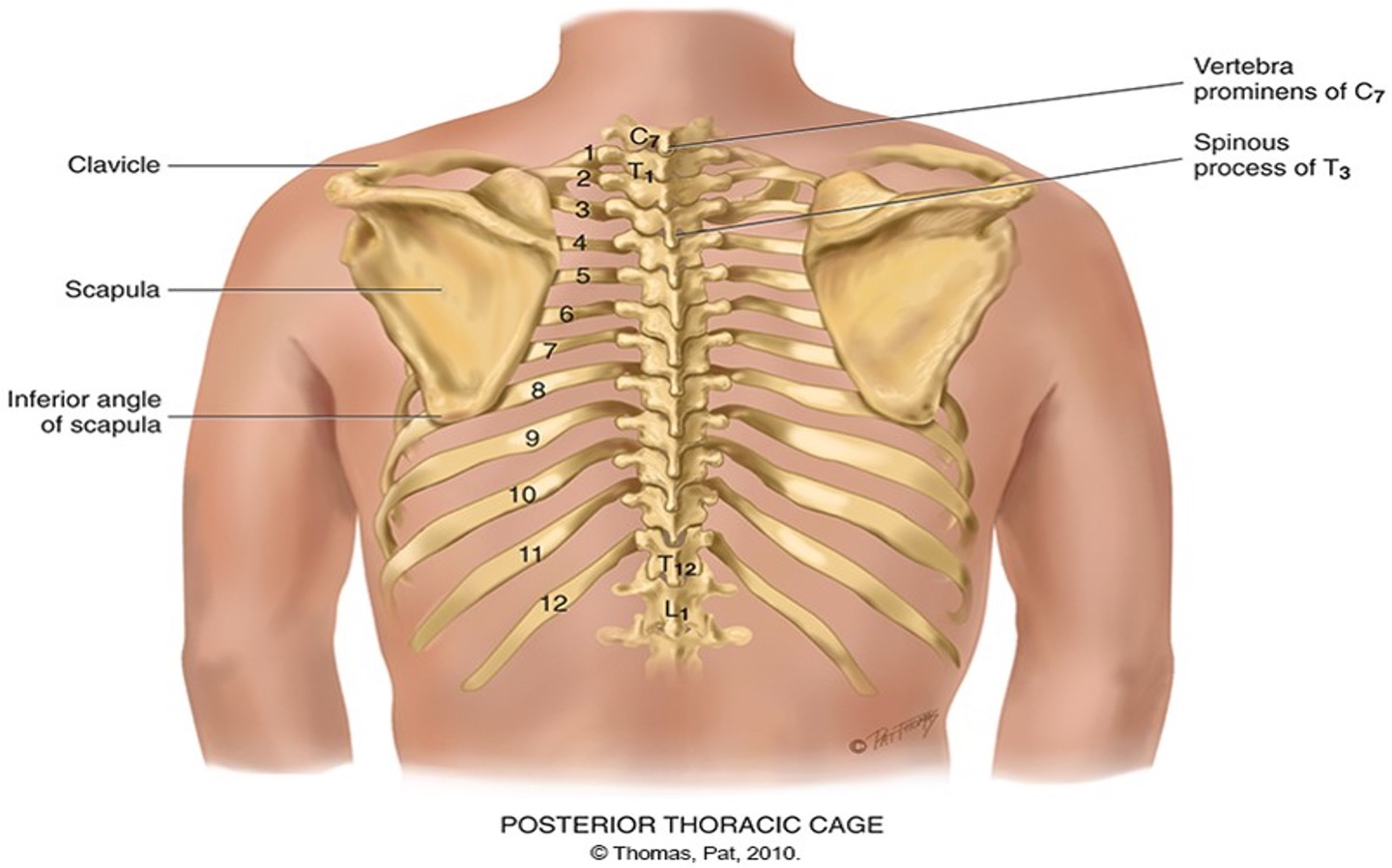
POSTERIOR THORACIC LANDMARKS
Vertebra Prominus: most prominent bony spur protruding at the base of the neck. upper C7 and lower T1.
Spinous process: aligns with the same number rib, only down to T4, after T4 the spinous process angels downward from the vetebral body.
The inferior body of the scapula: located symmetrically in each hemithorax. the lower tip is usually at the 7th and 8th rib.
Twelfth Rib: palpate midway between the spine and the person ‘s side to identify its free tip.
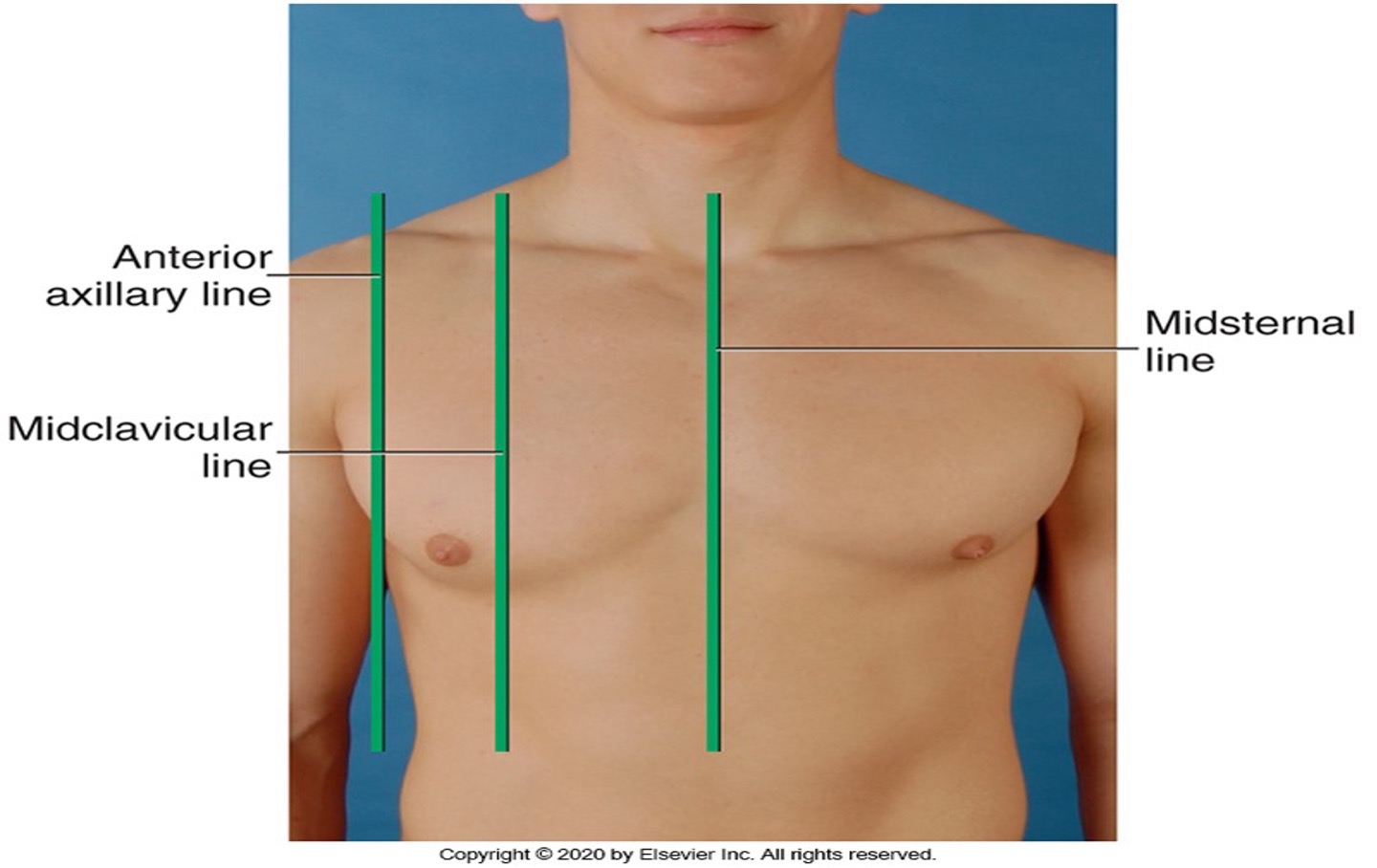
ANTERIOR REFERENCE LINES
Midsternal line
Midclavicular line- center of each clavicle at the point halfway palpated stenoclavicular and acromioclavicular joint
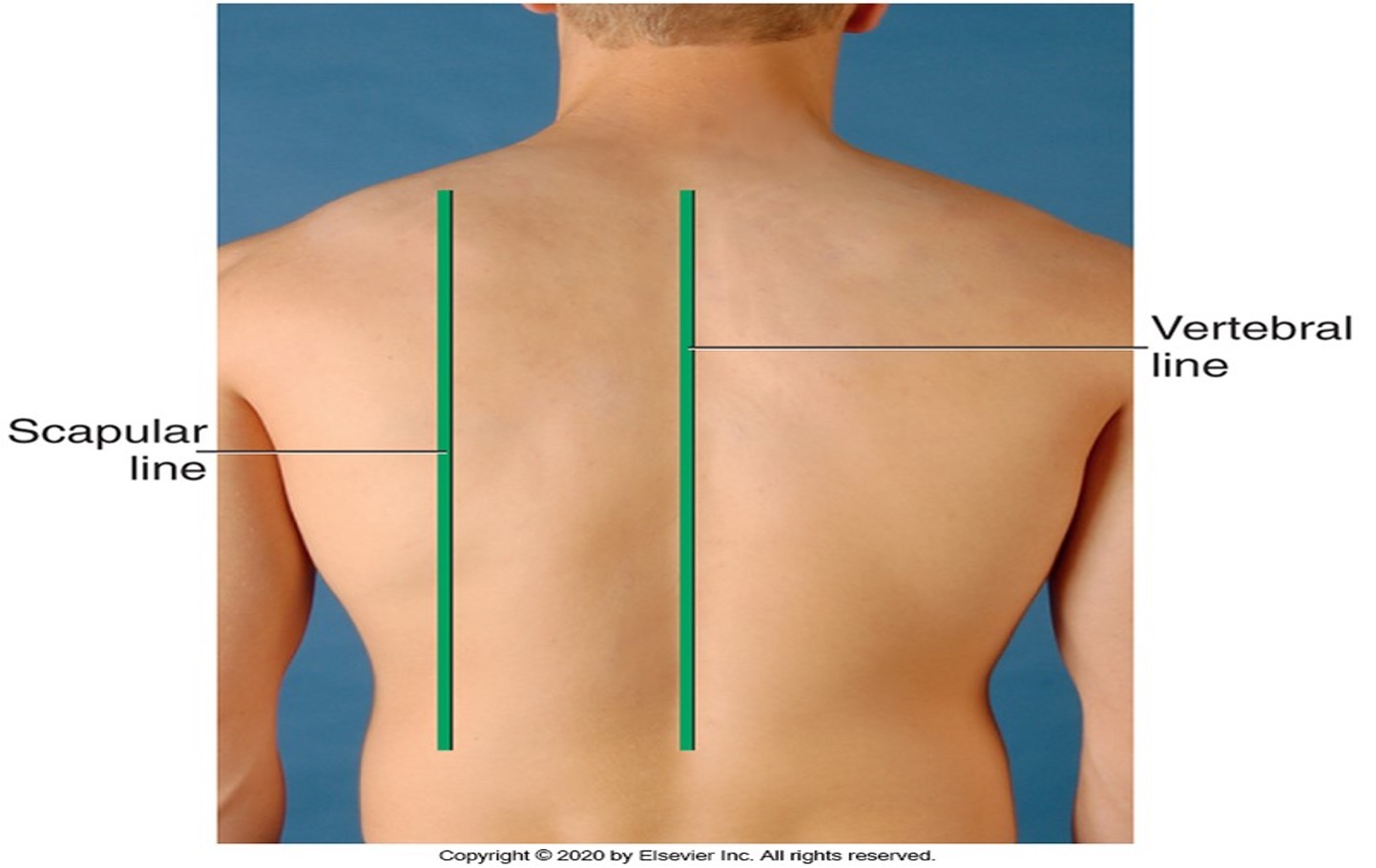
POSTERIOR REFERENCE LINES
vertebral or midspinal line
Scapular line
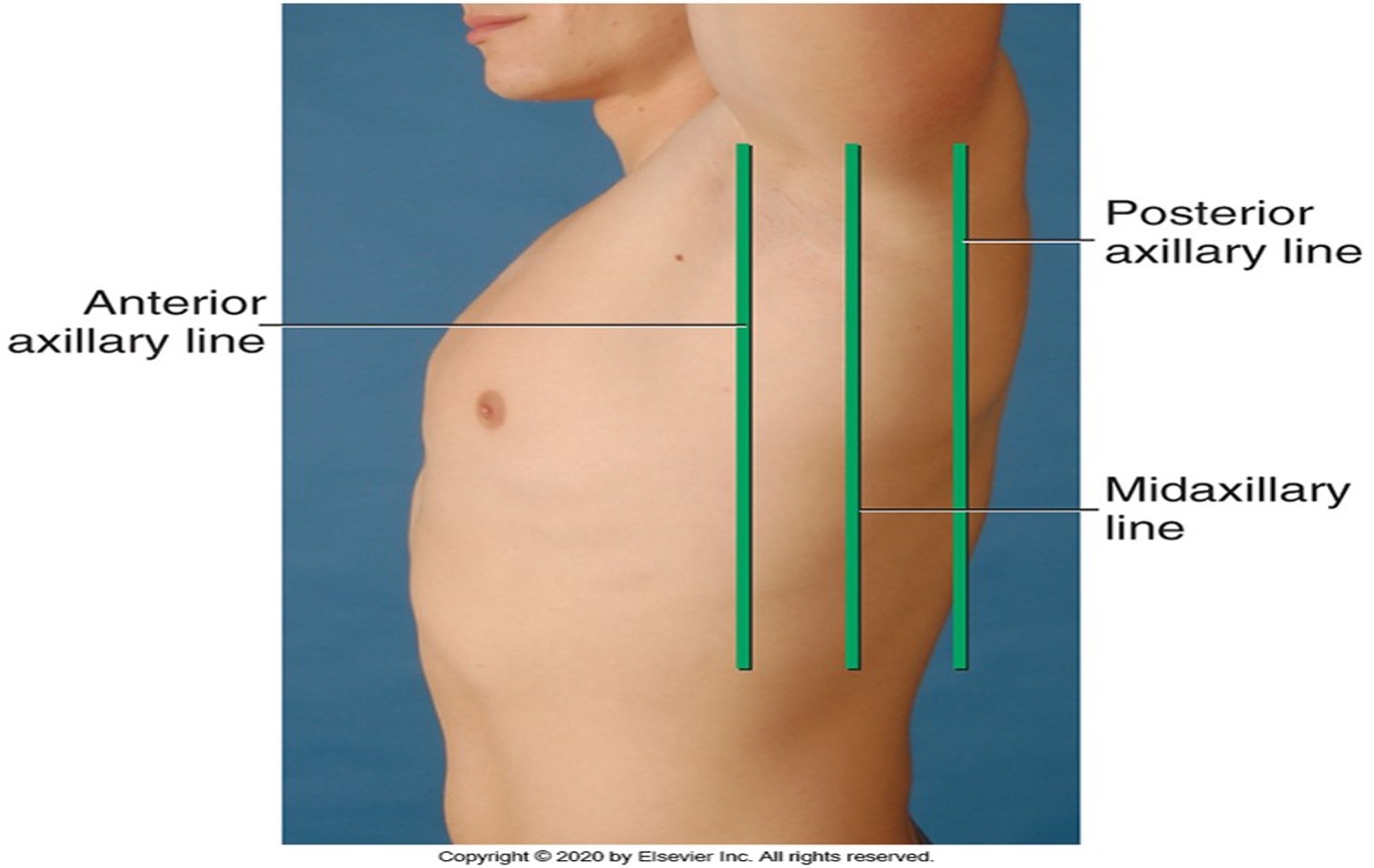
LATERAL REFERENCE LINES
90” arm up and divide the lateral chest by three line
anterior axillary- folds where the pectoralis muscle insert
posterior axillary- fold where the latissimus doors muscle inserts
midaxillary lineruns down from the apex of the axilla and lies between parallel to the other two.
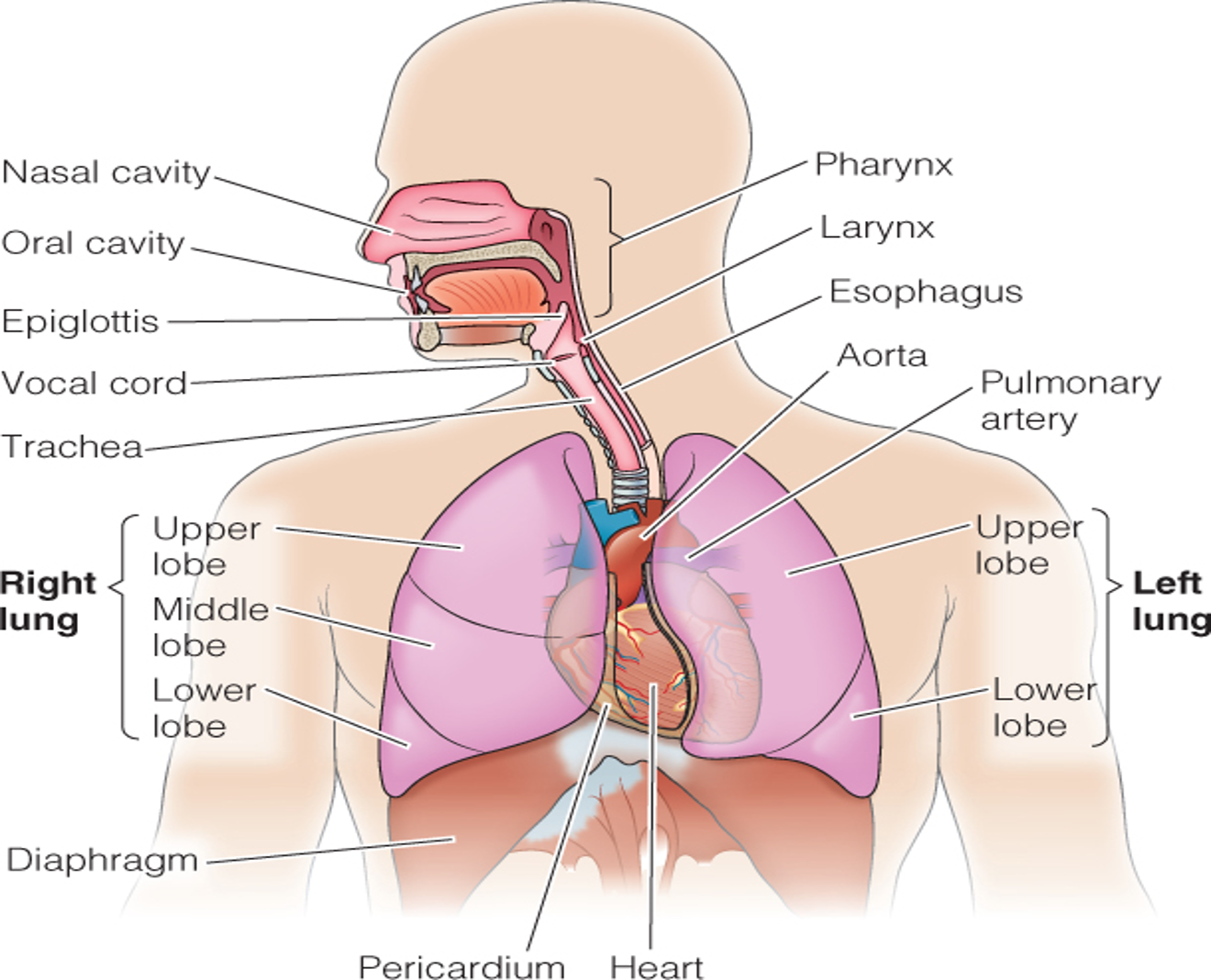
THORACIC CAVITY
Mediastinum: middle section of the thoracic cavivity that contains the esophagus, trachea, heart and great vessels.
the right and left pleural cavities contain the lungs
The Lung border
lung borders at apex, base, lateral and posterior positions.
LOBES OF THE LUNG
The lobes are seperated by fissure that run oblique through the chest.
LEFT LUNG
Bi-lobar: 2 lobes
•LUL, LLL
•Narrower due to heart
Anterior contains primarily upper lobe.
Posterior chest contains almost all lower lobe.
L Lateral view: both lobes
has no middle lobe
Right Lung
Three Lobes:
RUL, RML, RLL
Shorter due to liver
Anterior chest contains mostly upper and middle lobes with very little lower lobe.
Posterior chest contains almost all lower lobes.
R Lateral view: All three lobes
PLEURAE
PLEURAE: membranes form an envelope between lungs and chest wall.
VISCERAL PLEURA – lines outside of the lungs
PARIETAL PLEURA – lines inside of the chest wall & diaphram
PLEURAL CAVITY – The inside of the envelope – space between visceral & parietal pleura, lubrication; Normally has a vacuum, which holds lungs tightly against chest wall.
The Trachea and bronchi
transport gases between the environment and lung parenchyma. they constitute the dead space or space that is filled with air but not available for gaseous exchange.
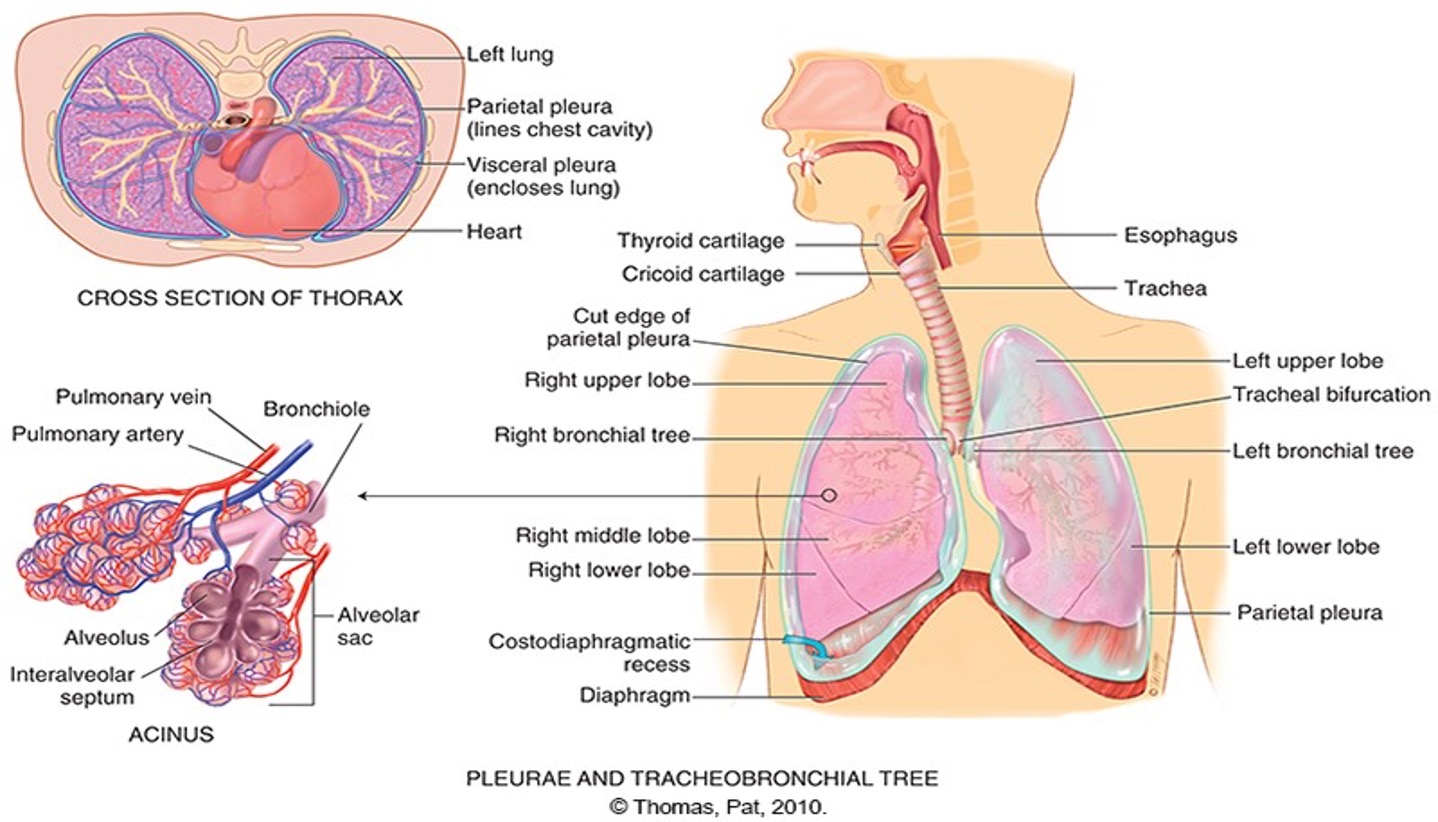 The Acinus
The Acinus
functional respiratory unit that consist of bronchioles, alveolar ducts, alveolar sac and alveoli.
MECHANICS OF RESPIRATION: FUNCTION
FOUR MAJOR FUNCTIONS OF RESPIRATORY SYSTEM:
1.Supplying oxygen to the body / energy production
2.Removing carbon dioxide
3.Maintaining homeostasis (acid-base balance) of arterial blood
4.Maintaining heat exchange
•By supplying oxygen to blood and eliminating excess carbon dioxide, respiration maintains pH or acid-base balance of blood – prevent acidosis or alkalosis
Hypoventillation causes build up of CO2 in the blood and Hyperventilation causes CO@ to be blown off
Control of respiration
involuntary control is mediated by respiratory center in the brainstem- pon and medulla.
The major feedback loop is humoral regulation
normal stimulation to breathe in most of us is increase CO2 in the blood or hypercapnia. a decrease in oxygen in the blood hypoxemia also increases the respiration but less effective.
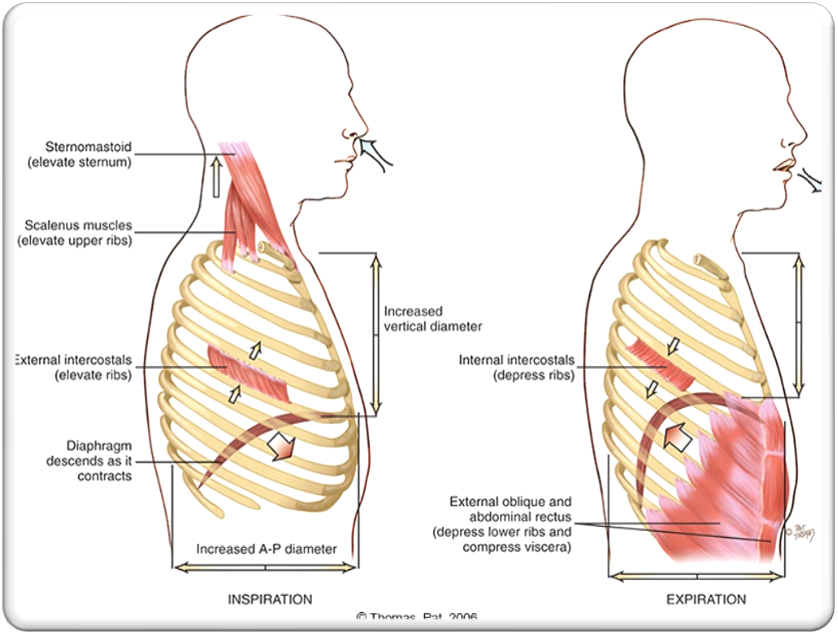
Changing chest size
•The major muscle used for respiration is the diaphragm. The intercostal muscle lifts the sternum and elevate the ribs during inspiration, increasing the anteroposterior diameter.
Inspiration – Active
During inspiration, contraction of the bell shaped diaphragm causes it to descend and flatten
•Exhalation- Passive
as the diaphraphm relaxes elastic force within the lungs, chest cage and abdomen causes it to dome up.
Forced inspiration
after heavy exercise or occuring pathologically with respiratory distress causes the the use of accessory muscle to heave up the sternum and rib cage.
can be voluntary or involuntary
MECHANICS OF RESPIRATION
CONTROL OF RESPIRATIONS
Feedback loop – Involuntary control by respiratory center in the brain stem consisting of the pons & medulla.
•Hypercapnia is an increase in the CO2 in the blood. And provides the normal stimulus to breathe.
•Hypoxemia
CHANGING CHEST SIZE
1.Air rushes into the lungs as chest size increases (inspiration) diaphragm contracts and drop
2.Air is expelled from lungs as chest recoils (expiration) and diaphragm relaxes.
Mechanical expansion and contraction of chest cavity alters size of thoracic container in two dimensions: vertical diameter and anteroposterior diameter.
Developmental competence
Infant and children:
first 5 weks of fetal life the primitive lung bud emerges
16 wks the conducting airway reaches that of the adult
32 wk surfactant is present
when the newborn inhale the first breath its follows by a lusty cry. aucultate fine crackles as a result of opening their airwayd and clearing fluid
if a mother smokes during pregnancy, the baby has an increase risk of lower birth weight, decrease head growth,and SIDS.
after birth of an infant experience second hand smoking, they are at risk for upper and lower respiratory infection such as otitis media, asthma, tooth decay, hearing loss, and metabolic syndrome, and later ADHD etc.
The Pregnant woman
enlarge uterus elevates the diaphragm by 4cm
increase in estrogen level relaxes the the chest cage ligaments
the total circumference of the chest cage is increase by 6cm.
although the diaphragm is elevated its not fixed because it moves with breathing even more during pregnancy, which results in 40% increase tidal volume.
increase awareness of the need to breathe develops in early pregnancy.
The Aging Adult
costal cartillage becomes more calcified thus the thorax is less mobile.
the elastic properties within the lungs become less distensible
increase in small airway closure decrease vital capacity and increase residual volume.
gradual loss of intraalveolar septa and decrease number of alveoli
this put them at risk for pulmonary complications.
lungs are less elastic and distensible which decrease their ability to collapse and recoil
NORMAL RANGE OF ABG
Ph = 7.35 – 7.45
PaCO2 = 35-45mmHg
Pa O2 = 80-100mmHg
SaO2 = 94*68%
Lungs help to maintain pH balance by adjusting the amount of CO2 through:
Hypoventilation
•Hyperventilation
RESPIRATIONS ACROSS THE LIFE CYCLE
INFANTS AND CHILDREN
INCREASED VULNERABILITY OF RESPIRATORY SYSTEM ASSOCIATED WITH
•ANATOMY & DEVELOPMENT
•ENVIRONMENTAL TOBACCO SMOKE (ETS) EXPOSURE
•INCREASED RATES OF ADOLESCENT SMOKING.
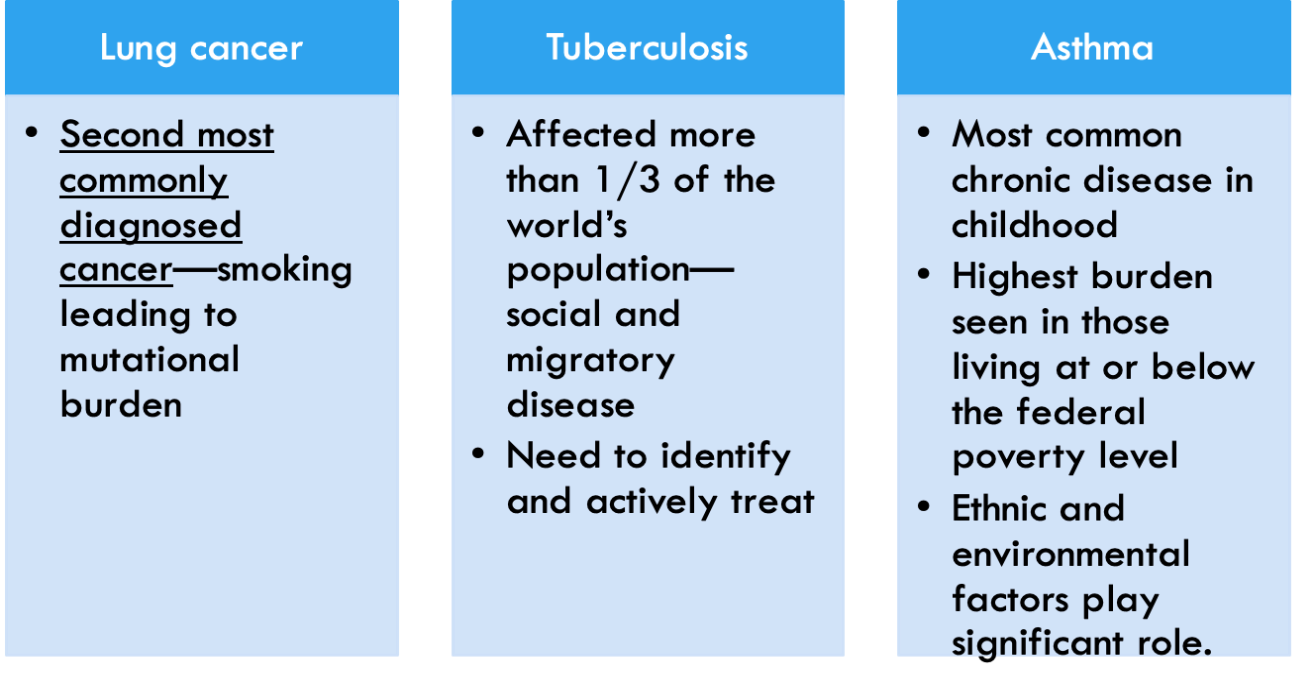
CULTURE AND GENETICS
lung cancer - 2nd leading dx cancer in both men and women. tabacco cause 90% of lung cancer
TB termed social and migratory disease, popular in countries with armed conflict.
Asthma most common chronic childhood disease.
ASSESSMENT: SUBJECTIVE DATA
•Cough
•Shortness of breath
•Chest pain with breathing
•History of respiratory infections
•Smoking history
•Environmental exposure
•Self-Care behaviors
COUGH
Do you have a cough? When did it start? Gradual or sudden
Ask about:
Duration
Frequency
Timing
Presence of cough as an irritating factor?
Cough productive or non-productive?
Identify related characteristics?
Quality of cough in terms of description?
Precipitating or alleviating factors
Treatments tried?
Rx and OTC medications?
Any associated symptoms?
Impact of cough on ADLs and quality of life?
SHORTNESS OF BREATH (SOB)
Ever had any shortness of breath or hard-breathing spells? Ask about
Precipitating factors
Severity
Duration
Impact of change of position?
Specific timing pattern?
Association with other clinical symptoms?
Triggering mechanisms r/t: food, environment, or emotion?
The measures taken when SOB occurs?
Treatment or medication both Rx and OTC?
Impact of sob on ADLs?
Progression of SOB?
CHEST PAIN WITH BREATHING
Any chest pain with breathing?
• Please point to exact location.
Onset timing/Constant versus intermittent
Pain characteristics:
• quality - describe
• intensity - rate
Associated clinical symptoms?
Any treatment interventions used?
HISTORY OF RESPIRATORY INFECTIONS
Past history of breathing trouble?
Lung diseases:
Bronchitis
Emphysema
Asthma
Pneumonia?
Unusually frequent or unusually severe colds
Family history of:
allergies
tuberculosis- rust sputum, night sweat, low grade fever in the afternoon
asthma-allergic hypersensitivity
Smoking history
Onset
Duration
Pattern of smoking
Secondhand exposure to smoke
Smoking cessation
Counseling using the five A’s: Ask, Advise, Assess, Assist, and Arrange*
ENVIRONMENTAL EXPOSURE
Are there any environmental conditions that may affect your breathing?
Ask about:
Occupational factors and exposure?
Protection from exposure?
Monitoring and follow-up to exposure?
Awareness of symptoms that might signal breathing problems?
PATIENT-CENTERED CARE
SCREENING AND FOLLOW-UP TESTING
When was the last time you had the following?
TB SKIN TEST
CHEST X-RAY STUDY
PNEUMONIA OR INFLUENZA IMMUNIZATION
History for Aging Adult
•Have you noticed any shortness of breath or fatigue with your daily activities?
Ask about:
•Tell me about your usual amount of physical activity.
•(For those with a history of chronic obstructive pulmonary disease, lung cancer, or tuberculosis): use lung function questionnaire in next slide.
•How is your energy level?
•Do you tire more easily?
•How does your illness affect you at home and at work?
•Do you have any chest pain with breathing?
•Do you have any chest
OBJECTIVE DATA: PREPARATION AND EQUIPMENT
PROVIDE RESPECT AND COMFORT WHILE ALLOWING FOR ACCESS OF EXAMINATION TECHNIQUES.
•Inspection, palpation, percussion, and auscultation
•Usually do this after posterior thyroid exam: Posterior chest, Lateral chest, then Anterior chest.
EQUIPMENT
Stethoscope
Pulse Ox
Alcohol wipe
POSTERIOR CHEST
INSPECTION: THORACIC CAGE
•Shape and configuration of chest wall.
•Anteroposterior Diameter = Ratio 1:2
•Position of person to breath.
•Assess skin color and condition.
•Note any lesions; inquire about changes.
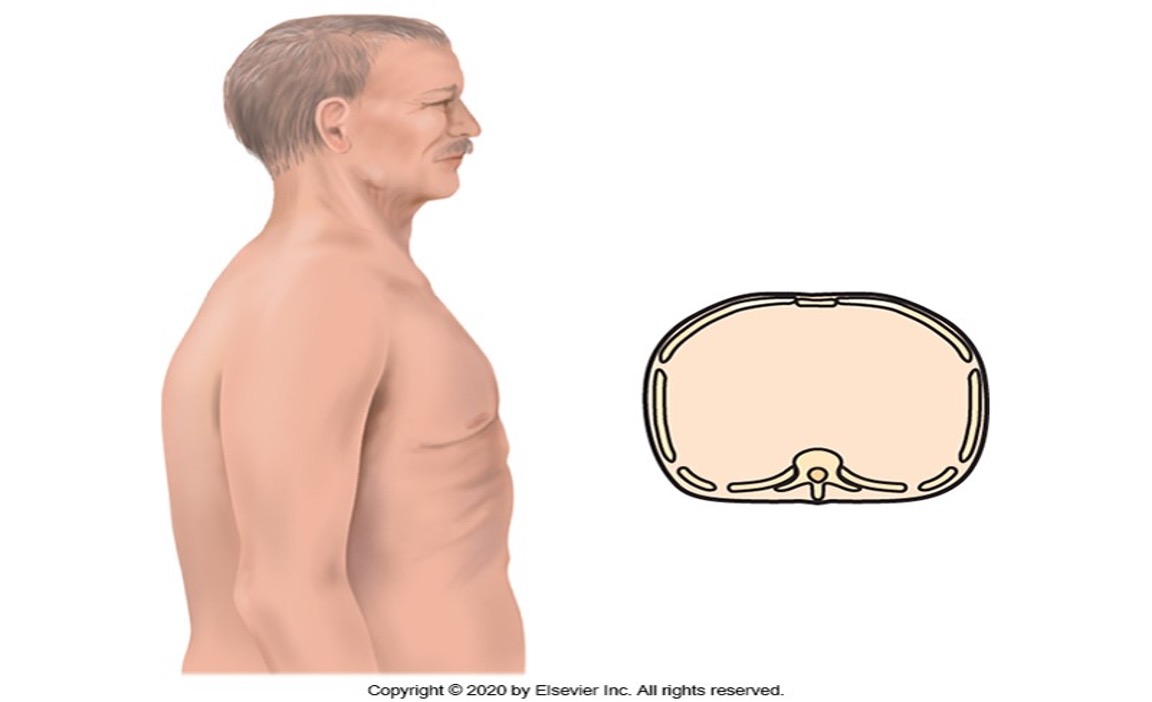
BARREL CHEST
An anteriorposterioe-to-posterior diameter ratio or barrel chest is obsereved in patients with COPD because of hyperinflation of the lungs. the ribs are more horizontal, and the chest appears as if held in continuous inspiration.
expected finding with a normal adult lungs
symmetric chest expansion
resonant percussion tone
vesicular breath sounds over the peripheral lung fields
muffled voice sound
POSTERIOR CHEST
PALPATION
Symmetric expansion—confirm by using hands @ T9-T10
Tactile Fremitus – Increased vs Decreased
•Palpate using the palmar base of the finger or the ulnar edge.
•Fremitus is most prominent between the scapulae and around the sternum
•Decreased = obstructed bronchi, pleural effusion, pneumo, emphysema
•Increased = consolidation (PNA)
•Palpate the entire chest wall
Crepitus – coarse, crackling sensation palpable over the skin surface; occurs when air escapes from lung into S/C tissue. (air in the subcutaneous tissue)
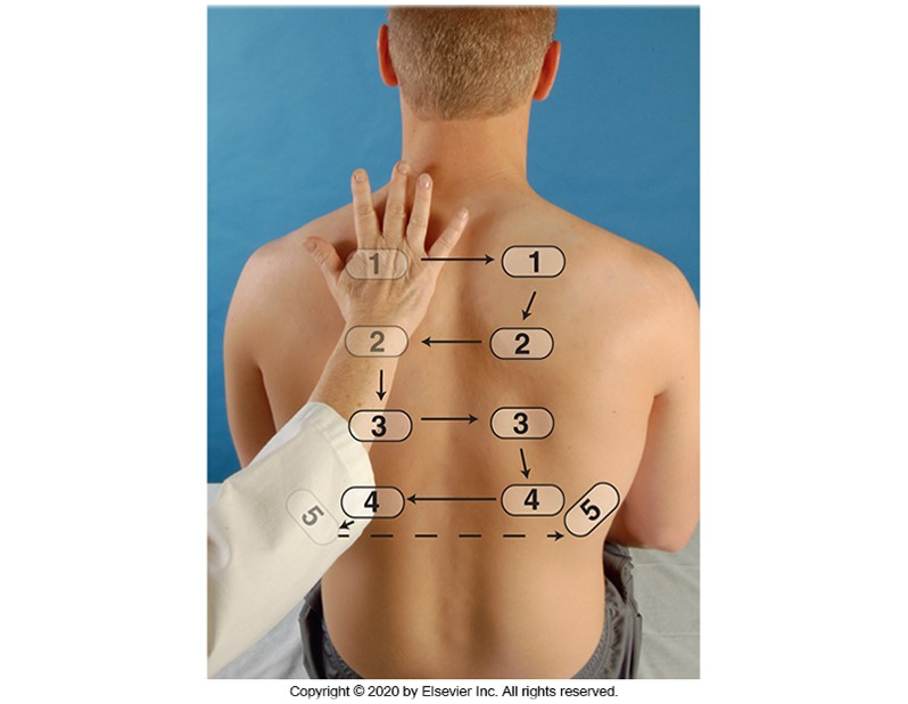
PERCUSSION: LUNG FIELDS
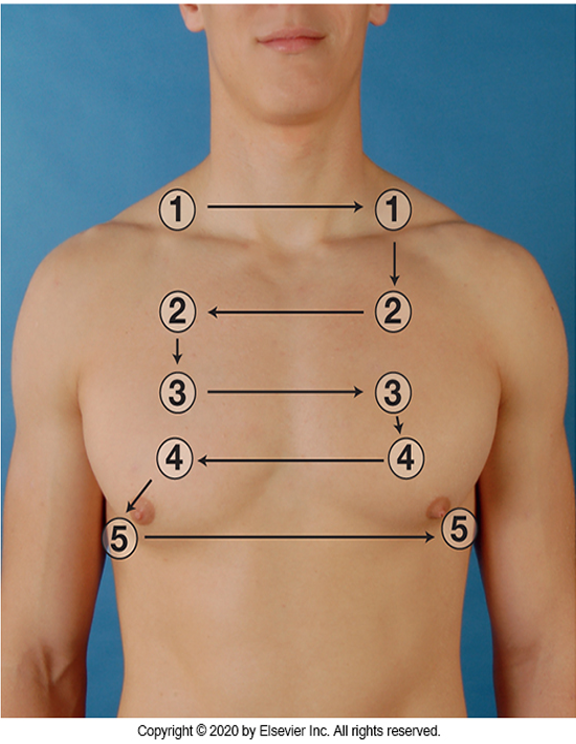
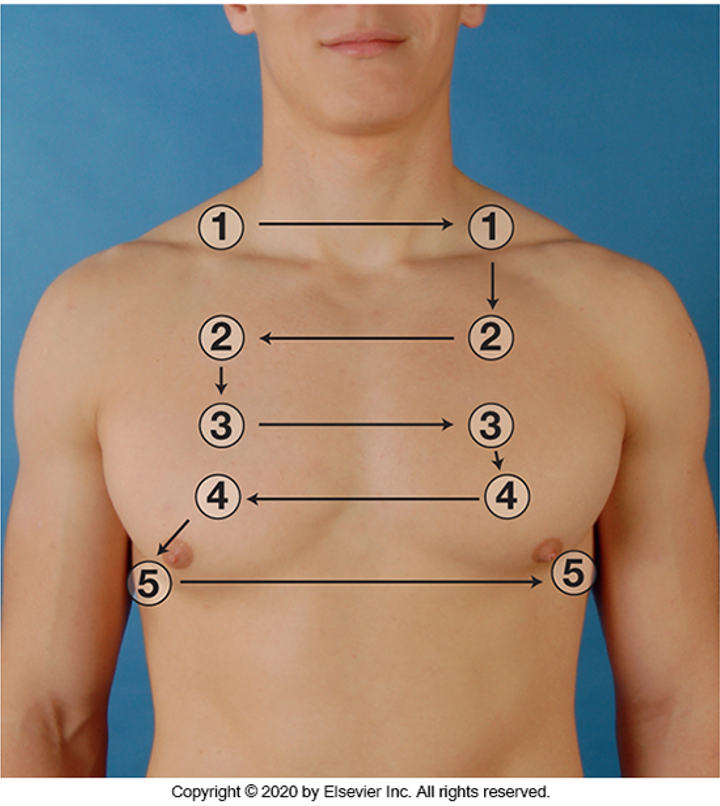
Start at apices, across shoulders, then interspaces side to side in 5cm intervals.
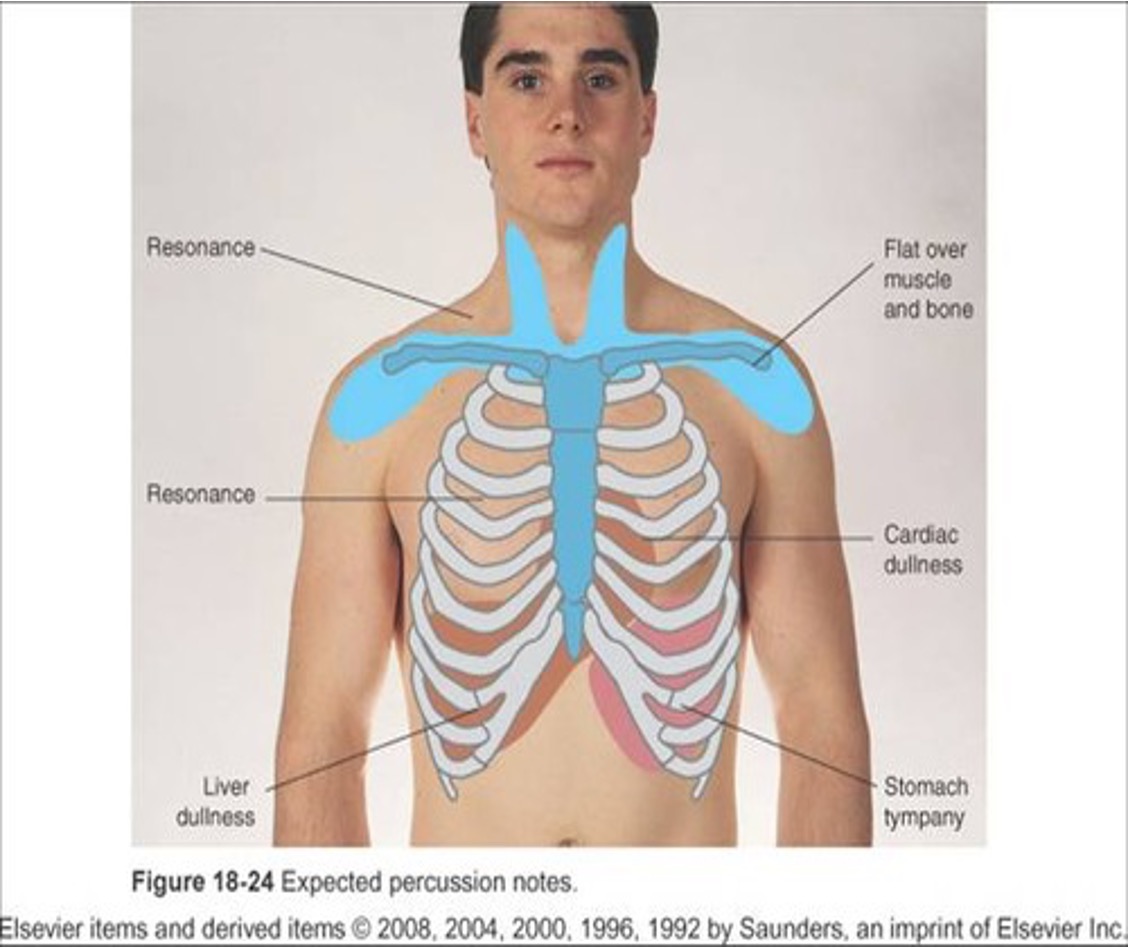
Resonance sound predominates in healthy lung tissue in adult.
Hyperresonance means too much air such as: emphysema, pneumothorax
Dull means abnormal density, pneumonia, tumor, atelectasis
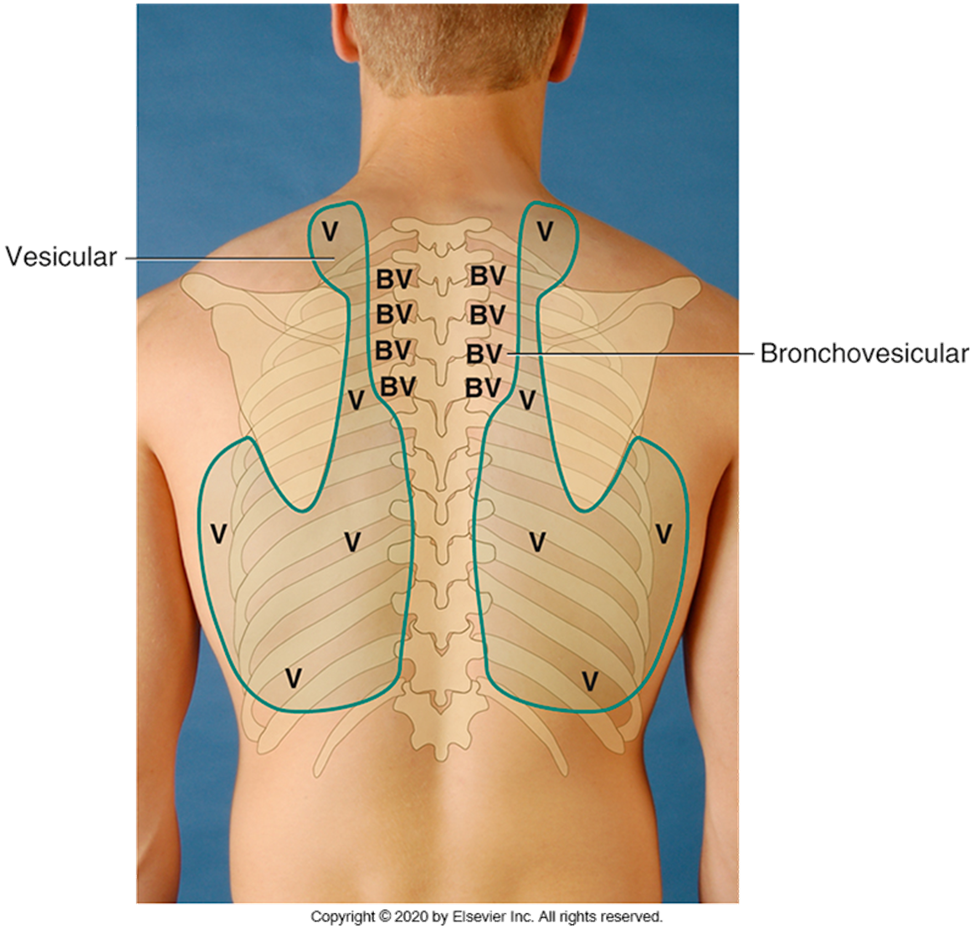
AUSCULTATION :
Have your patient breath through mouth and a little deeper than usual
Tell you if they become light headed
Use flat diaphragm to chest
Listen to 1 full respiration cycle
Compare both sides- from side to side
EXPECTED PERCUSSION NOTES
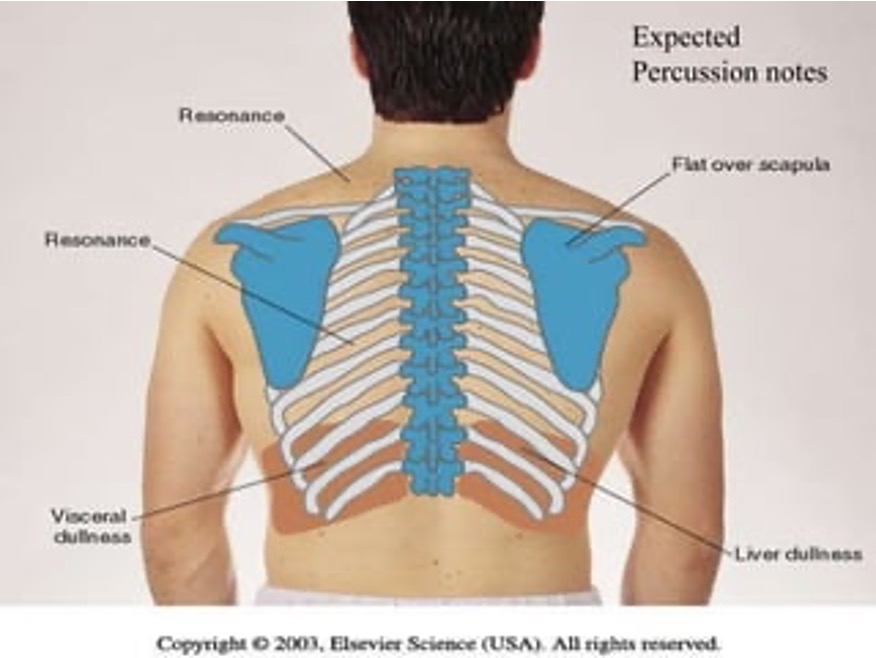
SOUNDS IN THE LOBES
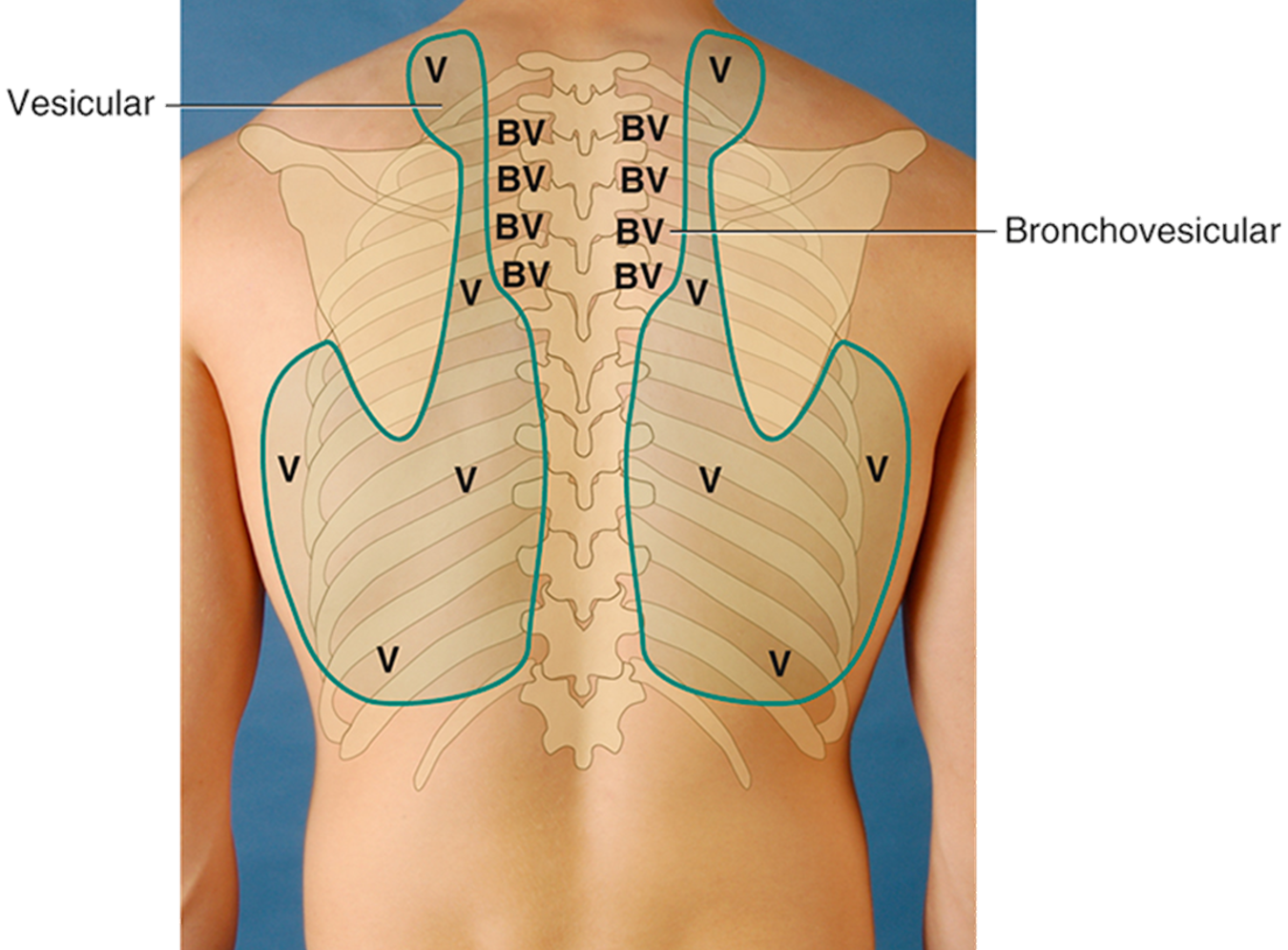
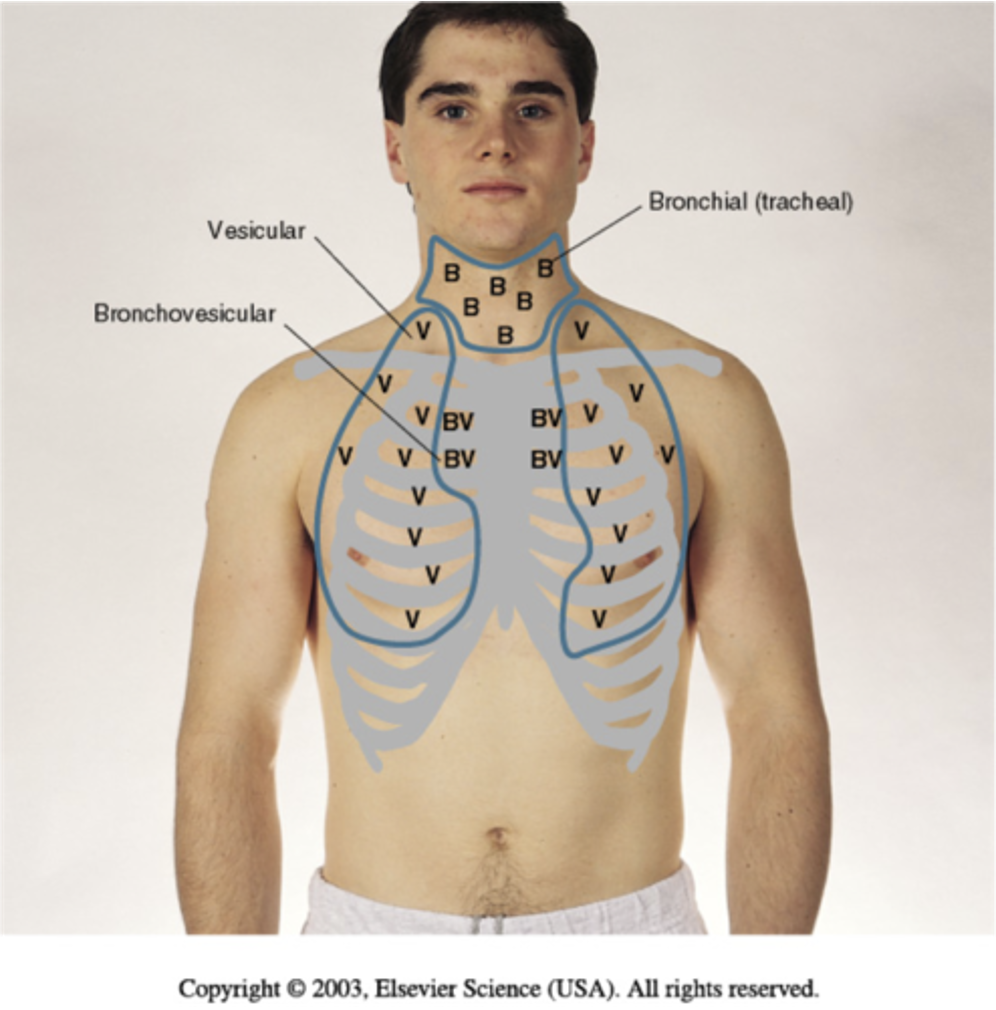
•BRONCHIAL (ANTERIOR ONLY – OVER TRACHEA & LARYNX)
•QUALITY = HARSH, HOLLOW, TUBULAR
•I < E
•AMPLITUDE = LOUD
•BRONCHOVESICULAR (BOTH ANTERIOR & POSTERIOR)
•heard over major bronchi, UPPER STERNUM, POSTERIOR BY THE SCAPULA AND 1ST & 2ND ICS
•PITCH = HIGH
•I = E
•AMPLITUDE = MODERATE
bronchovesicular breath sound is normal in the peripheral field for infants and young child up to age 5-6.
•Vesicular breath sounds(ANTERIOR & POSTERIOR)
•Quality: rustling, wind in the tree
•I > E
Amptitude; soft.
Vesicular breath sounds are low pitched, soft sounds with inspiration longer than expiration. this breath sound are expected over the peripheral lung field where air flows through smaller bronchioles and alveoli
DECREASED OR ABSENT SOUNDS
•CAUSES
1.OBSTRUCTION OF THE BRONCHIAL TREE BY SECRETIONS, MUCUS PLUG, OR FB
2.DECREASED LUNG ELASTICITY, EMPHYSEMA = LUNGS HYPERINFLATED
3.PLEURISY, PLEURAL THICKENING, PNEUMOTHORAX (AIR), PLEURAL EFFUSION (FLUID) IN THE PLEURAL SPACE.
SILENT CHEST - OMINOUS
ADVENTITIOUS SOUNDS
Added sounds that are not normally heard in lungs.
•Caused by moving air colliding with secretions or by popping open of previously deflated airways
Crackles (or rales)
•Fine – high-pitched popping, not cleared by cough
•Simulate: roll strand of hair b/t fingers near ear
•Coarse - sound like opening a Velcro fastner
•Pleural friction rub – coarse, sounds like thuds
Wheeze (or rhonchi) are terms commonly used by most examiners
•High pitched, musical squeaking = air squeezes – asthma
•Low pitched, musical snoring = obstruction
Stridor – high pitched, inspiratory = croup, epiglottitis, FB
Atelectasis: a type of adventitious sound that is not pathologic
Short, popping, crackling sounds that sound like fine crackles but do not last beyond a few breaths
VOICE SOUNDS
Normal voice transmission is soft, muffled, and indistinct
•you can hear sound through stethoscope but cannot distinguish exactly what is being said.
Increased lung density enhances transmission of voice sounds.
If you suspect lung pathology:
Bronchophony – person repeat “ninety-nine” is clear not soft muffled
Egophony – person long “ee-ee-ee” heard as “aaaa” not as “eeeeee”
Whispered pectoriloquy – “one-two-three” very clear not as faint muffled or inaudible
INSPECTION OF THE ANTERIOR CHEST
Note shape and configuration of chest wall.
Note skin color and condition.
Assess quality of respirations.
Note respiratory effort.
Observe for symmetry.
Determine if accessory muscles are being used.
PALPATION ANTERIOR CHEST
•Assess symmetric chest expansion, palpate chest wall.
•Any limitation in thoracic expansion is easier to detect on anterior chest because greater range of motion exists here with breathing.
•Note any tenderness or lumps.
•Note skin mobility, turgor, temperature, and moisture.
•Assess tactile (vocal) fremitus
Fremitus is a palpable vibration, that generates sound from the larynx and transmits it through patent bronchi and lung parenchyma to the chest wall where they felt vibration
•Compare vibrations from one side to other as the person repeats “ninety-nine.”
PERCUSSION ANTERIOR CHEST
•Begin percussing apices in supraclavicular areas
perform bilateral comparison
•Note borders of cardiac dullness normally found on anterior chest.
•On right, upper border of liver dullness is located in fifth intercostal space in right midclavicular line.
•On left, tympany is evident over gastric space.
AUSCULTATE ANTERIOR CHEST
Begin auscultation from the apices in supraclavicular areas to 6th rib.
•Perform bilateral comparison.
•One full respiration
•Do not auscultate directly over female breast tissue.
DEVELOPMENTAL COMPETENCE
Pregnant woman
•Thoracic cage may appear wider.
•Deeper respirations and an increase in tidal volume by 40%
Aging adult
•Increasing AP diameter, kyphosis, or an outward curvature of thoracic spine
•Chest expansion may be somewhat decreased, although still symmetric.
•Tend to tire easily during auscultation when deep mouth breathing is required
Acutely ill patient
•Use of second examiner to assist with positional changes
•Use of rolling technique if solo examiner but can interfere with bilateral comparison
INSPECTION
•Obligate nose breather until 3 months.
•Count respiratory rate for 1 full minute.
Normal rates for newborn are 30 to 40 breaths per minute but may spike up to 60 breaths per minute.
Respiratory pattern may be irregular when extremes in room temperature occur or with feeding or sleeping.
ABNORMAL FINDINGS: RESPIRATION PATTERNS
Rate:
•Tachypnea – greater than normal, rapid, shallow
•Bradypnea – less than normal
•Apnea – None for 10 seconds or more
Pattern:
•Cheyne-stokes respiration – respirations wax/wane in regular patter with 20 sec apnea
•Biot’s respiration – ataxisic, similar to Cheyne-stokes but pattern is irregular
Depth:
•Shallow or sighing (purposeful to expand alveoli)
Symmetry:
•Bilateral rise and fall of the chest with respiration
Audibility:
•Normally heard when several centimeters away from patient’s mouth or nose
Patient Position:
•Healthy person breaths comfortably in supine, prone, or upright position
Mode of Breathing:
•Normally inhale and exhale through the nose
SUMMARY CHECKLIST: THORAX AND LUNGS EXAMINATION
INSPECTION
Thoracic cage, respirations, skin color, and condition
A person’s facial expression, and LOC
PALPATION
Confirm symmetric expansion and tactile fremitus.
Detection of any lumps, masses, or Tenderness
PERCUSSION
Lung fields and estimate diaphragmatic excursion
AUSCULTATION
Assess breath sounds, and note any abnormal/adventitious breath sounds.
decrease or absent breath sound occurs with bronchial tree obstruction, as in emphysema, and when sound is obstructed, as in pleurisy, pneumothorax, or pleural effusion
Perform bronchophony, whispered pectoriloquy, or egophony as needed.
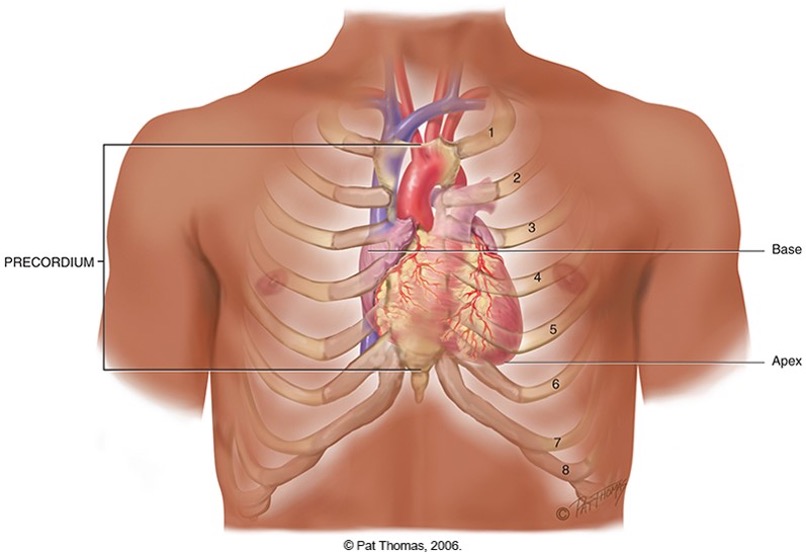
POSITION AND SURFACE LANDMARKS
Precordium: anterior chest area overlying heart and great vessels
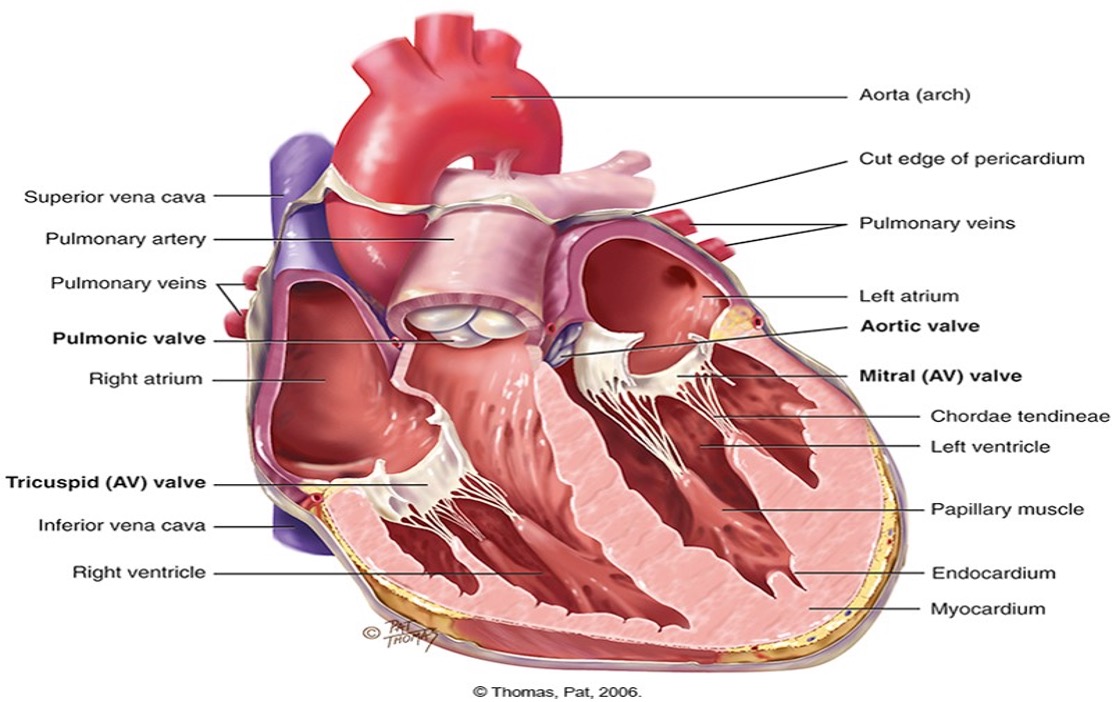
Heart has four chambers:
ØAtria and ventricles
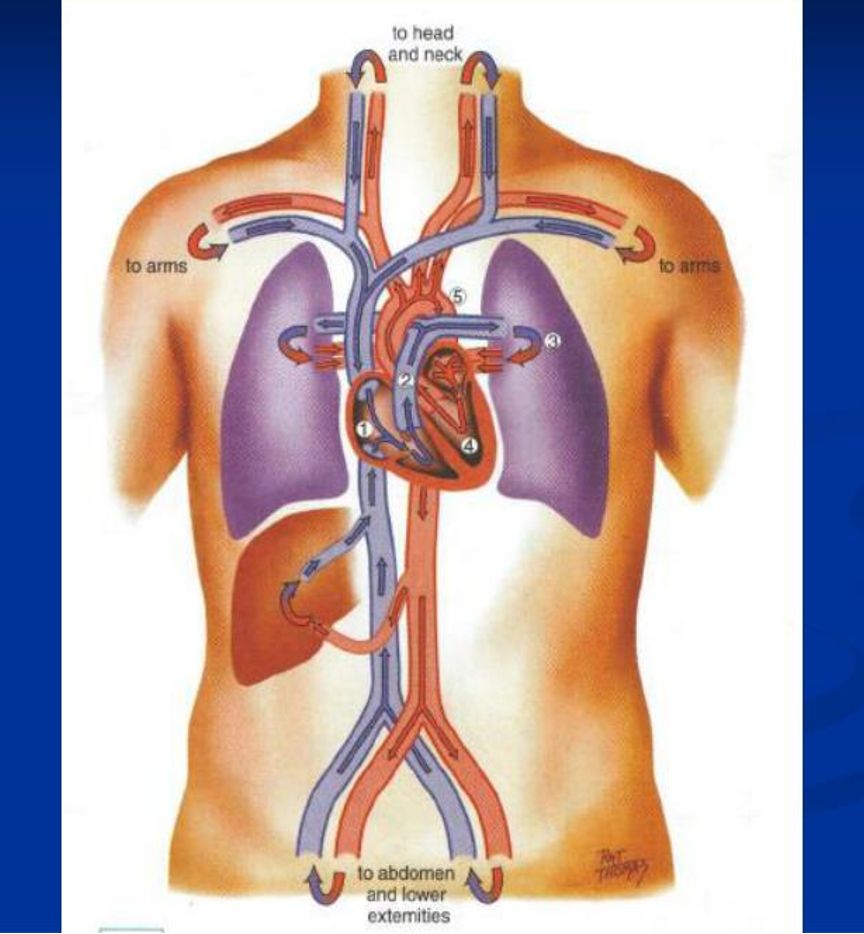
Great vessels: major arteries and veins connected to the heart
Blood vessels arranged in two continuous loops:
ØPulmonary circulation and systemic circulation
ØSystemic circulation
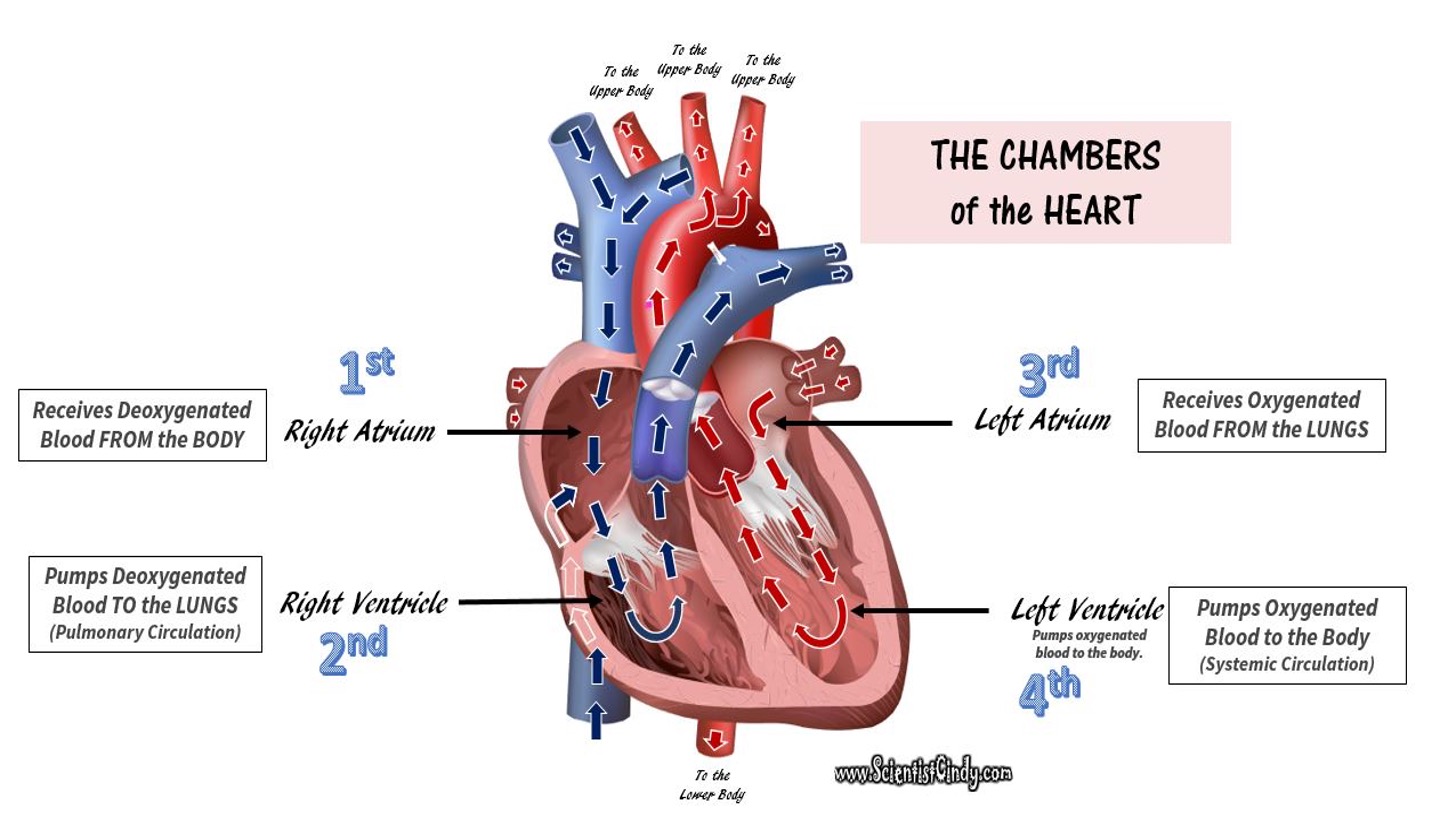
The heart chamber
AV valves
Two AV valves separate atria and ventricles:
Tricuspid valve: right AV valve
Bicuspid, or mitral valve: left AV valve
Valves’ thin leaflets are anchored by collagenous fibers (chordae tendineae) to papillary muscles embedded in ventricle floor.
AV valves open during ventricular diastole, to allow ventricles to fill with blood.
During systole AV valves close to prevent regurgitation of blood back up into atria.
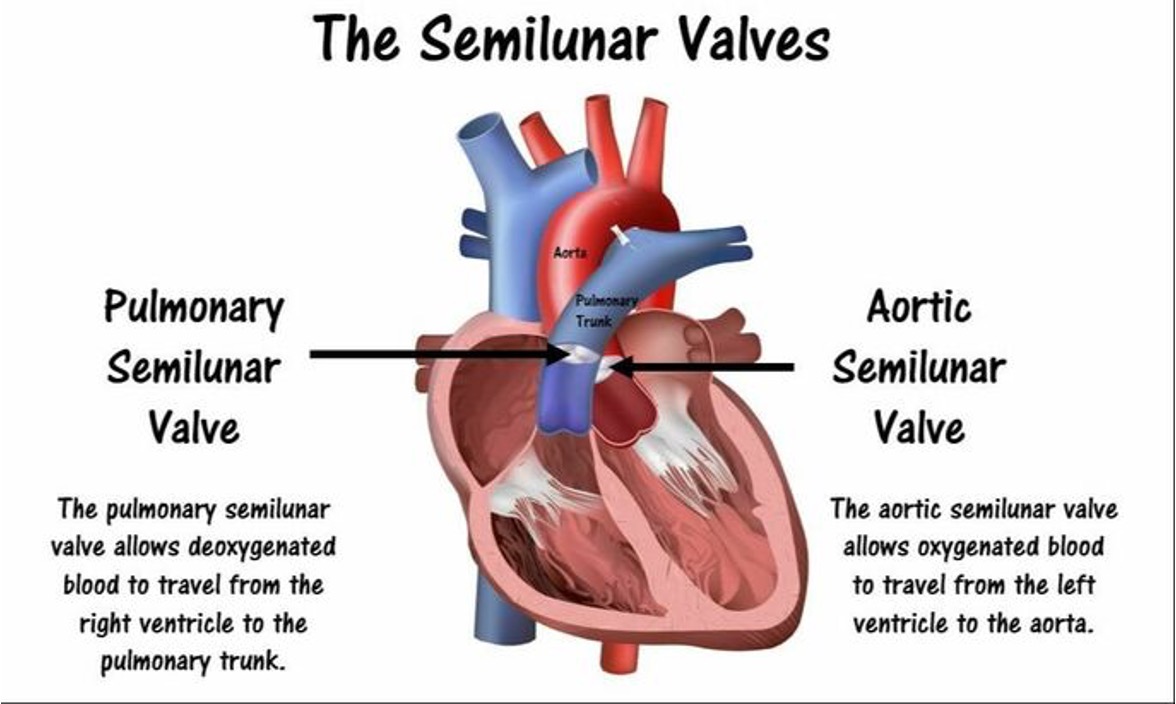
SL VALVES
Two SL valves are set between ventricles and arteries.
Each valve has three cusps that look like half moons.
Pulmonic valve: SL valve in right side of heart
Aortic valve: SL valve in left side of heart
Open during pumping, or systole, to allow blood to be ejected from heart
No valves are present between vena cava and right atrium, or between pulmonary veins and left atrium:
Abnormally high pressure in left side of heart gives a person symptoms of pulmonary congestion.
Abnormally high pressure in right side of heart shows in neck veins and abdomen.

JUGULAR VEIN DISTENTION
Assess CVP, standing on the right side to observe.
Top of EJ vein overlying sternomastoid, non palpable pulse.
Usually see in supine position and disappears when reach 45 degrees
Position patient at 30-45 degrees – Higher the pressure, the higher position needed
Remove pillow – why?
Turn head slightly away, shine light
CHAMBERS AND VALVES
Direction of blood flow
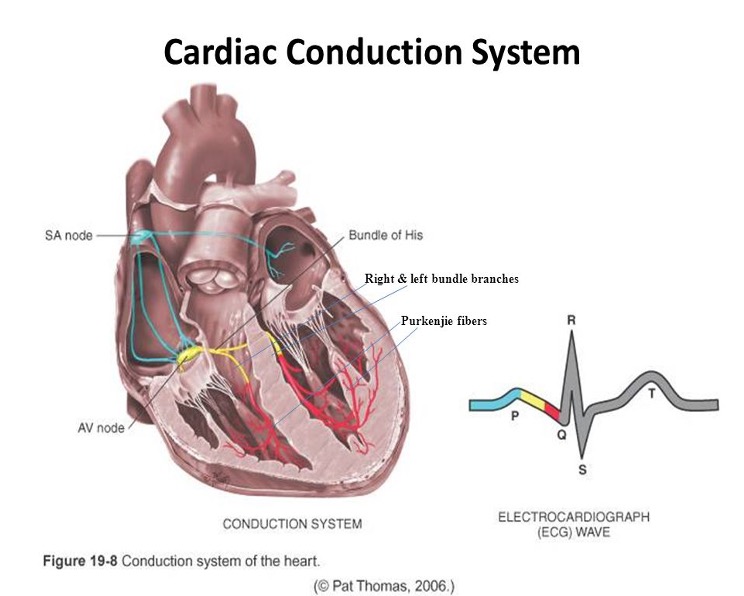
CARDIAC CYCLE
•The rhythmic movement of blood through the heart.
•There are both electrical and mechanical process for the heart.
•Electrical: SA - AV - Bundle of His – Rt and Lt Bundle branches
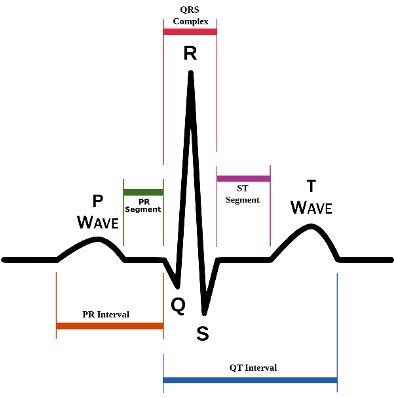
Electrocardiograph (ECG)
ECG waves PQRST:
P wave: depolarization of atria
P-R interval: from beginning of P wave to beginning of QRS complex (time necessary for atrial depolarization plus time for impulse to travel through AV node to ventricles)
QRS complex: depolarization of ventricles
T wave: repolarization of ventricles
Electrical events slightly precede mechanical events in heart.
CARDIAC OUTPUT
•It is how much blood your heart can pump in a minute
•(4L-6L/min for a resting adult)
•CO = SV x R
•SV – stroke volume (vol of blood in each systole)
•R – rate (how fast the heart beats/min)
•The heart can change CO based on metabolic needs
•Pre-load and Afterload affect the heart’s ability to adjust CO
•Preload is volume – venous return that builds during diastole. The length to which the ventricular muscle is stretched before the heart contracts.
•When blood return volume increased to ventricles increased, they are stretched to accommodate.
•Frank Starling’s Law: greater the stretch, the stronger the contraction.
•Afterload is pressure – it is the pressure needed to open the aortic valve against the higher aortic pressure.
•It is the resistance against which the ventricle must pump blood into the already pressurized body system.
•End of diastole: ventricles = 5-10mmHg
•Whereas Aorta = 70-80mmHg
•Ventricle must tense to overcome this pressure difference
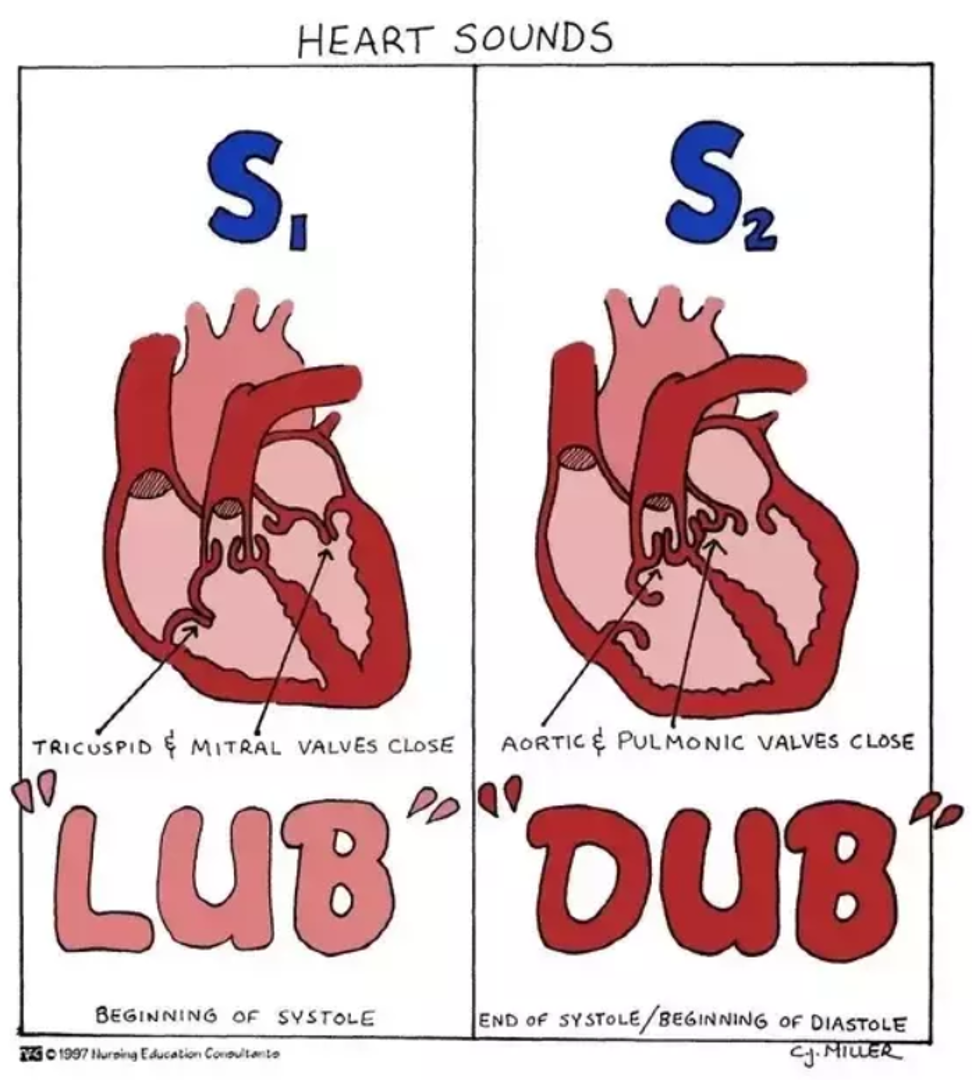
HEART SOUNDS
First heart sound (S1)
Occurs with closure of AV valves
Signals beginning of systole
Mitral component of first sound (M1) slightly precedes tricuspid component (T1).
Auscultate S1 loudest at apex but hear over all areas of pericardium
Second heart sound (S2)
Occurs with closure of semilunar valves
Signals end of systole
Aortic component of second sound (A2) slightly precedes pulmonic component (P2).
Auscultate S2 loudest at base
EXTRA HEART SOUNDS: S3
Normally, diastole is a silent event. But when conditions cause for turbulent flow, murmurs arise.
Third heart sound (S3)
•Occurs when ventricles resistant to filling during early rapid filling phase (protodiastole).
•Ex: If blood rapidly rushes into an overfilled left ventricle, it creates the S3 heart sound.
•Occurs immediately after S2
•When AV valves open and atrial blood first pours into ventricles.
•Associated with “ventricle gallop”.
EXTRA HEART SOUNDS: S4
Fourth heart sound (S4)
•Occurs at end of diastole, at pre-systole, when ventricle resistant to filling.
•It occurs as the atria push blood into a stiff ventricle. Therefore, this sound indicates that there may be an issue with the left ventricle, as it is inflexible. Non-compliant LV.
•Associated with “atrial gallop”
•S4 occurs just before S1.
EXTRA HEART SOUNDS: MURMURS
Gentle, blowing, swooshing sound that can be heard on chest wall
Conditions that create turbulent blood flow and collision currents
Conditions that can result in murmurs:
•Velocity of blood increases.
•Viscosity of blood decreases.
•Structural defects in valves
Difference in S3 and S4 murmurs?
CHARACTERISTICS OF SOUND
All heart sounds are described by:
Frequency or pitch: high or low
Intensity or loudness: loud or soft
Duration: very short for heart sounds; silent periods are longer
Timing: systole or diastole
Adventitious sounds
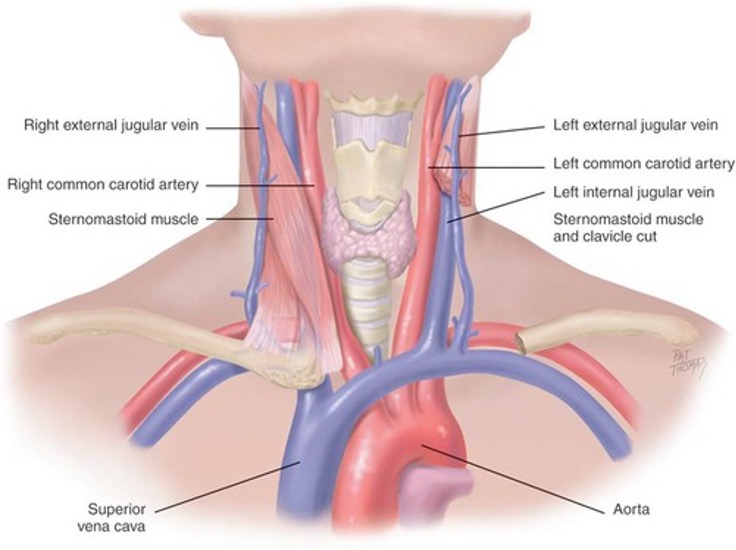
NECK VESSELS
Carotid artery
A central artery
Timing closely aligns with ventricular stroke
Located in the grove between trachea and the sternomastoid muscle
Jugular Venous
Empty unoxygenated blood directly into superior vena cava.
No valve between SVenaCava and RA, therefore can reflect what?
Two jugular veins present on each side of neck.
DEVELOPMENTAL COMPETENCE
Pregnant woman
•Blood volume increases by 30% to 50% during pregnancy.
•Despite increased cardiac output, arterial blood pressure decreases in pregnancy as a result of peripheral vasodilation.
Infants and children
•Fetal heart begins to beat after 3 weeks’ gestation.
•No point in circulating to lungs so heart reroutes blood circulation in heart until birth in two ways
•2/3 shunts through atrial septum (foramen ovale), left side and through aorta
•1/3 shunts through the right side of heart through pulm art. But detoured through ductus arteriosis to the aorta
Aging adult
•Closely interrelated with lifestyle, habits, and diseases
•Lifestyle, smoking, diet, alcohol use, exercise patterns, and stress have an influence on coronary artery disease.
HEMODYNAMIC CHANGES WITH AGING
Pressure/pulse changes
Isolated systolic HTN: Increase in systolic BP due to thickening and stiffening of the arteries
Left ventricular wall becomes thicker but the overall size of the heart does not change.
Pulse pressure increases.
No change in resting heart rate or cardiac output at rest
Ability of heart to augment cardiac output with exercise is decreased.
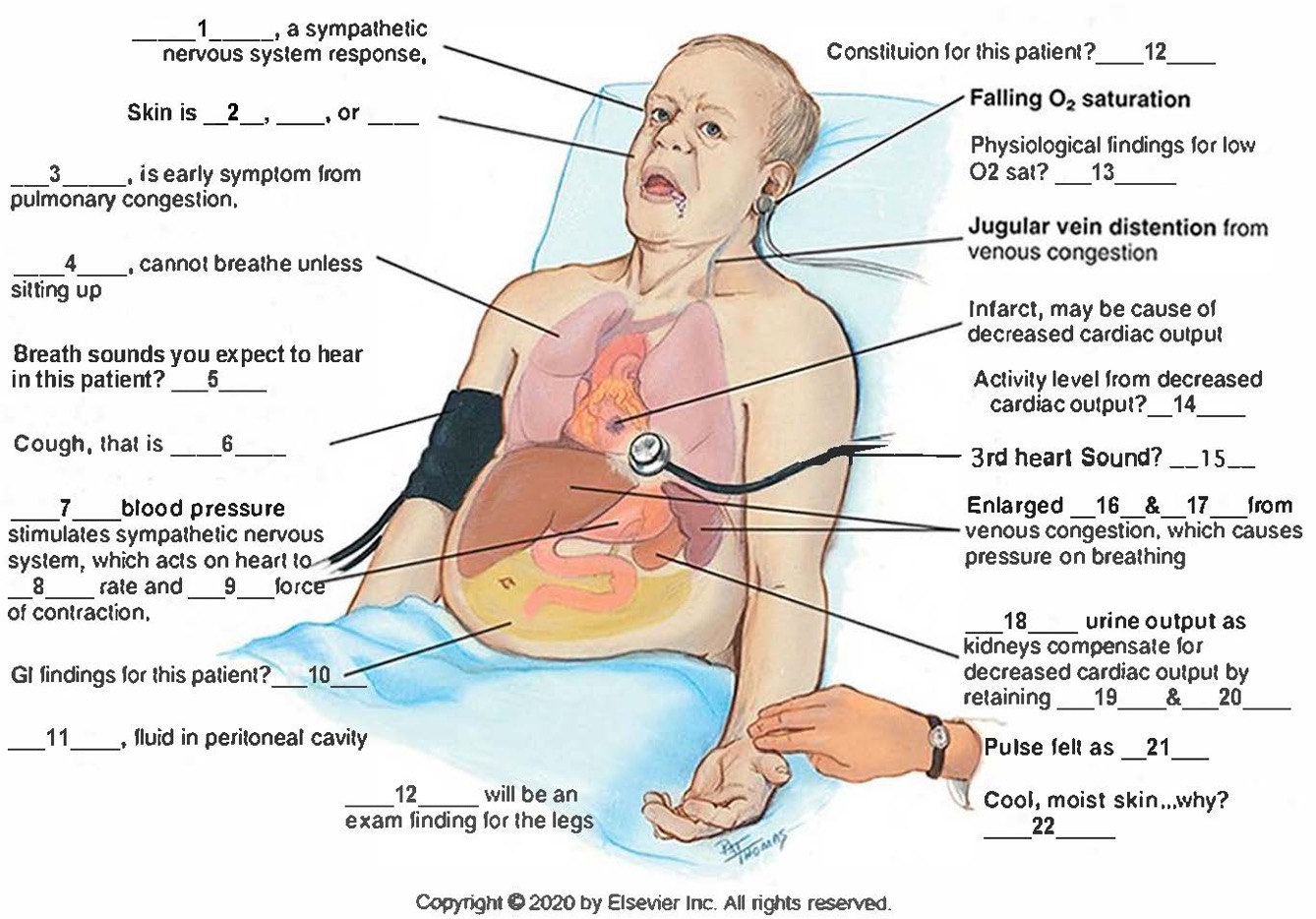
ASSESSMENT: SUBJECTIVE DATA
Chest pain
Dyspnea
Orthopnea
Cough
Fatigue
Cyanosis or pallor
Edema
Nocturia
Past cardiac history
Family cardiac history
Patient-centered care (cardiac risk factors)
NECK VESSELS: INSPECTION
Preparation:
To evaluate carotid arteries, a person can be sitting.
To assess jugular veins and precordium, the person should be supine with head and chest slightly elevated.
Inspect neck for jugular venous pulse
From jugular veins you can assess central venous pressure (CVP) and judge heart’s efficiency as a pump.
Position a person supine anywhere from a 30- to a 45-degree angle, wherever you can best see pulsations.
Observe for possible distention.
Characteristics of jugular versus carotid pulsations
Differentiate between: location, quality, respiration, palpable, pressure, and position of patient
NECK VESSELS: PALPATION AND AUSCULTATION
Palpate carotid artery
Palpate only one carotid artery at a time to avoid compromising arterial blood to brain.
Feel contour and amplitude of pulse, normal strength 2+.
Findings should be same bilaterally
Auscultate carotid artery
Assess for presence of carotid bruit.
Avoid compressing the artery which can create an artificial bruit.
Keep neck in neutral position and lightly apply stethoscope at
angle of jaw, midcervical area, and base of neck.
PRECORDIUM INSPECT AND PALPATE
Inspect anterior chest
Arrange tangential lighting to accentuate any flicker of movement.
Observe for any possible pulsations.
Palpate apical impulse -
note location size
amplitude duration
Palpate across precordium to assess for any possible pulsations.
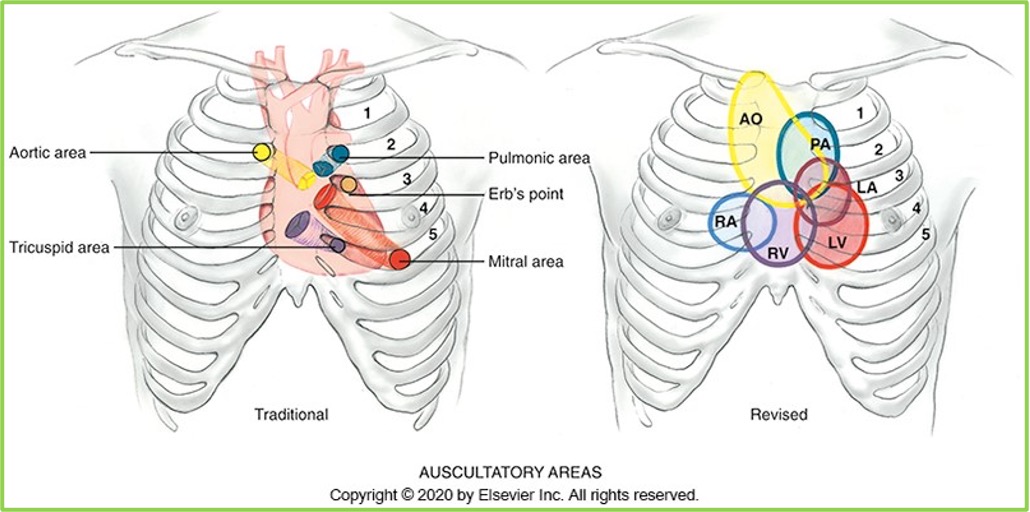
PRECORDIUM AUSCULTATION
Auscultate the 5 areas associated with heart valves.
1. Second right ICS: aortic valve area
2. Second left ICS: pulmonic valve area
3. Third ICS Left of the sternum: Erb’s point
4. Fifth ICS Left lower sternal border – Tricuspid area
5. Fifth ICS left midclavicular line - mitral valve area and Apex of the heart
2. Note rate and rhythm: describe characteristics
3. Identify S1 and S2
4. Listen for extra heart sounds: Describe characteristics.
5. Listen for murmurs: Timing, loudness, pitch, pattern, quality,
location, radiation posture and change of position.
DEVELOPMENTAL COMPETENCE:
CHILDREN
Note any extracardiac or cardiac signs that may indicate heart disease.
Poor weight gain, developmental delay, persistent tachycardia, tachypnea, dyspnea on exertion, cyanosis, and clubbing
Note that clubbing of fingers and toes usually does not appear until late in first year, even with severe cyanotic defects.
Palpate apical pulse
Be aware of location by age.
Rhythm remains characterized by sinus dysrhythmia.
Physiologic S3 is common in children.
Venous hum has no pathologic significance.
Assess for carotid bruit
DEVELOPMENTAL COMPETENCE: PREGNANT WOMAN AND AGING ADULT
Pregnant woman:
Vital signs increase in resting pulse rate of 10 to 15 bpm and drop in BP from normal prepregnancy level.
ØPalpation of apical impulse is higher and lateral compared with normal position.
ØHeart sounds: Changes due to increased volume and workload
Aging adult:
ØGradual rise in systolic blood pressure common with aging; widening of pulse pressure—be alert for orthostatic hypotension
ØLeft ventricular wall thickness increase.
ØPresence of supraventricular and ventricular dysrhythmias increases with age.