gi tract infections quiz - microbio (cls 532)
1/109
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
110 Terms
upper GI tract organs vs lower GI tract
upper GI:
Mouth ; esophagus ; stomach
lower GI:
Duodenum/jejunum
Small intestine—most of infections are happening in bottom of pili (regenerating all the time)
Ileum ; Colon
normal flora of upper GI tract
Upper GI tract is sterile
Acid kills most organisms w/in 30 minutes
food poisoning (general)
Organism forms toxins while growing in food
Toxins and bacteria are ingested with food
Toxins are absorbed by the body and cause disease
Bacteria are generally shed from the body without colonization
Most common agents
Staphylococcus aureus
Bacillus cereus
Clostridium botulinum
what is food poisoning classified as?
INTOXICATIONS
staph aueus food poisoning
Most common intoxication in the US
Not sure for other countries due to sanitation & dietary practices
Heat stable enterotoxin
Found in warm foods--processed meats and dairy products
Food becomes contaminated from exposure to skin and nasal secretions of food handlers
symptoms of s aureus food poisoning
Explosive onset of symptoms 1-6 hours after ingestion
Vomiting
Nausea
Abdominal cramps
Often followed by diarrhea
Lasts 8-10 hours
Recovery is usually complete in 24-48 hours
(s aureus food poisoning) staphylococcal enterotoxins
are superantigens!!!
Several different serotypes have been identified: SE A, B, C (1,2, & 3), D, E, etc
Heat stable toxin still present in food after thorough cooking
One strain can produce more than one type of toxin
Mode of action
Superantigens cause the release of cytokines (IL-2) which induce the symptoms of food poisoning
Thought to stimulate the nerve ending in the stomach lining (vagus nerve)
incubation period for s aureus food poisoning
30 min - 8 hours; usually 2-4 hours
bacillus cereus food poisoning type I
aka diarrheal type
characterized by abdominal pain with profuse watery diarrhea, nausea, tenesmus, lower abdominal cramps
8-16 hours after ingestion of contaminated food
meats, vegetable dishes, cakes, sauces, dairy products
Symptoms abate 12-36 hours later
toxins associated with b cereus food poisoning type I
4 heat labile toxins associated with this type
Hemolysin BL
Dermonecrotic & increases vascular permeability
Non-hemolytic enterotoxin
Enterotoxin T
Cytotoxin K
b cereus food poisoning type II
aka emetic type
Characterized by nausea and vomiting 1-6 hours after eating the offending food
Associated with rice dishes, cream and milk products, pastas
Symptoms resolve within 10-24 hours
Assoc w heat stabile toxin called cereulide
Endospores can survive normal cooking procedures
Under conditions of improper storage the spores germinate and the bacteria multiply to produce the toxins that cause the symptoms
clostridium botulinum (bacteria)
Gram positive spore forming, anaerobic rod
Found in soil, sediments or lakes and streams, and frequently in intestines of animals
Over 80 known species of Clostridium--Strains A, E, R, & F are most common
c botulinum intoxication
Cause by the ingestion of preformed botulinum toxin
Spores from the organism contaminate meats, vegetables and fish
Home processed foods are the most common source
fruits, chili, stew, spaghetti sauce
Spores are very heat resistant. Can survive food processing and canning if the temps are not high enough (121 C for 2.5 min or 111 C for 25 min)
Spores germinate in an anaerobic environment (canned goods)
development of c botulinum intoxication
Bacteria multiply and produce toxin
Toxin is formed only during sporulation
Bacterial growth may cause spoilage, but often the food is unaltered in appearance and taste
Food is consumed without adequate heating → person gets sick
Incubation period is 12-36 hours (dose dependent)
Toxin is inactivated at 80 C (175 F) for 10 minutes
botulism pathogenesis
Toxin is absorbed through the stomach and enters the blood
Clinical disease begins within 4-36 hrs after ingestion
Time depends on dosage
Symptoms include:
Nausea and vomiting
Double and blurred vision
Difficulty with swallowing and speaking
Weakness of neck and extremities
Difficulty with breathing
Acute flaccid paralysis of muscles – descends from the head downward
face, eyelids, thorax, diaphragm, extremities
Death usually occurs due to paralysis and respiratory failure
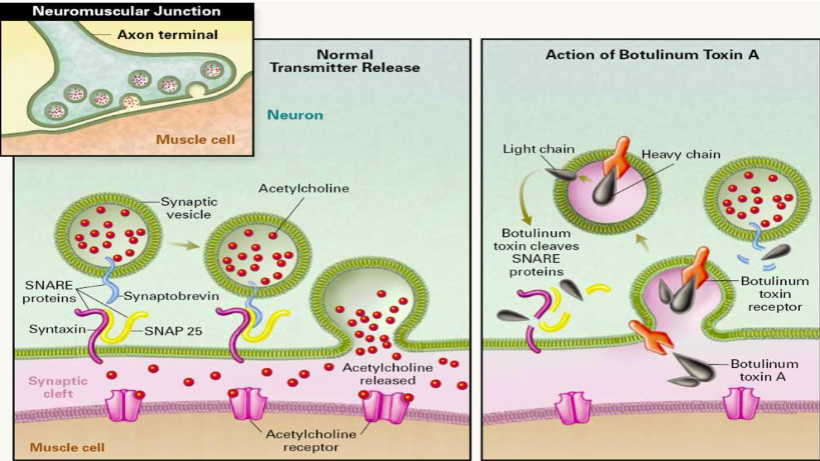
botulinum toxins
Simple AB toxin that interacts with other bacterial proteins that may protect the AB toxin from stomach acid and proteases, and help it transit the stomach wall
Once in the bloodstream, it is transported to neuromuscular junctions where it binds to glycolipids on the ends of the peripheral nerves
A-portion prevents the release of acetylcholine at peripheral nerve synapses
Nerve impulses can’t be transmitted, no muscle stimulation
Doesn’t kill neurons, just prevents them from functioning
infant botulism
First recognized in 1976
Now the most common form of Botulism in the USA
Seen most often in infants <20 weeks old
Spores ingested by infant
honey has been implicated in many cases of this
Spores germinate in gut
Lack of adult-like normal flora prevents microbial antagonism, thus no natural protection
symptoms of infant botulism
Colonizes the gut and produces toxin
Toxin is absorbed and causes disease
Symptoms
Constipation
Listlessness
Difficulty sucking and swallowing
Altered cry
Hypotonia
Muscle weakness--floppy baby
wound botulism (RARE)
Spores introduced into deep wounds
Host tissue consume oxygen
Spores germinate produce toxin
Typically seen in black tar heroin and other IV drug users
treatment of botulism
Antitoxin therapy effective if begun early
Life support for those severely affected
Antibiotic therapy to eliminate organism
Wound & Gut colonization
Prevention is the best way to avoid this food poisoning
If a can sprays you when you open it, don’t use it
Discolored contents
Bad odor
clostridium perfringens food poisoning
Patient ingests organism from contaminated food:
Beef, turkey, chicken, pork, gravy
Org grows and produces toxin once in the body
Needs 10^8 viable orgs to reach the small intestine to form toxin
Toxin A produced
symptoms of c perfringens food poisoning
Crampy abdominal pain develops 7-15 hours after ingestion
Diarrhea w foamy, foul-smelling stools
Little vomiting
No fever
Mild, self-limited, 2-3 days to recover
peptic ulcer disease (PUD)
Caused by Helicobacter pylori
Associated with stomach cancer, atrophic gastritis, & peptic ulcer disease
Responsible for 65-90% of gastric ulcers
Robin Warren & Barry Marshall proved that ulcers were bacterial in nature & won the 2005 Nobel Prize
reservoir for h pylori
Humans are probably the primary reservoir
Org infects stomach epithelium and duodenal epithelium
Infection rates increases with age
In developing countries nearly all adults are infected due to childhood acquisition
Percent infected corresponds to age: 10% of 10 yr olds are infected; 20% of 20 yr olds etc
In developed countries, infection rates lower but infection still occurs in childhood
(h pylori) transmission/infection
Fecal-oral is primary route
Oral-oral transmission may occur
Transient oral colonization appear to result from either route
Successful infection appears to require at least a transient low stomach acidity
Initial survival in the stomach requires bacterial urease
Converts urea to ammonia and carbon dioxide
Urease negative mutants do not cause disease
H pylori is a rapid urease producer
(h pylori) damage to gastric mucosa
Ammonia--toxic to gastric mucosa
Vacuolating toxin
Lethal to epithelial cells
Causes acidified vacuoles to form in epithelial cells
Unknown mechanism of toxicity
Gastric mucosa cells are destroyed
Urease itself damages the mucosa
(h pylori) host response & symptoms
Tissue damage stimulates inflammation
Inflammatory stimuli include tissue damage from ammonia and vacuolating toxin, LPS, and urease
50% of cases have bloating, stomach pain, vomiting
Symptoms develop 3-7 days after infection and resolve within 2 weeks
(h pylori) ulcers & cancer
Progression to ulcers is dependent upon host genetic factors, bacterial exotoxin, and environmental factors
Chronic inflammation may damage epithelial and subepithelial tissues to allow penetration of organism into mucosa, leads to gastric ulcer
Chronic inflammation leads to cancer through cell proliferation and oxidative burst products
Cause DNA damage
These factors increase the likelihood of mutation and hence cancer
treatment for h pylori
Antibiotics
Amoxicillin and metronidazole
Drugs must survive the stomach acidity
Proton pump inhibitors (PPIs)
Bismuth subsalicylate
Histamine (H-2) blockers if PPI's cannot be used
Also drugs must permeate mucin layer
normal flora of the lower GI tract
Anaerobes (predominant type found)
E coli & other enteric GNRs
Pseudomonas sp and other non-fermenting GNRs
CNS
Enterococci
Yeast
bacillary dysentery
caused by Shigella species
Most communicable of the bacterial diarrheal diseases
Humans and primates are only hosts
Obligate pathogen
Uncommon in developed countries
Endemic in underdeveloped countries
Does not survive in the environment
Not NF, although carrier states exist
Very low dosage, 10-100 orgs required for infection
order of virulence for shigella sp
S. dysentariae
S. flexneri (found in USA)
S. boydii
S. sonnei (most common in USA)
disease process of dysentery (shigella)
Starts as a moderate watery diarrhea with a low-grade fever
Symptoms change after 24 hours of diarrhea
Severe abdominal pain and cramping
High fever
Low-volume (several hundred mL) that is bright red (from blood) and mucoid (sloughing of intestinal epis)
Headache, convulsion, and possible kidney failure
Generally self-limiting with 5-7 days
incubation period for shigella sp dysentery
12 hours - 6 days; usually 2-4 days
(shigella dysentery) transmission & colonization
Ingestion of contaminated food or water by direct contact--fecal oral route
Highly communicable
Only need to ingest 10-100 organisms
Can survive the stomach acid
Colonizes the lower small intestine and the colon
Specific colonization factors are unknown
(shigella dysentery) penetration of bacteria in GI tract
Organism penetrate the intestinal wall through M-cells of Peyers patches
enter cells within an endosome or phagosome
M cell translocates organism to underlying macrophage
Organism can replicate inside the macrophage
Trigger apoptosis of the macrophage
Bacteria are liberated into lamina propria
(shigella dysentery) SPREAD of bacteria in GI tract
Liberated organisms invade the basolateral surface of epis
Active invasion requires Ipa B and Ipa C proteins
Insertion leads to cytoskeleton rearrangements, forms pseudopods
Pseudopods engulf organisms forming an endosome
Endosome lysed by Ipa B and C
Bugs grow free in host cytoplasm
Bacteria spread from the M cell (cell-cell spread)
Ipa and Ics proteins are expressed by organisms growing in the cytoplasm of the cells
process of cell to cell spread and invasion allows vast sections of the intestinal epithelium to be infected ; this intracellular multiplication causes epithelial cell death
(shigella) Ipa protein function
Made by Shigella and some E coli allow penetration & spread or organisms through the intestinal epithelium
Ipa proteins (IpaA, B, C) direct reorganization of the epithelial cell cytoskeleton, allowing uptake of the bacterium within a membrane-bound vacuole
IpaB/C directs lysis of the vacuole, allowing organism to enter cytoplasm
(shigella) Ics protein function
IcsA directs actin polymerization that push orgs into adjacent cell, where it is surrounded by a double layered vacuole
IcsB & IpaB/C lyse the first & second layers of the vacuole respectively, allowing access to adjacent cell's cytoplasm
host response to shigella dysentery
develops strong inflammatory response due to tissue damage, proinflammatory cytokines released by infected host cells, and presence of bacteria
Dramatic influx of phagocytes to infection sites damage cohesion of the epithelium and allows more extensive invasion of the epithelium by the org
Sheets of epithelial cells are sloughed from the intestinal wall due to inflammatory response and microbial action
Loss of epithelium damages lamina propria and associated blood vessels hemorrhage leading to bloody diarrhea
Inflammation limits infection to the epithelium and lamina propria
(shigella dysentery) infection clearance
Tissue and blood defenses
Complelement—shigella sensitive to complement except for S dysenteriae
Activated macros—orgs don't survive in them
Natural killer cells recognize foreign peptides on host cells
Immune response
Antigenicity of orgs--O antigen, Ipa proteins are good antigens
Infection is not protective
Usually lethal to those <5 yrs
Death from dehydration and septic shock induced by endotoxins
treatment for shigella dysentery
Provide supportive therapy
Hydration
Antibiotics increase the rate of clearance by reducing the bacterial load
Ciprofloxacin
Ceftriaxone or azithromycin (2nd line)
Antibiotics often induced a carrier state
No effective vaccine against Shigella
(shigella toxins) shigella enterotoxin
Found in S dysenteriae and S flexneri
Appear to be pore forming toxins
Leads to water loss through disruption of ion channels and electrolyte movement into lumen
(shigella toxins) cytolethal distending toxin
Not present in S sonnei
Compound AB toxin
Binds to many cell types
Causes changes in cytoskeletal structure and inhibition of cell proliferation
May contribute to diarrhea through loss of tight junction stability
(shigella toxins) shiga toxin (ST)
Compound AB toxin ; produced by S dysenteriae
Not required for dysentery; more severe if present
Released after cell death and lysis
Attracted to a glycolipid receptor located on certain intestinal epi and endothelial cells, kidney cells, B cells
Inflammation increases the number of receptors (G3b) due to induction of synthesis of the receptor
Action is an irreversible inhibition of protein synthesis due to inactivation of 60S ribosomal unit—fatal for the cell
role of shiga toxin in disease
Toxin lethal for intestinal epithelial cells expressing G3b receptor
Sections of the intestinal tract not infected with S dysenteriae will still be damaged by the toxin
Toxin entering bloodstream will damage the intestinal blood vessel
damage leads to formation of blood clots which further damages the tissue due to lack of blood
Toxin is not necessary for the diarrhea, but increases bleeding & abdominal pain/cramping experienced
shigella species bacteria info
Genetically identical to Escherichia ; DOESN’T WORK ON MALDI
Kept separate due to diseases each genus causes
4 groups--43 serotypes--grouped based on O antigen
Group A--S dysenteriae
Least isolated in the US
Most common in developing countries
Most virulent
15 serotypes
1 serotype produces Shiga toxin
groups and serotypes of shigella sp
Group A --S dysentariae
Group B – S. flexneri
8 serotypes and 9 subtypes
Found in US
Group C – S. boydii
19 serotypes
Group D – S. sonnei
Most common species isolated in the US
Has the mildest symptoms
1 serotype
hemolytic uremic syndrome (HUS)
Rare complication most commonly occurring in children
Form of acute kidney failure
Toxin binds to G3b receptor in kidney endothelial cells
damages cells triggering clot formation by attracting plts
increases number of plt receptors on endothelial cells so more clots keep forming
Extracellular compounds from NF organisms suppress Shiga toxin production
Bacteriodes thetaiotaomicron produces these compounds
Thus, an imbalance in bowel flora may predispose people to HUS
what is HUS characterized by?
Thrombocytopenia
Hemolytic anemia
Kidney failure
enterohemorrhagic e coli (EHEC)
Aka E coli O157:H7 based on its serotype
Shiga toxin producing E coli (STEC)
Causes hemorrhagic colitis and HUS
O104:H4 also causes HUS
O157:H7 grows as non-sorbitol fermenter on MAC a sorbitol agar
EHEC symptoms & reservoir
Get from cows
Hemorrhagic colitis--bloody diarrhea somewhat similar to dysentery
Intense abdominal pain
Moderate watery diarrhea that turns bloody
NO fever or MUCUS in stool (distinguishes it from dysentery)
transmission of EHEC
During processing, external surface of meat becomes contamination--when ground up it spreads through the meat
Orgs are killed by heating to 175 F, if not heated enough live orgs will be ingested
EHEC are resistant to stomach acid--100 orgs is enough to infect a person
Can also be transmitted by contact w fomites (diapers), water, improperly cured dried meats, apple cider and unpasteurized milk
(EHEC) colonization/penetration/spread
Orgs transit to intestine and adhere
Loose adherence is mediated by a pilus, called bundle forming pilus (Bfp)
Intimate adherence is mediated by the protein Initimin
Causes morphological changes in the host cell; deform the microvilli of the cell
Loose adherence is required for intimate adherence
Intimate adherence is required for diarrhea
Organisms invade epithelial cells, but not very efficiently
Does not spread cell to cell like Shigella
EHEC toxins
Shiga-like toxin (SLT)
Structure & action similar to shiga toxin
Blood in stool appears as a result from toxin production
Toxin mediated killing damages epithelium and leads to bleeding
Bleeding occurs mainly in the cecum and ascending colon
Thrombosis and microvasculature in the lamina propria w necrosis of mucosal villi
Damage leads to superficial ulceration and pseudomembrane formation
treatment of EHEC
Antibiotics shorten duration of symptoms and decrease transmission
Can treat with anti-shiga-like toxin (SLT) antibody is HUS is suspected
non-O157 E coli and HUS
Other strains of STECs have been shown to cause HUS
O26
O103
O111
O128
Problem bc they are sorbitol positive
cholera (general info)
Caused by vibrio cholerae
Several serotypes used to differentiate the strains
O antigens composition → O1 and O139 are the most virulent strains
Caused the 7th (O1) and 8th (O139) pandemics in the 1990s
Other serogroups are considered avirulent or cause less severe diarrhea
Dissimilarity in pathogenic and epidemic potential
No cholera toxin produced, but other endotoxins cause the symptoms
cholera in america
Foci along gulf coast
Serotype O1 Inaba
Associated w undercooked crabs and raw oysters
cholera symptoms
High volume diarrhea
Severa liters per day in mild cases; over 20 L/day in severe cases
Clear to opaque gray-white color –"rice water stool”
Intestinal contents are washed out, diarrhea consists of water and mucus
Muscle cramps and dizziness due to loss of electrolytes
Vomiting may occur but usually no fever
death from cholera occurs from what?
dehydration (!!)
Low blood volume leads to circulatory collapse
Fatalities highest in kids under 5
Worldwide estimated 100,000 deaths/year
what happens if cholera if non-fatal?
disease is self-limiting
Diarrhea subsides in about 48 hours
Mild symptoms may persist for another day
Organisms are flushed from the intestine with the diarrhea
Toxin poisoned intestinal cells must be sloughed from the mucosa
reservoir of cholera
ubiquitous in nature, found in seawater, colonizes shellfish, esp oysters, crabs, shrimp
transmission & colonization of cholera
Transmission
Organisms ingested with contaminated food or water
Contamination could be from infected individuals
Organism is sensitive to stomach acid so large quantities are needed → 10^9 to 10^10 orgs
Colonization
Organisms transit to small intestine where they colonize using pili
Organism adheres to gastric and intestinal mucosal cells
Secretes mucinase – aids in penetration of protective mucin layer
(cholera) cholera toxin
Compound A-B Toxin
Permanently activates ACase, which increases cellular cAMP concentration
cAMP activates a protein kinase –A-Kinase
A-kinase regulates the activity of ion channels in the membrane
Causes ions to move into the lumen of intestine, gradient cause water to move into lumen
Efflux overwhelms the water absorptive capacity of the intestine resulting in diarrhea
**evolutionary link between CF and cholera bc of the CFTR
(cholera) ZOT toxin
Disrupts the tight junction between intestinal epithelial cells (zona occludens)
Allows ions to flow into lumen
Single polypeptide
(cholera) ACE toxin
Enterotoxin shown to cause diarrhea in animals
Single polypeptide
Mechanism is unknown
treatment of cholera
Rehydration therapy most effective
Oral - water, salts, glucose (stimulates uptake in areas least affected by toxin)
IV – physiological saline
Antibiotics – aid in removal of colonized bacteria
Several brands of Cholera vaccine are available around the world
speciation of vibrio
Need to speciate vibrio due to variable pathogenicity of each species
Commercial systems: don’t work bc of the need for salt for all but V cholerae and V mimicus
Need to use traditional media supplemented w 1% NaCl
MALDI-Tof
gastroenteritis
Form of food poisoning
Acquired by oral fecal route
Bacteria must multiply in host to cause symptoms
Most common form of food poisoning
Campylobacter is most common cause
Salmonella sp is second most common cause
In the US only
symptoms of gastroenteritis
Initial symptoms develop 12-36 hours after ingestion
Nausea and vomiting lasting a few hours
Mild to high fever
Abdominal pain and diarrhea follow, can last for several days, stool may contain blood
Severity of abdominal pain depends on host susceptibility/virulence of organism
(gastroenteritis) vibrio parahemolyticus
Follows ingestion of contaminated seafood
Produces a hemolysin that is both cytotoxic and cardiotoxic
Mild to moderate disease
Usually, self-limiting 2-3 day duration
Symptoms
Watery, sometimes bloody diarrhea
Cramps, nausea
Vomiting
Headache
Low grade fever, chills
(gastroenteritis) aeromonas hydrophilia
Strong evidence supporting Aeromonas as causative agent of diarrhea, although the data is not absolute
Produces a cholera like extractable toxin that causes watery diarrhea
20% of those w Aeromonas infection had symptoms
(gastroenteritis) plesiomonas shigelloides
Mild, watery, diarrhea, no blood or mucous
Often associated with shellfish, oyster or untreated water consumption
Pathogenicity associated w enteropathogenic enterotoxin
(gastroenteritis) campylobacter jejuni
Slender, spirally curving to s-shaped or gull wing shaped GNRs
Microaerophilic and capnophilic
C jejuni is the most important species and most commonly isolated
Worldwide distribution
Recovered 2-7x more frequently than S&S (salmonella & shigella) in industrialized countries
(gastroenteritis) campylobacter coli
Occasional cause of gastroenteritis
Prefers pigs as hosts
5-10% of Campylobacter infections are C coli
Difference is just the hippurate hydrolysis reaction (neg)
MALDI-Tof
(campylobacter enteritis) signs & symptoms
Crampy abdominal pain
Bloody diarrhea
Chills, fever
(campylobacter enteritis) reservoir & transmission
Reservoir: cattle, swine, poultry, waterfowl, house pets
Transmission
Contaminated food--improperly cooked meat; unpasteurized milk
Low dosage--about 500 organisms
Direct contact with human carriers
Infected people may excrete the org for up to a month after symptoms have disappeared
Contaminated water
(campylobacter enteritis) colonization
Infects ileum and colon
Unknown adherence factors, but functional flagella are required
Org produces an enterotoxin that is responsible for the diarrhea
Enterotoxin activates host adenylate cyclase
(campylobacter enteritis) invasion & spread
Invade the intestinal mucosa
Multiply in lamina propria
Infections restricted to intestinal tract
Occasional septicemia will occur
(gastroenteritis) clearance of campylobacter
Inflammatory response kills orgs (phagocytes)
Inflammation is responsible for symptoms
Infection is usually self-limiting (resolves in 3-7 days)
Antibiotics are administered only if patient becomes septic
Org can be excreted for up to 1 month following abatement of symptoms
salmonella gastroenteritis
Common cause of gastroenteritis in the US
Causes enteric disease ranging from self-limited gastroenteritis w mild symptoms to typhoid fever, infections are usually not fatal
Moderate to severe GI symptoms
Diarrhea may be bloody
Symptoms appear 7-72 hours after ingestion of organism
(salmonella gastroenteritis) reservoir & transmission
In many animals, fowl, particularly poultry; farm animals
Direct transmission can occur from symptomatic individuals or carriers or animals (pet turtles)
Transmitted by contaminated food & water
Dairy products
Salmonella colonizes intestines of chickens
Eggs can become contaminated either via transovarian spread or on the surface after laying
Meat becomes contaminated during processing
Human disease results from ingesting uncooked meat or raw eggs
can occur from cross contamination of cutting boards, bowls etc
(salmonella gastroenteritis) colonization & invasion
Not resistant to stomach acid thus needs 10^6-10^8 orgs for disease
MUCH more than Shigella sp
Organisms transit to large and small intestine
Actively invade the intestinal epithelium thru columnar absorptive cells and M cells
Multiplication leads to death of the cells
Bugs released at the basolateral surface into lamina propria
Encounter complement and phagocytic cells
(salmonella gastroenteritis) resistance in salmonella
long LPS chain confers complement resistance
MAC forms too far from the bacterial surface
Absent LPS strains are avirulent; short LPS strains are less virulent
Can survive in macros by inducing a set of proteins for survival
EnvZ--sensor kinase that response to intracellular osmotic stress, phosphorylated OmpR
OmpR--a DNA binding protein that regulates protein expression
These proteins helps the organism survive both the O2 dependent and O2 independent mechanisms
Allows the bacteria to multiply in the macrophages
(salmonella gastroenteritis) spread and clearance
Bacteria usually stay within the lamina propria and epithelium
Can cause systemic infections if they invade the bloodstream
Infants / Immunocompromised
Mortality only 2% in treated cases
Organisms stimulate a strong inflammatory response and strong induced immune response
Responses limit the spread of infection
The org can't survive inside activated macrophages
Inflammatory response is responsible for abdominal pain
(salmonella gastroenteritis) treatment of salmonella
Usually self-limiting, and only requires antibiotic treatment in certain situations:
If infection becomes systemic
Carrier state develops
Site of carriage is unknown (gallbladder?)
35-40% of those infected become short term carriers (months)
1-4% of those infected become long term carriers (up to a year)
(salmonella gastroenteritis) prevention
Proper food handling
Salmonella is killed at temps high enough to denature proteins
Vaccines and treatments for chickens to prevent colonization
Improved meat processing techniques at processing plants
tribe salmonelleae
Most complex tribe even though there is only one genus and two species
S enterica (USA) and S bongori
Most ID systems just indicate that you have isolated a Salmonella species
clinical lab will perform limited serotyping for the O antigens
Organism is reported as Salmonella, Group B, or C1 or C2, or D, or E (NOT typhi, can be added)
Send to state health lab for complete serotyping
salmonella serological typing
Mainly done in the lab for Salmonella and Shigella; also done on some E coli
O antigens (somatic) heat stabile
K antigens (capsular) heat labile
Salmonella K antigens are known as Vi AGNs
May interfere with expression of O antigens
If it doesn't type, boil org and retest the O antigen tests
H antigens (flagellar) heat labile
e coli gastroenteritis (general)
Pathogenic and nonpathogenic forms of E coli exist
Non-pathogenic forms are NF—predominant species in the gut
Pathogenic forms are not NF
E coli strains are based on serotypes--pathogenicity not associated w specific serotypes
O antigens [somatic antigens]
H antigens [flagellar]
If E coli is suspected of being the cause of the disease, serotyping is often used for diagnosis
list of pathovars of e coli (5)
EIEC (entero-invasive)
ETEC (toxigenic)
EHEC (hemorrhagic)
EPEC (pathogenic)
EAEC (aggregative)
(e coli gastroenteritis pathovars) EIEC (enteroinvasive)
Same as shigella flexneri but not acid tolerant
transmission same; dosage is 10^6 orgs
infection of M cells & spread same
identical virulence factors
Causes disease identical to dysentery
Humans = only known reservoir
Colonization is by pili attaching to intestinal tract cells
EIEC strains do not produce Shiga toxin = no HUS
EIEC strains are LDC neg and almost all are non-motile
Treatment same as shigella dysentery
(e coli gastroenteritis pathovars) ETEC (enterotoxigenic)
Montezuma's revenge
Disease ranges from mild water diarrhea to severe diarrhea that is nearly identical to cholera
Reservoir is humans
Transmission = fecal oral route ; need 10^6 orgs to cause infection
Small intestine is colonized using pili
ETEC in developed vs developing countries
Endemic in developing countries
Causes 1.5 million deaths/year worldwide
800,000 of those deaths are in children <5 yrs
Death due to dehydration
In developed countries:
Associated w limited outbreaks
Usually not fatal
Aka traveler's diarrhea
ETEC (toxigenic) toxins
LT toxin—heat labile toxin
Structurally and functionally similar to cholera toxin
Compound AB toxin
ST toxin--heat stable toxin
Because LT and ST recognize different receptors a wider range of host cells will be poisoned
(e coli gastroenteritis pathovars) EPEC (enteropathogenic)
Serotypes implicated are O35 and O111
Generally mild to moderate diarrhea, but can be severe, cholera like
Infant mortality rate as high as 70% in undeveloped countries
ID’d by serology
Infections are usually self-limiting but can be treated w antibiotics
Humans are the only reservoir
Transmission by fecal-oral route
Need 10^6 orgs to cause infection
Organisms can invade the epithelium, but they really aren't that invasive
No known enterotoxins
(e coli gastroenteritis pathovars) EAEC/EAggEC (enteroaggregative)
Recently identified as pathogenic
Associated with a mild persistent diarrhea in children
Form dense clumps of bacteria on the surface of the epithelial cells
Binding is mediated by fimbriae
Found to produce heat stable toxin—not sure if it has role in the disease
Does not lead to HUS
(gastroenteritis) yersinia sp
GNR w 3 pathogenic speicies
Y pestis--bubonic and pneumonic plague
Y pseudotuberculosis--gastroenteritis (not common is US)
Y enterocolitica--gastroenteritis (common in US)
Both pathogenic and non-pathogenic (lack virulence factors) strains
(gastroenteritis) yersinia enterocolitica
Most prevalent in Scandanavia, Europe, Canada, and some parts of the USA
Produce a heat stable toxin
Similar to that produced by E. coli
Makes it invasive
1988 – Outbreak associated with eating chitterlings
cleaned/boiled pig intestines
Assoc w transfusion acquired sepsis because it can tolerate the cold