Chemical Coordination and Integration
Endocrine Glands and Hormones:
- Endocrine glands lack ducts and are hence, called ductless glands.
- Their ==secretions are called hormones.==
- The classical definition of the hormone as a chemical produced by endocrine glands and released into the blood and transported to a distantly located target organ has a current scientific definition as follows:
- Hormones are ==non-nutrient chemicals that act as intercellular messengers== and are produced in trace amounts.
- The new definition covers a number of new molecules in addition to the hormones secreted by the organized endocrine glands.
- ==Invertebrates possess very simple endocrine systems== with few hormones whereas a large number of chemicals act as hormones and provide coordination in the vertebrates.
Human Endocrine System:
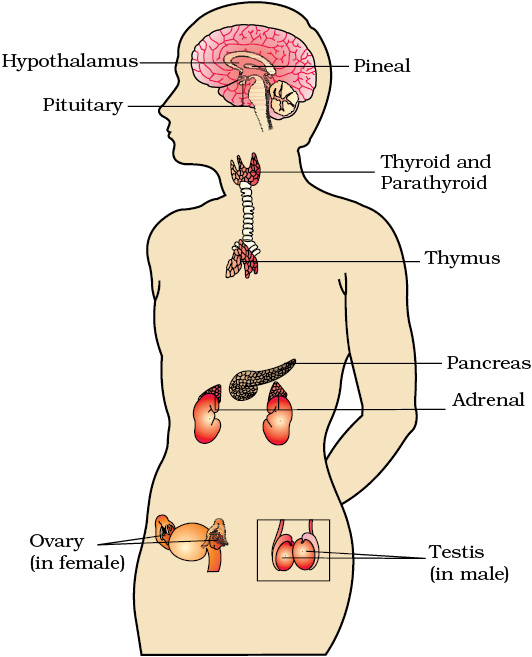
- The endocrine glands and hormone-producing diffused tissues/cells located in different parts of our body constitute the endocrine system.
- The ==pituitary, pineal, thyroid, adrenal, pancreas, parathyroid, thymus, and gonads (testis in males and ovary in females) are the organized endocrine bodies in our body.==
- In addition to these, some other organs:
- E.g., the gastrointestinal tract, liver, kidney, and heart also produce hormones.
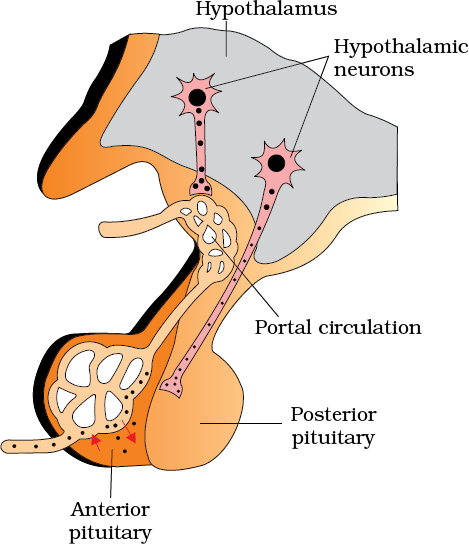
The Hypothalamus:
It contains several groups of ==neurosecretory cells called nuclei== which produce hormones.
These hormones regulate the synthesis and secretion of pituitary hormones.
- However, the hormones produced by the hypothalamus are of two types:
- The releasing hormones (which stimulate secretion of pituitary hormones)
- The inhibiting hormones (which inhibit secretions of pituitary hormones).
- For example, ==a hypothalamic hormone called Gonadotrophin releasing hormone (GnRH) stimulates the pituitary synthesis and release of gonadotropins.==
- ==On the other hand, somatostatin from the hypothalamus inhibits the release of growth hormone from the pituitary.==
These hormones originating in the hypothalamic neurons, pass through axons and are released from their nerve endings.
These hormones reach the pituitary gland through a ==portal circulatory system== and regulate the functions of the anterior pituitary.
The ==posterior pituitary is under the direct neural regulation of the hypothalamus.==
The Pituitary Gland:
The pituitary gland is located in a ==bony cavity called Sella tursica== and is attached to the ==hypothalamus by a stalk==.
It is divided anatomically into -
- Adenohypophysis consists of two portions, pars distalis, and pars intermedia.
- The pars distalis region of the pituitary, commonly called the anterior pituitary, produces growth hormone (GH), prolactin (PRL), thyroid stimulating hormone (TSH), adrenocorticotrophic hormone (ACTH), luteinizing hormone (LH), and follicle-stimulating hormone (FSH).
- Prolactin regulates the ==growth of the mammary glands and the formation of milk== in them.
- Over-secretion of GH stimulates ==abnormal growth of the body leading to gigantism== and low secretion of GH results in ==stunted growth resulting in pituitary dwarfism.==
- Excess secretion of growth hormone in adults especially in middle age can result in ==severe disfigurement== (especially of the face) called Acromegaly, which may lead to serious complications, and premature death if unchecked.
- The disease is hard to diagnose in the early stages and often goes undetected for many years until changes in external features become noticeable.
- ==TSH stimulates the synthesis and secretion of thyroid hormones from the thyroid gland.==
- ==ACTH stimulates the synthesis and secretion of steroid hormones called glucocorticoids from the adrenal cortex.==
- LH and FSH stimulate gonadal activity and hence are called gonadotropins.
- In males, LH stimulates the ==synthesis and secretion of hormones== called androgens from the testis.
- In females, LH induces ==ovulation of fully mature follicles== (Graafian follicles) and ==maintains the corpus luteum==, formed from the remnants of the Graafian follicles after ovulation.
- In males, FSH and androgens ==regulate spermatogenesis.==
- FSH stimulates the ==growth and development of ovarian follicles== in females.
- Pars intermedia secretes only one hormone called ==melanocyte-stimulating hormone (MSH).==
- MSH acts on the melanocytes (melanin-containing cells) and regulates the ==pigmentation of the skin.==
- However, in humans, the ==pars intermedia is almost merged with pars distalis.==
- Neurohypophysis (pars nervosa) also known as posterior pituitary, stores and releases two hormones called ==oxytocin and vasopressin==, which are actually synthesized by the hypothalamus and are transported axonally to the neurohypophysis.
- ==Oxytocin acts on the smooth muscles of our body and stimulates their contraction.==
- In females, it stimulates a ==vigorous contraction of the uterus at the time of childbirth, and milk ejection== from the mammary gland.
- Vasopressin acts mainly in the kidney and ==stimulates the resorption of water and electrolytes by the distal tubules== and thereby reducing the loss of water through urine (diuresis).
- Hence, it is also called anti-diuretic hormone (ADH).
- An impairment affecting the synthesis or release of ADH results in a diminished ability of the kidney to conserve water leading to water loss and dehydration.
- This condition is known as ==Diabetes Insipidus.==
The Pineal Gland:
- The pineal gland is located on the dorsal side of the forebrain.
- Pineal secretes a hormone called ==melatonin.==
- Melatonin plays a very important role in the ==regulation of a 24-hour (diurnal) rhythm of our body.==
- For example, it helps in maintaining the normal rhythms of the sleep-wake cycle, and body temperature.
- In addition, melatonin also influences ==metabolism, pigmentation, the menstrual cycle as well as our defense capability.==
Thyroid Gland:
The thyroid gland is composed of two lobes which are located on either side of the trachea.
- Both lobes are interconnected with a thin flap of connective tissue called the isthmus.
The thyroid gland is composed of follicles and stromal tissues.
- Each thyroid follicle is composed of follicular cells, enclosing a cavity.
- These follicular cells synthesize two hormones, ==tetraiodothyronine or thyroxine (T4 ) and triiodothyronine (T3 ).==
- ==Iodine== is essential for the normal rate of hormone synthesis in the thyroid.
- The deficiency of iodine in our diet results in ==hypothyroidism and enlargement of the thyroid gland commonly called goiter.==
- Hypothyroidism during pregnancy causes defective development and maturation of the growing baby leading to stunted growth ==(cretinism)==, mental retardation, low intelligence quotient, abnormal skin, deaf-mutism, etc.
- In adult women, ==hypothyroidism may cause the menstrual cycle to become irregular.==
- Due to cancer of the thyroid gland or due to the development of nodules of the thyroid glands, the rate of synthesis and secretion of the thyroid hormones is increased to abnormally high levels leading to a condition called ==hyperthyroidism== which adversely affects the body's physiology.
- Exophthalmic goiter is a form of hyperthyroidism, characterized by enlargement of the thyroid gland, protrusion of the eyeballs, increased basal metabolic rate, and weight loss also called ==Graves’ disease.==
- Thyroid hormones play an important role in the regulation of the basal metabolic rate.
- These hormones also support the process of ==red blood cell formation.==
- Thyroid hormones control the ==metabolism of carbohydrates, proteins, and fats.==
- The ==maintenance of water and electrolyte balance== is also influenced by thyroid hormones.
The thyroid gland also secretes a ==protein hormone called thyrocalcitonin== (TCT) which regulates the ==blood calcium levels.==
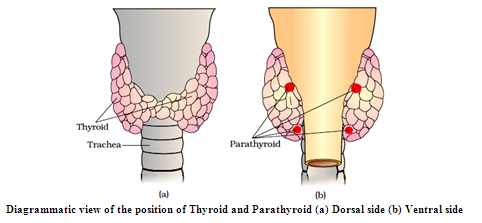
Parathyroid Gland:
- In humans, four parathyroid glands are present on the back side of the thyroid gland, one pair each in the two lobes of the thyroid gland.
- The parathyroid glands secrete a peptide hormone called parathyroid hormone (PTH).
- The secretion of PTH is regulated by the circulating levels of calcium ions.
- Parathyroid hormone (PTH) ==increases the Ca2+ levels in the blood.==
- PTH acts on bones and stimulates the ==process of bone resorption== (dissolution/demineralization).
- PTH also stimulates the ==reabsorption of Ca2+ by the renal tubules and increases Ca2+ absorption from the digested food.==
- It is, thus, clear that PTH is a ==hypercalcemic== hormone, i.e., ==it increases the blood Ca2+ levels.==
- Along with TCT, it plays a significant role in calcium balance in the body
Thymus:
- The thymus gland is a lobular structure located between lungs behind the sternum on the ventral side of the aorta.
- The thymus plays a major role in the development of the immune system.
- This gland secretes the ==peptide hormones called thymosins.==
- Thymosins play a major role in the ==differentiation of T-lymphocytes==, which provide ==cell-mediated immunity.==
- In addition, thymosins also promote ==the production of antibodies to provide humoral immunity.==
- The ==thymus is degenerated in old individuals== resulting in a decreased production of thymosins.
- As a result, the immune responses of old persons become weak.
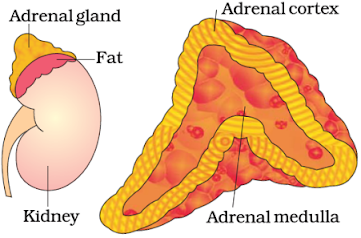
Adrenal Gland:
Our body has one pair of adrenal glands, one at the anterior part of each kidney.
The gland is composed of two types of tissues.
- The centrally located tissue is called the adrenal medulla, and outside this lies the adrenal cortex.
- The underproduction of hormones by the adrenal cortex alters carbohydrate metabolism causing acute weakness and fatigue leading to a disease called ==Addison’s disease.==
- The adrenal medulla secretes two hormones called ==adrenaline or epinephrine and noradrenaline or norepinephrine.==
- These are commonly called ==catecholamines.==
Adrenaline and noradrenaline are rapidly secreted in response to the ==stress== of any kind and during ==emergency situations== and are called emergency hormones or hormones of Fight or Flight.
- These hormones increase ==alertness, pupillary dilation, piloerection (raising of hair), sweating, etc.==
- Both the hormones increase the ==heartbeat, the strength of heart contraction, and the rate of respiration.==
Catecholamines also stimulate the ==breakdown of glycogen== resulting in an increased ==concentration of glucose== in the blood.
- In addition, they also stimulate the ==breakdown of lipids and proteins==.
The adrenal cortex can be divided into three layers, called:
- zona reticularis (inner layer)
- zona fasciculata (middle layer)
- zona glomerulosa (outer layer).
The adrenal cortex secretes many hormones, commonly called corticoids.
- The corticoids, which are involved in carbohydrate metabolism are called glucocorticoids.
- ==In our body, cortisol is the main glucocorticoid.==
- Glucocorticoids stimulate ==gluconeogenesis, lipolysis, and proteolysis==; and inhibit ==cellular uptake and utilization of amino acids.==
- Glucocorticoids, particularly cortisol, produce ==anti-inflammatory reactions and suppress the immune response.==
- Corticoids, which regulate the ==balance of water and electrolytes== in our body is called ==mineralocorticoids.==
- ==Aldosterone== is the main mineralocorticoid in our body.
- Aldosterone acts mainly at the renal tubules and stimulates the ==reabsorption of Na+ and water and the excretion of K+ and phosphate ions.==
- Thus, aldosterone helps in the ==maintenance of electrolytes, body fluid volume, osmotic pressure, and blood pressure.==
- Cortisol is also involved in maintaining the ==cardiovascular system== as well as kidney functions.
- Cortisol stimulates ==RBC production.==
Small amounts of androgenic steroids are also secreted by the adrenal cortex which plays a role in the ==growth of axial hair, pubic hair, and facial hair== during puberty.
Pancreas:
- The pancreas is a composite gland that acts as both exocrine and endocrine glands.
- The endocrine pancreas consists of ‘Islets of Langerhans’.
- There are about 1 to 2 million Islets of Langerhans in a normal human pancreas representing only 1 to 2 percent of the pancreatic tissue.
- The two main types of cells in the Islet of Langerhans are called α-cells and β-cells.
- The α-cells secrete a hormone called glucagon, while the β-cells secrete insulin.
- Glucagon is a peptide hormone and plays an important role in ==maintaining normal blood glucose levels.==
- Glucagon acts mainly on the ==liver cells (hepatocytes) and stimulates glycogenolysis resulting== in increased blood sugar (hyperglycemia).
- In addition, this hormone stimulates the process of ==gluconeogenesis== which also contributes to hyperglycemia.
- Glucagon reduces cellular ==glucose uptake and utilization==.
- Thus, glucagon is a hyperglycemic hormone.
- ==Insulin is a peptide hormone==, which plays a major role in the regulation of glucose homeostasis.
- Insulin acts mainly on ==hepatocytes and adipocytes== (cells of adipose tissue) and ==enhances cellular glucose== uptake and utilization.
- As a result, there is a rapid movement of glucose from the blood to hepatocytes and adipocytes resulting in ==decreased blood glucose levels== (hypoglycemia).
- Insulin also stimulates the ==conversion of glucose to glycogen== (glycogenesis) in the target cells.
- The glucose homeostasis in the blood is thus maintained jointly by the two – insulin and glucagon.
- Prolonged hyperglycemia leads to a complex disorder called ==diabetes mellitus which is associated with loss of glucose== through urine and the formation of harmful compounds known as ==ketone bodies.==
- Diabetic patients are successfully treated with ==insulin therapy.==
Testis:
- A pair of the testis is present in the scrotal sac (outside abdomen) of male individuals.
- Testis performs dual functions as a primary sex organ as well as an endocrine gland.
- The testis is composed of seminiferous tubules and stromal or interstitial tissue.
- The Leydig cells or interstitial cells, which are present in the intertubular spaces produce a group of hormones called ==androgens mainly testosterone.==
- Androgens regulate the ==development, maturation, and functions of the male accessory sex organs like epididymis, vas deferens, seminal vesicles, prostate gland, urethra,== etc.
- These hormones stimulate ==muscular growth, growth of facial and axillary hair, aggressiveness, low pitch of voice==, etc.
- Androgens play a major stimulatory role in the process of ==spermatogenesis== (formation of spermatozoa).
- Androgens act on the central neural system and influence ==male sexual behavior (libido).==
- These hormones produce ==anabolic (synthetic) effects on protein and carbohydrate metabolism.==
Ovary:
- Females have a pair of ovaries located in the abdomen.
- The ovary is the primary female sex organ that produces one ovum during each menstrual cycle.
- In addition, the ovary also produces two groups of steroid hormones called:
- Estrogen
- The estrogen is synthesized and secreted mainly by the growing ==ovarian follicles.==
- Estrogens produce wide-ranging actions such as stimulation of ==growth and activities of female secondary sex organs, development of growing ovarian follicles, the appearance of female secondary sex characters (e.g., the high pitch of voice, etc.), and mammary gland development.==
- Estrogens also regulate ==female sexual behavior.==
- Progesterone.
- After ovulation, the ruptured follicle is converted to a structure called ==corpus luteum, which secretes mainly progesterone.==
- Progesterone supports a ==pregnancy.==
- Progesterone also acts on the ==mammary glands and stimulates the formation of alveoli== (sac-like structures which store milk) and ==milk secretion.==
- The ovary is composed of ==ovarian follicles and stromal tissues.==
Hormones of Heart, Kidney, and Gastrointestinal Tract:
- Hormones are secreted by some tissues which are not endocrine glands.
- For example, the atrial wall of our heart secretes a very important peptide hormone called atrial natriuretic factor (ANF), which decreases blood pressure.
- When blood pressure is increased, ANF is secreted which causes ==dilation of the blood vessels.==
- This ==reduces blood pressure.==
- The juxtaglomerular cells of the kidney produce a peptide hormone called ==erythropoietin which stimulates erythropoiesi==s (formation of RBC).
- Endocrine cells present in different parts of the gastrointestinal tract secrete four major peptide hormones, namely:
- Gastrin:
- It acts on the gastric glands and stimulates the secretion of hydrochloric acid and pepsinogen.
- Secretin
- It acts on the exocrine pancreas and stimulates the secretion of water and bicarbonate ions.
- Cholecystokinin (CCK)
- It acts on both the pancreas and gall bladder and stimulates the secretion of pancreatic enzymes and bile juice, respectively.
- Gastric inhibitory peptide (GIP).
- GIP inhibits gastric secretion and motility.
- Several other non-endocrine tissues secrete hormones called growth factors.
- These factors are essential for the normal growth of tissues and their repairing/regeneration.
Mechanism of Hormone Action:
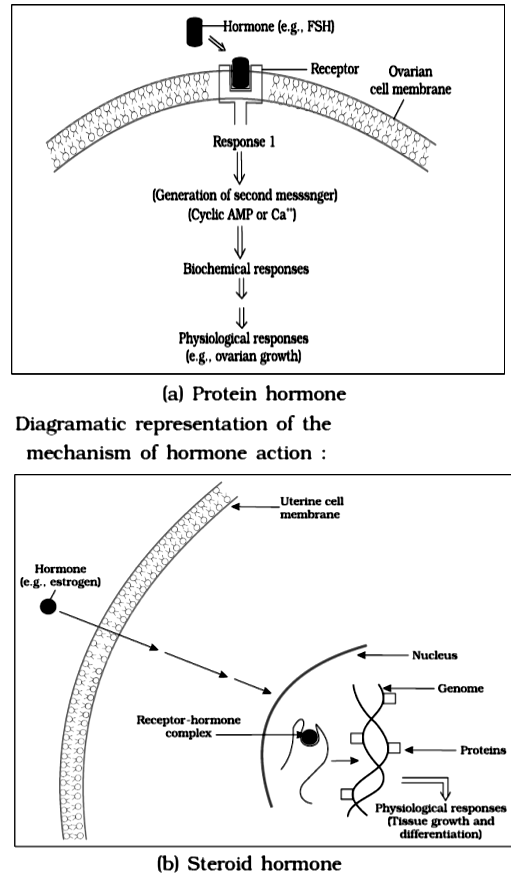
Hormones produce their effects on target tissues by binding to specific proteins called hormone receptors located in the target tissues only.
Hormone receptors present on the cell membrane of the target cells are called membrane-bound receptors and the receptors present inside the target cell are called intracellular receptors, mostly nuclear receptors (present in the nucleus).
The binding of a hormone to its receptor leads to the formation of a hormone-receptor complex.
- Each receptor is specific to one hormone only and hence receptors are specific.
- Hormone-Receptor complex formation leads to certain biochemical changes in the target tissue.
- Target tissue metabolism and hence physiological functions are regulated by hormones.
On the basis of their chemical nature, hormones can be divided into groups :
- Peptide, polypeptide, protein hormones (e.g., insulin, glucagon, pituitary hormones, hypothalamic hormones, etc.)
- Steroids (e.g., cortisol, testosterone, estradiol and progesterone)
- Iodothyronines (thyroid hormones)
- Amino-acid derivatives (e.g., epinephrine).
Hormones that interact with membrane-bound receptors normally do not enter the target cell, but generate second messengers (e.g., cyclic AMP, IP3 , Ca++ etc) which in turn regulate cellular metabolism.
Hormones that interact with intracellular receptors (e.g., steroid hormones, iodothyronines, etc.) mostly regulate gene expression or chromosome function by the interaction of the hormone-receptor complex with the genome.
Cumulative biochemical actions result in physiological and developmental effects.