1: Energy and Fuel Metabolism Fed and Fasted State
1/121
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
122 Terms
What are the main components of food from which energy can be captured/stored (fed state)? energy production via ________
proteins, fats, carbohydrates; oxidation

In fasting state, we release _____ from glycogen. Making glucose de nova is called ____. Protein can be broken down to make _______.
In the fasting state, we release fat and carbon as glucose from glycogen, making glucose de nova (gluconeogenesis), break down protein to make glucose
Where is most ATP made?
oxidative phosphorylation
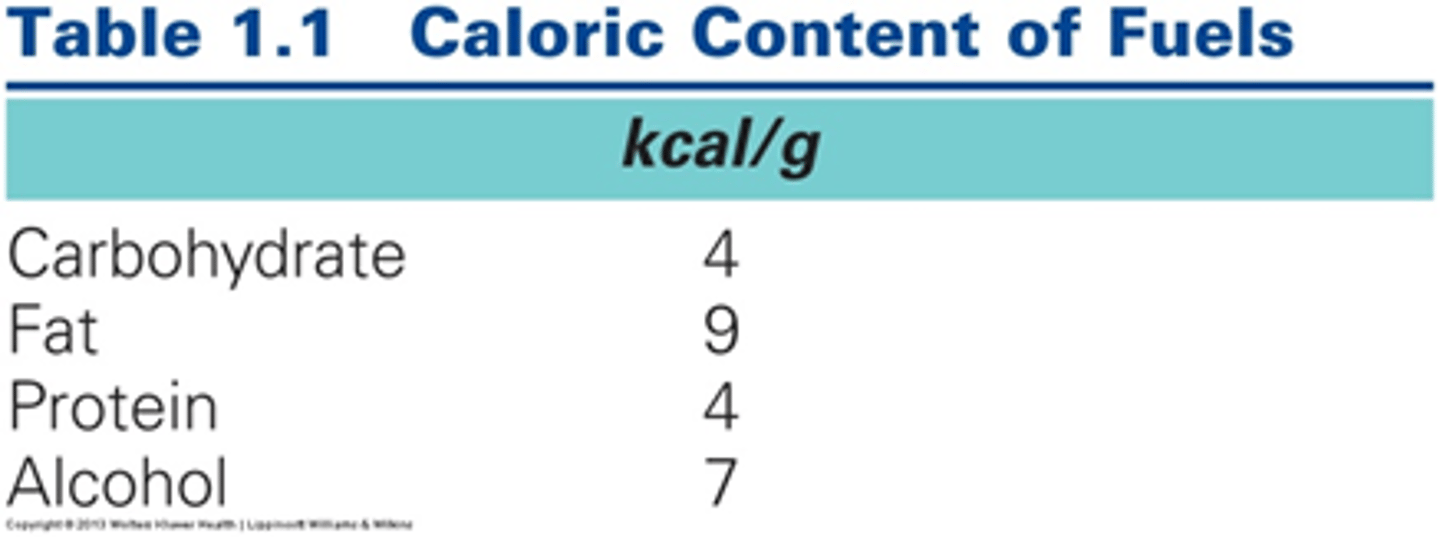
What are the caloric contents of the main fuels obtained from food?
ATP Structure - chemical reasoning behind hydrolysis
we have hydrolysis (split water), and we cleave one of the phosphate-phosphate bonds. This releases energy.
3 phosphate groups packed puts strain/energy for - charges to be close. Hydrolyzing - releases energy (energy used to drive the process forward)
We intake compounds for _______. What biomolecules and extra component needed?
biosynthesis. Proteins, lipids, carbs, and nucleic acids with co-factors for proteins.
What are the three possible fates for ingested food?
metabolism (fuel oxidation catabolism or biosynthesis anabolism), fuel storage, or detox (ethanol) and waste disposal
What are the two types of metabolism ingested food may undergo?
fuel oxidation (catabolism) or biosynthesis (anabolism)
Glucose needs to be in ____ at all times
This has to be present in blood at all times.
Glucose can make _____ to make glycogen. Glucose is stored in _____ and _____. Plants linking glucose form _______.
We can make polymers of glucose (link monomers) to make glycogen. Glucose stored in liver/muscles. Plants: linking glucose = starch.
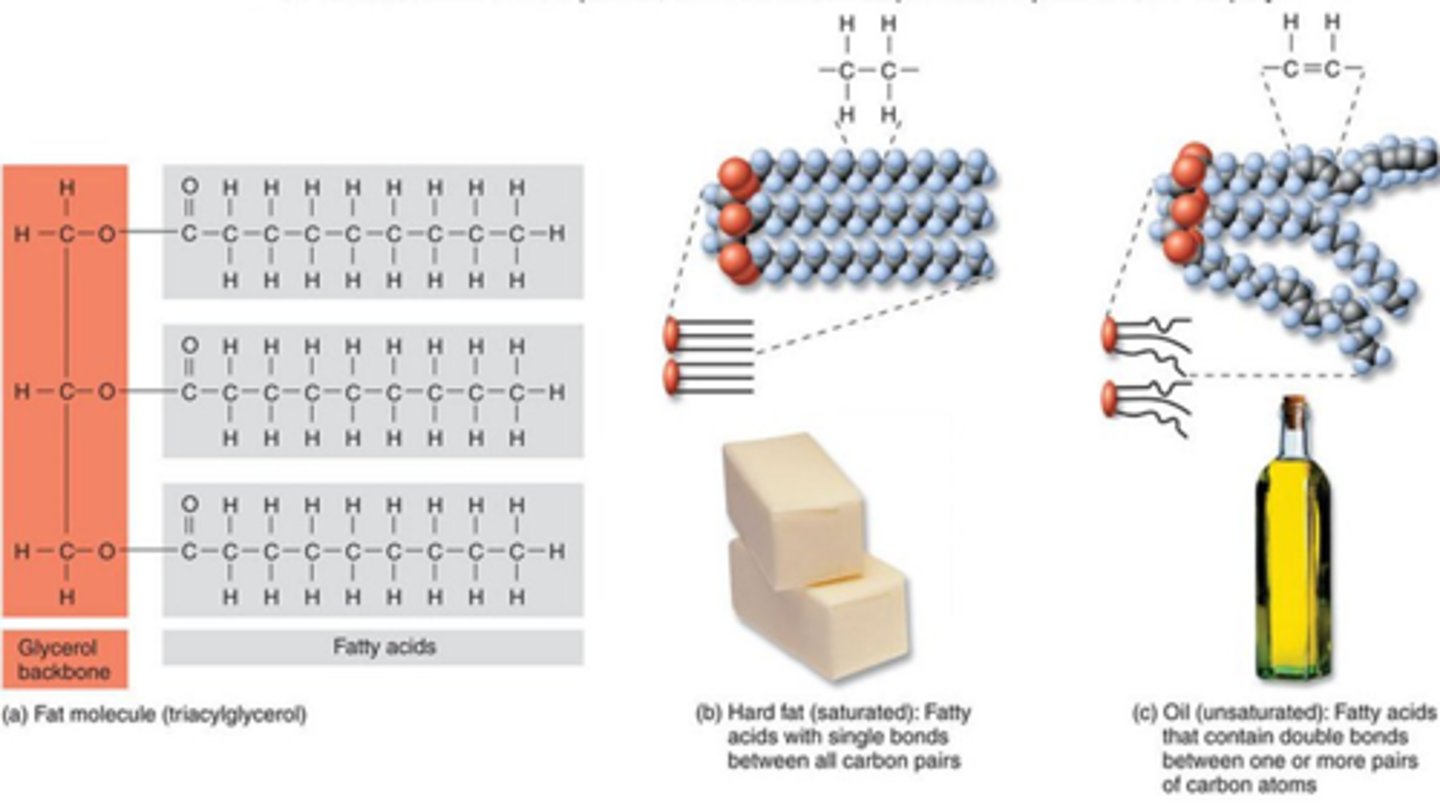
Triglyceride structure
Triglyceride refers to hydrophobic molecule (glycerol backbone and esterified to each carbon of glycerol backbone a fatty acid chain. Tri (three fatty acids). Acyl (hydrocarbon chains). Glycerol (backbone)
How do saturated and unsaturated fatty acids differ?
Saturated doesnt have double bonds - like coconut oil - while unsaturated has one or more double bonds - kink.
How will saturated and unsaturated fats behave at room temperature?
Saturated will be hard and unsaturated will be liquid
What is another name for a fat molecule?
triacylglycerol
Where is the majority of the fuel within the body stored?
fat
If we go on a protein or carb only diet, we gain weight stored as ____
fat. Convert macromolecule to fat if we have an excess over what body needs. Excess glucose = lipogenesis. Amino acid - N group off to make FA.
Muscle glycogen, liver glycogen, and protein as fuel storages.
Which one is most important?A
Glycogen is the most imp liver source to maintain blood glucose even if its the least.
Glycogen is also stored in muscles (a lil more) but is selfish unlike liver.
Protein greater than both - protein muscle broken down to make glucose.
What is the daily energy expenditure?
basal metabolic rate + physical activity
What is basal metabolic rate?
the rate at which the body uses energy while at rest to keep vital functions going
how does BMR change with age, sex, body size, and physiological conditions (exercise, sick, pregnant)?
decreases with age (young - high), more in men cuz more muscle, more body mass = high BMR, more active = high BMR, sick = high BMR, pregnancy = high BMR
How will physical activity be estimated to calculate DEE?
30% BMR for sedentary, 60% BMR for moderate activity, and 100% BMR for heavy activity
How are pounds converted to kg?
1 kg/2.2 lbs x wt in lbs = wt in kg
How is BMR calculated?
24 kcal/day/kg x wt in kg (males)
21.6 kcal/day/kg x wt in kg (females)
How is DEE calculated?
DEE = BMR (kcal/day) x 1.(activity level factor)
Activity Components (sedentary, moderate, high)
Sedentary: 30% of the BMR (0.30 converted to 1.3) e.g., desk job and no exercise
Moderate activity: 60% of the BMR (0.60 converted to 1.6) e.g., 2h moderate exercise/day
High activity: 100% of the BMR (1.00 converted to 2) e.g., 2-3h vigorous exercise/day
DEE
DEE is how many kcal at that activity level to maintain their body weight
DEE>BMR or DEE
lose weight; not meeting energy requirements so gain weight
How is BMI calculated?
weight in kg/height in meters squared
What does the number of a BMI indicate?
<18.5 underwt
18.5
obese
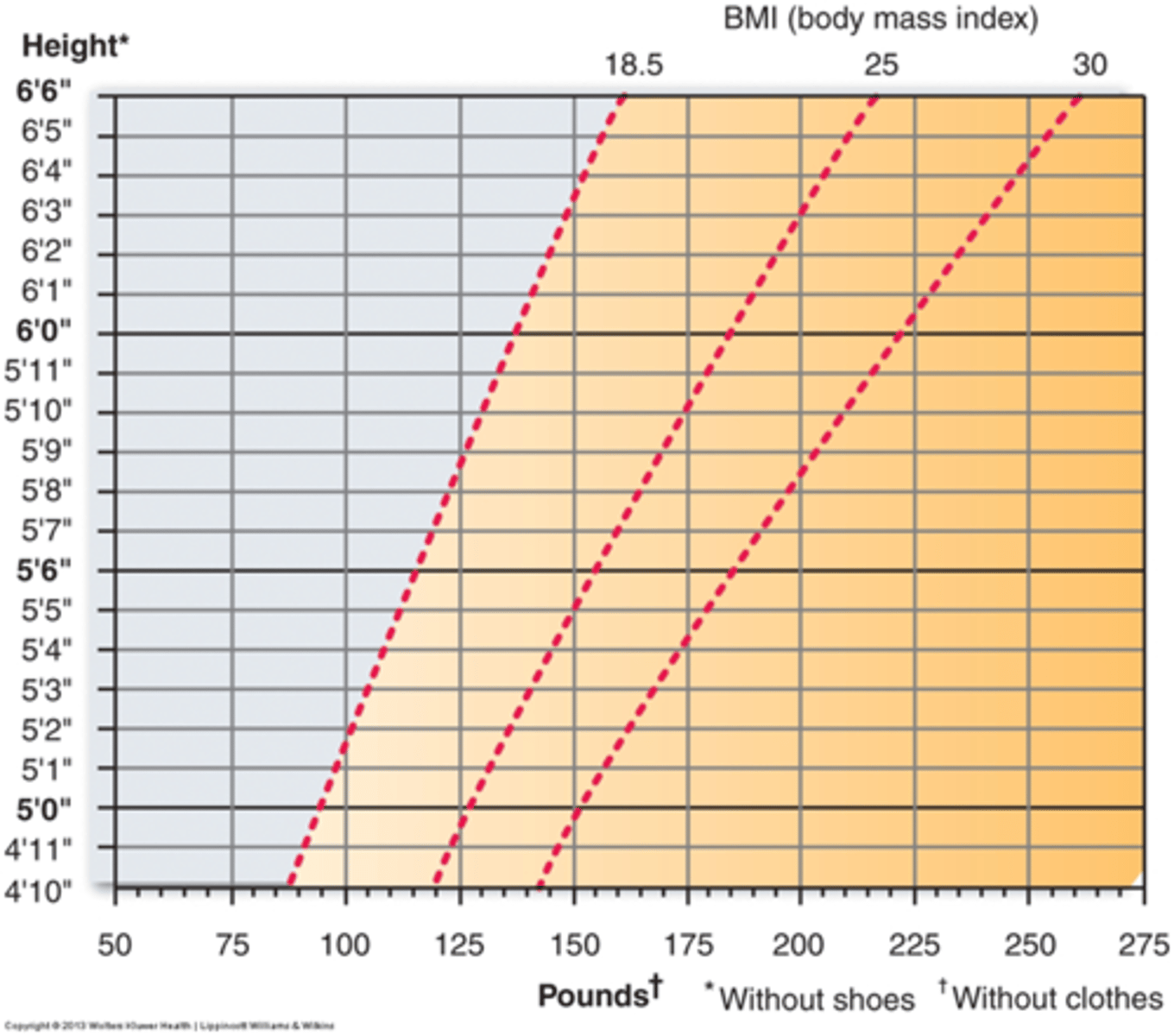
Recommended BMI - why isn't it perfect
18.5-24.9 is recommended BMI; doesn't account for muscle or fat distribution so athlete could be considered obsese
What amount of calories would someone want to consume to maintain weight?
consume same amount of calories as DEE (cals out=cals in)
What does it take to lose a pond through diet?
500 cal/day less that DEE (lose 1 pound per week)
What does it take to lose a pound through exercise?
work/expend 3500 calories to lose one pound
FAD Diet and Rapid Weight Loss
loss of a significant amount of water weight rather than just fat. '
The body loses glycogen and water when calorie intake is reduced so BMR decreases in starvation mode to conserve energy.
Decrease in BMR: The body burns fewer calories at rest and when returning to a normal diet, gains weight more quickly even if it is the same nutrients they consumed before the diet.
What type of foods should be eaten to maintain a helathy diet?
nutrient dense foods
What are the essential fatty acids from plant sources? for what?
alpha-linolenic acid (omega 3)
linoleum acid (omega 6)
Essential fatty acids to make membrane lipids/signaling molecules that body can't make.
What are the essential fatty acids from animal sources?
alpha-linolenic acid
eicosapentaenoic acid (EPA)
docosahexaenoic acid (DHA)
What are essential amino acids?
Body can not produce so must be obtained by body
Threonine, Histidine, Isoleucine, Lysine, Valine, Tryptophan, Phenylalanine, Methionine, and Leucine
Which source of protein is better and why?
animal as it has all the essential aa in adequate amounts (plants lack some aa)
What amino acids are especially important in children and pregnant women?
Arginine (R) and histidine (H) (think moms are the Real Heroes)
WHat aa is tyrosine made from?
phenylalanine (important in people with PKU!)
What aa is cysteine made from?
methionine
How are free aa acids used?
to make protein, precursors, and oxidized to make energy (think free aa POP)
What type of patient might exhibit a positive nitrogen balance?
children and pregnant women (think positive growing). Good thing.
What type of patient might exhibit a negative nitrogen balance?
people not eating enough/the right proteins (think kwashiorkor)
What leads to edema in patients with kwashiorkor?
decreased serum proteins (albumin) (think has a pot belly) - hypoalbuminemia
kwashiorkor - how does it cause anemia
can't synthesize hemoglobin (lack of protein)
How does Kwashiorkor affect protein synthesis?
negative nitrogen balance and lack of essential aas leads to inability to synthesize proteins
What will the diet of a patient with kwashiorkor contain?
adequate calories but lack of protein
What is marasmus?
caloric deficiency
Marasmus clinical representations
skin and bones; loss of body fat & muscle wasting
What are the water soluble vitamins?
fat solube?
B and C
A, D, E, K
Vitamin
organic molecules required in small amts. Used as a cofactor for enzymes. Make coenzymes.
What will a patient with a vitamin A deficiency present with?
night blindness, skin problems (dry/scaly skin), and keratinization of epithelium in GI, respiratory, and GU tract
What is the solubility of vitamin A?
fat soluble
What sources does vitamin A come from?
eggs, meat, dairy, green leafy veggies, and intensely colored vegetables
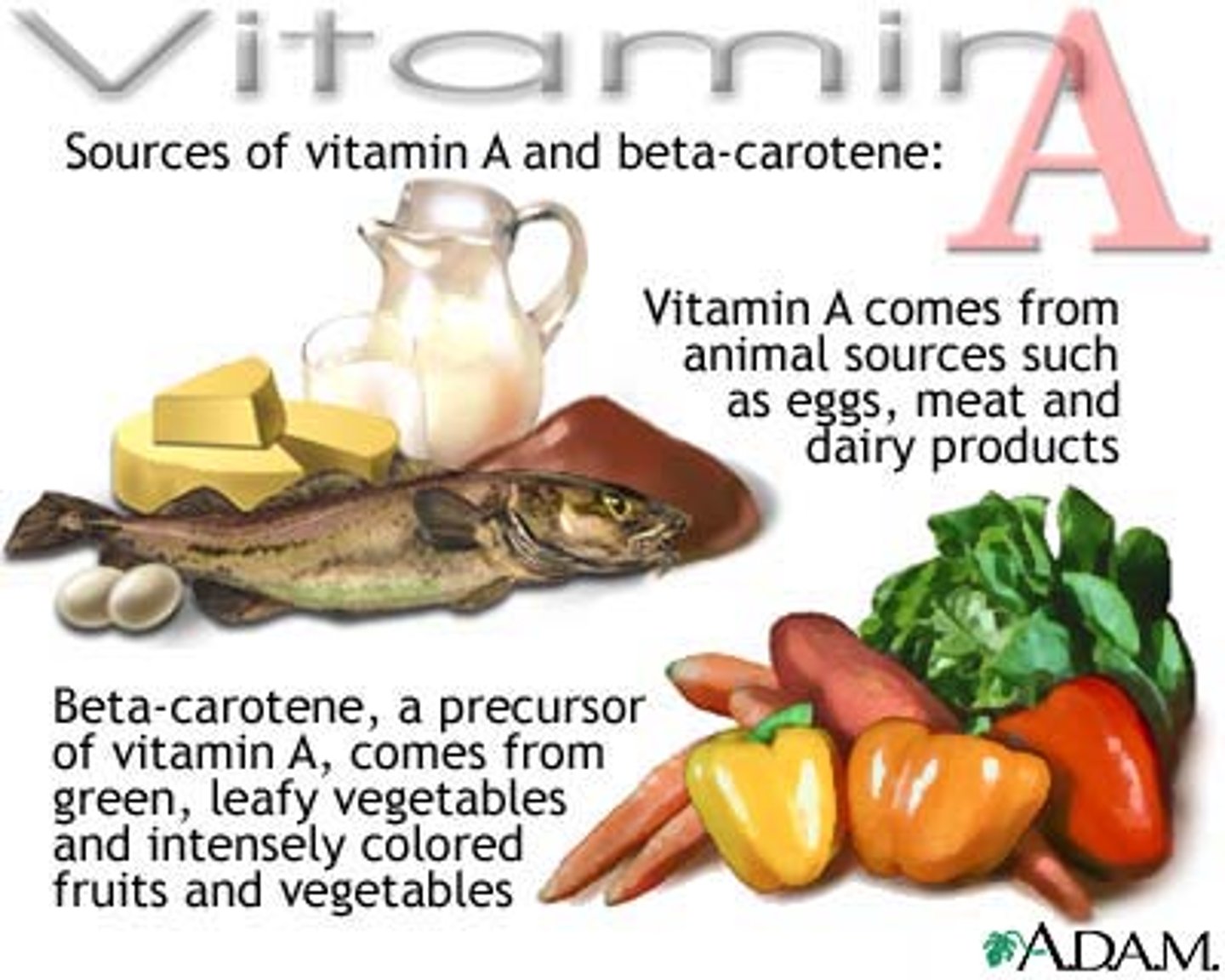
What is the precursor to vitamin A?
beta-carotene
What are the benefit of vitamin A?
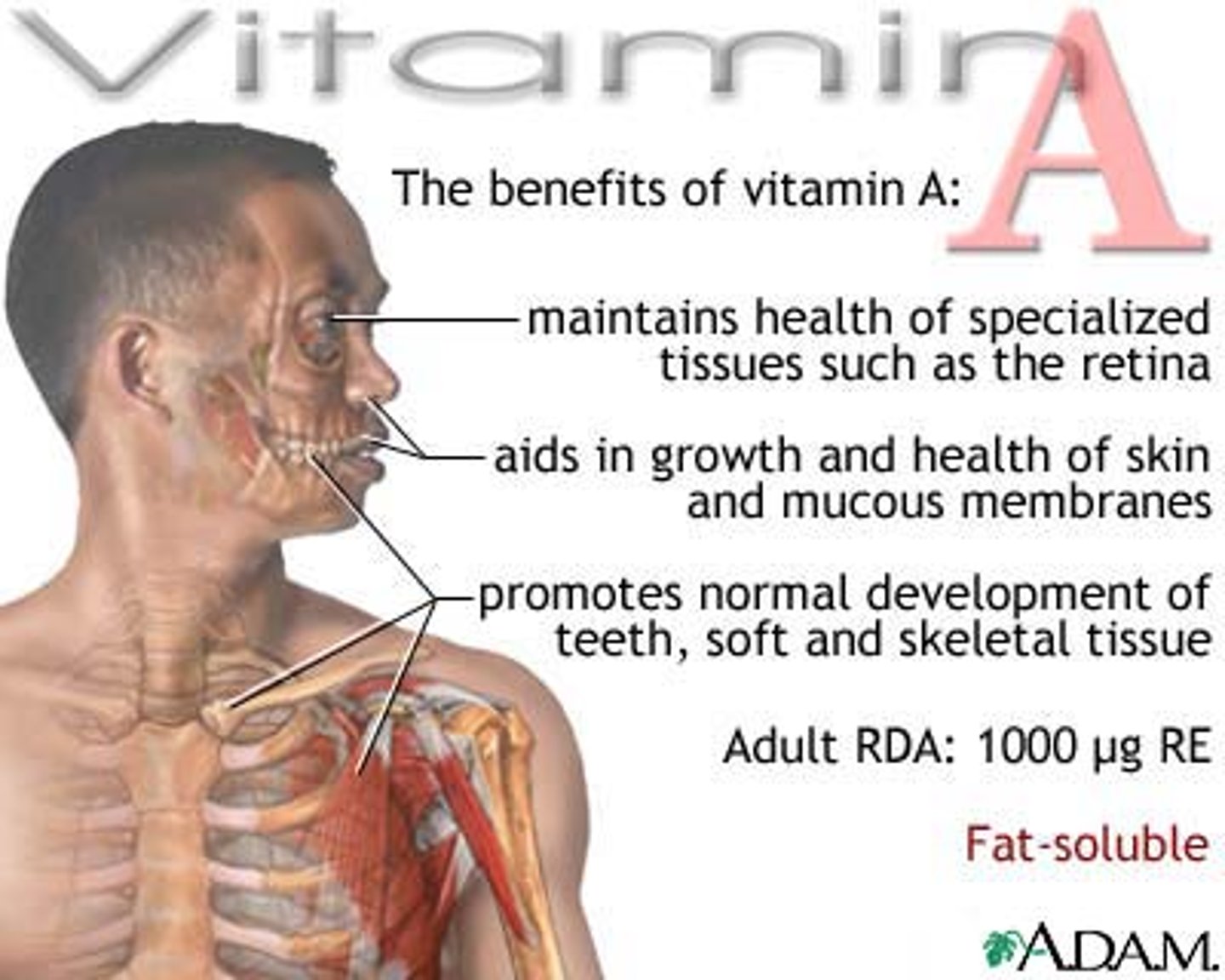
Vitamin A Consequences of Deficiency
night blindness, dry/scaly skin, keratinization of epithelium in. Gi/resp/Gu tract
Why is Vitamin A harder to have a deficiency in?
Fat-soluble vitamins. Harder to develop deficiency since they are fat-soluble so stored in adipose tissue. Takes time to have enough deficit that a deficiency develops.
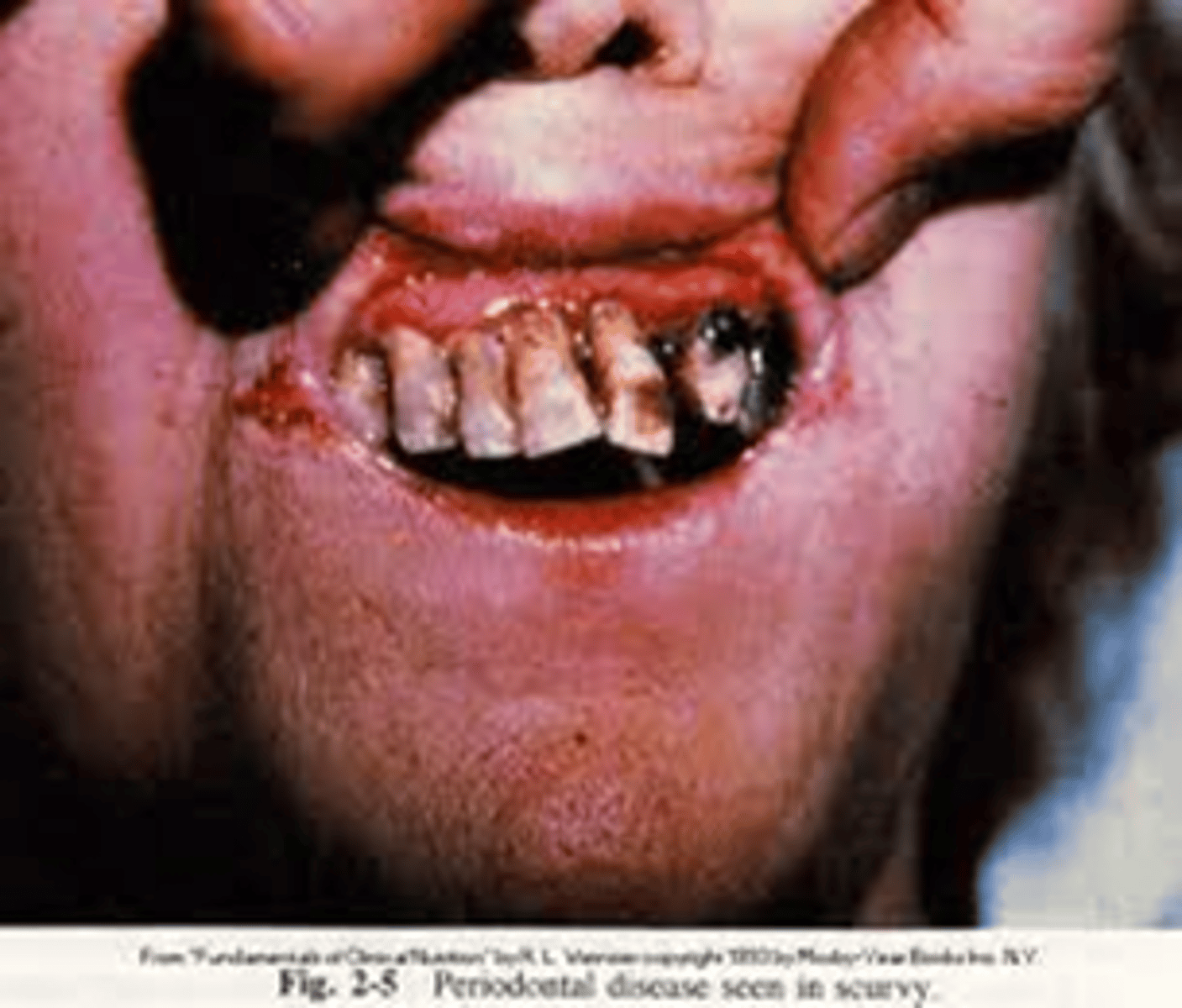
What vitamin is deficient in a patient with scurvy?
vitamin C
What are the characteristic signs of vitamin C deficiency?
scurvy characterized by weakness, anemia, bruising, bleeding gums, subcutaneous hemorrhage, and loose teeth
Defect in collagen formation: needed for cofactor for enzyme
arching bones, joints, and muscles in adults
rigid position, pain (infants)
What are good sources of vitamin C?
Citrus fruits and vegetables, green pepper, broccoli, strawberries, potatoes
What are the characteristic signs of pellagra?
dementia, diarrhea, dermatitis, death (4 d's) and red tongue
Dermatitis: develop photosensitivity (reddened skin areas anywhere sun exposed like face, neck, hands, feet if outside w/o shoes. Pigmented rash in sun-exposed areas. Develop bright red tongue - buzz word
diarrhea, constipation, vomiting - GI upset.
Dementia - Any neurological signs/symptoms like hearing voices/sounds not there. Have lack of sensation or sensation that shouldn’t be there. Neurologic symptom.
Death - severe/prolonged niacin deficiency. Leading up to that point: skin, bright red tongue, Gi, and neurological symptoms
What vitamin is insufficient in a patient with pellagra?
vitamin B3 (niacin)
What are good sources of niacin?
poultry, fish, lean meat, eggs, dairy, and nuts
What is the function of vitamin K?
blood coagulation
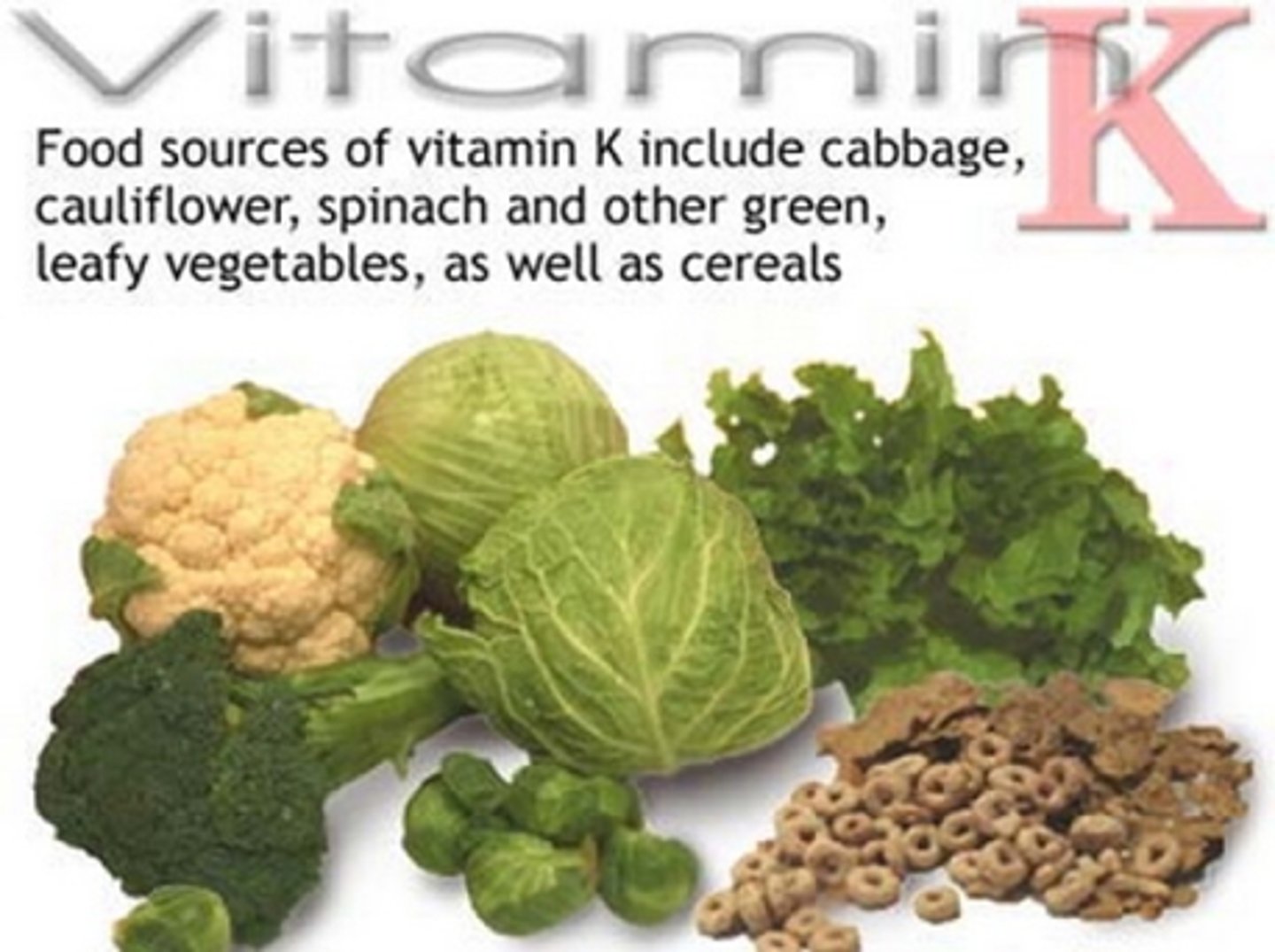
What are good sources of vitamin K?
cabbage, cauliflower, spinach, other green leafy veggies, and cereal (think vitamin Kale)
What are the characteristic signs of vitamin K deficiency?
defective blood coagulation, hemorrhagic anemia of newborn (rare but fatal)
All newborns Vitamin K shot (extra doesn't hurt them) but susceptibility to hemorrhagic anemia is counteracting that.
What vitamin is deficient in a patient with rickets?
vitamin D
What is rickets?
weakening and softening of the bones brought on by extreme calcium loss (due to low vitamin D)
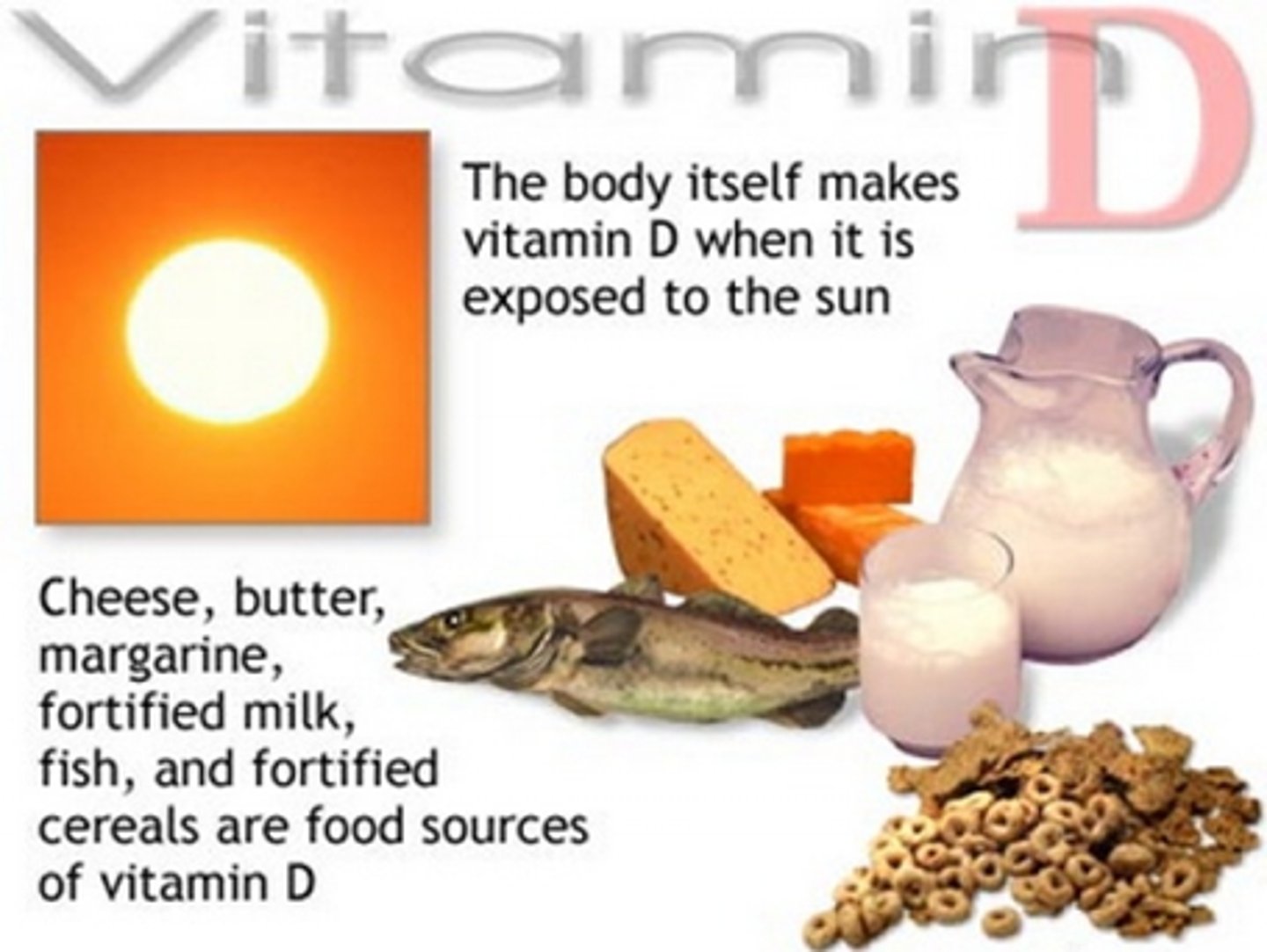
What are good sources of vitamin D?
sunlight exposure, salmon, fortified whole milk, fortified cereal, cheese, butter, and margarine
Vitamin D - can make in body via sunlight (UV light). To have a a vitamin D deficiency develop, deficient in diet but also location where ur not getting enough sunlight exposure. Higher latitudes - dietary deficiency + not getting enough sunlight exposure
What are the characteristic signs of vitamin D deficiency?
Children - rickets (softening of long bones - bowing)
Adults - osteomalacia (inadequate bone mineralization)
In adults is referred to osteomalacia (losing calcium from bones already solidified). Osteomalacia - referred to as stones, moans, and groans due to joint pain.
What are the characteristic signs of vitamin B12 deficiency?
impaired cell division, growth
megaloblastic anemia
neurologic symptoms like tingling in extremities, changes in balance/gate, buzzing in ears
Think "stay 12 feet from the blast (megaloblastic anemia) or you'll develop neurologic symptoms and impair your growth"
What are good sources of vitamin B12?
eggs, meat, poultry, shellfish, milk, and milk products. It is also added to fortified grain products, such as cereals
What is the function of vitamin B12?
Important for metabolism, the formation of RBCs, and maintenance of the CNS
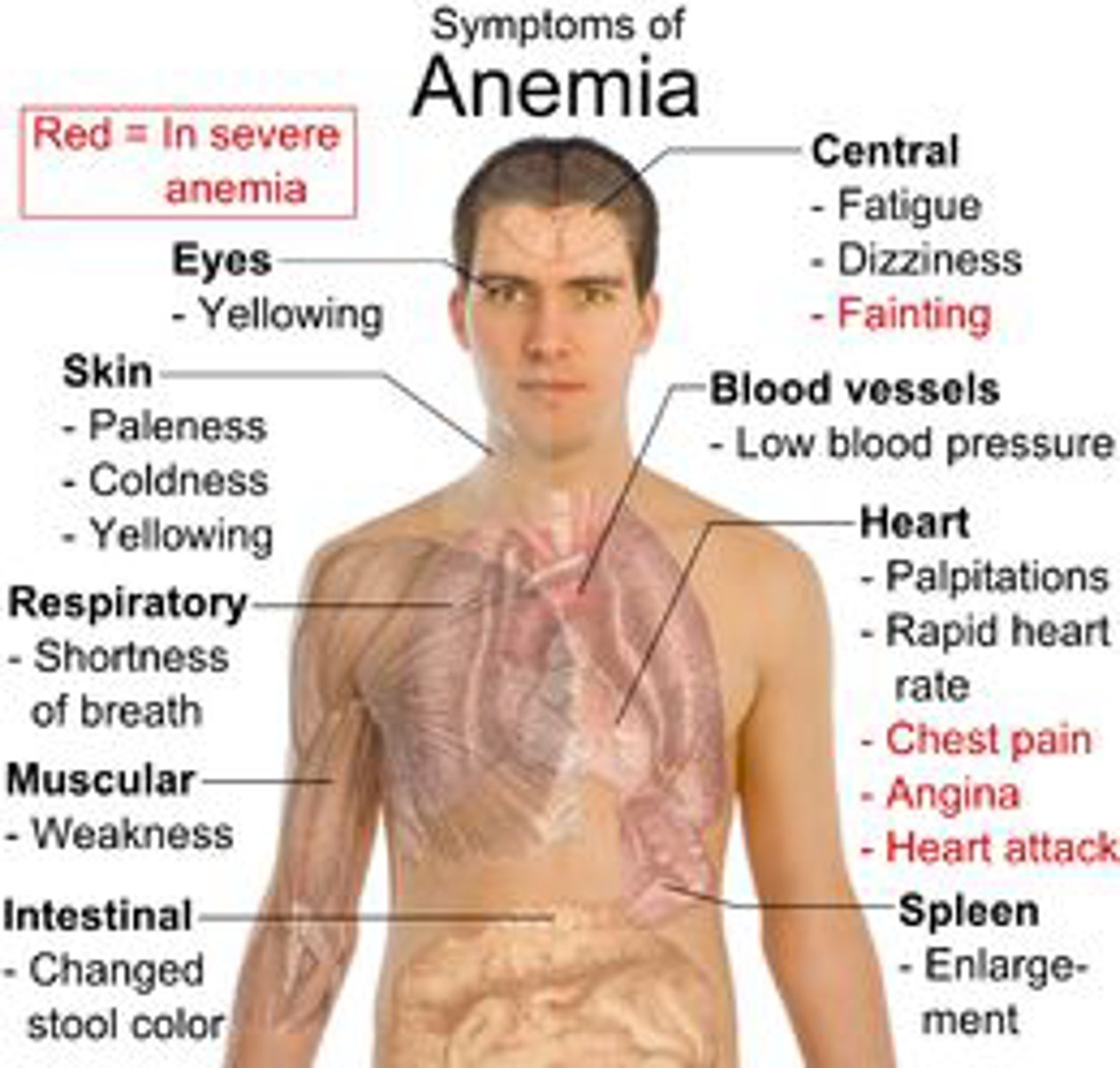
What are the symptoms of anemia?
don't have to know too much
What is the other term for vitamin B9?
folate
What are characteristic signs of vitamin B9 (folate) deficiency?
Impaired cell division/growth, megaloblastic anemia (immature RBC), neural tube defects.
Anemia: tired, fatigued, shortness of breath (SOB), physically appear tired, labs has low RBC
Megaloblastic anemia - some cells didn't mature properly like neutrophil with segmented part in it.
What are good sources of vitamin B9?
beans, legumes, citrus fruits and juices, whole grains, dark green leafy vegetables, poultry, pork, shellfish, and liver
What are the functions of vitamin B9?
Aids in production of RBCs, aids in synthesis of DNA, works with B12 and vitamin C to help the body digest
Why does what we eat matter?
can reduce risk of chronic degenerative disease
What does the fed state encompass?
beginning to completion of absorption
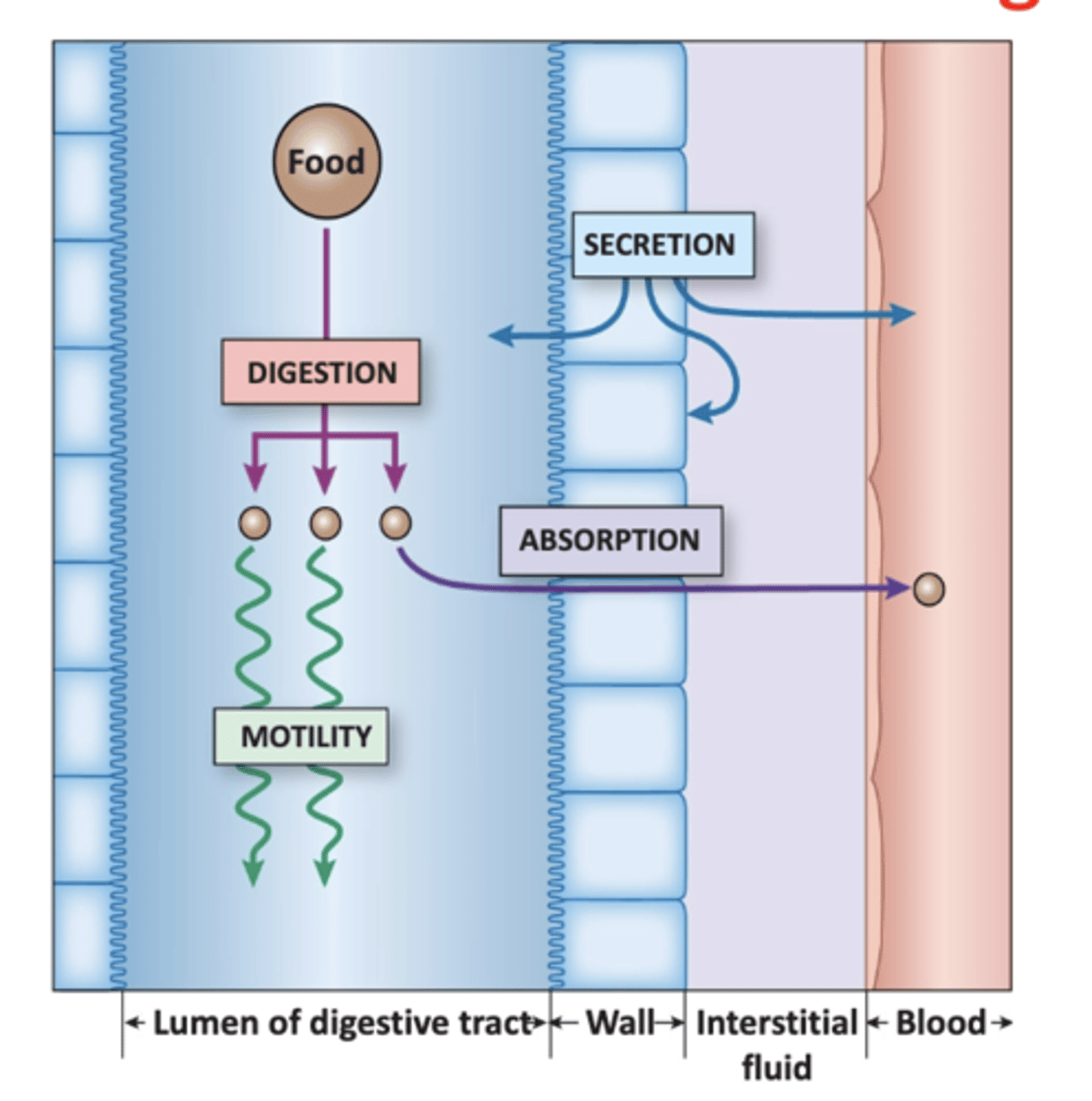
Digestion Overview in SI/Blood
Small intestine in blue on left. Blood vessel closely associated with SI in red. Epithelial cells blocks (food goes from SI → blood). Chemical breakage in SI. Smaller units absorbed cross intestinal epithelial cells → bloodstream. Absorptive state - first food molecule is absorbed across intestinal epithelial → blood to the time last food molecule is absorbed.
What macromolecules can be stored?
Glucose (glycogen + triglycerides) and Fats (triglycerides)
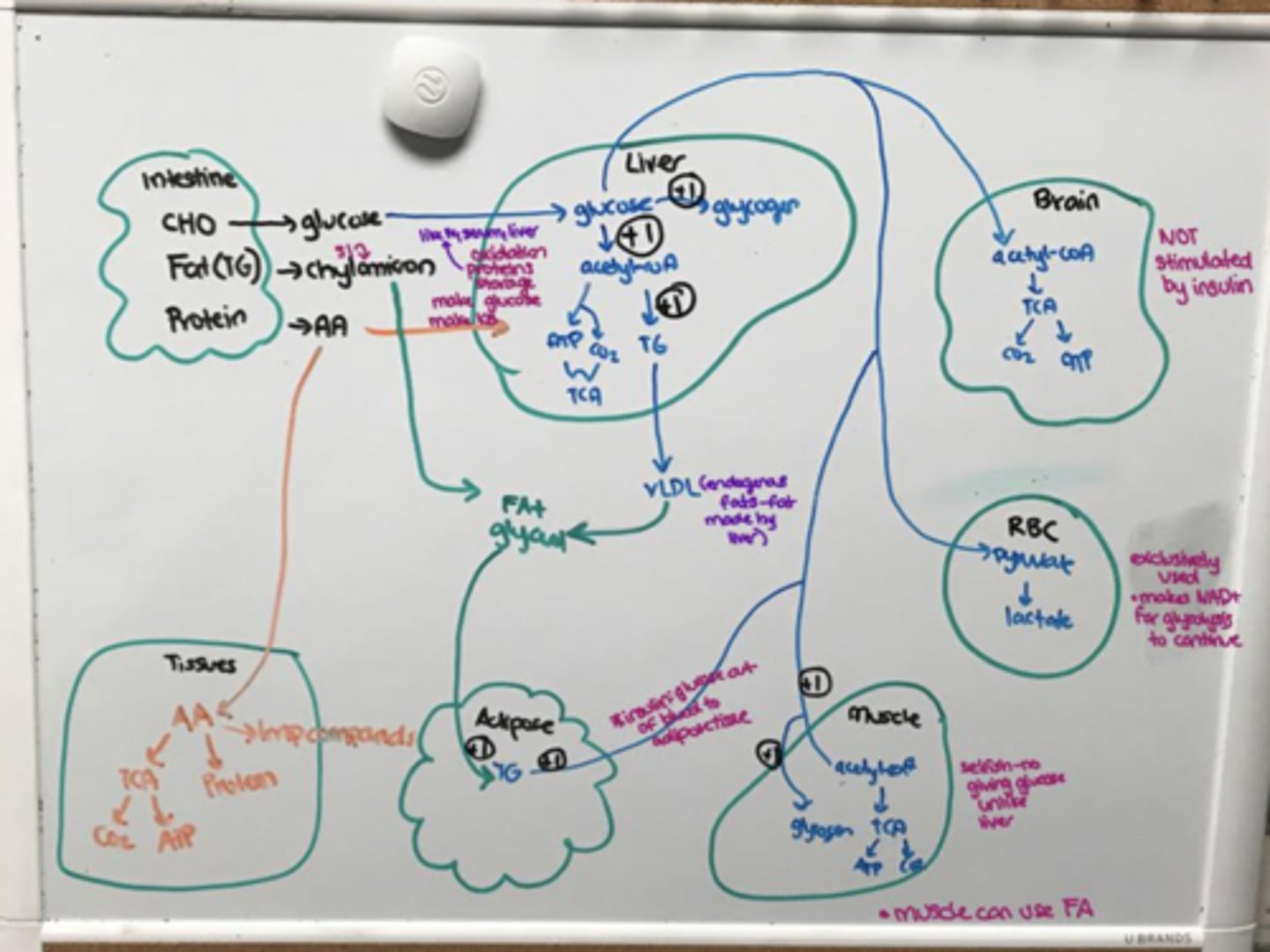
Fed State Draw Diagram
Lipoproteins
triglycerides and chylomicrons (transport lipids in blood)
Lipoproteins made where? Why do we have them?
Liver (VLDL) and intestine (chylomicrons)
outer surface hydrophilic (contact aqueous serum) and inner hydrophobic
LDL/HDL major consitutes
cholesterol
Insulin promotes ___ oxidation, ______synthesis, _____synthesis, and ______ synthesis
glucose, glycogen, fat, protein
Anthropometrics
what is it? normal range? what happens when it falls below 70 but below 40.
Thermometer with blood glucose. 70-100 normal range. Hypoglycemic is below where you start to feel cranky, feel hungry, shake, sweaty, confused, slower in thinking.
Glucagon and epinephrine bring up glucose. Cortisol supplied to get glucose in blood.
Anthropometrics
Very below 40
Anything below this is tumor in pancreas, inability to bring food in body, permanent brain damage/death.
Anthropometrics
till what level do we not go to?
Good news: normal healthy individual without pathology never get into that range. Body can stay in normal glycemic range. Even fasting, we still stay in that range as liver is at work.
Anthropometrics
below 40?
Rarely below 40 due to liver. If so, lethargy, convulsions, and coma result - not enough to maintain conciousness.
Anthropometrics used to measure what? What happens when you exceed daily caloric needs?
Ways to use basic measurements to get indication of nutritional status/growth. BMI, skinfold thickness, mid-upper arm muscle, and waist circumference (look for abdominal obesity).
When food intake exceeds daily caloric needs, the body stores this fuel as fat and glycogen.
Chronic Excess Food Consumption Disorders (describe/genetic or environmental)
Hypercholesterolemia
Hyperglycemia
Hyperlipidemia
All associated with what?
elevated cholesterol caused by mutation in a specific protein or excessive cholesterol intake.
high blood glucose levels caused by either mutations in specific proteins or tissue resistance to insulin.
High blood lipids caused by mutations in specific proteins or ingestion of high-fat diets.
Associated with CVD - increase cancer, problems in gallbladder.
Ivan A: fasting blood glucose elevated, high cholesterol (Elevated triglycerides (hyperlipidemia),
Positive steps to decrease BP, heart rate, and stroke. Dietary recommendation - limit carbs, fat, and salt
Post-absorptive states
Absorptive - molecules being actively absorbed vs postabsorptive. 2 hours for glucose to go back to normal glycemic range. Peaks after hour of eating. Things coming down.
Basal state (brief fast) in overnight fast vs prolonged fasting (3 days fasting starved state)
Mobilize any fuel means glucose coming from liver AND FA coming from adipose. Low insulin secretion.
Fact: mobilizing fuel is a concerted effort (both at same time).
Fasting starts when mobilizing fuel: brief → prolonged fast transition. Two ways to define this: at the 3 day mark. Functionally, we know prolonged fast started when brain using ketones.