Module 3 & 4 : Immunology and Hematology
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
What’s our first line of defense?
It is our physical and biochemical barrier: skin, mucous, cilia, etc.
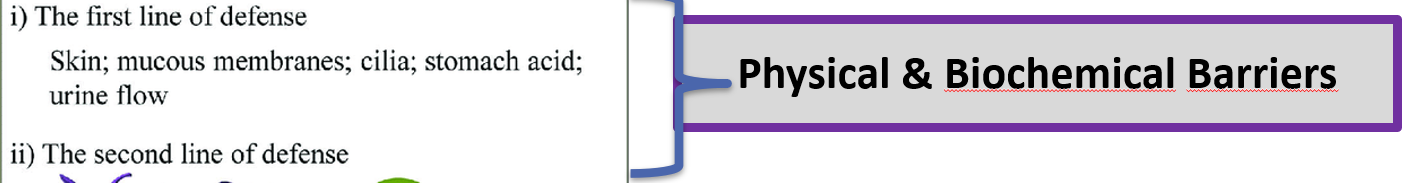
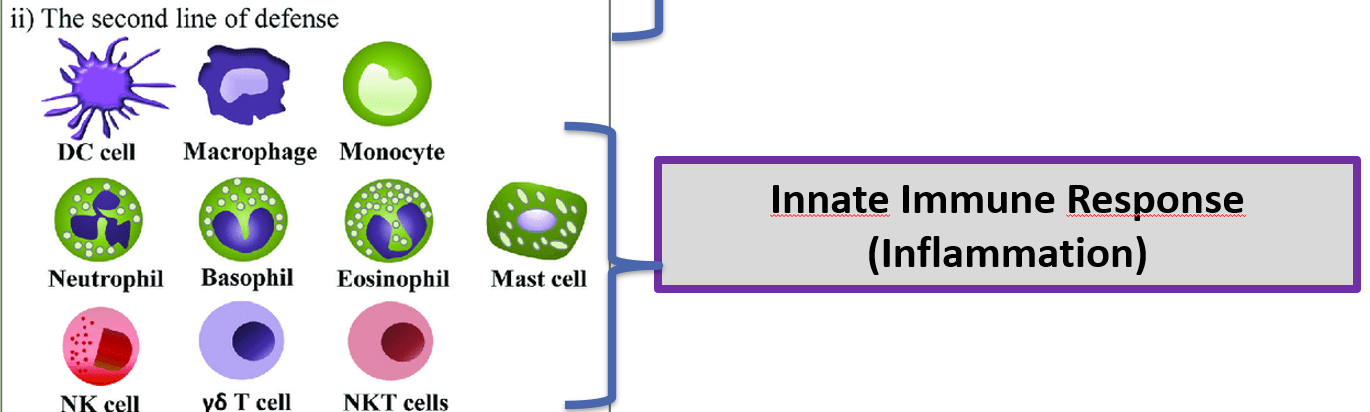
What’s called our second line of defense ?
Innate Immune Responses.
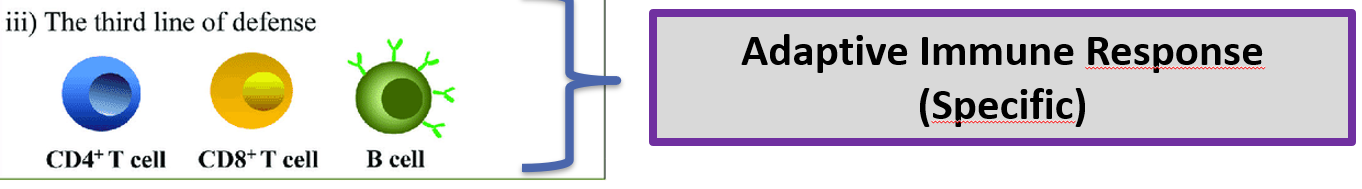
What’s called our third line of defence?
Adaptive Immune Response
What’s a microbiome?
Bacteria and fungi that colonize every surface of our body including internally when they have access from an outside point (ex. gastrointestinal, lungs, etc.). Microbiome is very beneficial in maintaining health and supporting/training the immune system as well as producing enzymes to help us digest .

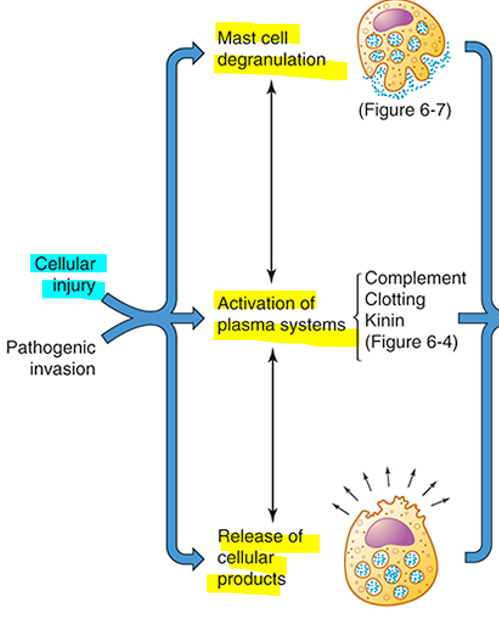
What are the 3 main events occuring after cellular injury?
Mass cell degranulation, activation of plasma systems and release of cellular product.
What impact does inflammation hve systemicaly?
Cause fever due to pyrogens secretion (IL-1)
Increase in white blood cell count
Blood clothing promoting factor (Il-6, fibrinogen, CRP)
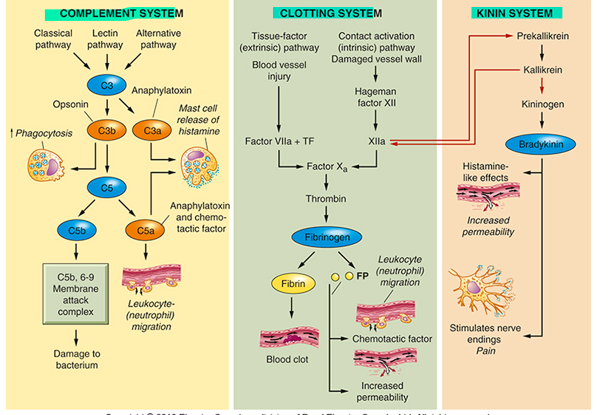
From which organ are the Complement system, the Clotting system and Kinin synthesized from ?
The liver, so if it is impaired, these systems may not function properly.
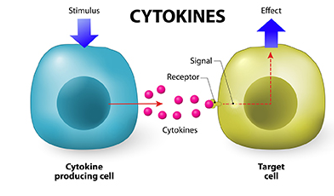
What are cytokine?
Small molecule that each has a specefic role in communicating information to trigger a reaction. They are involved in cell signaling and immune response.
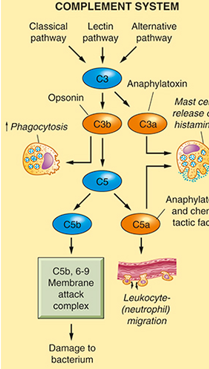
What is the role of the Complement System?
Make the immune system more optimum by :
Creating vasodilatation and recruiting more immune cell to the impacted tissue ( Anaphylatoxin)
Opsonin promote cell to phagocyte by giving them a better grip
The membrane attack complex form pore that tarket bacteria to destroyed their membrane.
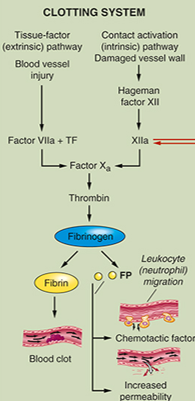
What is the role of the Clotting System?
Important for wound healing by preventing bleeding and promoting clotting factors.
What is the role of the Kinin System?
Activate inflammatory cells and contribute to vasodilation as well as increasing vascular permeability during the inflammatory response. In addition, it plays a role in pain sensation and smooth muscle contraction.

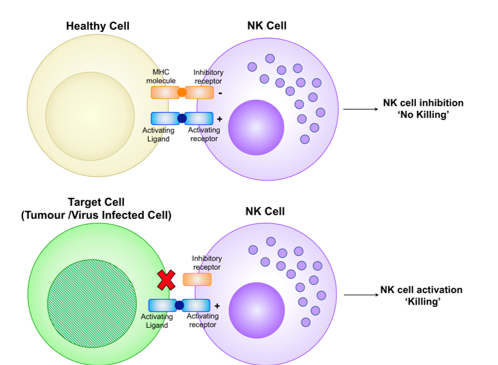
How does the natural killer cell induce killing?
By analysing if a cell has the MHC-1 protein on their surface. If a cell lacks MHC-1, the natural killer cell indentify it as infected (since virus inhibit it to be expose) and then promote apoptosis of the cell.
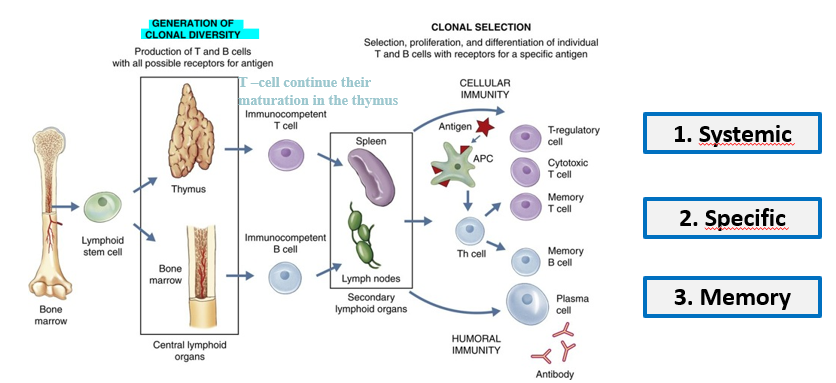
What are the three main characteristics of the adaptive immunity?
It is specefic, Systemic and has a MEMORY!!!
Wich immunoglobolin protect the mother and the fœtus?
IgG

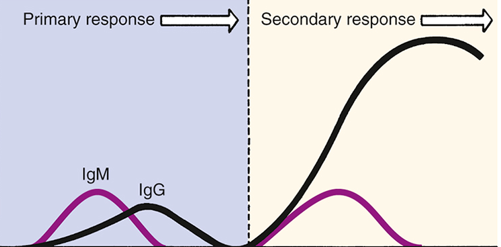
How do vaccines work?
Vaccines stimulate the immune system to recognize and fight specific pathogens by introducing an antigen that mimics the disease-causing organism. It will cause an smalll increase in IgM and IgG after activating 2 signal. Then, if the individual get infected in the futur, the body will only need1 signal to activate this immuntity and the reaction will be much more faster and optimum.

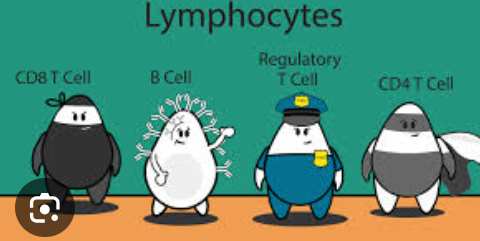
Explain the pathway of Humoral response.
The bacteria get phagocytose = digests it = present protein on their membrane has class two MHC2 = travel in the lymph nodes = show the antigen to the T-Helper cell (first signal) = which will create antigen (differentiated and multiply) = The T-cell search for the B-cell= has to activate the b-cell (second-signal) = secrete antibodies and be memory cells
In central tolerance test for immune cell, what is the possitive and negative selection?
Positive : look at cells that react to a pathogen and keep them. Kill theone that does not react.
Negative : look at cell that overeact to a pathogen and killed those immature T-cell.
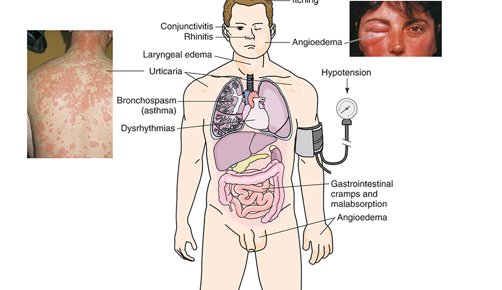
What differentiated the type 1 hypersensitive reaction over the other?
It is mediated by IgE
Mast cell overreaction are the main trigger
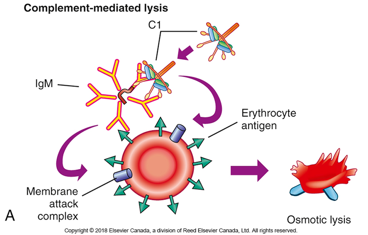
What differentiated the type 2 hypersensitive reaction over the other?
It is tissu specefic.
Antibodies are binding to tissue specefic protein.
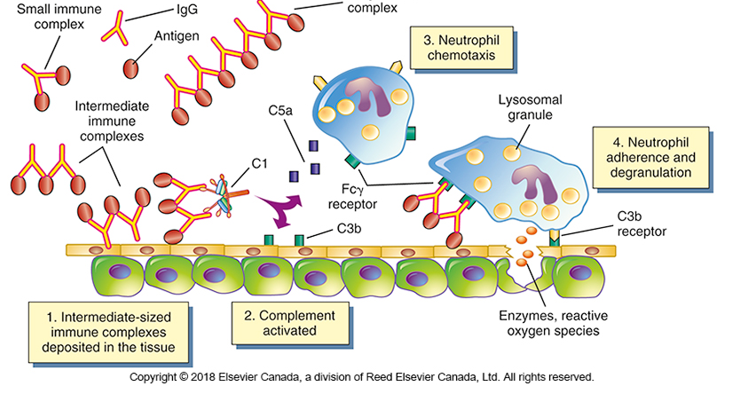
What differentiated the type 3 hypersensivity reaction over the other?
It involves immune complex formation (antibody clumbs toguetter) that deposits in tissues, leading to inflammation and damage. Neutrophile increase this immune reaction with his chemotaxis and degranulation.
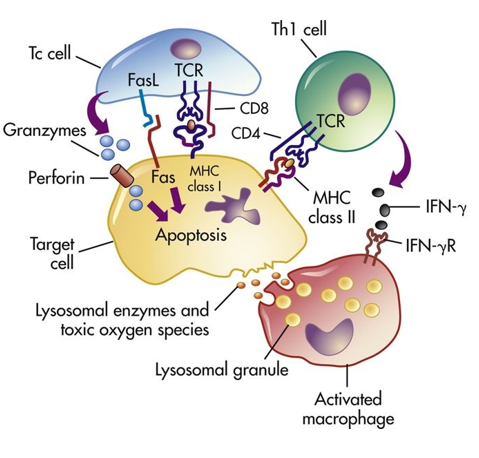
What differentiated the type 4 hypersensity reaction over the other?
It is a delay hypersensitive reaction
Only T-cell are involve
Explain how hypoxia leads the the stimulation of erythropoiesis
The hypoxia indices factor (HIF) detects drops in blood oxygen levels, which triggers the production of erythropoietin
Explain in what way the body would compensate in the context of low iron, and in the context of high iron
When the iron levels are low, the body will compensate by activation hepcidin, which promotes dietary absorbing of iron.
When they are high, the hepcidin will promote the storage of iron into ferritin in the liver or in the spleen, which can then be used in the synthesis of new erythrocytes
Explain how deficiency in intrinsic factor can lead to anemia, name the type of anemia associated with this cause.
Intrinsic factor is necessary to absorb Vitamin B12, therefore, if it is deficient, there will be less B12, which is necessary for the formation of eruythrocytes. This is pernicious anemia.
Explain the RBC characteristics and explain the rational behind iron deficiency
In iron deficiency, RBCs are hypochromic, meaning they are pale in color due to decreased interactions between oxygen and iron, which gives it their usual bright red aspect. They are also microcytic, meaning smaller, due to impaired hemoglobin synthesis.
In what type of anemia may an increased amount of reticulocytes be present, and why?
Reticulocytes are the precursors of RBCs. In hemolytic anemia, there is a premature destruction of RBC, so they are not able to form completely, which is why there is an increased count of their precursor molecule.
Explain how the immune response in infectious mononucleosis leads to the unwanted proliferation of the virus
Infectious mononucleosis is caused by the Epstein-Barr virus (EBV), which affects B-cells. Therefore, the immune response triggers a proliferation of those B-cells, leading to activation and proliferation of the virus.
Explain how leukemia leads to a decreased production of normal hematopoietic cells.
In leukemia, there is uncontrolled proliferation of malignant leukocytes, which leads to an overcrowding of the bone marrow, which is unable to keep up with the production of normal, healthy hematopoietic cells.
Explain how disseminates intravascular coagulation (DIC) could lead to a hemorrhage
In DIC, the increased activation of platelets leads to an increased consumption of coagulation factors, resulting in a decreased availability of these factors when they are actually necessary. This increases the risk of a hemorrhage if there is a bleed/lesion when a large percentage of coagulation factos are used up.
Explain how each element of the Virchow’s Triad increase the risks of a thromboembolic event.
Injury to the blood vessel endothelium: cell injury sends pro-inflammatory signals, which activates the coagulation cascade and leads to the formation of thrombus
Abnormalities of blood flow: turbulent or stagnant blood flow promotes clotting because it allows for clotting factors to accumulate, leading to thrombus formation
Hypercoagulability of the blood: if there is increased presence of clotting factors in the blood, there is an increased chance of thrombus activation and formation