Ch 37: Renal Function & Micturition
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
40 Terms
What are podoytes?
food processes that surround capillaries and form filtration slits.
What cells control the width of the podocyte slits? how do they do this?
Mesangial cells contain actin and myosin fibers, and control the width of podocytes by contracting or relaxing.
contraction decreases surface area, reduces filtration.
relaxation increases surface area and filtration.
What are some factors that constrict mesangial cells?
angiotensin II
Vasopressin (ADH)
NE
Histamine
What are some factors that relax mesangial cells?
ANP
Dopamine
PGE2
cAMP
What is the normal GFR?
125 mL/min (180 L/ day)
What is the standard glomerular hydrostatic pressure?
60 mmHg
What is the standard net filtration pressure in the glomerulus?
10 mm Hg
What is Kf?
This is the glomerular capillary filtration coefficient. It tends to remain unchanged (12.5mL/min)
The Kf of glomerular cells is generally invariable, but what conditions may cause a decrease in Kf and subsequent decrease in GFR?
chronic hypertension (high pressure damages tissues)
obesity/ diabetes mellitus (high glucose damages kidneys)
glomerulonephritis (infection)
What are the two mathematical determinants of renal blood flow?
delta-P (the difference between entering renal pressure and leaving renal pressure.
R (the total renal vascular resistance, sum of arterial, pelvis, and vascular resistance)
What effect does sympathetic activity have on GFR and RBF, why?
sympathetic activity results in an overall decrease in renal blood flow and glomerular filtration rate due to an overall decrease in blood going to the kidneys.
What blood vessels bring blood into the glomerulus?
afferent arterioles
What blood vessels remove blood from the glomerulus?
efferent arterioles
What MABP (mean atrial BP) range allows the renal system to maintain a stable GFR?
80-180 mmHg
What is the myogenic mechanism?
reflex contraction of afferent arterioles when blood pressure rises (reduces incoming blood)
What is the tuboglomerular feedback mechanism?
paracrine substances from DCT may cause smooth muscle contraction.
A patient has a kidney stone partially blocking the ureter of one kidney. Based on your knowledge of renal physiology, which of the following statements is correct?
A. the patient will have problems with salt and water balance due to a loss of 50% renal function
B. GFR in the affected kidney will decrease
C. Urinary flow will be reduced by approximately 50%
D. Hydrostatic pressure in the tubules will be decreased
E. renal failure will occur.
The correct answer is B. The blockage of urine leaving the kidney will result in an increase in Bowmans capsule pressure.
This resistance on glomerular hydrostatic pressure will reduce the overall filtration rate.
What is the pathway of myogenic autoregulation?
An increase in arterial pressure results in an increase in GFR and Blood flow.
However, increase in pressure also results in an increase in blood vessel stretching. This stretching increases calcium entry into the cells, which increases vascular resistance.
Increase in vascular resistance leads to decreased blood flow and GFR
This loop operates to regulate GFR and Blood Flow
How does modification of efferent arteriolar resistance happen via the tubuloglomerular feedback system? (5 points, long answer)
A decrease in arterial pressure results in a decrease in glomerular hydrostatic pressure, whicih results in a decrease in GFR.
Decreased GFR = less Na reabsorbed, which is detected by macula densa cells.
In response, macula densa cells increase renin secretion, which activates the renin-angiotensin II pathway.
Angiotensin II ultimately increases efferent arteriole resistance, thus decreasing the amount of fluid leaving the glomerulus (increasing pressure)
this increase in pressure ultimately increases glomerular hydrostatic pressure, thus increasing GFR.
How does modification of afferent arteriolar resistance happen via the tubuloglomerular feedback system?
The mechanism is similar to the efferent tubules. However, the decrease in macula densa NaCl results in a decrease in afferent arteriolar resistance, which increases renal blood flow.
This increases glomerular hydrostatic pressure and GFR
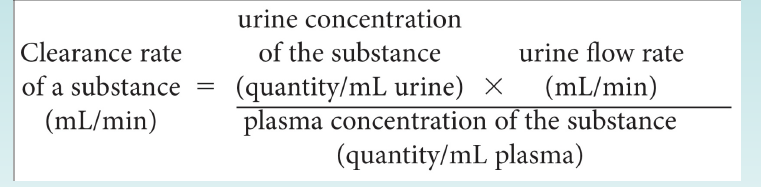
What is the formula for Kidney Clearance Rate in mL/min?
Pay attention to the units!
If a substance is filtered, but not reabsorbed or secreted, what would the relationship be between its plasma clearance rate and the GFR?
Substances that are exclusively excreted through the urine will have a plasma clearance rate equal to the GFR
If a substance is filtered and reabsorbed, but not secreted, what is the relationship between its plasma clearance and the GFR.
Substances that are almost completely reabsorbed will have a clearance rate lower than the GFR.
If a substance is filtered and partially reabsorbed, but not secreted, what will its clerance rate be in relation to the GFR?
Substances that are partially reabsorbed, will always have a clearance rate less than the GFR.
If a substance is filtered and secreted, but not reabsorbed, what is the relationship between its clearance rate and the GFR?
Substances that are filtered and secreted but not reabsorbed, such as hydrogen ions, will be mostly excreted in the urine and their clearance rate will always be greater than the GFR.
How does inulin allow determination of GFR?
Inulin is not reabsorbed, and is completely excreted through the urine. As a result, clearance rates of inulin allow for determination of GFR.
What does plasma clearance of PAH (para-amino hippuric acid) allow us to determine.
This substance is completely secreted so that the blood flowing through the kidney is completely free of it. As such, its clearance rate estimates renal blood flow.
How is glucose reabsorbed from the lumen into tubular cells?
Via sodium-glucose cotransporters SGLT transporters
What is the countercurrent multiplier?
As you descend the loop of Henle, the osmolarity of the tube contents increases. Likewise, ascending the loop decreases osmolarity.
What is a transport maximum?
The maximum amount of a substance that can be transported by the kidneys. This is defined for every nephron in both kidneys.
further increases in tubular load will not be reabsorbed and are excreted.
What is threshold?
the tubular load at which transport maximum is exceeded in some nephrons.
some nephrons have lower transport maximums than others, so some nephrons may still be able to continue filtering a solute.
What is the threshold for glucose? What does it mean for this level to be reached?
Threshold for glucose is 200mg/dL. At this point, some nephrons will reach their capacity for glucose and stop reabsorbing it.
What is the transport maximum for glucose? What does it mean for this level to be reached?
At approximately 350mg/dL all nephrons will stop reabsorbing glucose and it will be excreted in the urine.
What is the function of aldosterone?
This hormone increases Na channels to reabsorb more sodium and secrete more potassium. (increased Na in interstitial fluid)
What is the function of ANP?
This hormone is produced in the heart and decreases sodium channel activity, prevents reabsorption of sodium (increased excretion)
acts by increased cGMP levels which in turn inhibit sodium channels.
What is amiloride? How does it work?
Amiloride is a “potassium sparing” diuretic. It exclusively acts by restricting sodium channel activity, thus increases Na concentration in the lumen, which in turn increases water secretion and urine volume.
may result in hyperkalemia as sodium is needed to excrete potassium.
What is the role of S2-4 in the micturition reflex?
The parasympathetic innervation of S2-S4 act as motor neurons for the constriction of the detrusor muscle and relaxation of the internal urethral sphincter
stimulation promotes urination
What is the role of the sympathetic nervous system L1-L3 in the micturition reflex?
These neurons act as motor neurons to the internal urethral sphincter and inhibitory to the detrusor.
this stimulation prevents urination. increase tone of internal sphincter and inhibit contraction of the detrusor.
What do the pudendal nerves do in the micturition reflex?
These nerves, S2-S4, carry somatic fibers to control the external urethral sphincter.
Which sect of the motor nervous system is most important for micturition?
The parasympathetic nervous system is the most important for urination.
the sympathetic system has no significant role, mostly prevalent in ejaculation.