Quiz 5: Biomedical Sciences
1/97
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
What is the key function of the kidney?
Homeostasis — it maintains internal constancy of electrolytes, water, acid-base status, and blood components
What are the nine major functions of the kidney?
Glomerular filtration
Water homeostasis
Sodium homeostasis
Potassium regulation
Calcium/vitamin D regulation
Acid-base balance
Blood pressure control
RBC production (erythropoietin)
Gluconeogenesis
What happens if homeostasis fails for: Glomerular Filtration?
↓ GFR → loss of filtration
What happens if homeostasis fails for: Water Homeostasis?
Water imbalance → Δ serum Na⁺
What happens if homeostasis fails for: Na+ Homeostasis?
Na+ imbalance → edema or congestion (e.g., heart failure)
What happens if homeostasis fails for: K+ Regulation?
K+ imbalance → arrhythmia, paralysis
What happens if homeostasis fails for: Ca2+/vitamin D Regulation?
Ca2+/Vit D imbalance → ↑ PTH, osteoporosis
What happens if homeostasis fails for: Acid-Base Balance?
Acid-base imbalance → pH changes
What happens if homeostasis fails for: Blood Pressure Control?
change in blood pressure (increase or decrease)
What happens if homeostasis fails for: RBC Production?
RBC production failure → anemia
What happens if homeostasis fails for: Gluconeogenesis?
Gluconeogenesis loss → hypoglycemia
What are the two major structural components of the nephron?
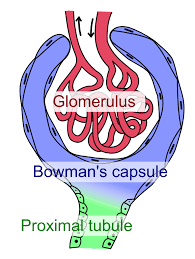
Glomerulus and Tubule
Glomerulus
tuft of coiled capillaries that filters plasma.
allows some substances to pass from the blood into the renal tubules.
Tubule
reabsorbs, secretes, and metabolizes solutes to maintain homeostasis
How many glomeruli exist per kidney, and what follows each?
~1 million glomeruli per kidney; each connects to its own tubule
Which part of the nephron is considered the "workhorse"?
The tubules, since they reabsorb and secrete solutes to maintain balance
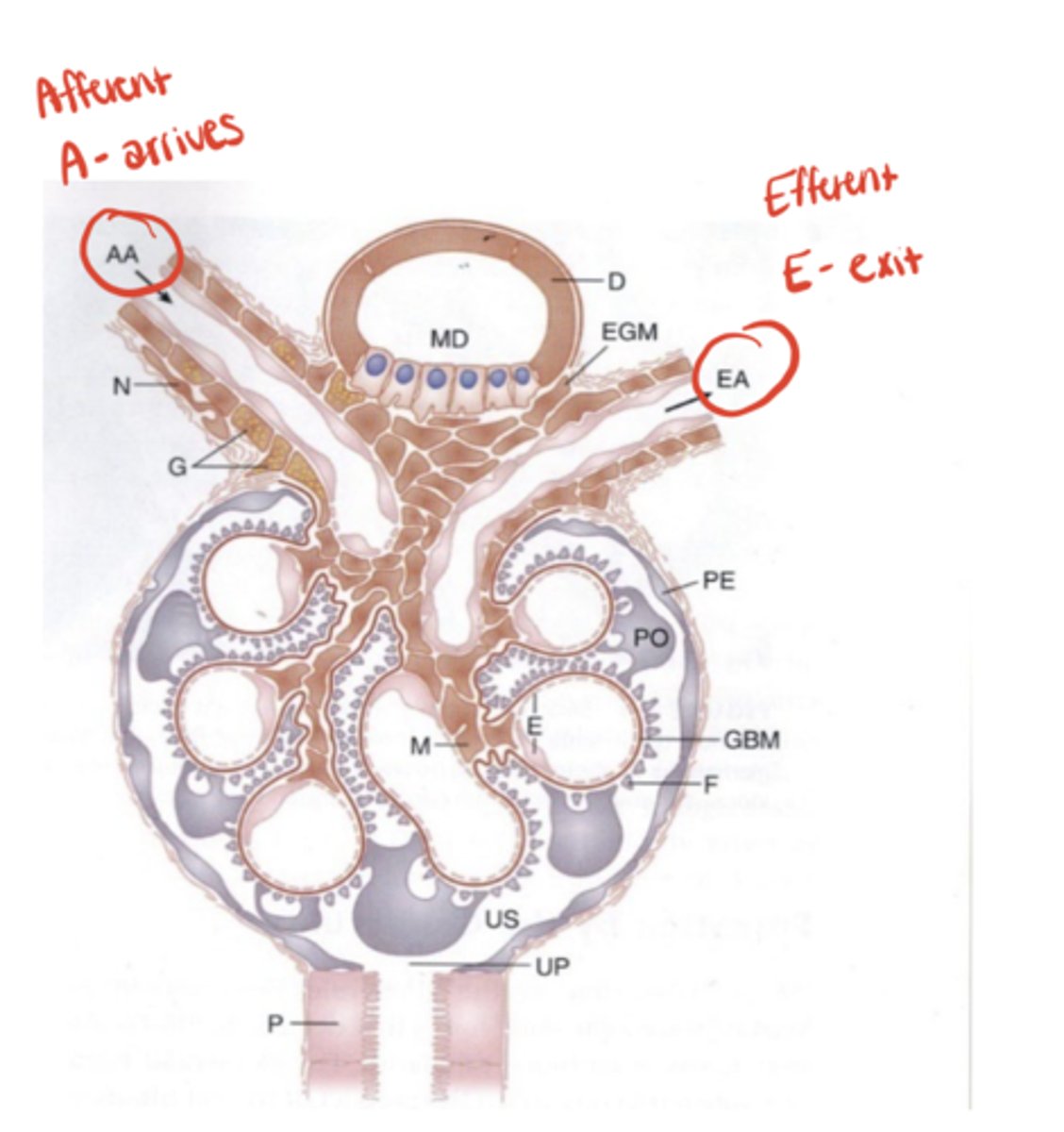
What makes glomerular circulation unique?
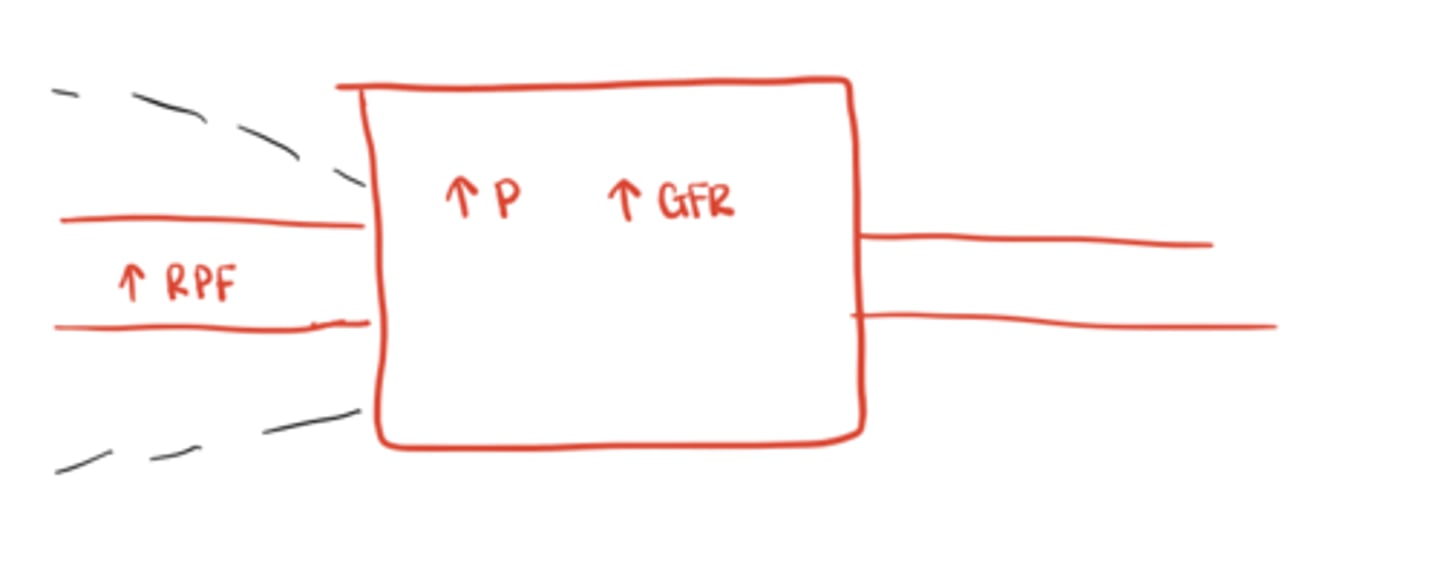
It’s arranged in series between two resistance vessels — the afferent and efferent arterioles
What percent of cardiac output goes to the kidneys?
~20%
- roughly 1 L/min of blood flow
What is the renal plasma flow (RPF)?
About 600 mL/min (since ~40% of blood is RBCs, 60% is plasma)
Afferent Arteriole
arrives to glomerulus
Efferent Arteriole
exits the glomerulus
What is Bowman's space?
The urinary space surrounding the glomerulus where filtered plasma collects
What are the three layers of the glomerular filtration barrier?
1. Capillary endothelium
2. Basement membrane
3. Podocyte foot processes with slit pores
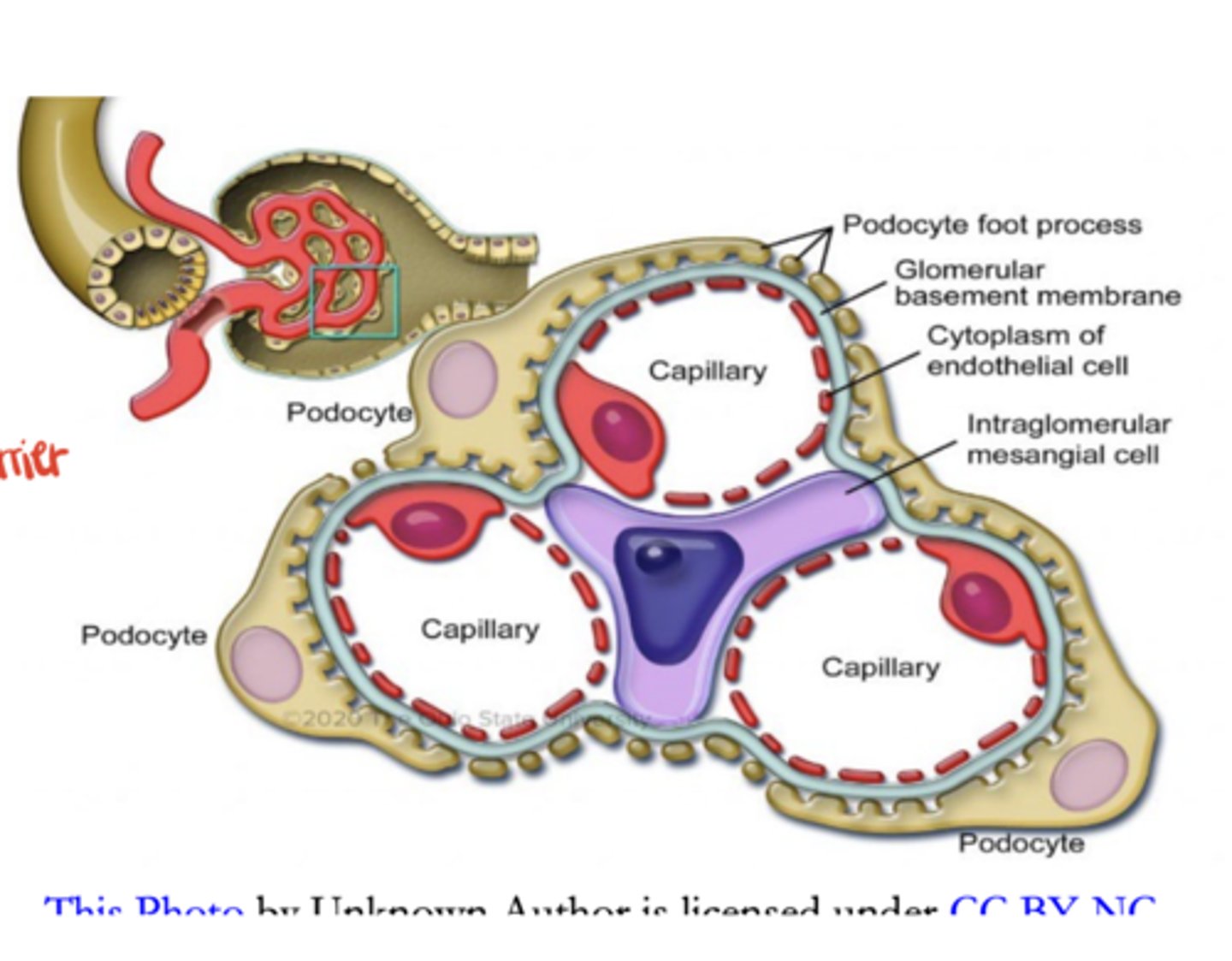
What two factors determine whether a molecule is filtered?
Size and charge, with size being the primary determinant
Which plasma components are freely filtered?
Molecules < 7,000 Da
Which components are excluded from filtration?
Molecules > 65,000 Da (ex. albumin)
What happens to a drug bound to albumin?
It cannot be filtered, though some may still enter urine via tubular secretion
Why is maintaining GFR critical?
Because GFR determines the kidney's ability to maintain homeostasis and drug clearance
What is the relationship between glomerular pressure and GFR?
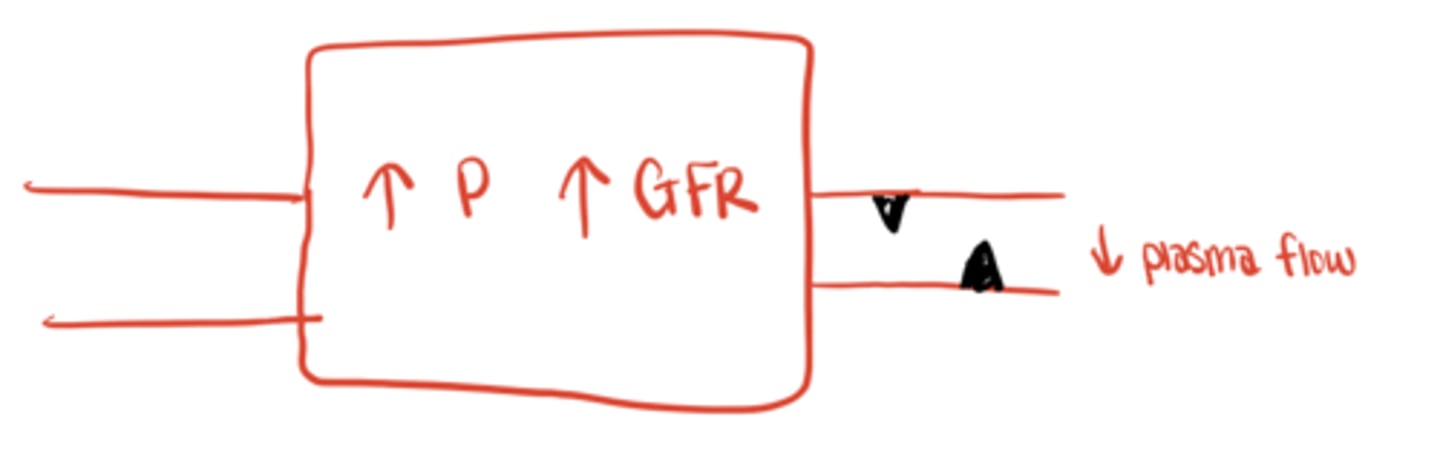
↑ Pressure → ↑ GFR; ↓ Pressure → ↓ GFR
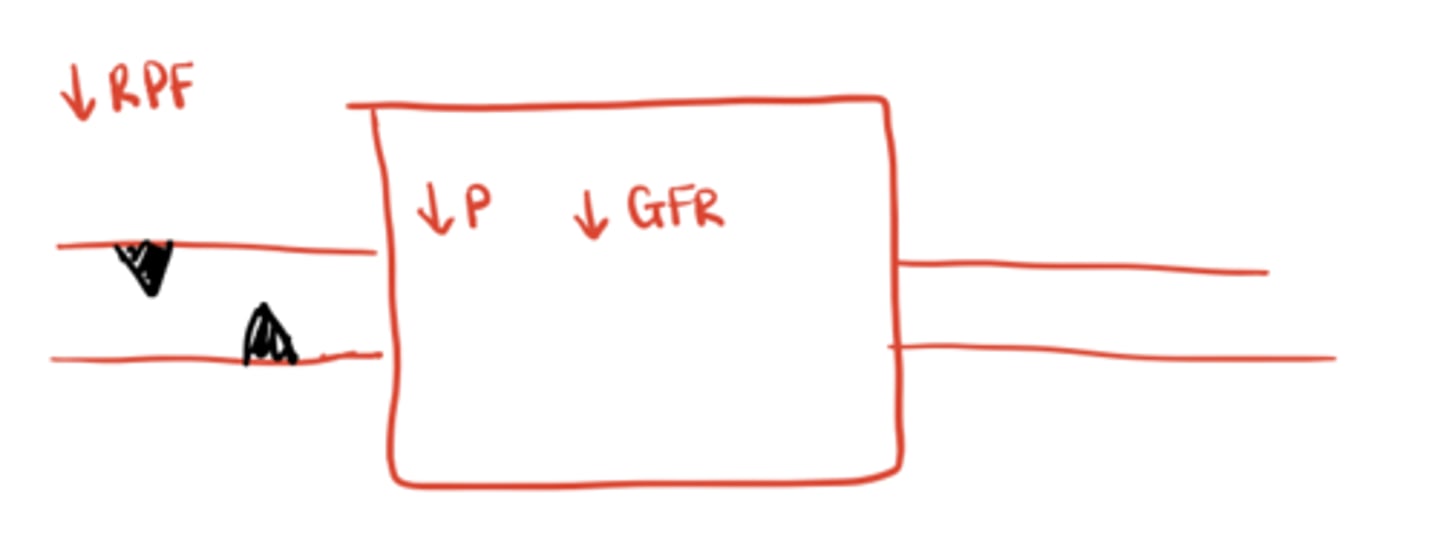
What happens if the afferent arteriole constricts?
↓ Renal plasma flow → ↓ glomerular pressure → ↓ GFR
What happens if the afferent arteriole dilates?
↑ Blood flow and pressure in glomerulus → ↑ GFR
What happens if the efferent arteriole constricts?
Blood exits more slowly → ↑ glomerular pressure → ↑ GFR
Which mediators regulate these vessels?
Angiotensin II: constricts both, but mainly the efferent.
Norepinephrine: constricts both (reduces flow).
Prostaglandins: dilate the afferent arteriole
What happens if a patient takes NSAIDs?
NSAIDs inhibit prostaglandins → afferent constriction → ↓ renal plasma flow and GFR
What happens if a patient takes ACE inhibitors or ARBs?
They block angiotensin II → efferent dilation → ↓ glomerular pressure → ↓ GFR
What is the consequence of taking both an ACE/ARB and an NSAID during volume depletion (e.g., GI bleed)?
Severe drop in GFR → acute kidney injury (AKI)
What is clearance?
The volume of plasma completely cleared of a substance per unit time (volume/time)
Clinically, what is creatinine clearance assumed to equal?
GFR (though it slightly overestimates true GFR because creatinine is also secreted)
What is the unit of creatinine clearance?
mL/min volume/time
What is filtered load?
The total amount of a solute filtered from plasma into the glomerulus:
Filtered Load= (Free Plasma Concentration) x (GFR)
ex. Na+ = 140 mEq/L × 180 L/day = ~25,000 mEq/day
What is the excretion rate?
The total amount of solute excreted in urine:
urine flow rate x [solute urine]
ex. Urine Na+ = 90 mEq/L; Urine flow = 2.5 L/day → 225 mEq/day
Does renal clearance care how a substance enters urine?
No, it includes both filtration and secretion
What is the equation for renal clearance?
Clearance x Plasma[x] = Volume Urine x Urine [x]
****Excretion Rate / Plasma concentration
Does clearance differentiate between secretion and filtration?
No, it measures total removal
When should measured creatinine clearance (CrCl) be used?
1. very high body mass (e.g., bodybuilders)
2. very low body mass (frail, elderly)
3. vegetarians
4. AKI
5. high-risk/toxic drugs requiring precise dosing
6. liver disease
How is CrCl calculated from a 24-hour urine?
CrCl= (Urine Volume x Urine Creatinine) / Plasma Creatinine
Osmolality
mmol solute / kg H₂O
Osmolarity
mmol / L H₂O
Can osmolality and osmolarity be used interchangeably?
yes because 1 kg ≈ 1 L
What is the formula to estimate serum osmolality?
2 x [Na+] + BUN/2.8 + Glucose/18
Serum osmolality is driven mainly by
Na+
How does water move between compartments?
Freely, to equalize osmolality between intracellular (ICF) and extracellular (ECF) spaces
What model is used for sodium disorders?
A two-compartment model: intracellular and extracellular spaces
What happens when extracellular osmolality increases?
Water leaves cells → cell shrinkage
What regulates serum osmolality?
Water balance (intake vs excretion) controlled by ADH + thirst
What is average water intake per day?
≈ 1-1.5 L from drinking + 0.35-0.5 L from metabolism
What is "fixed water loss"?
Unregulated losses ≈ 0.5 L/day via stool, sweat, and respiration
How does the kidney maintain water balance?
By varying urine output (1-1.5 L/day) under ADH control
What type of problem does altered serum Na⁺ concentration indicate?
Almost always a water problem, not primarily sodium
What two mechanisms regulate plasma osmolality?
ADH (vasopressin) and thirst
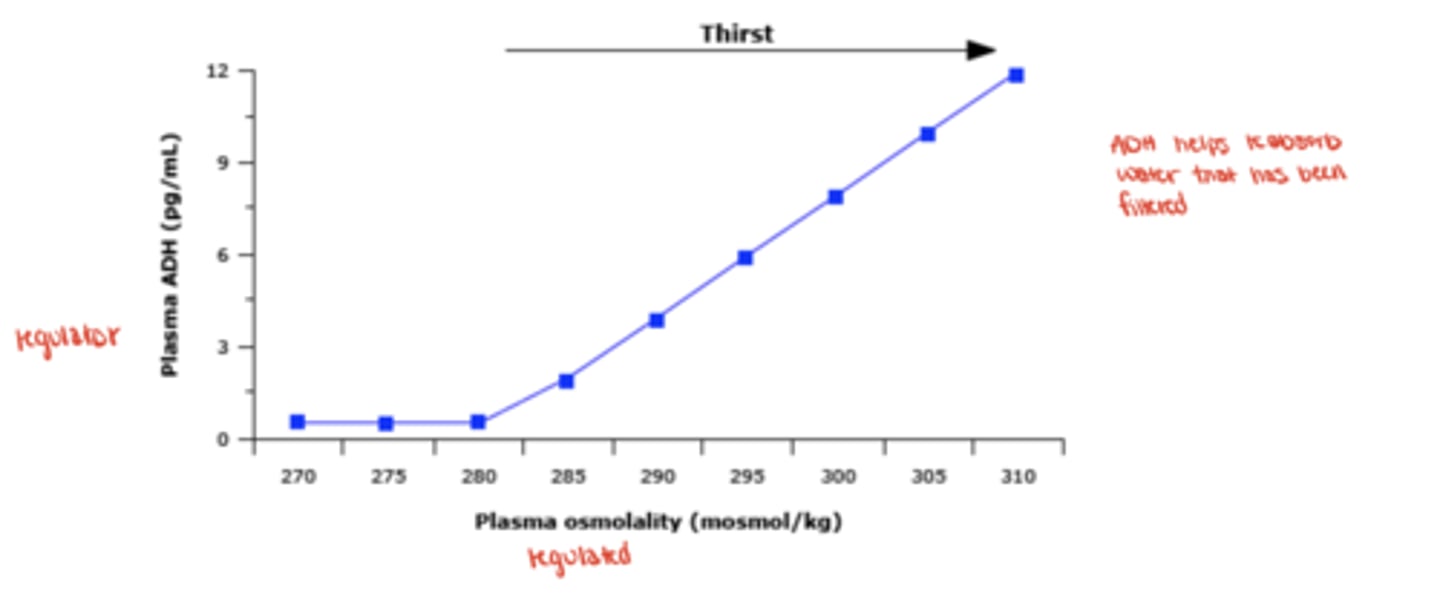
How sensitive are osmoreceptors to change?
1-2 % increase in osmolality → maximal ADH secretion
What non-osmotic factors stimulate ADH release?
↓ circulating volume (baroreceptors), nausea (strongest trigger), pain, and various drugs
What are common drug classes that increase ADH?
Narcotics, SSRIs, NSAIDs, PPIs, some chemotherapies, monoclonal antibodies
What pulmonary and malignant conditions increase ADH?
Pneumonia, TB, granulomatous disease, and cancers causing ectopic ADH
Are collecting-duct cells normally permeable to water?
No, they need ADH-activated aquaporin channels
Describe how ADH increases water reabsorption.
ADH binds V₂ receptors → aquaporin-2 channels insert in luminal membrane → water enters cell → blood
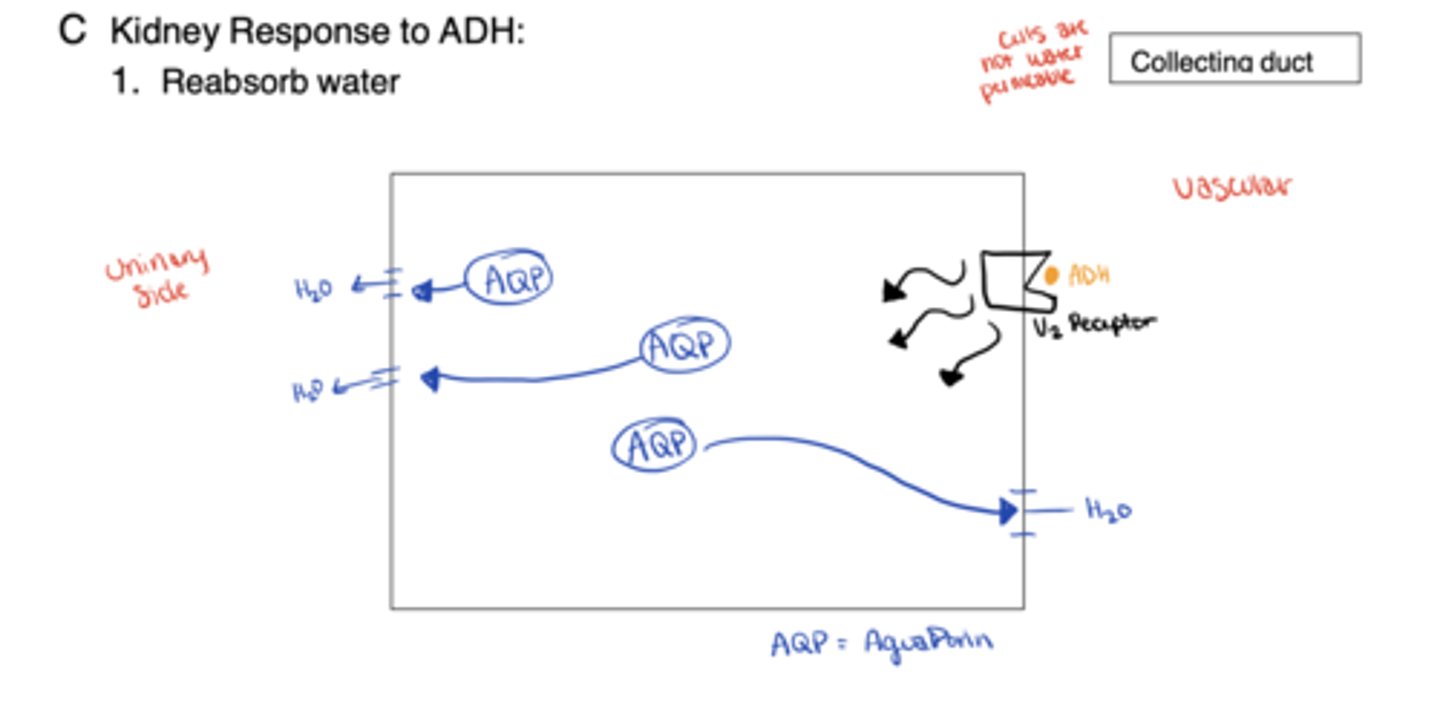
What disorders arise from problems with ADH, V₂ receptor, or aquaporins?
Diabetes insipidus (lack/response failure) or SIADH (excess activity)
What does hyponatremia indicate?
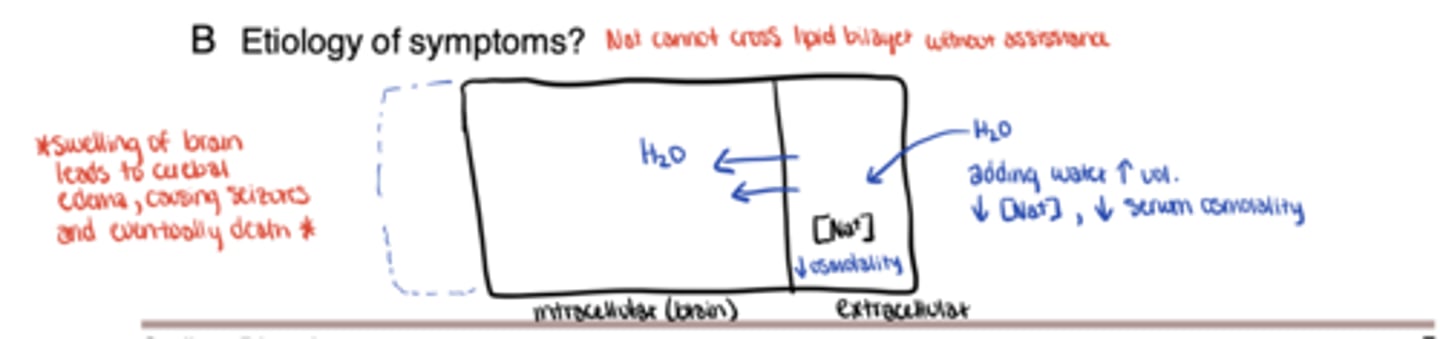
Positive water balance: too much water relative to Na⁺
What is the main clinical mechanism?
Water retention or intake exceeds excretion, lowering serum Na⁺ and osmolality
Which organ is most affected by low osmolality?
The brain → cerebral edema
What are symptoms of hyponatremia?
Fatigue, nausea, confusion, headache, seizures, coma; severe when Na⁺ < 115 mEq/L
Why do neurologic symptoms of hyponatremia occur?
Water shifts → cell swelling → ↑ intracranial pressure → brain edema
Case: In an elderly woman with seizures and Na 120 mEq/L, normal BP & no edema, what is likely volume status?
Euvolemic hyponatremia
What early information should be collected in such cases of euvolemic hypnatremia?
Full history, med review (esp. new SSRIs, PPIs, chemo), vitals, volume exam
How is volume status categorized in Na⁺ disorders?
Hypovolemic, euvolemic, or hypervolemic
What causes hypovolemic hyponatremia?
Loss of Na⁺ and H₂O via bleeding, vomiting, diarrhea, diuretics
Which diuretics most commonly cause Na⁺ loss?
Thiazides > loops (furosemide)
When is thiazide-induced hyponatremia most likely?
Within first 3 months or after dose increase, but may appear later
What is SIADH?
Syndrome of Inappropriate ADH — excess ADH without osmotic/volume need
What are typical causes of SIADH?
Drugs (SSRIs, narcotics, antipsychotics, COX-2 inhibitors) or nausea/pain
What are common lab findings in SIADH?
Urine osmolality > serum osmolality; urine Na > 40 mEq/L
Why should diuretics be stopped before urine studies?
they distort urine Na⁺/osm data → misclassification
What conditions cause hypervolemic hyponatremia?
Heart failure, cirrhosis with ascites, nephrotic syndrome
What does this hypervolemic hyponateremia indicate prognostically?
Poor outcome marker in advanced organ disease
What is hypernatremia?
Negative water balance: too little water for Na⁺
What are key symptoms of hypernatremia?
Thirst, lethargy, fatigue, weakness, seizures, coma, death
At what Na⁺ level do severe neurological signs usually appear?
> 160 mEq/L
What is the earliest and most specific symptom of hypernatremia?
Thirst (patient will ask for water)
What causes cellular dehydration in hypernatremia?
Water shifts from ICF → ECF to balance increased osmolality
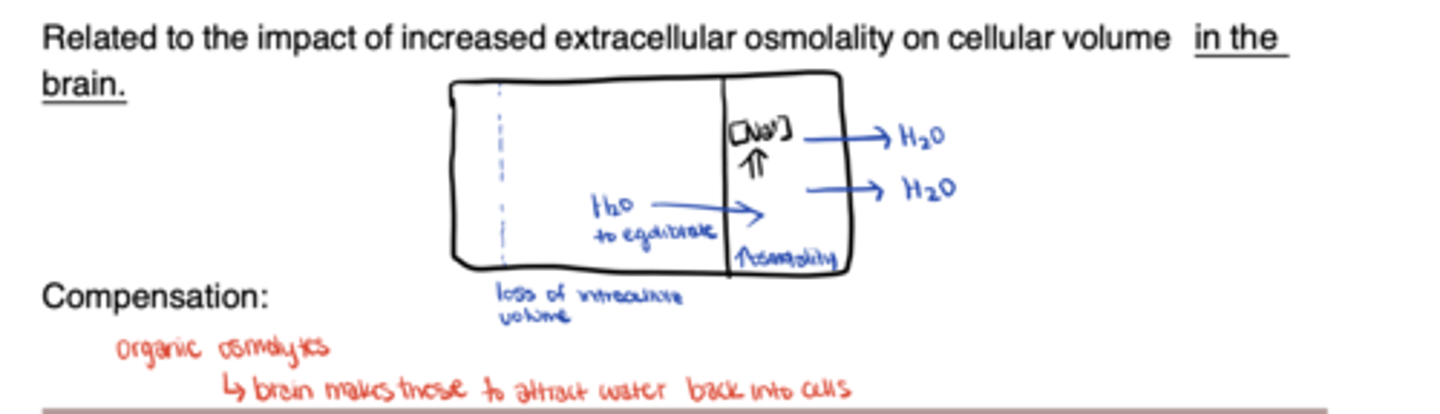
How does the brain partially adapt to hypernatremia?
Produces organic osmolytes to pull water back into cells
Why does brain adaptation affect correction?
Rapid correction → osmotic swelling → risk of cerebral edema
ALWAYS correct slowly
What are major causes of hypernatremia?
↓ intake (no access or impaired thirst) or ↑ loss (burns, fever, diarrhea, renal loss)
Who is at highest risk for intake deficits?
Elderly, disabled, or dependent patients in hospitals/care facilities
How does aging affect water regulation?
Thirst mechanism declines → reduced intake response
How can the kidney lose excess water?
Impaired ADH production/response → dilute urine
How can you tell if the kidney is failing to conserve water?
Urine osmolality < 100 mOsm/kg → lots of water in urine → renal water loss
Which drugs cause renal water loss?
V₂ antagonists (tolvaptan), lithium, ifosfamide, ofloxacin
What non-drug osmotic diuretics raise Na⁺?
Mannitol and excess glucose