Heart anatomy and blood circulation
1/37
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
38 Terms
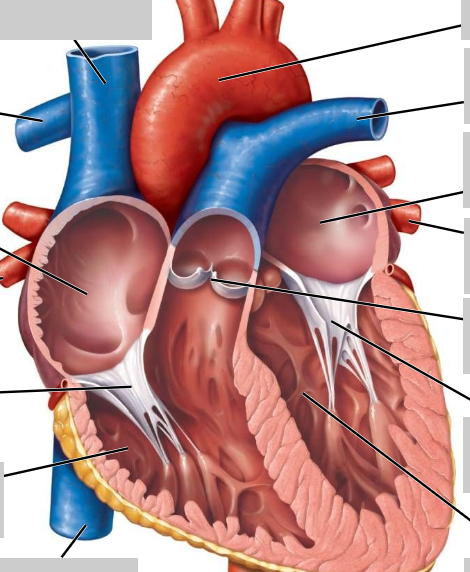
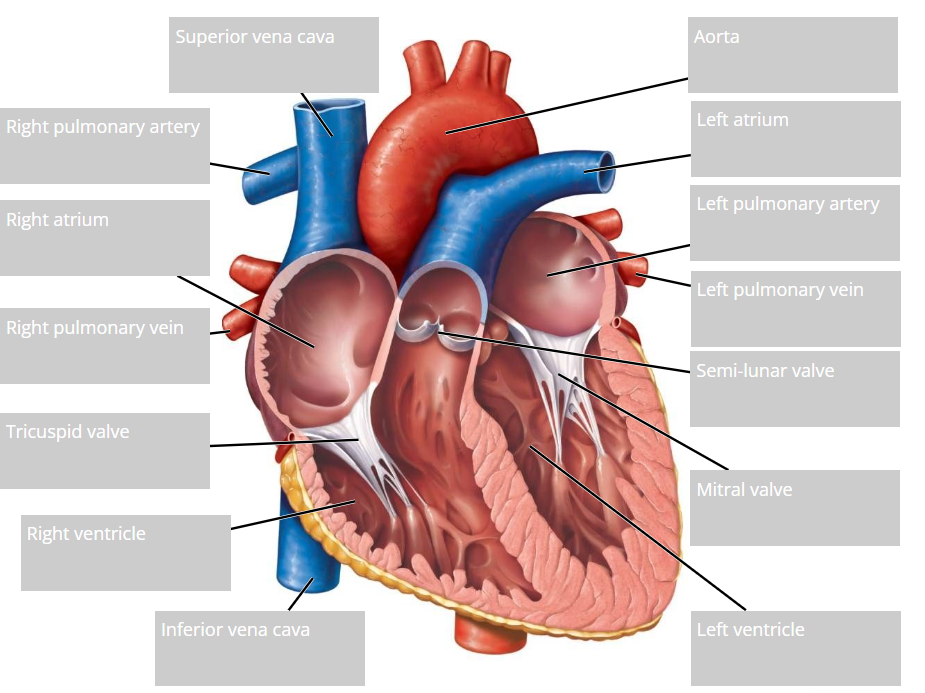
Label this heart
Does the apex of the heart sit on the left side or right side of the body's midline?
towards YOUR left
Which chamber of the heart has the thickest walls and why do you think this is necessary?
-The ventricles, specifically the left ventricle. This is because the ventricles have to pump blood to a further distance than the atria. The left ventricle, however, has to pump the blood to the rest of the body, whereas the right ventricle has to pump it to the lungs only. So, the left ventricle has thicker walls has it has to contract at a higher pressure.
What is the foramen ovale and where is it located? What would happen if it did not close at birth and right atrial pressure exceeds left atrial pressure?
--It's located in the interatrial septum. The interatrial septum is in between the right and left atrium.
Before birth and in the fetus, the lungs haven't fully functioned yet, so gas exchange can't happen effectively. The foramen ovale allows oxygenated blood from the placenta to flow directly into the left atrium of the fetus without having to use the lungs. The blood then goes to the left ventricle and then to systemic circulation. In most cases, if the foramen ovale didn't close at birth, the left atrial pressure would be greater than the right atrial pressure, so the flap would stay closed. Therefore, nothing significant would occur and the fetus would be asymptomatic. However, if the right atrial pressure is greater than the left atrial pressure, the pressure gradient would reverse. This means that the blood could flow from the right to left atrium. This is bad because it allows deoxygenated blood from the systemic venous return to enter the systemic circulation by bypassing the lungs. This is allowing deoxygenated blood to go into the arteries around the body again rather than be expelled by the lungs, which is dangerous as this deprives the arteries and therefore the tissue cells of oxygen.
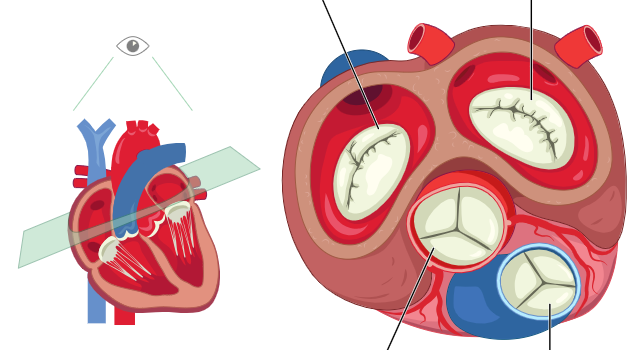
Label the valves of the heart
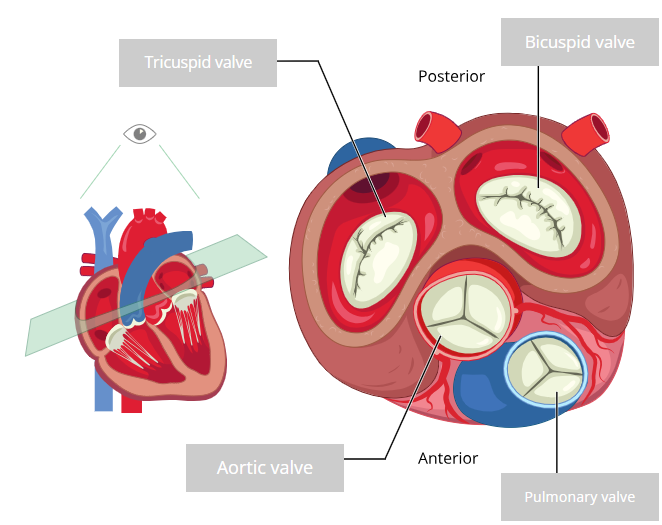
What are the semilunar valves called?
-the aortic valve
-the pulmonary valve
Semilunar valves: From which vessels do these valves prevent ‘back-flow’?
-the aortic valve prevents the backflow from the aorta
-the pulmonary valve prevents back flow from the pulmonary artery
Mitral valve (bicuspid): Which two heart chambers does it connect?
-it connects the the left atrium and left ventricle together
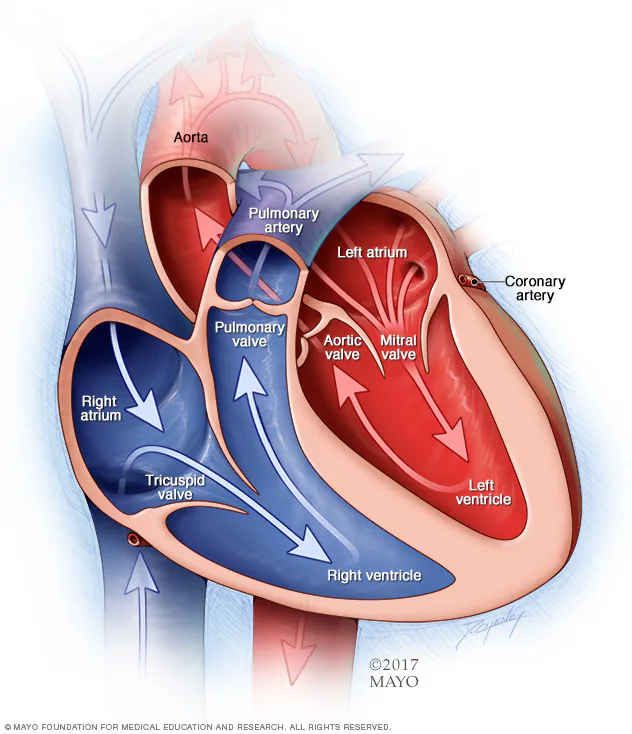
Tricuspid valve: Which two heart chambers does it connect?
-Right atrium and the right ventricle

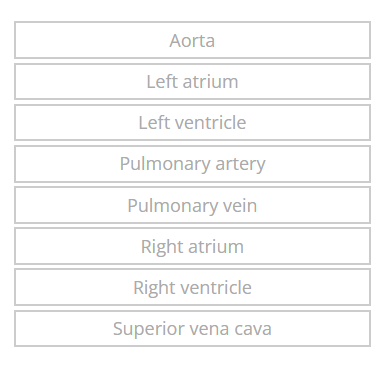
State whether each blood vessel transports oxygenated or deoxygenated vessel

What does this show?
-red and blue to indicate oxygenated and deoxygenated blood, respectively. (Right pulmonary veins are not represented.)
What would be the effect of a tricuspid valve that did not close properly and how could it affect the filling of the heart?
-if it doesn't close properly, then tricuspid regurgitation happens. This could lead to blood to flow back up into the right atrium instead of out of the heart when the right ventricle contracts.
What effect would this change in filling have on the force of contraction of the cardiac muscle and why?
-there would be a decreased distention(the abnormal expansion of the heart) of the cardiac muscles, causing the force of contraction to be decreased

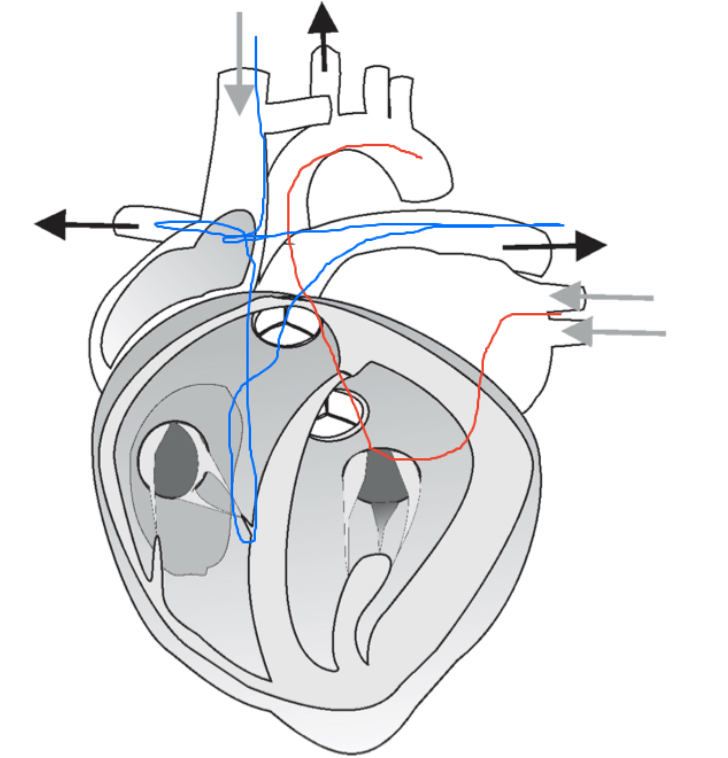
Label the conduction pathway of the heart
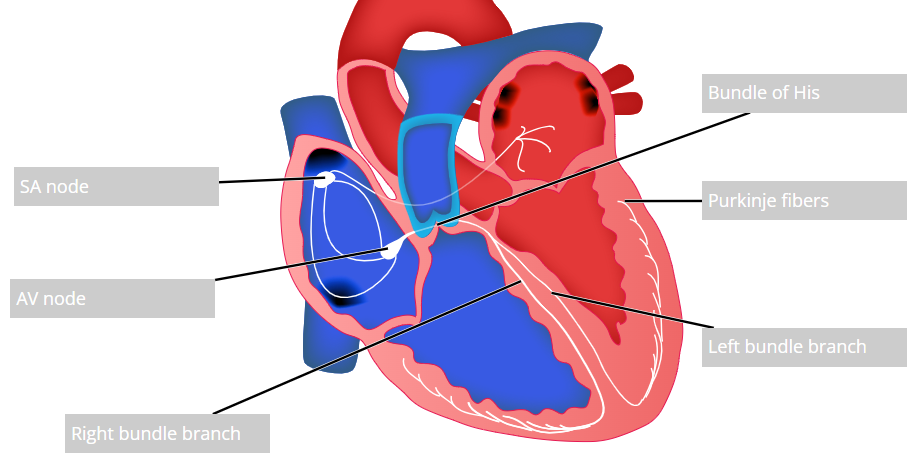
What would happen if electrical transmission through the sinoatrial node and/or the bundle of His were blocked?
-it could lead to a patient having a heart block, but the type of heart block can vary. These can cause arrhythmias. For example, they could have a first-degree block, which is a delay in their AV conduction. Or, the patient could have a third degree block.
If the heart rate increases, what happens to the duration of diastole?
-The duration of diastole shortens
Explain why it is possible for the pressure in the aorta to remain above 60-100 mm Hg during ventricular relaxation (when ventricular pressure drops nearly to zero).
-The aorta is a large artery, so it has lots of elastin fibres. These elastic tissues help to maintain the blood pressure when the ventricles are relaxing.
During the cardiac cycle, when is the muscle of the heart most effectively perfused with blood - during systole, or during diastole?
-During diastole
What effect therefore could an increased heart rate have on the perfusion of cardiac muscle?
-Decreased perfusion
Can you predict any problems for patients whose blood supply to cardiac muscle is compromised, if, for example, they exercise heavily or are under stress?
-If a person is under stress or exercising heavily, they tend to have a higher heart rate. So during diastole, less blood is perfused into the cardiac muscles, which could increase the risk of the person having a heart attack
Explain how a sphygmomanometer works in measuring blood pressure
-The cuff is placed on the upper part of the person's arm and then inflated. When it's inflated above the systolic blood pressure, the brachial artery is completely compressed, causing the blood flow to that area to stop, causing no pulse to be detected in that region. The pressure that the cuff exerts is higher than the brachial artery pressure. The cuff then deflates, allowing blood to re-flow to the brachial artery, which causes a pulse to be detected early. Now, the pressure exerted by the cuff= the systolic blood pressure. Then, the pressure at the cuff eventually decreases to a level that matches the diastolic blood pressure. Because the artery is now fully open, the normal, regular pulse can be measured.
What are some possible sources of error or variation in the sphygmomanometer/stethoscope technique of blood pressure measurement?
--body position. If the patient's arm isn't at heart level when checking their blood pressure, it can cause the reading to be too high or too low (if arm is below the heart, it can cause high blood pressure reading. If the arm is higher than heart level, it can cause low blood pressure reading.
-full bladder can increase patient's blood pressure reading by 10-15mmHg
-human error with stethoscope. If it's placed incorrectly i.e. not directly over the brachial artery, it can make it harder for the healthcare professional to detect the Korotkoff sounds.
-human error. If healthcare professional is hearing incorrectly, it could give wrong diastolic or systolic values
-if the cuff size is too big, it could give false low readings. If the cuff size is too small, can give false high reading.
Clinically, two careful measurements of blood pressure with a one-minute interval are recommended. A repeat measurement should be taken when there is any uncertainty. True or false?
-true

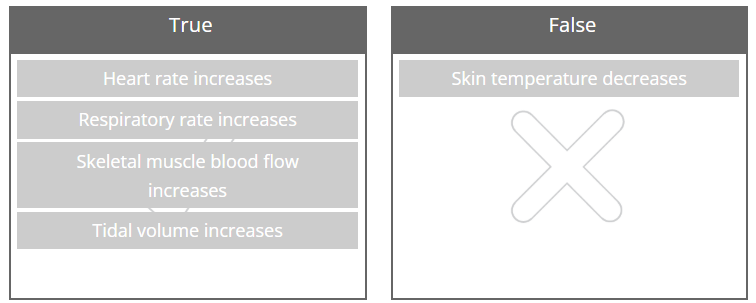
Which of the following statements are true during exercise, and which are false?
At rest, the heart rate is most affected by which of the following?
Circulating epinephrine
Parasympathetic (vagal) nervous innervation
Sympathetic nervous system
-Parasympathetic (vagal) nervous innervation
During moderate exercise, the heart rate is most affected by which of the following?
Decreased levels of circulating epinephrine
Increased parasympathetic (vagal) nervous innervation
Increased sympathetic nervous innervation
-Increased sympathetic nervous innervation
Which of the following is altered the most in conditions where heart rate is increased?
QRS interval
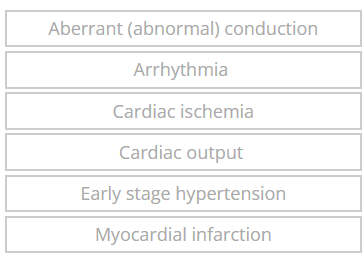
Which is detectable by ECG and which isn’t?
Which of these ventricular arrhythmias commonly results in death?
Premature ventricular complexes
Ventricular fibrillation (VF)
Ventricular tachycardia
-ventricular fibrillation
Describe the technique in which you would take this patient’s blood pressure using an automated device.
-1. pt should be sat for at least 5 mins and not have recently exercised, had caffeine or smoked, as this could affect bp readings
2. Pt's arm should be at heart level, feet flat and legs not crossed.
3. Place cuff on upper arm of pt.
4. Start the automated device and make sure pt isn't moving
5. Record the reading and repeat it again to make sure it's accurate. If the first 2 readings differ by more than 5mmHg, take a third reading. You should record the lowest reading of the last two readings. Do the same on the other arm
6. If pt did have postural hypotension, you would need to measure their standing blood pressure.
You take the patient’s blood pressure according to the guidelines and note the following results:
Left arm: 145/92 mmHg
Right arm: 148/94 mmHg
Describe the next steps you will take to identify if this patient has stage 1 hypertension.
-Offer the pt ABPM (or HBPM if they decline ABPM or they can't tolerate it) because the pt has a bp of higher than 140/90. The ABPM would involve 24 hour monitoring. You would then use the average of at least 14 daytime readings to confirm stage 1 hypertension diagnosis. If pt wants to do HBPM instead, it would involve them measuring their BP twice a day, morning and evening for 4–7 days. The readings from the first day would be discarded and you would take into account the average of the remaining readings. Stage 1 hypertension is confirmed if the average ABPM or HBPM reading is 135/85mmHg or more. If confirmed, you should also assess the pt's cardiovascular risk by doing a QRISK2/3 score, and assess for target organ damage e.g. through blood tests .
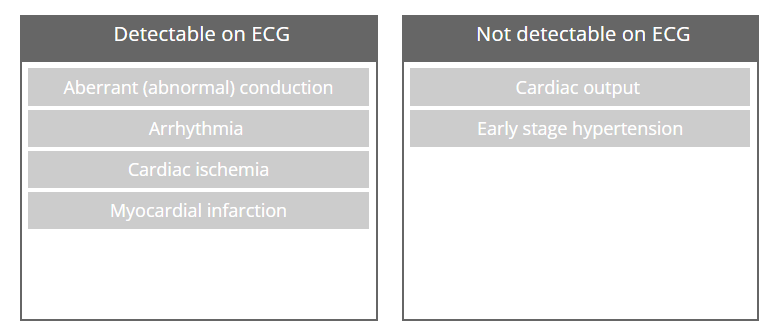
Outline 7 differences between ambulatory blood pressure monitoring (ABPM) and home blood pressure monitoring (HBPM)
Discuss your next steps if pt has HBPM or ABPM of 135/85 or more e.g. 139/82, and any action you would take in explaining these results to your patient.
-need to take into account daytime average. I would explain to the pt that their blood pressure readings show that their BP is slightly higher than normal and that it's confirmation of stage 1 hypertension. I would tell them this doesn't mean they are immediately in serious danger, but that if it's left untreated, it could lead to cardiovascular problems. Also, discuss the results of their cardiovascular risk and any target organ damage. I would then decided on the treatment I think is suitable. If the pt is less than 80 years and has target organ damage, diabetes, renal disease, cardiovascular disease, or QRISK of 10% or more, then you should offer the pt an antihypertensive drug treatment and lifestyle advice. If the pt is at low risk and has no comorbidities, you should pffer lifestyle advice first, and monitor BP regularly.
lifestyle advice:
Reduce salt and alcohol intake.
-Eat a balanced diet, and especially increase in fruit and vegetables.
-Exercise regularly (at least 150 minutes/week).
-Maintain a healthy weight
Limit caffeine and manage stress.
Plan follow-up:
- you should arrange a review with the pt in 3–6 months to reassess blood pressure and response to lifestyle changes (or treatment if started).
You have assessed the patient’s cardiovascular risk and identified this to be 10.5% (10.5% chance of suffering a cardiovascular event such as a heart attack or stroke in the next 10 years). You plan to follow-up with some further tests so now proceed to discussing next steps with regards to lifestyle interventions and treatment.
Outline below your recommendations for lifestyle interventions for this patient:
-Reduce salt intake: Aim for less than 6 g pf salt per day, which is around 1 teaspoon. It can help to not put salt on the dinner table.
-Increase fruit and vegetables (at least 5 portions a day).
-Choose things such as wholegrains, lean protein, and dairy that is low fat.
-Limit saturated fat intake and instead replace it with unsaturated fats (e.g. nuts, olive oil, nuts, oily fish like salmon).
-Limit sugar intake and processed foods to help manage weight as losing weight to a healthy level can reduce CVD risk significantly.
-Encourage at least 150 minutes of moderate to intense exercise every week (e.g. brisk walking, cycling, or swimming).
-advise pt to limit alcohol intake to no more than 14 units a week, preferably with some of those days alcohol-free.
-Advise pt to carry on not smoking.
-Reduce caffeine intake
-Encourage stress reduction techniques to help reduce blood pressure if they do experience stress g.g. through relaxation exercises, journal etc.
-pt should aim for 7–9 hours of sleep per night.
-Advise pt to get their BP checked regularly at home or in the clinic.
identify the chosen treatment path and considered drug treatment you would prescribe for this patient. (52 yr old indian woman, no diabetes and just takes paracetamol)
-The chosen treatment path would be the pt being prescribed an ACEI or an ARB. Since she doesn't take any other prescription medications other than paracetamol, there is no preference on the drug in terms of which has less interactions. Also, no contraindications in terms of her medical conditions. Also, if she has targted organ damage, closelsy monitor. If i was to prescribe an ACEi, it would likely be ramipril starting with 1.25mg once a day and after 1 month, have a consultation with pt and check bp to see if the strength needs to be increased. If i was to prescribe them an ARB, it would be losartan 50mg once a day (as she is younger than 75) for 4 weeks, then a review to see how she is doing and to check her BP and to increase strength if necessary.
What follow-up and monitoring advice would you provide to your patient after prescribing them ACEi or ARB?
--whether i prescribed ACEi or ARB, i would monitor pt's renal function and blood potassium even if it was normal before she took medication. I would plan for her to get a blood test for her renal function and blood potassium about 1-2 weeks after starting either medication and 1-2 weeks after any increase in her dose. The renal function test would include urea, electrolytes and creatinine. Then, i would ask her to get another blood test done after 3 months of starting the treatment. After the 3 month mark, I would want her to be monitored annually but if she is at higher risk of problems due to blood test results, then I would want her to be monitored for a blood test more frequently than annually e.g. every 6 months. In terms of monitoring blood pressure, I would want it to be checked after 4 weeks of starting the medication whether in clinic or at home. If her blood pressure is higher than her target, I would consider possibly adding another medication or increasing the strength. If her blood pressure is stable, I would review her BP and her adherence to the medication, including side effects every 3-6 months then annually. After 4 weeks of taking the medication, I would also have a consultation with her to see how she is doing with any side effects and adherence. Her BP target is: Clinic BP less than 140/90 mmHg and ABPM less than 135/85 mmHg as she is under 80
Define these
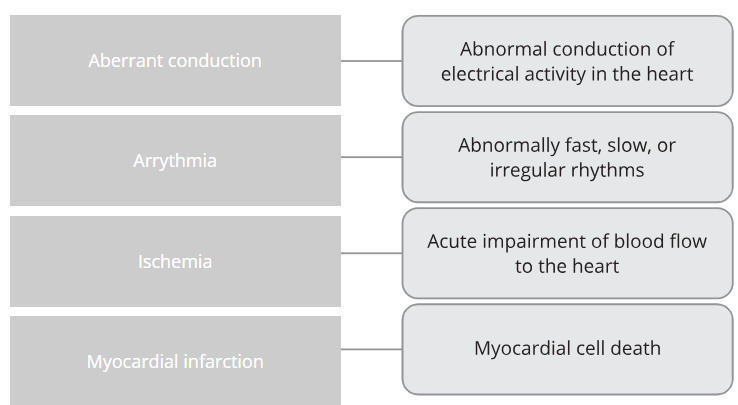
Which of these can be implied from a wide QRS complex?
-A ventricular origin of the condition