SECTION 05: FERTILIZATION, PREGNANCY, PARTURITION, AND LACTATION
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
By the end of Section 05, you should be able to:
Describe the processes by which male and female gametes unite.
Compare and contrast the roles of the corpus luteum and the placenta in secreting hormones to support the fetus.
Describe the process of parturition with an emphasis on the positive feedback loop.
Describe the process of lactation with an emphasis on its hormonal control
🌟 SIMPLE OVERVIEW:
Fertilization is when sperm and egg meet and form a zygote. This usually happens in the ampulla of the fallopian tube. After fertilization, the zygote becomes a morula, then a blastocyst, and eventually implants in the uterus.
– STAGES OF FERTILIZATION & IMPLANTATION - 📍 Step 1: Ovum Transport
Ovum (egg) is released from the ovary at ovulation
Fimbriae sweep the egg into the fallopian tube
Peristalsis (smooth muscle waves) moves it to the ampulla
Flashcard:
🥚 Ovum released → Fimbriae → Ampulla via peristalsis
STAGES OF FERTILIZATION & IMPLANTATION 📍 Step 2: Sperm Transport
Sperm deposited in vagina
Must pass cervical mucus (thin only around ovulation due to high estrogen)
Reach uterus → myometrial contractions push them toward oviducts
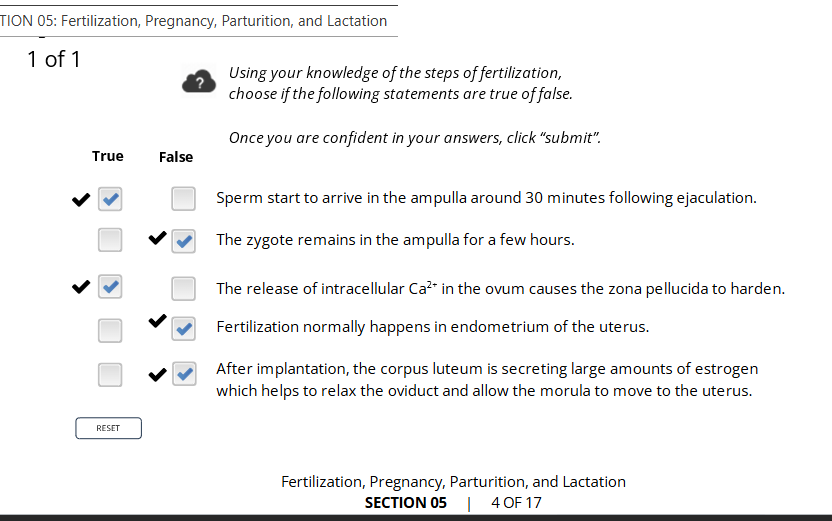
Reach ampulla ~30 minutes after ejaculation
Flashcard:
🧬 Sperm swim + uterus helps push → Reach egg in ampulla
STAGES OF FERTILIZATION & IMPLANTATION
📍 Step 3: Fertilization
Sperm passes corona radiata (outer follicle layer) using enzymes
Binds to ZP3 on zona pellucida
Triggers acrosome reaction → enzymes released to digest through
First sperm fuses with egg, enters, triggers Ca²⁺ release
Flashcard:
🧠 Key proteins:
Fertilin (sperm) binds to ZP3 (egg)
Acrosome enzymes digest the zona
Ca²⁺ release = blocks other sperm + finishes meiosis
📍 Result of Ca²⁺ Release in Egg
📍 Step 4: Implantation
Zygote divides → becomes morula (solid ball)
Morula → blastocyst (hollow ball with inner cell mass)
Moves to uterus (helped by progesterone)
Blastocyst floats for a few days, nourished by endometrial secretions
Then implants into uterine lining → fully buries itself
Flashcard:
🍼 Morula → Blastocyst → Uterus → Implants in endometrium
✅ Summary Flow (One-Liner Memory Aid):
Ovary → Ampulla → Fertilization → Zygote → Morula → Blastocyst → Uterus → Implantation
how sperm meets the egg and fertilization occurs 🧬 SIMPLE OVERVIEW:
Fertilization is the epic journey where sperm travels through the female reproductive tract to reach and fuse with the egg in the ampulla of the fallopian tube. From 300 million sperm, usually only one wins — forming a zygote, the very first cell of a new human life.
HOW SPERM MEETS THE EGG (9 steps) - 📍 Step 1: Sperm Enters the Vagina
~300 million sperm are ejaculated
Many die in the acidic vaginal environment
Seminal fluid helps protect some sperm
Flashcard:
✅ 300 million sperm enter → many die in acid → few survive
📍 Step 2: Cervix Opens (During Ovulation)
Cervical mucus becomes thin from high estrogen
Sperm swim through; some get stuck, others go on
Flashcard:
✅ Cervical mucus thins at ovulation → sperm can pass
📍 Step 3: Journey Through the Uterus
Uterine contractions help push sperm toward the fallopian tubes
Immune cells kill many sperm
Flashcard:
✅ Uterus helps move sperm → immune system attacks
📍 Step 4: Fallopian Tube & Cilia
Half of sperm go to the wrong side
The rest go toward the egg
Cilia push egg toward uterus, sperm swim against it
Sperm become hyperactive due to chemical changes
Flashcard:
✅ Sperm swim upstream → hyperactive from chemical triggers
📍 Step 5: Reaching the Egg
Only a few dozen sperm make it to the egg
Egg is surrounded by:
Corona Radiata (outer cell layer)
Zona Pellucida (protective glycoprotein shell)
Flashcard:
✅ Few sperm reach egg → must get through 2 layers
📍 Step 6: Penetration & Fusion
Sperm bind to ZP3 receptors on zona pellucida
Triggers acrosome reaction → releases enzymes
Sperm burrow into the egg
Flashcard:
✅ Sperm binds to ZP3 → acrosome enzymes digest entry path
📍 Step 7: Zinc Spark + Egg Reaction
First sperm to enter triggers:
Zinc spark (new discovery!)
Ca²⁺ release
Zona hardens to block other sperm
Sperm tail left outside
Egg completes meiosis II
Flashcard:
✅ 1 sperm fuses → sparks, hardening, meiosis II finishes
📍 Step 8: Fertilization & Zygote Formation
Male and female DNA form pronuclei (each with 23 chromosomes)
Microtubules pull them together
Chromosomes merge → zygote formed
Unique genetic code is created (eye color, sex, etc.)
Flashcard:
✅ Pronuclei merge → new life starts = zygote
📍 Step 9: Zygote Moves to Uterus
Cilia sweep the zygote to the uterus
It will implant into the endometrial lining
Will grow for the next 9 months if conditions are right
Flashcard:
✅ Zygote → uterus → implants → pregnancy begins
✨ Bonus: Zinc Sparks (from video)
Zinc released by egg during fertilization
Visible as "sparks" using special photography
May help doctors choose healthy embryos during IVF
Flashcard:
✅ Zinc spark = sign of healthy egg activation 🧬⚡
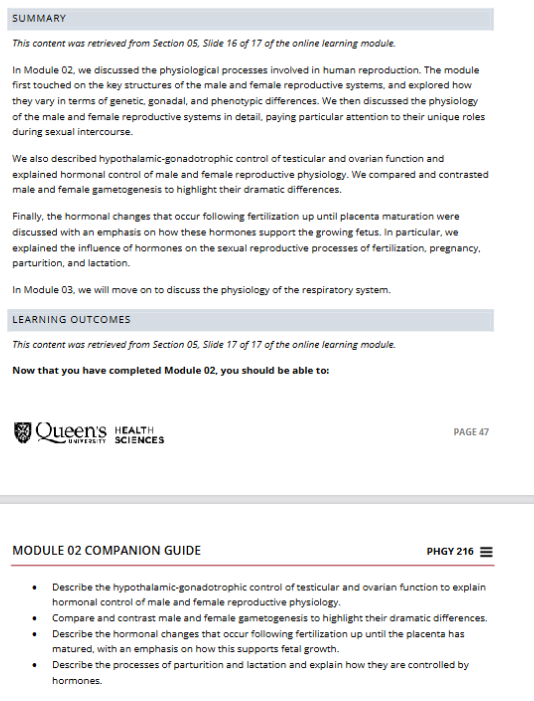
Activity
🌟 SIMPLE EXPLANATION:
Identical twins = 1 egg + 1 sperm → splits into 2 babies
Fraternal twins = 2 eggs + 2 sperm → 2 babies at the same time
📍 What are Identical (Monozygotic) Twins?
1 egg is fertilized by 1 sperm
The single zygote splits into two embryos
They share 100% identical DNA
Usually share a single placenta
Flashcard:
👯♀ Monozygotic = One egg splits → identical twins (same DNA + usually shared placenta)
📍 What are Fraternal (Dizygotic) Twins?
2 eggs released and fertilized by 2 separate sperm
Develop as two separate zygotes
Genetically like siblings (share ~50% DNA)
Always have separate placentas
Flashcard:
👫 Dizygotic = Two eggs, two sperm → fraternal twins (different DNA + separate placentas)
📍 Key Differences at a Glance:
🧠 Quick Memory Tip:
“Mono” = One egg → Mirrored twins
“Di” = Two eggs → Different twins
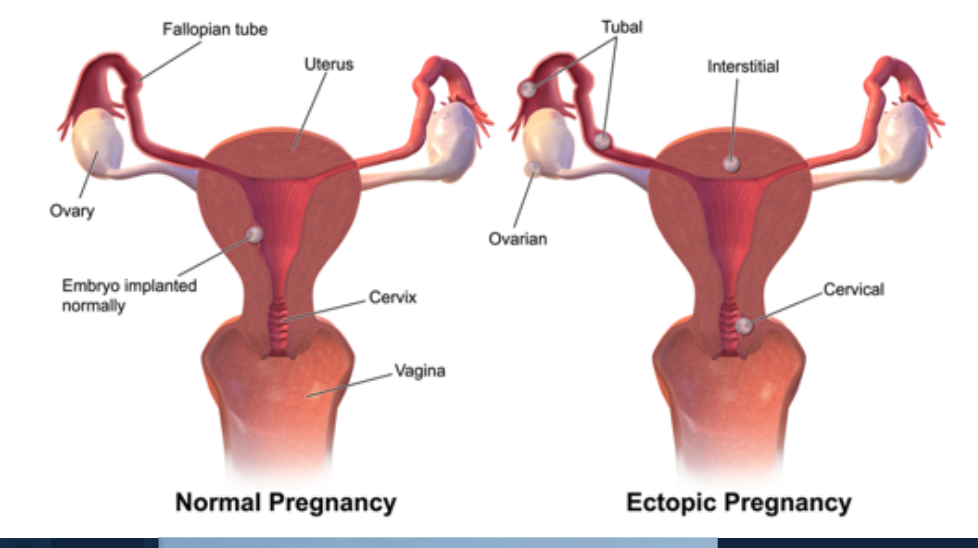
🌟 SIMPLE OVERVIEW:
In a normal pregnancy, the fertilized egg implants in the uterine lining.
In an ectopic pregnancy, the egg implants outside the uterus, most commonly in the fallopian tube.
This can be dangerous and requires urgent treatment to avoid serious health risks.
📍 What is a normal pregnancy?
Fertilized egg implants in the uterus
➤ Safe space for embryo growth
Flashcard:
✅ Normal = Uterus implantation → safe for development
📍 What is an ectopic pregnancy?
Fertilized egg implants outside uterus
Most commonly in the fallopian tube (tubal)
Can also implant in the ovary, cervix, or abdomen
Flashcard:
❌ Ectopic = Wrong place (fallopian tube, ovary, cervix)
📍 Why is a tubal pregnancy dangerous?
The fallopian tube is too narrow and thin-walled
Pregnancy only needs to grow to jellybean size to rupture the tube
This can cause severe internal bleeding
Flashcard:
⚠ Tubal pregnancy can burst tube → major bleeding
📍 How common is ectopic pregnancy?
~1 in 60 pregnancies
Rare, but serious
Flashcard:
📊 Ectopic = ~1 in 60 pregnancies
📍 Risk Factors? - ectopic pregnancies
📍 Treatment?
Must be treated medically or surgically
Prevents life-threatening bleeding
Flashcard:
🚑 Treat fast! Ectopic = medical emergency
placenta development and function 🌟 SIMPLE OVERVIEW:
The placenta is an organ that forms during pregnancy to support the growing baby. It connects the baby to the uterus via the umbilical cord and acts like the baby's lungs, kidneys, and digestive system — all in one!
PLACENTA DEVELOPMENT TIMELINE - 📍 4 Weeks
By day 12, the embryo is fully embedded in the uterine lining
The surrounding endometrial tissue begins forming the placenta
Flashcard:
🪴 Week 4 = Implantation complete → placenta starts forming
PLACENTA DEVELOPMENT TIMELINE 📍 8 Weeks
Placenta is not fully formed yet, but is already working
Begins exchanging nutrients and waste
Flashcard:
🔄 Week 8 = Placenta is functional, even if not fully built
PLACENTA DEVELOPMENT TIMELINE 📍 12 Weeks
Maternal blood supply to placenta is now complete
Placenta has all structures needed to support fetus until birth
Flashcard:
✅ Week 12 = Placenta fully developed & fully connected to mom’s blood
PLACENTA DEVELOPMENT TIMELINE 📍 40 Weeks
Placenta continues to grow and function throughout pregnancy
Acts as:
Lungs (gas exchange)
Digestive system (nutrients)
Kidneys (waste removal)
Umbilical cord connects baby to placenta
Flashcard:
🧠 Week 40 = Placenta = baby’s life support (lungs + kidneys + food source)
📍 EXTRA: Placenta Functions
📍 Progesterone
Also rises steadily during pregnancy
Maintains endometrium
Suppresses contractions (prevents early labour)
Flashcard:
🛡 Progesterone = Stabilizes uterus lining + stops early contractions
hCG (Human Chorionic Gonadotropin) 📍 Source
First hormone secreted by the developing placenta
Starts early in pregnancy
Flashcard:
🧬 hCG = First hormone from placenta
hCG (Human Chorionic Gonadotropin) 📍 Function
Mimics LH → binds to LH receptors
Maintains corpus luteum → keeps producing estrogen + progesterone
Corpus luteum becomes “corpus luteum of pregnancy”
Flashcard:
🛡 hCG = Supports corpus luteum → maintains hormone levels
hCG (Human Chorionic Gonadotropin) 📍 Timeline
Peaks early (first 10 weeks)
Drops to low, steady level once placenta takes over hormone production
Corpus luteum stays until birth
Flashcard:
📈 Peaks early → 📉 lowers after week 10
hCG- 📍 Other Roles
Stimulates Leydig cells → testosterone in male fetus
Needed for male reproductive development
May be linked to morning sickness
Flashcard:
👶 hCG = Triggers testosterone in male fetus
🤢 Linked to morning sickness (unclear role)
hCG - 📍 Clinical Use
Detected in urine before embryo seen
Basis of pregnancy tests
Flashcard:
✔ hCG = Detected in pregnancy tests
📍 Can the Placenta Make Estrogen from Cholesterol?
❌ No. The placenta can’t make estrogen from cholesterol directly
It needs DHEA (a hormone made by the fetal adrenal cortex)
Flashcard:
🚫 Placenta can’t make estrogen from cholesterol → needs fetal DHEA
📍 Where Does Estrogen Come From?
1. Cholesterol from maternal + fetal blood
2. Cholesterol → converted into DHEA by fetal adrenal cortex
3. DHEA enters fetal blood → then goes to placenta
4. Placenta converts DHEA → estrogen (estriol) → releases into maternal blood
Flashcard:
🛤 Cholesterol → DHEA (fetus) → Estriol (placenta) → Mom’s blood
📍 Main Type of Estrogen from Placenta?
Estriol
(vs. estradiol from ovaries)
Flashcard:
🧬 Placenta = estriol, Ovaries = estradiol
📍 Why Is Estriol Important?
Used as a marker for fetal health
Indicates proper DHEA production (fetal adrenal health)
Flashcard:
🩺 Estriol = Fetal viability check marker
📍 Functions of Estrogen (Estriol) in Pregnancy
Increases myometrium growth (uterus muscle mass)
Prepares uterus for labour
Promotes mammary duct development
Flashcard:
💪 Builds uterus + 🍼 Preps breast ducts for milk + 🚼 Preps for labour
📍 Source of Progesterone Early in Pregnancy
Corpus luteum produces it first
Placenta takes over by ~10 weeks
Flashcard:
🟡 Week 1–10 = Corpus luteum
🔵 Week 10+ = Placenta makes enough progesterone
📍 How is Placental Progesterone Made?
Cholesterol from maternal blood enters placenta
Placenta converts cholesterol into progesterone
Progesterone is secreted into maternal blood
Flashcard:
🛤 Cholesterol → Progesterone (in placenta) → into mom’s blood
📍 Does Placenta Need Help Making Progesterone?
❌ No. Placenta can make progesterone on its own
Unlike estrogen, it doesn’t need fetal precursors
Flashcard:
✅ Placenta = independent for progesterone
❌ Needs fetal DHEA for estrogen
📍 Functions of Progesterone in Pregnancy
Maintains endometrium
Keeps cervical mucus plug in place
Prepares milk glands
Inhibits uterine contractions (prevents early labour)
Flashcard:
🛡 Progesterone = Protects pregnancy (lining, mucus, milk, stops contractions)
Estrogen & Uterine Contractions (Parturition) 📍 What triggers labor prep at the end of pregnancy?
A surge in estrogen near the end of gestation
Flashcard:
📈 End of pregnancy = ↑ Estrogen surge
estrogen’s role in parturition (childbirth) (2 roles) - 📍 Role 1: Gap Junction Formation
Estrogen increases gap junctions between myometrial cells
This allows the uterus to contract as one unit
Flashcard:
🔗 Estrogen = ↑ gap junctions → uterus contracts together
📍 Role 2: Oxytocin Receptor Increase
Estrogen increases oxytocin receptors in the myometrium
Makes the uterus more sensitive to oxytocin, even in low amounts
Flashcard:
🎯 Estrogen = ↑ oxytocin receptors → uterus responds better to oxytocin
estrogen’s role in parturition (childbirth) - final result
Coordinated uterine contractions that respond strongly to oxytocin
→ Prepares uterus for labour
Flashcard:
🤰 Estrogen = primes uterus for strong, coordinated labour contractions
Positive Feedback Loop in Labour (Parturition) - 📍 What starts the loop?
Estrogen ↑ → uterus becomes more sensitive to oxytocin
Oxytocin (from posterior pituitary) triggers uterine contractions
Flashcard:
🟢 Estrogen ↑ → uterus sensitive to oxytocin → 🔁 contractions start
Positive Feedback Loop in Labour (Parturition) 📍 Step-by-Step Cycle:
↑ Uterine Contractions
Fetus pushed against cervix
Neuroendocrine reflex triggered
↑ Oxytocin secretion
↑ Prostaglandin production
More prostaglandins = stronger uterine contractions
Flashcard:
👶 Pressure on cervix → reflex → ↑ oxytocin → ↑ prostaglandins → ↑ contractions
📍 What kind of feedback loop?
Positive feedback loop
Keeps going until the baby is born and pressure is gone
Flashcard:
🔁 Positive feedback = keeps increasing until birth
Positive Feedback Loop in Labour (Parturition) 📍 When does it stop?
After delivery, cervical pressure is gone → oxytocin returns to normal
Flashcard:
🛑 Birth ends the loop → oxytocin levels ↓
📍 What is the role of positive feedback in parturition?
It ensures a continuous and increasing cycle of contractions by raising oxytocin levels.
Flashcard:
🔁 Positive feedback = ↑ oxytocin → ↑ contractions → ↑ cervix pressure → ↑ oxytocin
Why Positive Feedback Is Necessary for Birth
Strong uterine contractions are needed to push the baby out
Cervical pressure triggers even more oxytocin → stronger contractions
This loop continues until the baby is delivered
Flashcard:
🤰 No feedback = weak contractions → cervix won’t open → baby can’t be delivered
📍 What happens if positive feedback didn’t happen?
Oxytocin would not increase
Contractions would stay weak or stop
Cervix would not dilate
Labour would stall → no birth
Flashcard:
❌ No feedback = no progress → labour fails
📍 What ends the feedback loop?
Once the baby is born, the cervix is no longer stretched, so oxytocin levels fall
Flashcard:
🛑 Birth = cervix pressure gone → oxytocin drops → feedback ends
📍 What are mammary glands made of?
Ducts: carry milk to the nipple
Lobules: clusters of alveoli that produce milk
Alveoli: milk-secreting units lined by epithelial cells
Myoepithelial cells: surround alveoli and contract to eject milk
📍 Where is milk made?
In alveolar epithelial cells
→ milk is secreted into the lumen of alveoli
→ moves through ducts to the nipple
📍 What hormone builds milk ducts?
Estrogen
→ Develops the milk duct system
📍 What hormone forms alveoli?
Progesterone
→ Promotes growth of alveoli (milk sacs)
📍 What stimulates milk production enzymes?
Prolactin
hCG
→ Together, they prep the breast to make milk
📍 Why is milk not secreted before birth?
High estrogen and progesterone block prolactin
→ After parturition, these drop
→ Prolactin is now free to trigger milk production
📍 BONUS – Milk ejection (let-down reflex)
Caused by oxytocin triggering myoepithelial cell contraction
📍 What triggers milk production and ejection?
Suckling → stimulates mechanoreceptors in nipple → signals sent to hypothalamus
STIMULATION OF LACTATION 📍 What two hormones are involved?
Oxytocin (from posterior pituitary)
Prolactin (from anterior pituitary)
📍 Oxytocin – What does it do?
Released from posterior pituitary
Causes contraction of myoepithelial cells
➝ Ejects milk from alveoli
🔄 Can also be triggered by baby crying
📍 Prolactin – What does it do?
Released from anterior pituitary
Stimulates milk production in alveolar epithelial cells
📍 What regulates prolactin?
↓ PIH (Prolactin Inhibiting Hormone = dopamine)
↑ PRH (Prolactin Releasing Hormone = possibly oxytocin)
📍 Key concept from the diagram:
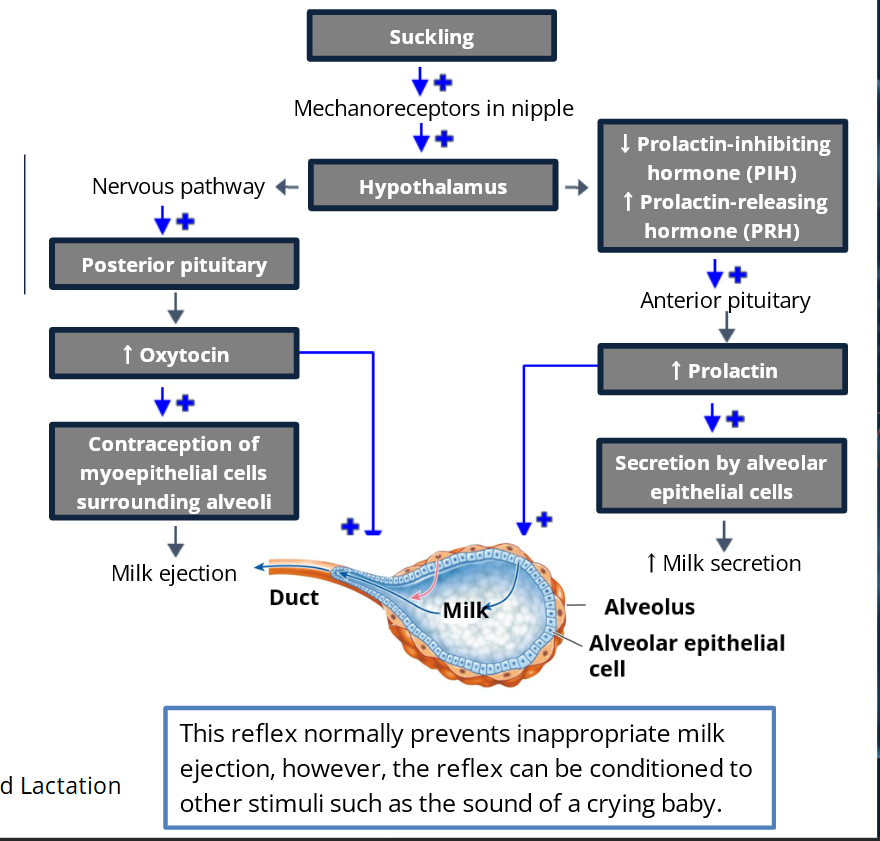
Milk ejection = oxytocin
Milk production = prolactin
Milk must be ejected actively – baby can’t suck it out from alveoli alone
📍 What regulates prolactin? (further explanation)
🔽 PIH = Prolactin Inhibiting Hormone
Real name: Dopamine
Job: Tells the anterior pituitary to NOT release prolactin
Think of it like a brake pedal. When dopamine is high → no prolactin is made.
🔼 PRH = Prolactin Releasing Hormone
This one encourages prolactin release
It's less clearly defined, but is suspected to be oxytocin acting within the hypothalamus (⚠ not the same oxytocin that causes milk ejection — just similar).
Think of it like the gas pedal. When PRH goes up → prolactin gets released.
🧠 How this works during breastfeeding:
Baby suckles → sends signal to hypothalamus
Hypothalamus ↓ dopamine (PIH) and ↑ PRH
This tells anterior pituitary to release prolactin
Prolactin → makes more milk 🍼
Module 2 summary and learning outcomes