pubh exam 3
1/160
Earn XP
Description and Tags
6, 7, 8
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
161 Terms
Which of the following is true of tests used for screening for disease?
1. One positive screening test usually is not sufficient to diagnose a
disease.
2. Changes within the range of normal test results may be due to
disease presence.
3. The range of normal is not the same for all individuals, groups or
populations.
4. All of these are correct.
4. All of these are correct.
Which statement best describes the mortality due to drug overdoses in
the United States?
1. Deaths from motor vehicles exceed deaths from drug overdoses.
2. Deaths from drug overdoses implies willful intent of victims.
3. Deaths from drug overdoses has declined in recent years.
4. None of the above.
3. Deaths from drug overdoses has declined in recent years.
Why is lung cancer considered a ’serious’ illness?
1. It accounts for substantial morbidity and mortality.
2. Treatment is well-established.
3. It is easily detected.
4. All of the above.
1. It accounts for substantial morbidity and mortality.
Which of the following statements is true about QALYS?
1. A QALY may be interpreted as a year of life at full health compared
to immediate death.
2. QALYs take into account the number of life-years saved.
3. In economic analyses, the cost of an additional QALY of less than
$50,000 is considered to be cost-effective in the U.S.
4. All of the above are correct.
4. All of the above are correct.
Which of the following can be considered cost-effective?
1. An intervention that reduces the cost while increasing the net-
benefit of care.
2. An intervention that reduces the cost and net-benefits of care.
3. An intervention that increases net benefit, but increases cost of
care.
4. An intervention that reduces cost of care
1. An intervention that reduces the cost while increasing the net-benefit of care.
public health framework for differentiating disease and disability
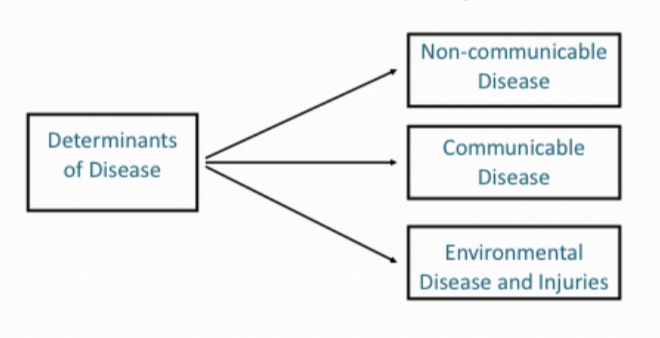
by separating a "health condition" (which includes disease) from "disability," which is an umbrella term for impairments, activity limitations, and participation restrictions
Disease is seen as an interruption of normal body function (pathology) or a health condition itself
Disability results from the interaction between this condition and environmental factors, and the individual's resulting limitations in daily activities and social roles
non-communicable diseases (NCDs)
chronic conditions that do not result from acute infectious processes and are not communicable
a disease that has a prolonged course that does not resolve spontaneously and for which a complete cure may be difficult to achieve
characteristics of non-communicable disease
complex (multifactorial) causes
long latency period
prolonged course of illness
functional impairment/disability
common etiologies across similar conditions
coronary heart disease
problems with blood vessels supplying the heart muscles
cerebrovascular disease
problems with blood vessels supplying the brain
peripheral arterial disease
problems with blood vessels supplying the arms and legs
congenital heart disease
malformation of heart structure
Cardiovascular disease risk factors - major modifiable factors
tobacco use
hypertension
hyperlipidemia
physical inactivity/obesity
unhealthy diets
diabetes
? :
SES, mental heal, heavy alcohol use, medication use, personality
Cardiovascular disease risk factors - non modifiable factors
age
gender
heredity
race/ethnicity
inflammatory markers
cancer
30-50% due to lifestyle
proliferative cell growth beyond usual boundaries
benign : non cancerous
in-situ : localized and has not spread from where it started
invasive : spread from original location to surrounding tissue
cervical cancer risk factors
HPV infection, smoking, family history, poverty, no PAP test
lung cancer risk factors
tobacco, radiation, asbestos, radon, air population
great cancer risk factors
reproductive hormones, weight, race, age
colorectal cancer
age, diet, family history
diabetes
disorder of the metabolism
gestational
glucose intolerance
type1 (10%) : genetic/biological
type2 (90%) : biological & sociological
diabetes - major modifiable factors
unhealthy diets
physical inactivity
obesity/overweight
hypertension
high cholesterol
? :
low birth weight, SES, mental health, heavy alcohol use, heavy sugar consumption, light fiber consumption
Chronic Obstructive Pulmonary Disease (COPD)
90% of deaths are in low to middle income countries
two main conditions that make it up :
chronic bronchitis
inflammation of the airways and a persistent cough with mucus
emphysema
involves damage to the air sacs in the lungs, leading to SOB
major stages in the disease process
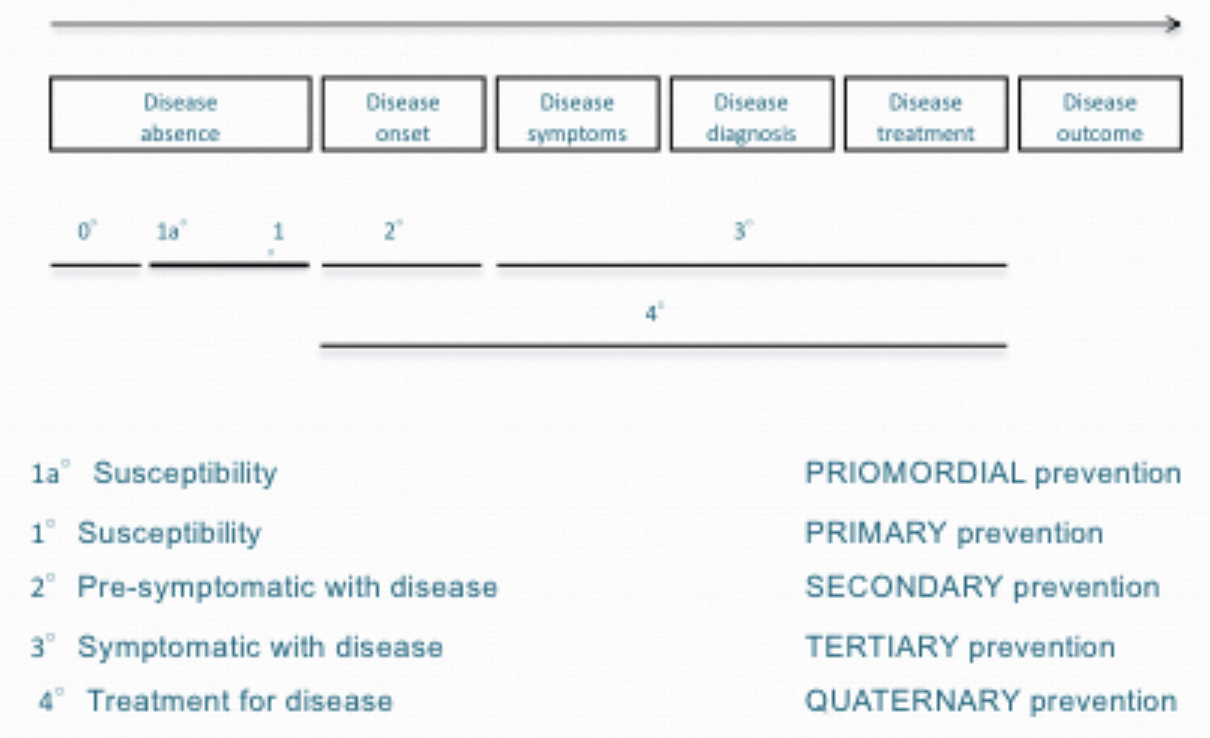
disease absence, disease onset, disease symptoms, disease diagnosis, disease treatment, disease outcome
principle mechanism for chronic disease control : secondary prevention to detect re-symptomatic disease
disease screening
the application of simple medical tests/procedures with asymptomatic individuals in search of evidence of pathology/disease
blood pressure, BMI, weight and waist circumference, skin checks, cholesterol, bloop pressure, vision, hearing, STIs, substance use, urinalysis, cancer, mental acuity, diabetes
a presumptive judgement distinguishing apparently well persons from actually well persons
intention to be efficacious (results influences clinical decisions) and effective (results influence disease course)
why screen? secondary prevention
disease is serious
disease has an asymptomatic period for early detection
early detection improves survival, reduces morbidity, lowers costs
public is willing to be screened
why not screen? secondary prevention
yield is low (resources expended on persons who do not benefit)
biological and test variability makes screening results less reliable
false security with false negative results delay diagnosis and treatment
unnecessary intervention with false positive produces unnecessary stress/anxiety, pain/discomfort, expense, inconvenience, and/or pathological exposures
end results are unchanged
true positive : screen works
the diagnostic gold standard determines : disease present
the screening test result suggests : disease present
false positive : screening fails
the diagnostic gold standard determines : disease is absent
the screening test result suggests : disease is present
the gold standard
the most definitive or accurate diagnostic method available for a specific disease, used as a benchmark to compare other tests against.
screening test
is a quick, preliminary test to identify individuals at increased risk for a disease
false negative : screening fails
the diagnostic gold standard determines : disease is present
the screening test result suggests : disease is absent
true negative : screening works
the diagnostic gold standard determines : disease is absent
the screening test result suggests : disease is absent
the efficacy of a test is judged by
how well it identifies diseased and non-diseased cases
measures by concepts of sensitivity and specificity
a test is considered sensitive when
it is good at identifying disease when it is present
a test is considered specific when it is
good at identifying non-disease when there is no disease
sensitivity
true positive / (true positive+false negative)
specificity
true negative / (true negative+false positive)
the effectiveness is a test is judged by
how well it predicts whether a person has or does not have a condition
a test with a Positive Predicative Value (PPV+)
when a positive result is indicative of the presence of a condition
a test has a Negative Predicative Value (PPV- or NPV)
when a negative result is indicative of the absence of a condition
PPV+
TP / (TP+FP)
PPV-
TN / (TN+FN)
positive predictive values are
higher when specificity (ability of the test to correctly identify those without the condition is high) and prevalence of the condition is low
negative predictive values are
higher when sensitivity (ability of the test to correctly identify those with the condition is high) and prevalence of the condition is high
efficacy and effectiveness of screening : the necessary trade offs
in the interest of achieving high sensitivity, a test tends to have low specificity
its really important to find cases
in the interest of achieving high specificity, a test tends to have low sensitivity
it’s really important to exclude individuals
in order for a test to be sensitive it will necessarily identify a fair number of false positives in the course of capturing many true positives
therefore the positive predictive value of a sensitive test tends to be low
in order for a test to be specific, it will necessarily identify a fair number of false negatives in the course of excluding true negative
therefore, the negative predictive value of a specific test tends to be low
Deciding who is ill and who is not is
both a scientific and social consideration
Persons who are considered ill have different rights and responsibilities than persons who are not
illWe want to distinguish the two groups, but the screening tool necessarily will produce
errors (declaring some health people ill and some ill people healthy)!
lowering the screening threshold
captures more ill persons, BUT misclassifies many healthy people as ill
raising the screening threshold
captures more healthy persons, BUT misclassifies many ill persons healthy
sensitivity?
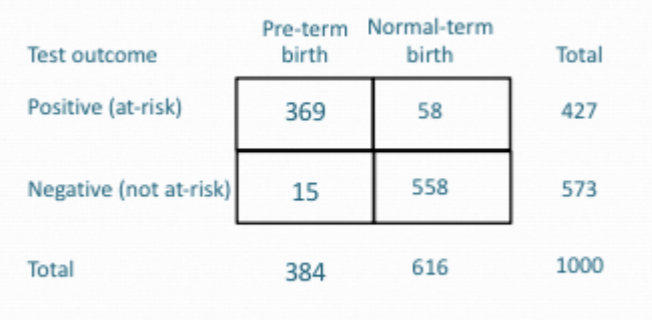
369 / 384 = 0.961
specificity?
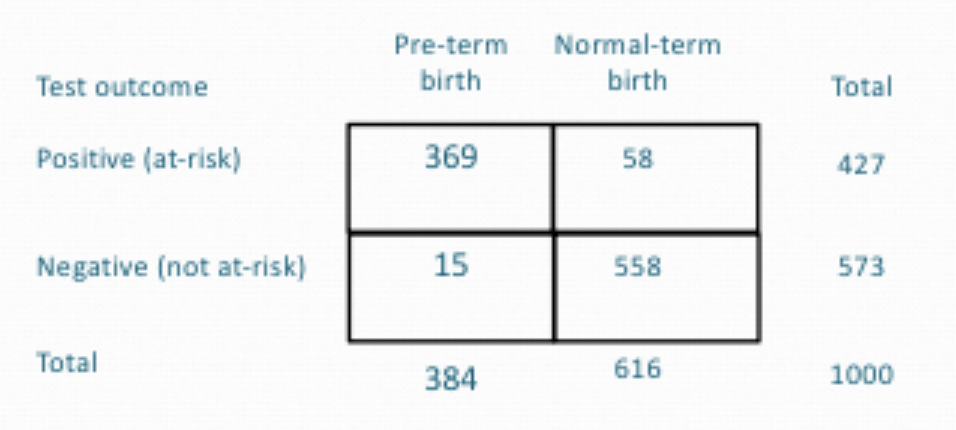
558 / 616 = 0.906
positive predictive value
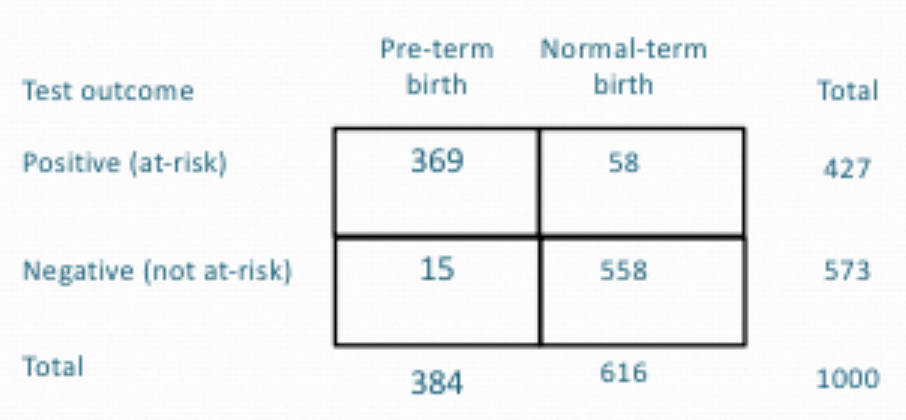
369 / 427 = 0.864 (86.4%)
negative predictive value
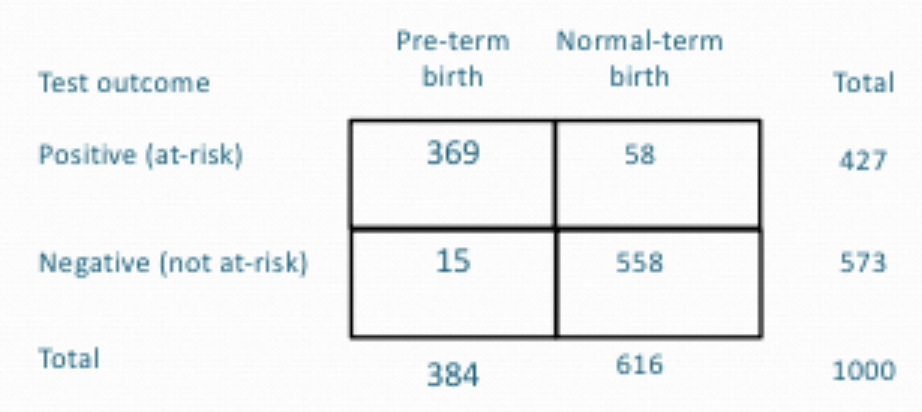
558 / 573 = 0.974
what is true of HIV
It has a longer incubation period than influenza.
It can be transmitted before it can be detected by commonly used antibody
tests.Drug treatment can reduce the degree of communicability.
which characteristic of infectious disease is reflected in the following
statement? “Hepatitis B can survive for extended periods of time in
contaminated needles.”
Persistence in the environment is evident
which disease is the least likely to be eradicated?
influenza
what is true of tuberculosis (TB)
Tuberculosis may remain contained in the body for decades without causing
disease.Isolation has been used in the past as a major strategy for controlling the
spread of TB.People with AIDS are at increased risk of developing active TB
What has been successfully used to control communicable
diseases?
Contact tracing
Isolation
Treatment upon exposure
Communicable disease:
illness due to a microorganism such as bacterium, parasite or virus that is transmitted person-to-person or animal/physical environment to humans via air, water, fomites, insect or animal bites
Non-Communicable Disease (NCDs) that can be influenced or triggered by
infectious agents:
• Cervical cancer, for example, is caused by the Human Papilloma Virus
(HPV).
• Liver cirrhosis and cancer can be the byproduct of Hepatitis B and C.
• Stomach cancer is associated with H pylori infection.
• Heart health may be compromised by a history of COVID-19
• Heart attack and stroke may be triggered by Influenza
• Rheumatic heart disease can be caused by streptococcal infection.
Communicable diseases that can be influenced or triggered by NCDs
• Smoking and diabetes can increase the risk of tuberculosis.
• HIV treatment can increase the risk of cardiovascular disease.
• Malnutrition can make individuals susceptible to HIV, TB, Malaria, etc
biological sources of communicable diseases
bacterium
viruses
fungus
parasite
bacterium
single-celled microorganism able to exist free-living as a parasite
virus
microorganisms unable to exist independent of living cell
fungus
spore-producing organisms that feed on organic matter
parasite
organism living in, on, or with another organism in order to obtain nutrients
examples of bacterial infections
salmonella, e.coli, bubonic plague, MRSA
examples of viral infections
varicalle —> chicken pox
rubella —> measles
pertussis —> whooping cough
examples of fungal infections
tinea pedis - athlete’s foot
candidiasis - thrush
tinea corpori’s - ringworm
parasite infections
guinea worm disease
pinworm disease
vectors
an organism that is usually an arthropod like a mosquito or tick, that carries and transmits infectious agents such as viruses, bacteria, or parasites between hosts
bedbugs, Lyme disease
dengue fever
Virus caused by the bite of infected Aedes mosquitoes.
While many cases are mild, causing flu-like symptoms, severe can lead to serious complications like hemorrhaging, shock, and death.
no specific cure, but treatment focuses on managing symptoms with rest and fluids
tick-borne illnesses
bacterial, viral or parasitic diseases spread through the bite of infected
ticks.
Symptoms can vary but often include fever, headache, fatigue, and muscle aches
fomites
inanimate objects that can transmit infectious microorganisms
and be the source of disease
Common infections: MRSA, Adenovirus, Coronavirus, hand, foot, and mouth
disease, Influenza, Norovirus, Rhinovirus, and Rotavirus
sporadic
unexpected, infrequent, irregular
endemic
expected, regular, indefinite, bounded
epidemic
unexpected, abnormal, finite, bounded
pandemic
unexpected, abnormal, irregular, finite, unbounded
Ignaz Semmelweis (1818-1865)
emphasized handwashing with chlorinated lime water to reduce maternal mortality from puerperal fever
John Snow (1813-1858)
stopped a London cholera outbreak by limiting access to a contaminated public water supply.
Joseph Lister (1827-1912)
introduced antiseptic methods in surgery, based on Pasteur's findings, to prevent wound infections.
communicable disease framework - how do conditions that cause disease relate?
Agent, Host, Environment
Agent - communicable disease framework
factor(s) external to the individual capable of causing disease, illness
host - communicable disease framework
the individual capable of acquiring disease, illness
environment - communicable disease framework
the setting in which the agent and host come into contact
10 steps in outbreak investigations
• Establish the existence of an outbreak
• Prepare for fieldwork
• Verify the diagnosis
• Define and identify cases
• Use descriptive epidemiology to assess burden to population
• Develop causal(transmission) hypotheses
• Use analytic epidemiology to evaluate the hypotheses
• Refine hypotheses
• Implement control and prevention measures
• Communicate findings to the public
infectivity
ability of a bacteria, fungi, parasites or virus to enter into a living organism through horizontal transmission
direct contact
spread of infectious organism from one person to other
indirect contact
spread of infectious organism by individual coming in contact with contaminated object
modes of infectious transmission
airborne, soil, blood-borne, droplet, diet, zoonosis, oral, sexual contact, vector, bites, fomites
airborne - modes of infectious transmission
anthrax, measles, TB, smallpox, varicella
soil - modes of infectious transmission
tetanus, intestinal worms
blood borne - modes of infectious transmission
HIV/AIDS, hepatitis C
droplet - modes of infectious transmission
pneumonia, flu, pertussis, TB, mumps, chickenpox
diet - modes of infectious transmission
e.coli
zoonosis - modes of infectious transmission
avian flu, swine flu
oral - modes of infectious transmission
choler, hepatits A, polio, rotavirus, salmonella
sexual contact - modes of infectious transmission
gonorrhea, herpes, chlamydia
vector - modes of infectious transmission
malaria, yellow fever
bites - modes of infectious transmission
bubonic plague, rabies, cat-scratch fever