A&P II Blood, lymphatic and Immunity Study Guide
5.0(1)
5.0(1)
New
Card Sorting
1/148
Study Analytics
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
149 Terms
1
New cards

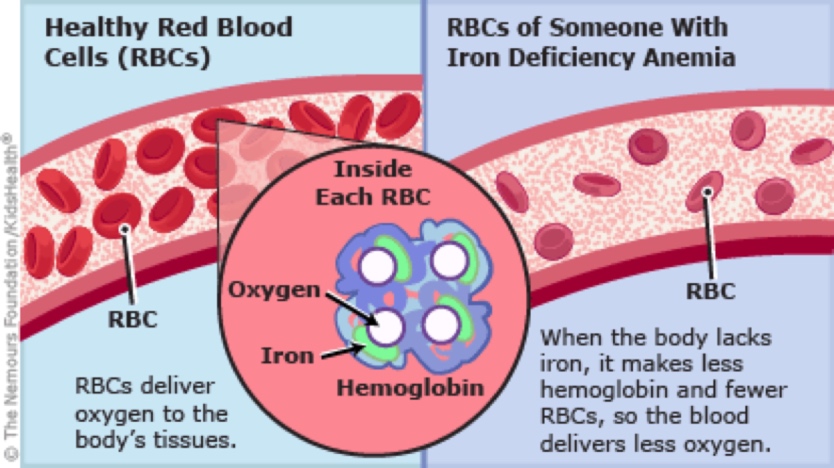
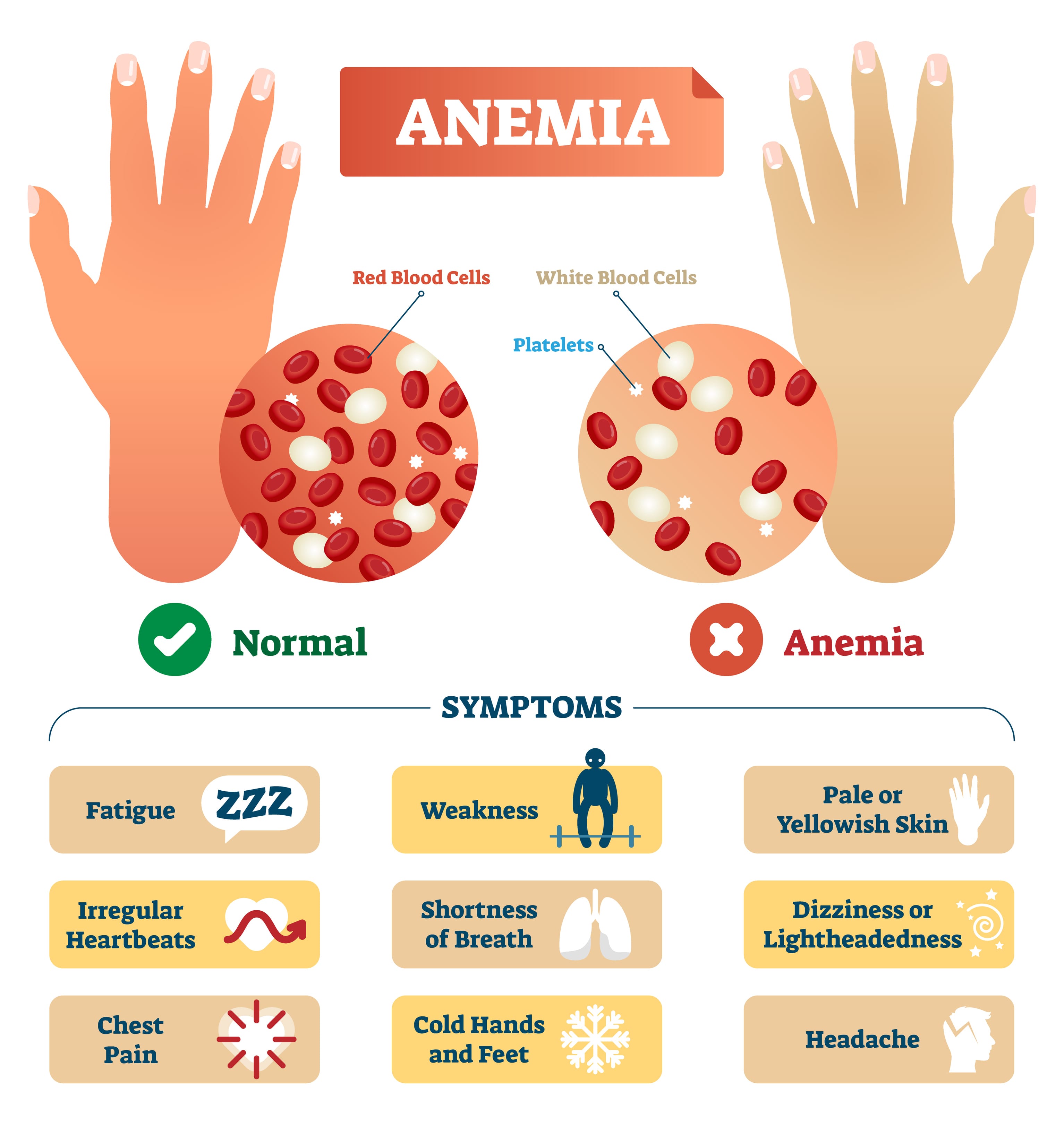
If an RBC is missing Fe++ (Iron), what **CANNOT** form correctly in the cell? How does this affect the RBC’s function?
1. Hemoglobin cannot form correctly in the RBC, if there is no Iron present.
2. Heme contains one Iron ion which is critical for binding O2, therefore the RBC won’t be able to transport O2, creating an Anemia specifically Iron deficiency Anemia.
2
New cards
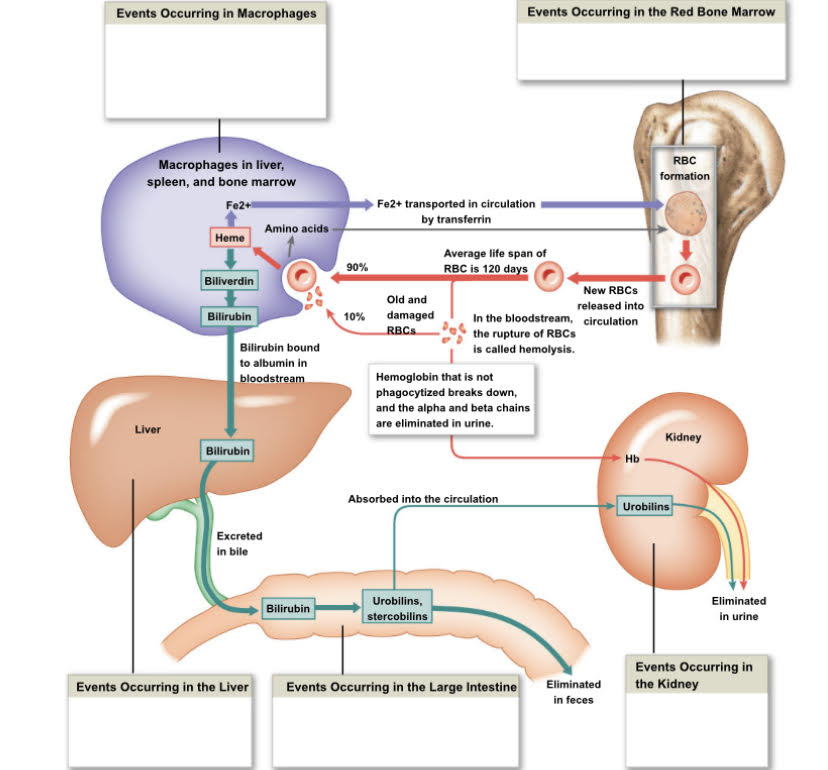
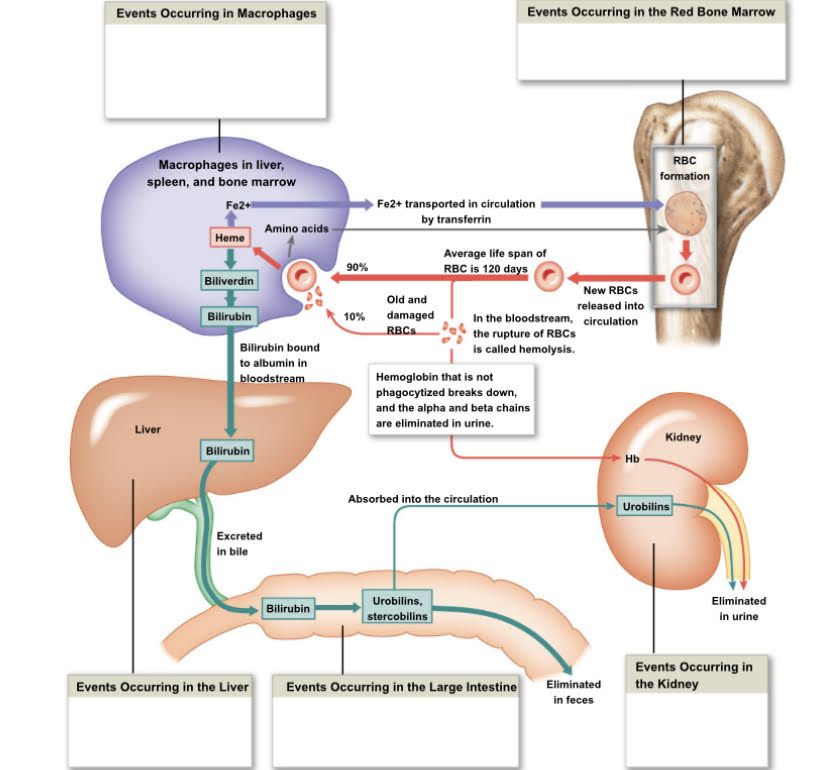
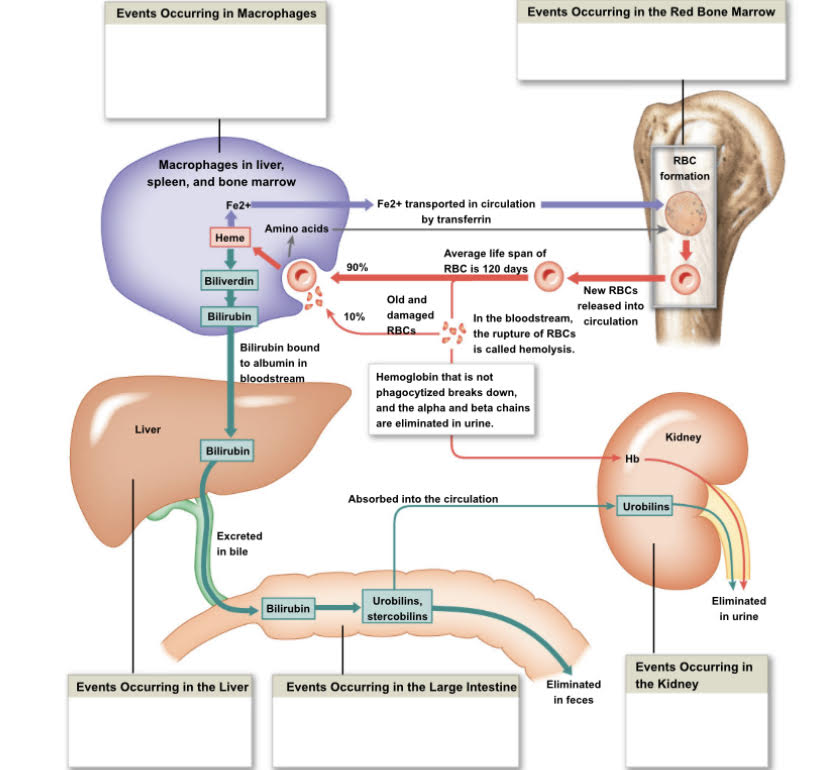
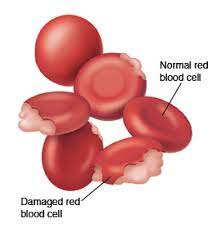
Describe how Old RBC’s are destroyed and recycled by the body?
1. Old damaged RBC’s are destroyed by being engulfed by a Macrophage that is found in the liver, spleen and bone marrow which breakdown into Amino acids and released back into the bloodstream
2. The RBC breaks down more to Heme and Fe++ (Iron)
1. The Iron is transported in Circulation by Transferrin back to the Red Bone Marrow to make more RBC’s which get released into circulation, repeating the cycle.
3. Heme is converted to Biliverdin
4. Biliverdin is converted to Bilirubin by the liver
1. The Bilirubin is then excreted in the bile then once in the Colon its converted to
1. Urobilins: absorbed into the circulation into the kidney eliminated in urine (makes it yellow)
2. Stercobilins: eliminated in feces
3
New cards
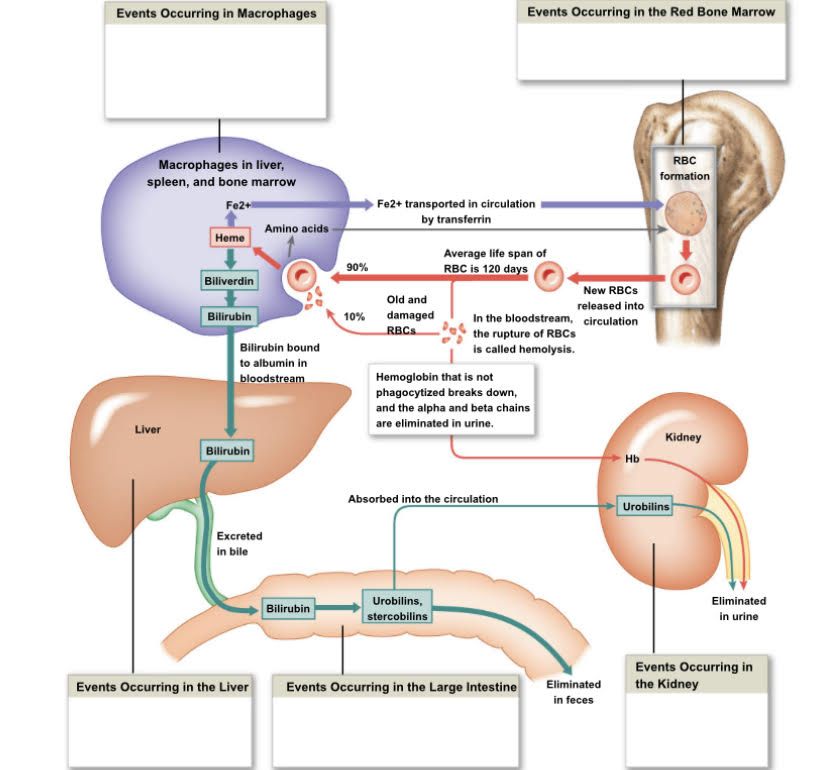
Where does Bilirubin come from?
Bilirubin comes from the breakdown of hemoglobin by a macrophage. Heme is broken down to biliverdin which is then broken down to Bilirubin.
4
New cards
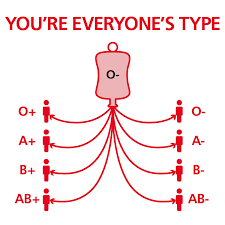
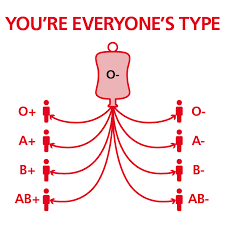
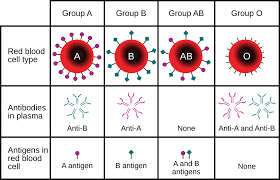
What is a universal donor?
Type O negative blood is a universal donor because you have neither A nor B antibodies. It has to be negative because if it is positive then it could cause a agglutinate reaction to those sensitized to rh positive which is bad or make that person sensitized to rh positive which is dangerous if exposed to it again.
5
New cards
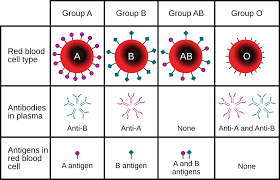
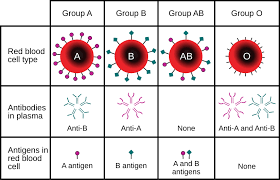
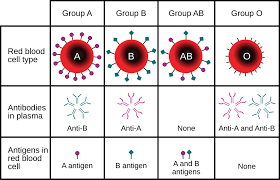
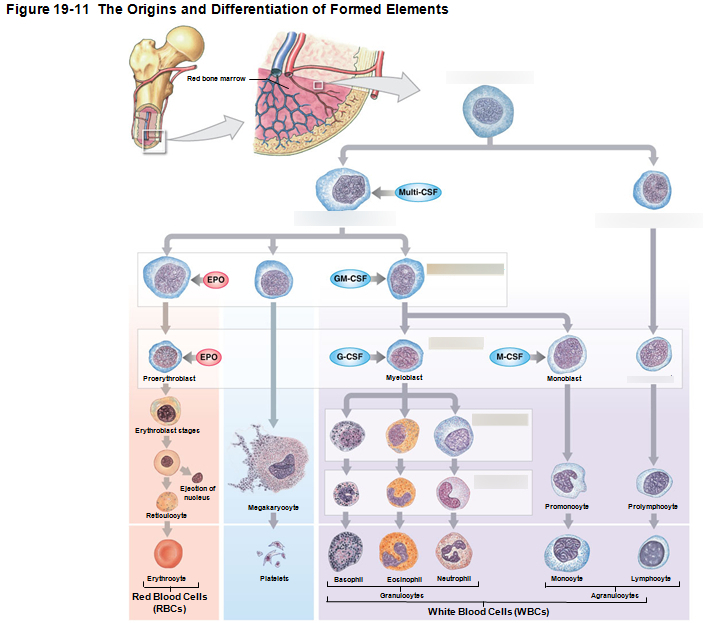
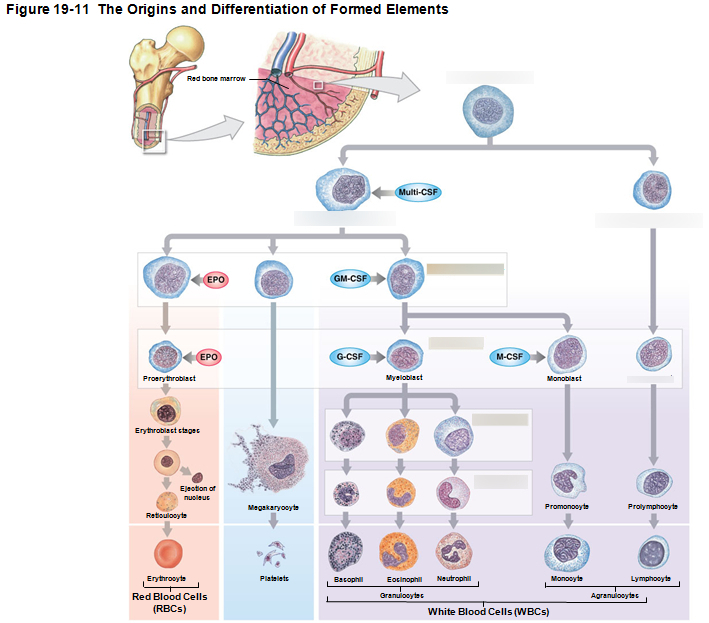
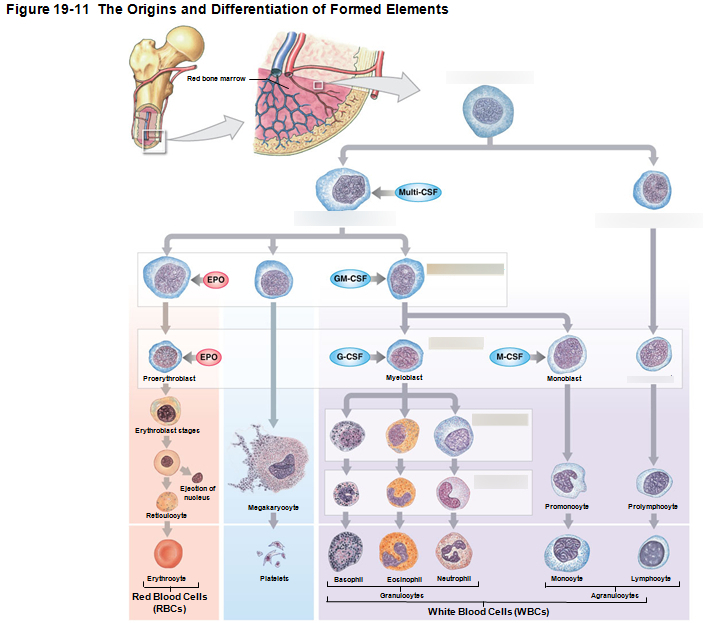
What are the four types of blood ?
1. Type A
1. Has type B antibodies
2. Type B
1. Has type A antibodies
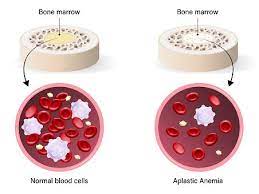
3. Type O
1. Has both A and B antibodies
4. Type AB
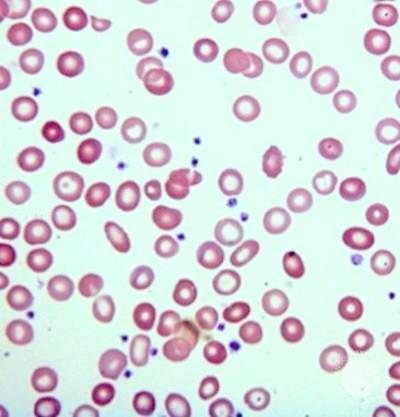
1. Has Neither A Nor B antibodies
6
New cards
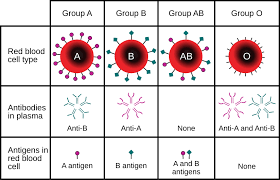
If type A blood, what antigens and antibodies does it posses?
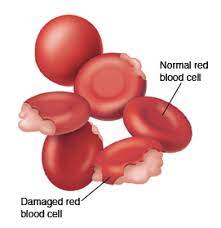
* Type A blood has RBC’s with surface antigen A only
* If you have Type A blood, your plasma contains anti-B antibodies, which will attack Type B surface antigens.
* If you get blood from Type B, it will attach to the anti-B antibodies you have and will cause an agglutinate (clot) reaction which you don’t want!
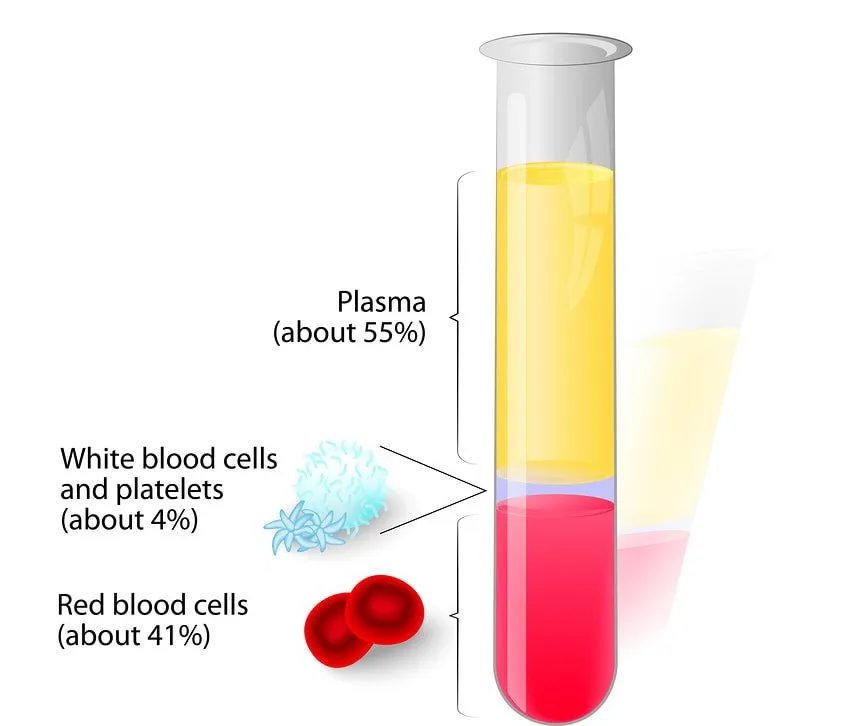
* If you have Type A blood, your plasma contains anti-B antibodies, which will attack Type B surface antigens.
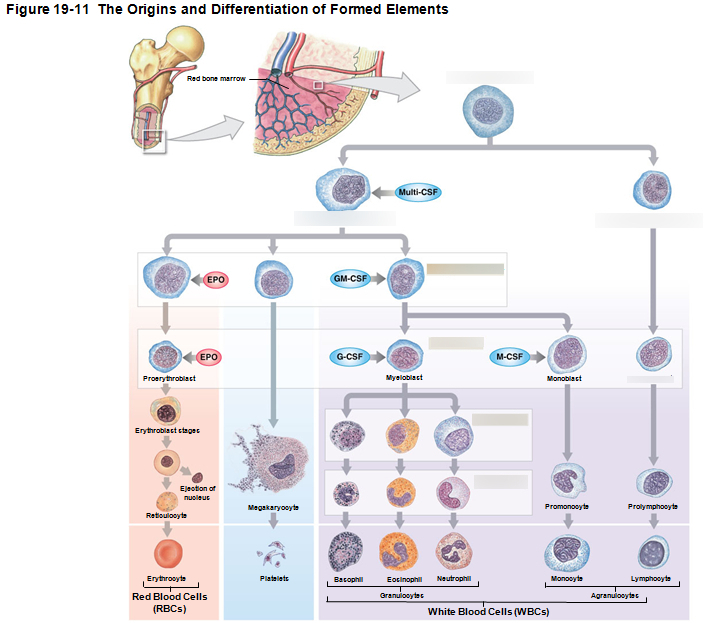
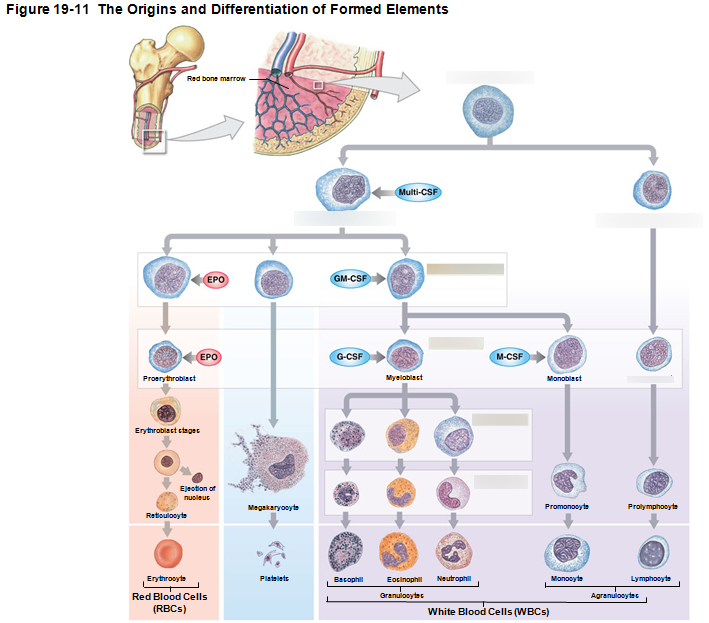
* If you get blood from Type B, it will attach to the anti-B antibodies you have and will cause an agglutinate (clot) reaction which you don’t want!
7
New cards
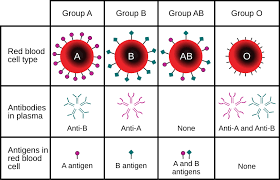
If type B blood, what antigens and antibodies does it posses?
* Type B blood has RBC’s with surface antigen B only
* If you have Type B blood, your plasma contains anti-A antibodies, which will attack Type B surface antigens.
* If you get blood from Type A, it will attach to the anti-A antibodies you have and will cause an agglutinate (clot) reaction which you don’t want!
* If you have Type B blood, your plasma contains anti-A antibodies, which will attack Type B surface antigens.
* If you get blood from Type A, it will attach to the anti-A antibodies you have and will cause an agglutinate (clot) reaction which you don’t want!
8
New cards
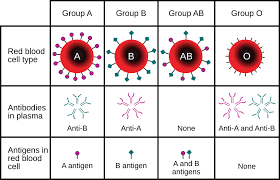
If type AB blood, what antigens and antibodies does it posses?
* Type AB blood has RBC’s with surface antigen A&B only
* If you have Type AB blood, your plasma contains no antibodies, If you did it would attack each others antigens.
\
* If you have Type AB blood, your plasma contains no antibodies, If you did it would attack each others antigens.
\
9
New cards
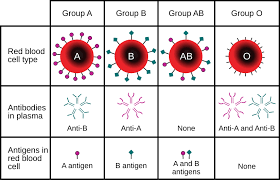
If type O blood, what antigens and antibodies does it posses?
* Type O blood has no antigens on its surface.
* If you have Type O blood, your plasma contains anti-A and anti-B antibodies.
\
* If you have Type O blood, your plasma contains anti-A and anti-B antibodies.
\
10
New cards
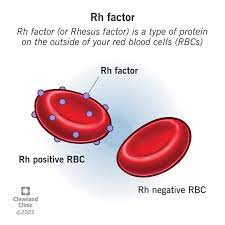
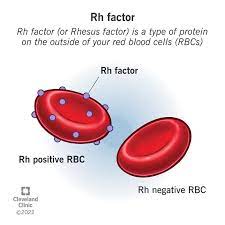
What does it mean when you are a positive or negative in your blood type?
* %%Positive%% means you %%posses%% the %%RH factor%% which does %%not produce%% the %%Rh antibodies%%
* ==Negative== means you ==Do Not Posses== the ==Rh== factor, However you ==do produce Rh antibodies.==
* ==Negative== means you ==Do Not Posses== the ==Rh== factor, However you ==do produce Rh antibodies.==
11
New cards
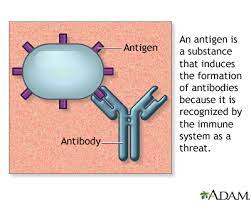
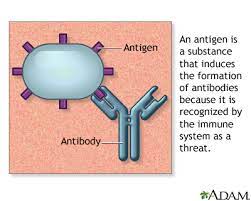
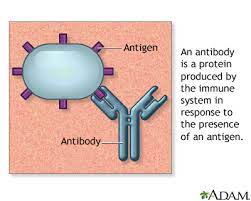
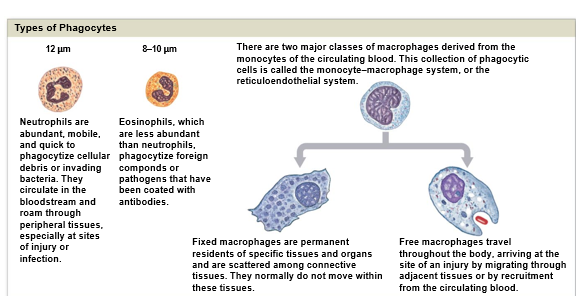
What is an Antigen?
* Anti stands for antibody and gen stands for genesis(creation of).
* In other words antibody generator
* In other words antibody generator
12
New cards
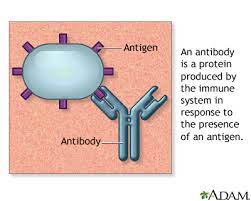
What is an Antibody?
Antibody is what is produced in response for a specific antigen to bind to. That antigen being something foreign that is Not suppose to be there. If an antibody binds to an Antigen that was suppose to be there, that would be an autoimmune disease. (body attacking itself)
13
New cards
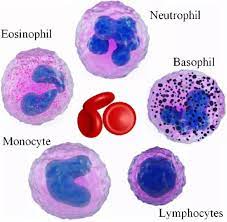
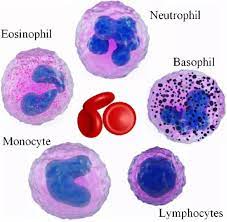
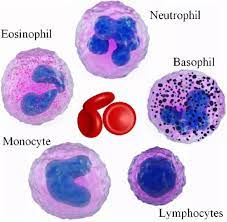
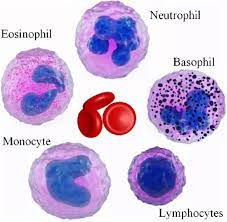
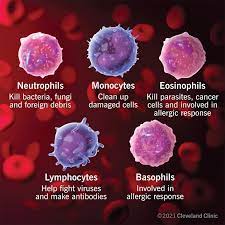
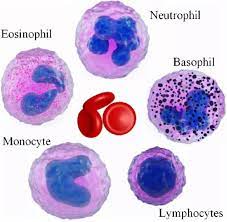
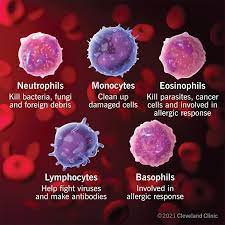
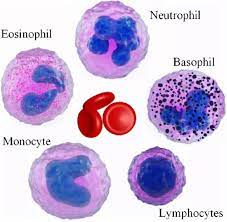
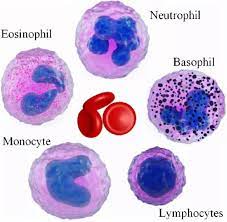
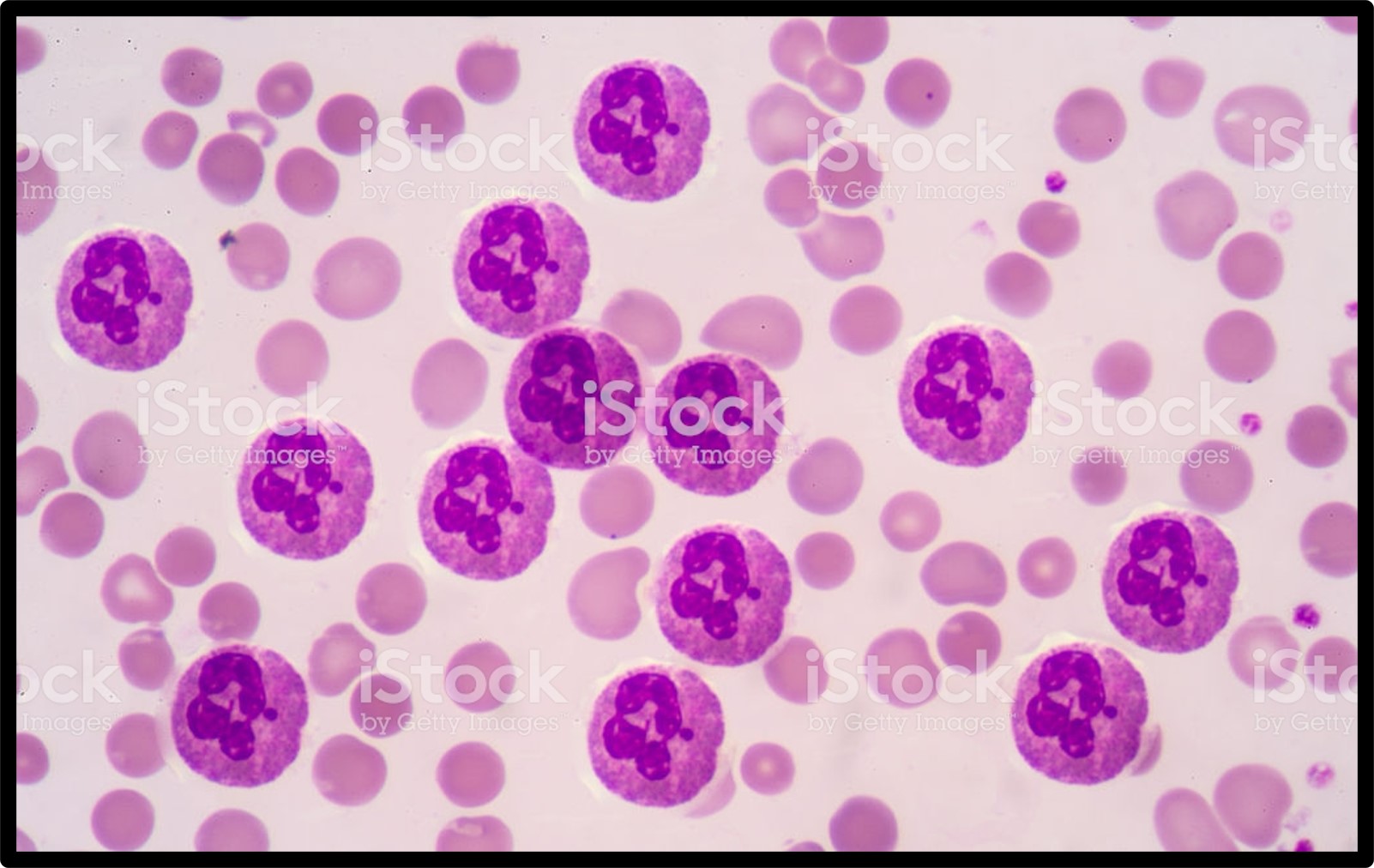
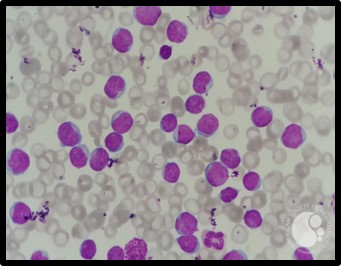
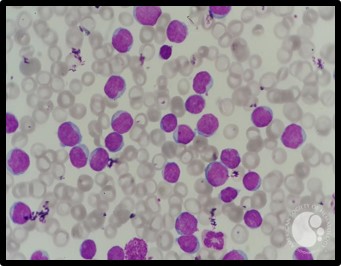
What are the five types of leukocytes(WBC’s)?
1. Neutrophils (55-70%)
2. Lymphocytes (20-40%)
3. Monocytes (2-8%)
4. Eosinophils (1-4%)
5. Basophils (.5-1%)
14
New cards
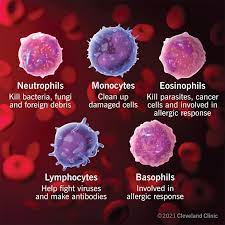
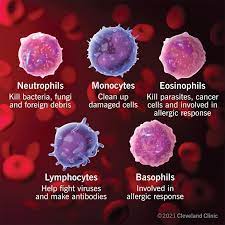
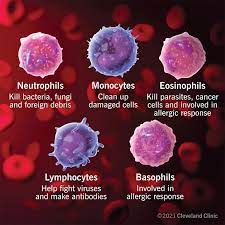
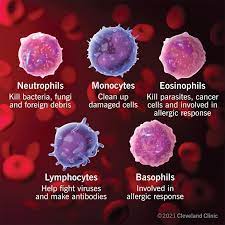
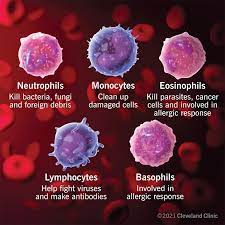
What is the Function of a Neutrophil?
* The first to attack in a bacterial infection
* They engulf and digest pathogens(which is the process of phagocytosis)
* Do this by the process of **Degranulation**
* They release %%Prostaglandins%% and %%leukotrienes%% (to help mediate the inflammation response which can do many things such as speed up replication of WBC’s , attract other WBC’s to the area to get the infection under control)
* When Neutrophils eat the pathogens and eat the cell debris they will start to die creating **Pus**
* They engulf and digest pathogens(which is the process of phagocytosis)
* Do this by the process of **Degranulation**
* They release %%Prostaglandins%% and %%leukotrienes%% (to help mediate the inflammation response which can do many things such as speed up replication of WBC’s , attract other WBC’s to the area to get the infection under control)
* When Neutrophils eat the pathogens and eat the cell debris they will start to die creating **Pus**
15
New cards
A high Neutrophil count indicates what?
Indicates there is a bacterial infection.
16
New cards
What is Degranulation?
* Removes granules from cytoplasm
* Defensins (peptides from lysosomes) attack pathogen membranes
* Defensins (peptides from lysosomes) attack pathogen membranes
17
New cards
What is Pus?
* An accumulation of dead neutrophils, dead bacteria and tissues.
* They’ve eaten the bad guy and do degranulation by releasing a toxic chemical inside the cell, not only does it kill the microbe it, it kills the cell(WBC) too which forms the pus.
* They’ve eaten the bad guy and do degranulation by releasing a toxic chemical inside the cell, not only does it kill the microbe it, it kills the cell(WBC) too which forms the pus.
18
New cards
What is the function of an Eosinophil?
* Attacks large parasites(worms)
* Does this by Excreting toxic compounds such as Nitric Oxide and Cytotoxic enzymes
* Controls Inflammations with enzymes that reduce inflammatory effects of neutrophils and mast cells
* Produces anti-histamine to control that inflammatory response
\
* Does this by Excreting toxic compounds such as Nitric Oxide and Cytotoxic enzymes
* Controls Inflammations with enzymes that reduce inflammatory effects of neutrophils and mast cells
* Produces anti-histamine to control that inflammatory response
\
19
New cards
A high Eosinophil count indicates what?
Indicates worm infections, autoimmune and allergic diseases
20
New cards
What is the function of a Basophil?
* Involved in the inflammatory response
* Releases Histamine
* Dilates blood vessels(vasodilation) which increases capillary permeability causing them to be leaky and cause swelling, hives etc.
* Releases Heparin
* Prevents blood clotting
* Releases Histamine
* Dilates blood vessels(vasodilation) which increases capillary permeability causing them to be leaky and cause swelling, hives etc.
* Releases Heparin
* Prevents blood clotting
21
New cards
A high count of Basophils indicate what?
Indicates autoimmune inflammatory
22
New cards
What is the function of Monocytes?
* Eats viruses and bacteria. Therefore increases in numbers during viral and bacterial infections.
* Secretes substances that attract immune system cells and fibrocytes to the injured area.
* Secretes substances that attract immune system cells and fibrocytes to the injured area.
23
New cards
A high count of Monocytes indicates what?
Indicates Mononucleosis which is a viral infection
24
New cards
What is the function of Lymphocytes?
* Part of the body’s specific defense system (Immunity) that help fight bacteria and make antibodies
* T-cells destroy bacteria
* B-cells make antibodies to bind to that foreign antigen preventing it from getting in our system.
* T-cells destroy bacteria
* B-cells make antibodies to bind to that foreign antigen preventing it from getting in our system.
25
New cards
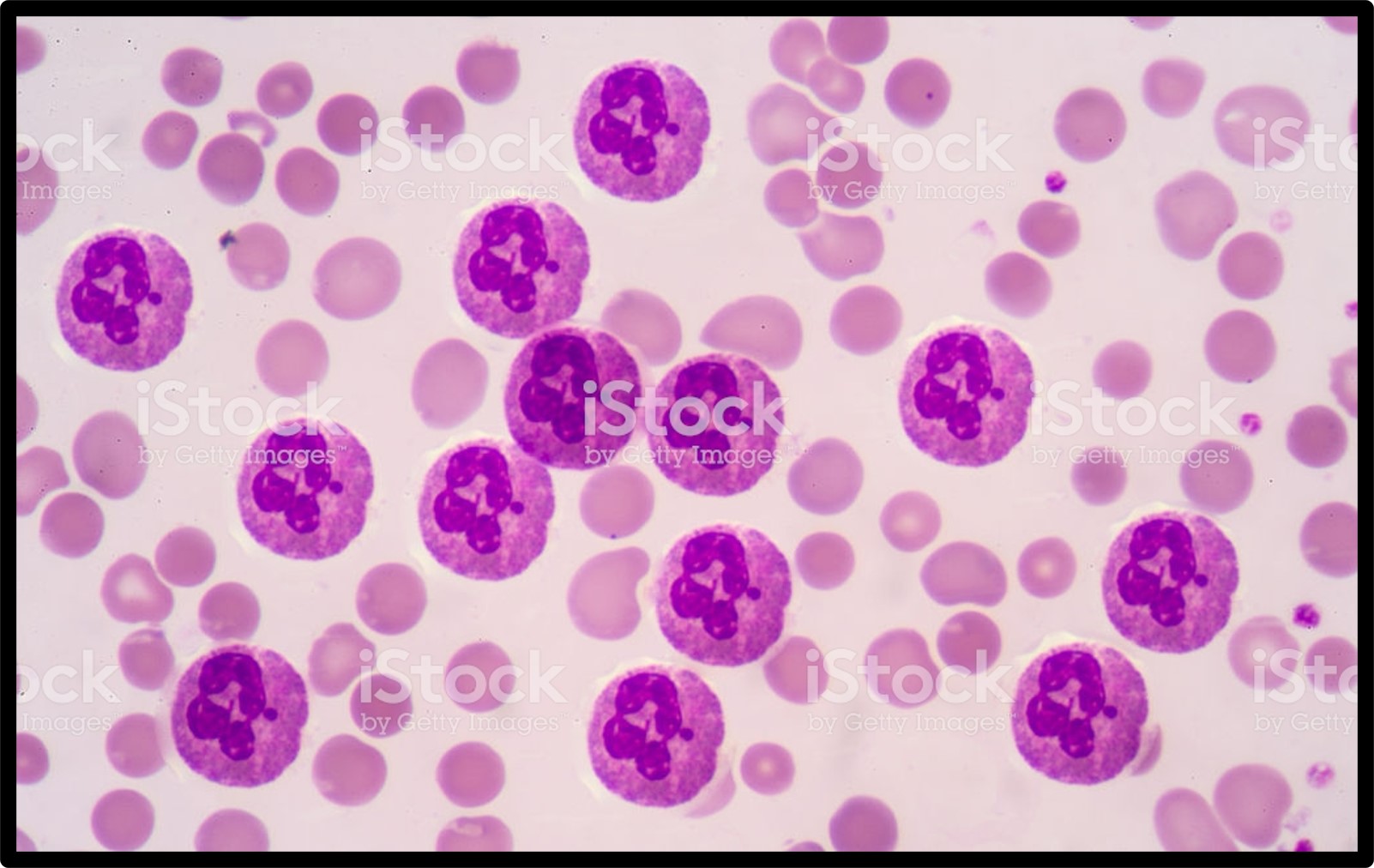
A high count of lymphocytes indicates what?
Indicates leukemia
26
New cards
What are the steps in Blood clot formation?
1. Vascular Phase (happens in the blood vessel)
2. Platelet Phase (forms platelet plug)
3. Coagulation Phase (converts fibrinogen to Fibrin so RBC can stick to it)
27
New cards
Describe the Vascular phase of blood clot formation?
When we cut it open, the Endothelial cells will contract, remember the Endothelial lining is Inside and that smooth lining ensures that RBC’s don’t stick to it, but we want those RBC’s to stick bc we want them to CLOT!
* Therefore, Endothelial cells contract(vasoconstriction) and expose basement membrane to bloodstream so it can stick and clot!
* Endothelial cells release some clotting factors that’s going to initiates that repair work we want, releasing ADP, tissue factor and Prostacyclin
* Also releases Endothelins which stimulate smooth muscle contraction and cell division (vasoconstriction)
* Which endothelial plasma membrane becomes sticky and seals off blood flow
* Therefore, Endothelial cells contract(vasoconstriction) and expose basement membrane to bloodstream so it can stick and clot!
* Endothelial cells release some clotting factors that’s going to initiates that repair work we want, releasing ADP, tissue factor and Prostacyclin
* Also releases Endothelins which stimulate smooth muscle contraction and cell division (vasoconstriction)
* Which endothelial plasma membrane becomes sticky and seals off blood flow
28
New cards
Describe the Platelet phase of blood clot formation
Begins 15 seconds after injury.
* The platelet phase of hemostasis begins with the attachment of platelets to sticky surfaces, to the basement membrane, to exposed collagen fibers, and to each other. As they become activated, platelets release a variety of chemicals that promote aggregation, vascular spasm, clotting and vessel repair.
* The chemicals released are
* ADP (Adenosine diphosphate)
* Thromboxane A2 and serotonin
* Clotting factors
* Platelet derived growth factor (PDGF)
* Calcium Ions
* The platelet phase of hemostasis begins with the attachment of platelets to sticky surfaces, to the basement membrane, to exposed collagen fibers, and to each other. As they become activated, platelets release a variety of chemicals that promote aggregation, vascular spasm, clotting and vessel repair.
* The chemicals released are
* ADP (Adenosine diphosphate)
* Thromboxane A2 and serotonin
* Clotting factors
* Platelet derived growth factor (PDGF)
* Calcium Ions
29
New cards
What is the danger that comes with the Positive feedback mechanism with the Platelet phase?
The initiation of clotting, stimulates more stuff leading to more aggregation, however, since it is Positive feedback there is a danger that the cycle will continue all the way to your Cardiovascular system. Thus, clotting all of your blood in all of your vessels, bc they are all connected. Which we don’t want!
30
New cards
Describe the Coagulation phase of blood clot formation
Begins 30 seconds or more after the injury
Coagulation, or blood clotting, involves a complex sequence of steps (cascade reactions) of enzymes and proenzymes that form three pathways leading to the conversion of circulating fibrinogen into the insoluble protein fibrin. As the fibrin network grows, blood cells and additional platelets are trapped in the fibrous tangle, forming a blood clot that seals off the damaged portion of the vessel
Coagulation, or blood clotting, involves a complex sequence of steps (cascade reactions) of enzymes and proenzymes that form three pathways leading to the conversion of circulating fibrinogen into the insoluble protein fibrin. As the fibrin network grows, blood cells and additional platelets are trapped in the fibrous tangle, forming a blood clot that seals off the damaged portion of the vessel
31
New cards
What are the three pathways of the Coagulation phase of the blood clot formation?
1. Extrinsic pathway
2. Intrinsic pathway
3. Common pathway
32
New cards
Describe the Extrinsic pathway of the coagulation phase of blood clot formation.
* Begins in the vessel wall and can Occur outside the bloodstream when the vessel has been at the exposure to collagen fibers can help activate it.
* The damaged cells release tissue factor (TF) which helps start the cascade
* TF + other compounds = enzyme complex that…
* Activates Factor X (where Common Pathway starts)
* The damaged cells release tissue factor (TF) which helps start the cascade
* TF + other compounds = enzyme complex that…
* Activates Factor X (where Common Pathway starts)
33
New cards
Describe the Intrinsic pathway of the coagulation phase of blood clot formation.
Begins with circulating Proenzymes within bloodstream(inside the vessel)
Activation of enzymes by collagen fibers being exposed
The platelets will release factors (PF-3) which helps activate the clotting mechanism
Thus, the series of reactions activates Factor X (Common Pathway Starts)
Activation of enzymes by collagen fibers being exposed
The platelets will release factors (PF-3) which helps activate the clotting mechanism
Thus, the series of reactions activates Factor X (Common Pathway Starts)
34
New cards
Describe the Common pathway of the coagulation phase of blood clot formation.
Starts at Factor X (need common pathway to clot!)
Where the intrinsic and extrinsic pathways converge (meet) and forms enzyme Prothrombinase that converts prothrombin to thrombin and thrombin converts fibrinogen to fibrin which forms blood clot.
Where the intrinsic and extrinsic pathways converge (meet) and forms enzyme Prothrombinase that converts prothrombin to thrombin and thrombin converts fibrinogen to fibrin which forms blood clot.
35
New cards
What are the ways in which loss of blood is prevented?
1. Prostacyclin released by endothelial cells inhibits platelet aggregation (prevents clotting everywhere)
2. Inhibitory compounds released by other WBC’s
1. Chemicals have been released from this damaged tissue that are going to draw WBC’s to the area bc there could be Pathogen invasion and we have damaged tissue that needs to be engulfed (macrophage) and gotten rid of.
3. Circulating enzymes breakdown ADP (which is a clotting compound)
4. Negative (inhibitory) feedback form serotonin
1. The clot formation itself is positive feedback but we don’t want the clotting to go any further than the damaged area therefore, we initiate a Negative feedback from Serotonin
5. Development of blood clot isolates the area
36
New cards
Why is Iron important in RBC’s ?
Iron is needed to make hemoglobin. Hemoglobin requires iron which is critical for binding to O2 and transporting O2 to other areas in the body. Without iron there is no RBC’s and if there is no RBC’s we will be dead .
37
New cards
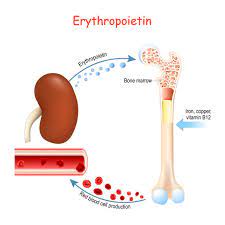
What is Erythropoietin and what does it do?
* a.k.a. Erythropoiesis stimulating hormone
* Hormone secreted by the kidneys and released when the body is in a hypoxic (low O2) state. It stimulates the production of RBC’s .
* Occurs only in Myeloid tissue(Red Bone Marrow) in adults , the stem cells mature to become RBC’s
* \
* Hormone secreted by the kidneys and released when the body is in a hypoxic (low O2) state. It stimulates the production of RBC’s .
* Occurs only in Myeloid tissue(Red Bone Marrow) in adults , the stem cells mature to become RBC’s
* \
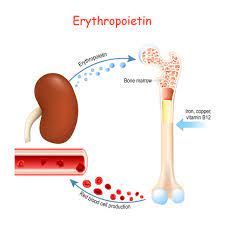
38
New cards
how does high altitude make humans secrete EPO?
Gases move by pressure gradients. Pressure is low on a mountain which can’t move the gas into you which puts you into a state of Hypoxia which stimulates you to release EPO increasing RBC and ability to transport more O2 giving you an advantage if doing an endurance sport.
39
New cards
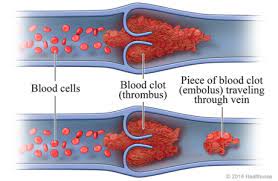
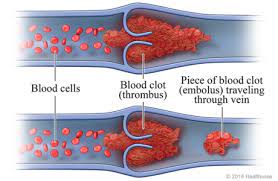
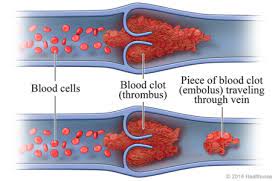
What is a thrombus?
A stationary clot that gets its name from thrombocyte(a.k.a. platelet which is a cell fragment involved in clotting)
40
New cards
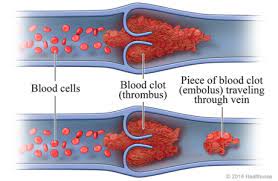
What is an embolus?
Circular clot which is very dangerous, more worse than a thrombus(stationary clot)
41
New cards
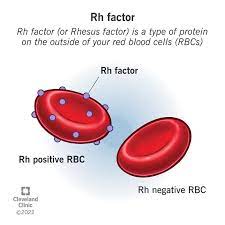
What is the Rh factor?
A.K.A. D Antigen
* If the Rh antigen is present you are Rh positive (Rh+)
* If the Rh antigen is absent you are Rh negative (Rh-)
* Only sensitized(exposed) Rh- blood has anti-Rh antibodies (only important when woman are pregnant, Rh- can cross the placenta)
* If the Rh antigen is present you are Rh positive (Rh+)
* If the Rh antigen is absent you are Rh negative (Rh-)
* Only sensitized(exposed) Rh- blood has anti-Rh antibodies (only important when woman are pregnant, Rh- can cross the placenta)
42
New cards
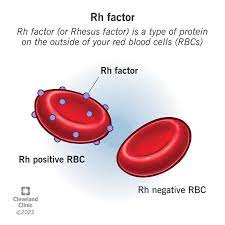
How do we produce Rh antibodies?
You do not produce the antibodies against an Rh antigen unless you are exposed(sensitized).
* Therefore, Rh+ you won’t make any antibodies because you have the Rh factor(antigen) you don’t want to attack yourself (autoimmune disease)
* If you are Rh- , you don’t have the Rh antibody until you’ve been exposed (sensitization).
* Therefore, Rh+ you won’t make any antibodies because you have the Rh factor(antigen) you don’t want to attack yourself (autoimmune disease)
* If you are Rh- , you don’t have the Rh antibody until you’ve been exposed (sensitization).
43
New cards
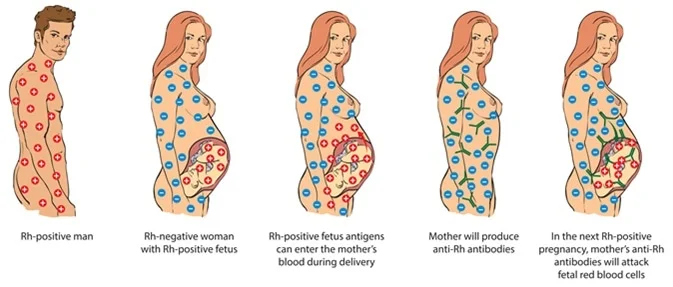
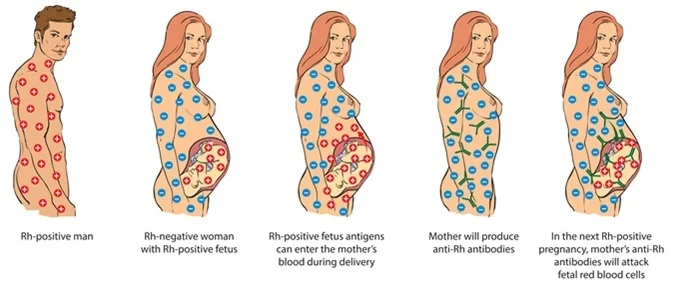
Why is sensitized Rh- blood important to woman who are pregnant?
If mom is Rh-, and the baby is Rh- there is no problem. However, if Dad is Rh+ making the baby Rh+, if the placenta tears and Mom and the baby’s blood mixes. This exposes(sensitized) Mom to Rh+ , thus making antibodies against it.
Furthermore, if the 2nd baby comes and is also Rh+, Mom has made the antibodies against Rh+ from the 1st baby and will attack the 2nd baby’s blood which is called hemolytic syndrome of newborns.
Furthermore, if the 2nd baby comes and is also Rh+, Mom has made the antibodies against Rh+ from the 1st baby and will attack the 2nd baby’s blood which is called hemolytic syndrome of newborns.
44
New cards
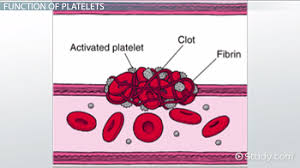
What is the function of platelets?
1. Releases important clotting chemicals (fibrinogen)
1. The forms from fibrinogen. Fibrinogen is the dissolved form of Fibrin that circulates in your blood.
1. When blood isn’t forming a clot the fiber isn’t solid, its dissolved as fibrinogen and circulates so with the help of platelets releasing these clotting initiations it will go through its formation and become a solid structure
2. Temporarily patch damaged vessel walls (only small damages won’t be able to patch major arteries or big lacerations)
3. Reduces the size of a break in a vessel wall

45
New cards
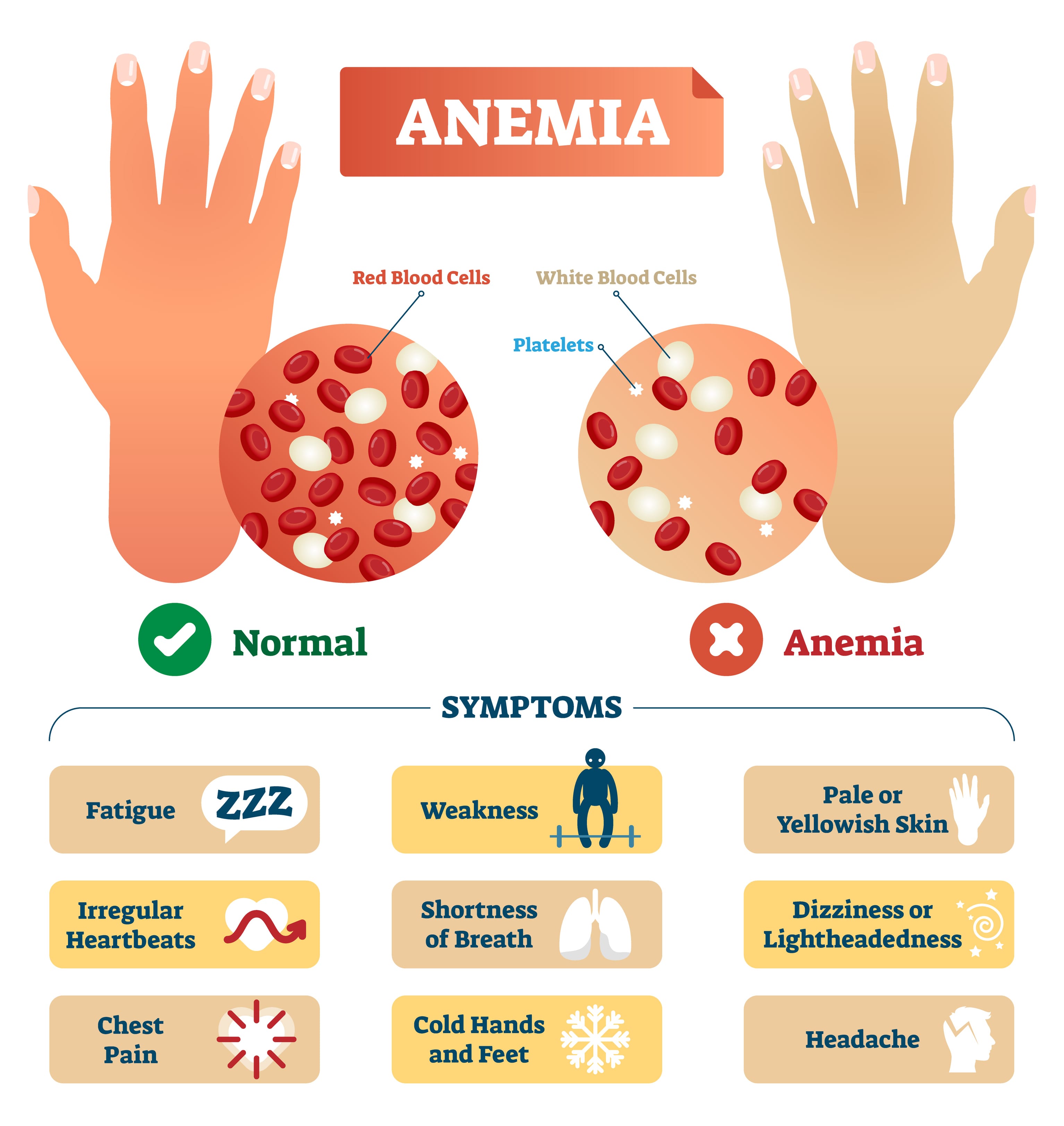
What is anemia?
Reduced O2 carrying capacity of the blood
46
New cards
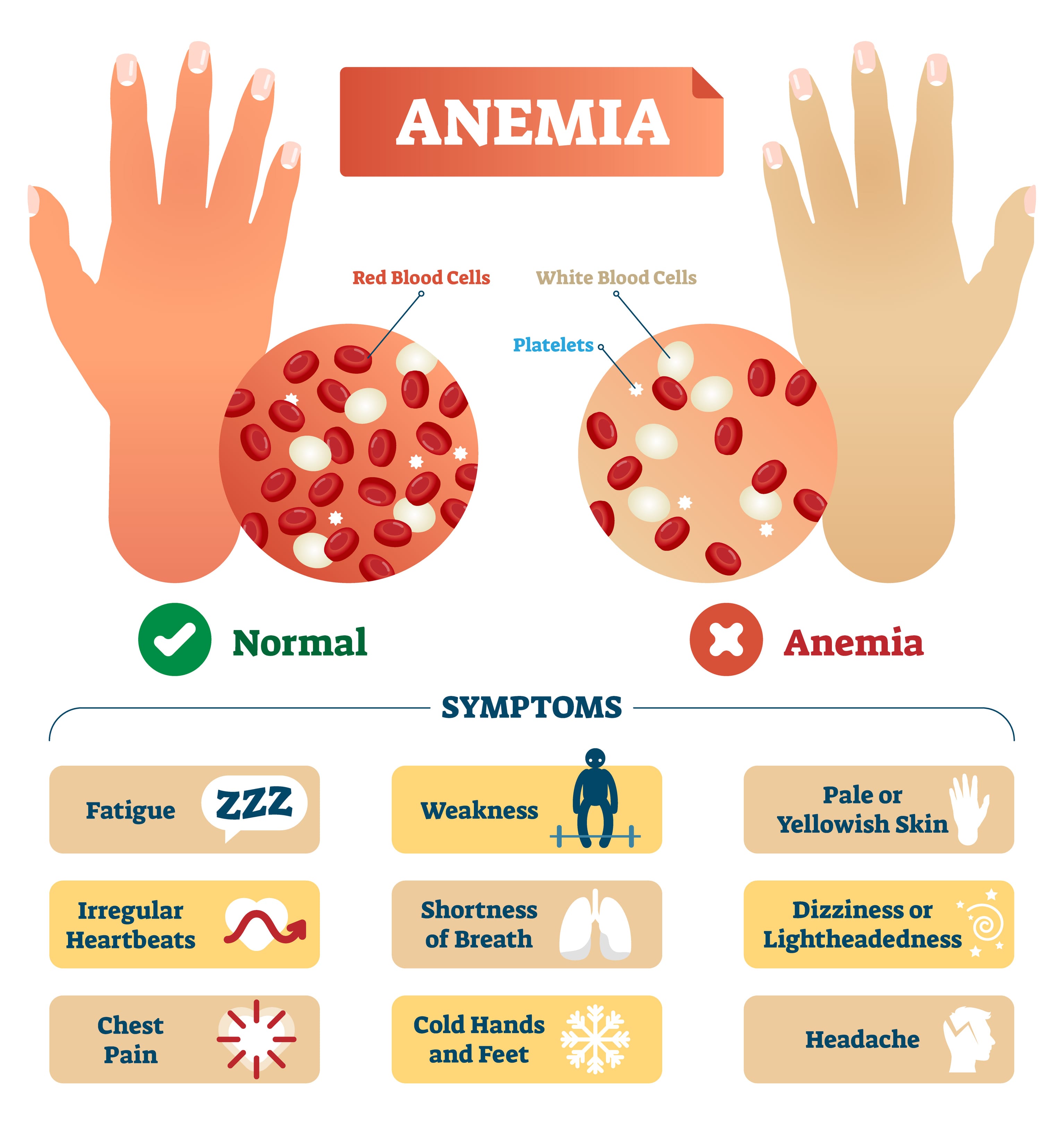
Explain why iron deficiency can lead to anemia?
The lack of Iron means there is a lack of hemoglobin, you can’t make hemoglobin without iron which means you will have Iron deficiency anemia.
(if hemoglobin deficient then you won’t be able to transfer O2, which causes many problems including death)
(if hemoglobin deficient then you won’t be able to transfer O2, which causes many problems including death)
47
New cards
What is aplastic anemia ?
Ex: Aids (worst anemia!). Caused by toxic chemicals, radiation. Damages Bone marrow (without stem cells there will be no blood cells)
48
New cards
What is Hemolytic anemia?
* RBC’s lysing
* Caused by toxic chemicals
* Can happen with Chemotherapy.
* Chemotherapy drugs target any cells that are actively dividing, But your Red Bone Marrow is dividing which will drop your blood count. Red bone marrow is your stem cells which is crucial for production of blood cells.
* Caused by toxic chemicals
* Can happen with Chemotherapy.
* Chemotherapy drugs target any cells that are actively dividing, But your Red Bone Marrow is dividing which will drop your blood count. Red bone marrow is your stem cells which is crucial for production of blood cells.
49
New cards
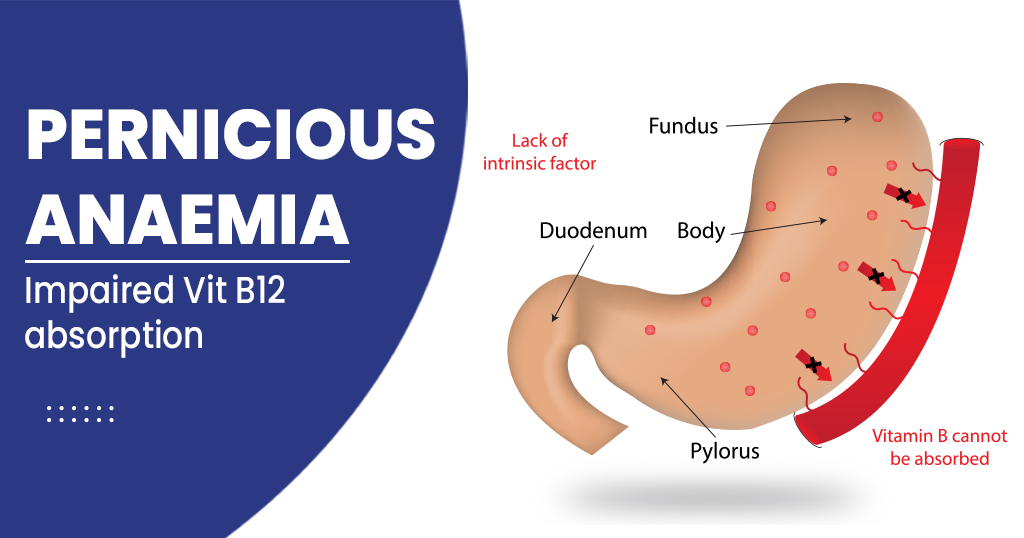
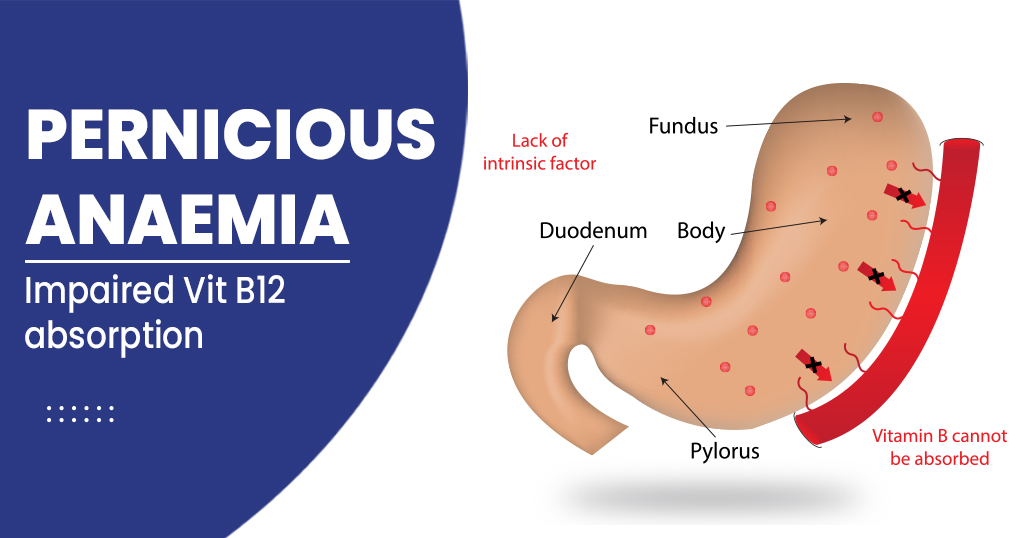
What is Pernicious Anemia?
The inability to absorb vitamin B12 leading to excess of immature cells bc of lack of intrinsic factor. To fix this, you’re able to get injections of B12.
50
New cards
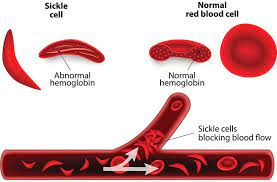
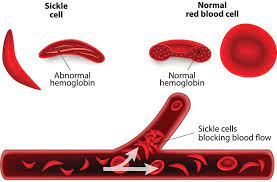
What is Sickle cell disease ?
Defective gene, meaning you are born this way. RBC’s are abnormally shaped causing the macrophage to think the RBC is an old damaged one and eats/engulfs the RBC, thus getting rid of it causing anemia.
51
New cards
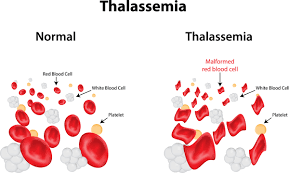
What is Thalassemia?
Defective gene, meaning you are born this way. You are hemoglobin deficient, Red blood cells short lived. This means RBC won’t be able to transfer O2.
52
New cards
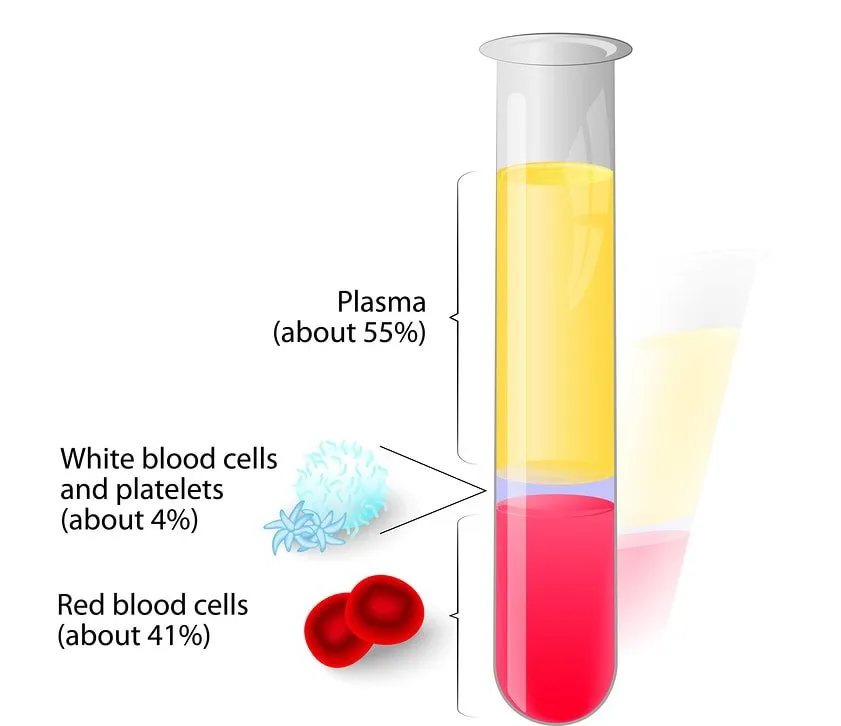
What is a hematocrit?
a.k.a. packed cell volume (PCV) percentage of RBC’s in centrifuged whole blood.
Male: 40-54
Female: 37-47
Male: 40-54
Female: 37-47
53
New cards
Describe a RBC.
Transports O2 and CO2 (if exposed to CO2 than transport that as well)
Derived from the Myeloid stem cell that’s derived from hemocytoblasts.
Derived from the Myeloid stem cell that’s derived from hemocytoblasts.
54
New cards
Describe a WBC.
Part of the immune system, fights infections, phagocytosis and makes antibodies.
Derived from Myeloid stem cells that’s derived from hemocytoblasts.
Lymphocytes are derived from lymphoid stem cells and also derived from hemocytoblasts.
Derived from Myeloid stem cells that’s derived from hemocytoblasts.
Lymphocytes are derived from lymphoid stem cells and also derived from hemocytoblasts.
55
New cards
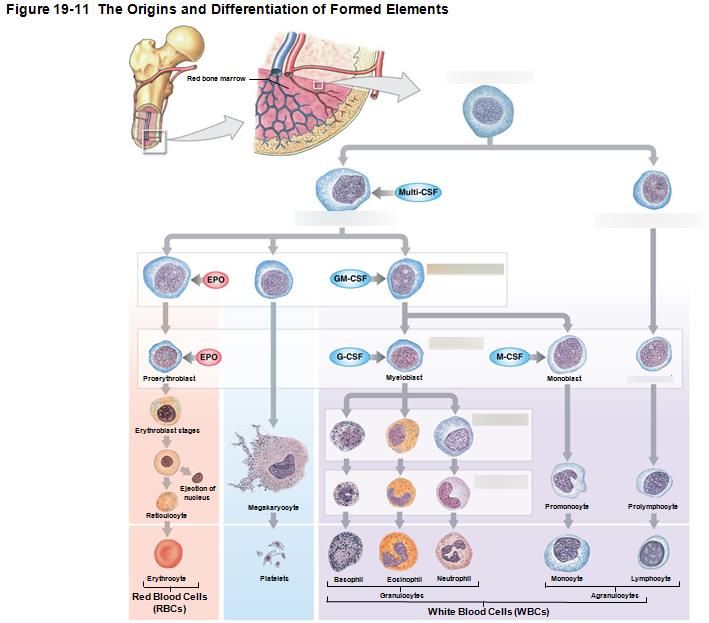
Describe a Platelet or thrombocyte(humans don’t have this)
Cell fragments involved in clotting. Animals that have thrombocyte have the complete cell and they have the same function, clotting.
Derived from Myeloid stem cells that’s also derived from hemocytoblasts.
Derived from Myeloid stem cells that’s also derived from hemocytoblasts.
56
New cards
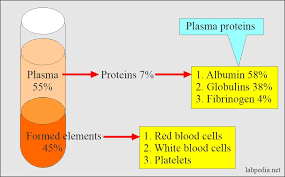
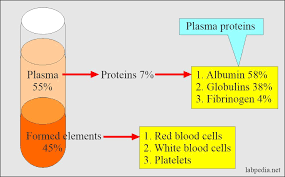
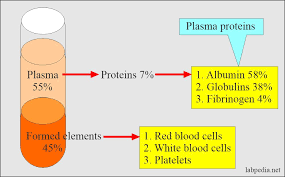
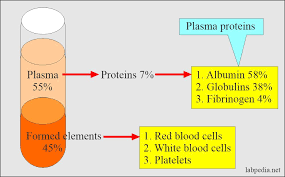
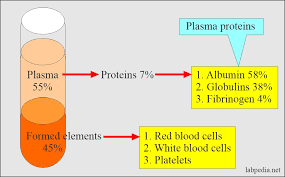
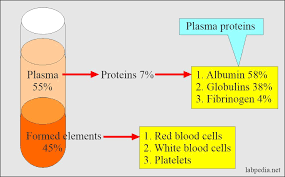
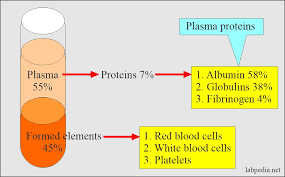
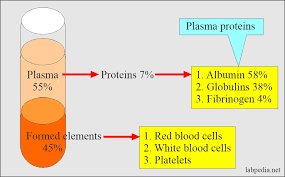
What are the three types of plasma proteins?
1. Albumins (54-60%)
2. Globulins (35-38%)
3. Fibrinogen (4-7%)
57
New cards
What is the function of the plasma protein, Albumin?
* Helps transport substances such as fatty acids, thyroid hormones and steroid hormones.
* Fats will float in water of bloodstream so Fats are attached to Albumin protein to stay in suspension and transported.
* Really large protein that is important to maintain osmotic pressure of blood.
* Fats will float in water of bloodstream so Fats are attached to Albumin protein to stay in suspension and transported.
* Really large protein that is important to maintain osmotic pressure of blood.
58
New cards
What is the function of plasma protein, Globulin?
Helps transport globulins(small molecules): hormone binding proteins, metalloproteins(transports metal ions), apolipoproteins(Transports fat proteins), and steroid binding proteins
A.K.A. antibodies called immunoglobulins(Globular protein for immunity)
A.K.A. antibodies called immunoglobulins(Globular protein for immunity)
59
New cards
What is the function of the plasma protein, Fibrinogen?
* Helps molecules that forms clots and produce long, insoluble strands of fibrin.
* Fibrinogen is dissolved in the plasma, when initiating the clotting mechanism, it turns to Fibrin and becomes solid at that point in time
* Fibrinogen is dissolved in the plasma, when initiating the clotting mechanism, it turns to Fibrin and becomes solid at that point in time
60
New cards
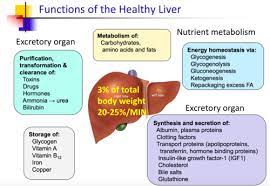
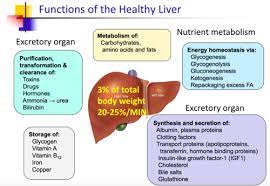
Where in the body are plasma proteins manufactured?
* More than 90% of plasma proteins are made in the **liver**.
* Antibodies(lymphocyte/B-cells) made by plasma cells
* Peptide hormones(doesn’t have many amino acids bonded) made by endocrine organs
* Antibodies(lymphocyte/B-cells) made by plasma cells
* Peptide hormones(doesn’t have many amino acids bonded) made by endocrine organs
61
New cards
Describe the steps of the clotting mechanism ending with firbin.
1. Cut through the artery or vein triggers the **Vascular phase** (vascular spasm) Endothelial cells contract and expose basement membrane to bloodstream, releasing clotting factors (ADP, tissue factor, Prostacyclin) which now endothelial plasma membranes become sticky sealing off blood flow.
2. The Platelet phase occurs first with **Platelet Adhesion**(attachment), attaches to sticky endothelial surfaces to basement membranes to exposed collagen fibers starting **Platelet Aggregation**. Platelets stick together forming a **Platelet plug** which closes small breaks.
3. After, in Cascade reactions, there are **2 pathways Extrinsic and Intrinsic** that both lead to the **3rd pathway which is the Common Pathway** that ends converting fibrinogen into insoluble fibrin, the **Coagulation Phase**.
1. **Extrinsic Pathway**
1. Begins in the vessel wall, damaged cells release tissue factor (TF) starts the cascade by TF + other compounds= enzyme complex that activates Factor X (common pathway)
2. **Intrinsic Pathway**
1. Begins with Circulating proenzymes within the bloodstream(blood vessel) activating enzymes by collagen fibers being exposed. Platelets releasing factors PF-3 that helps activate the clotting mechanism thus activating Factor X (common pathway)
3. **Common Pathway**
1. Starts at Factor X, forming enzyme **Prothrombinase** that converts **prothrombin** to **thrombin** thus converting thrombin to **fibrinogen** and fibrinogen to **Fibrin** forming a **clot**.
4. **Clot Retraction**
1. Pulls torn edges of vessel closer together, trying to make the wound smaller. Which makes it easier for fibrocytes, smooth muscle cells and endothelial cells to complete repairs.
62
New cards
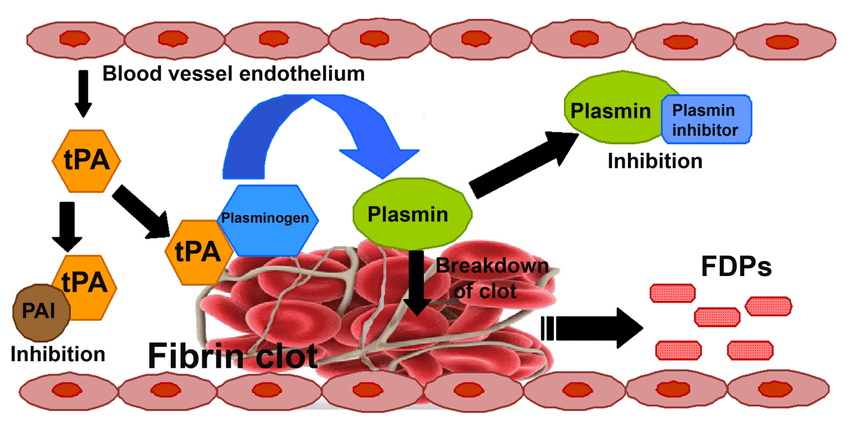
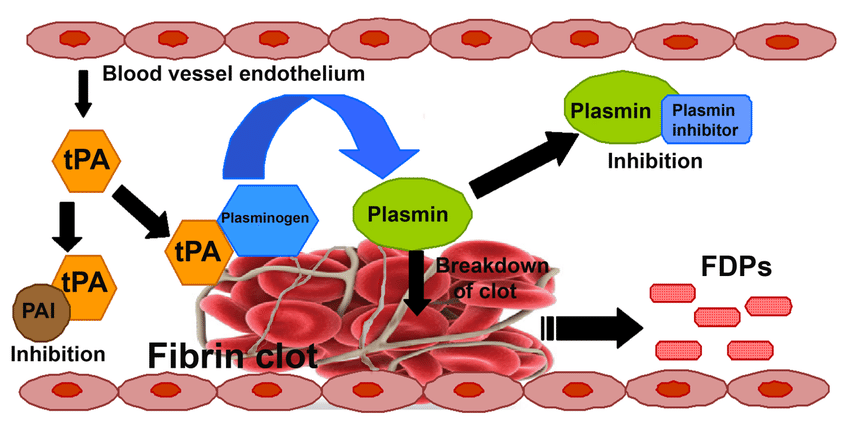
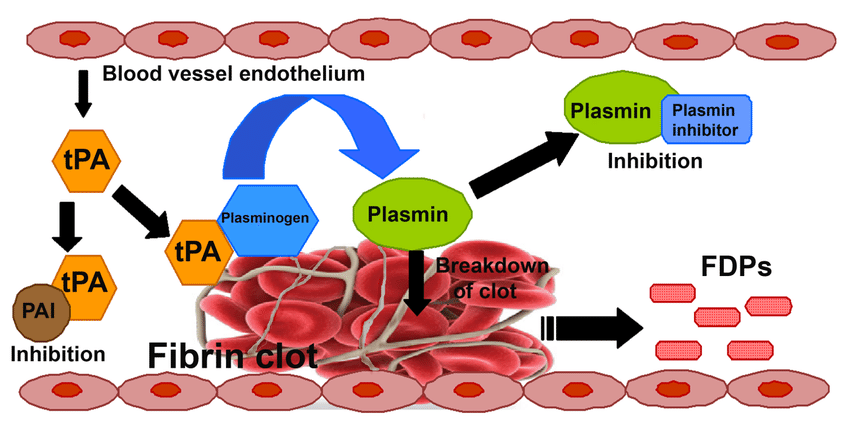
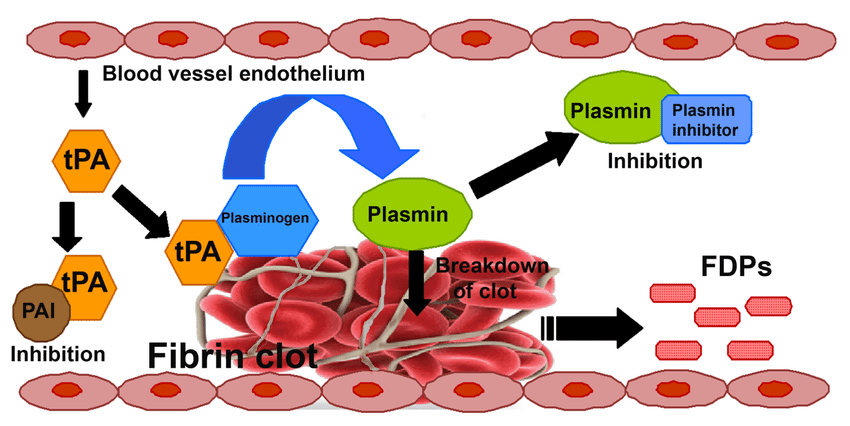
What is Fibrinolysis?
“Breakdown of fibers”
* Slow process of dissolving clot.
* Thrombin and tissue plasminogen activator (t-PA) which breaks/dissolves down clot activates plasminogen. Plasminogen will then produce Plasmin which gets rid of fibrin clots and digests fibrin strands.
* Slow process of dissolving clot.
* Thrombin and tissue plasminogen activator (t-PA) which breaks/dissolves down clot activates plasminogen. Plasminogen will then produce Plasmin which gets rid of fibrin clots and digests fibrin strands.
63
New cards
How will the scab/clots go away?
Through the process of fibrinolysis we do not need to pick the scab , it will breakdown on its own. Technically, we have scabs and clots inside the body, when we get a bruise you’ve damaged a bunch of blood vessels that leaked blood into the surrounding tissue and the clotting reaction occurs to block all those off, you’ve got clots everywhere within that bruise which need to be broken down thus going through fibrinolysis.
64
New cards
What is Hemostasis?
The cessation of bleeding, meaning trying to help us maintain homeostasis by stopping you from losing too much blood.
65
New cards
What triggers a platelet plug formation?
The exposed basement membrane, basil lamina and collagen fibers will cause the endothelial cells to become sticky(platelet adhesion) and adhere to platelets and each other forming the platelet plug(platelet aggregation)
66
New cards
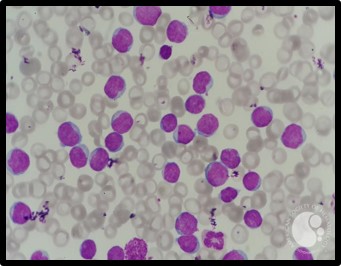
Give a description of a Neutrophil
* Polymorphonuclear (nucleus has many lobes)
* Has Granulocytes
* Phagocytic
* Constitutes 50-70% of circulating WBC’s
* Has Pale cytoplasm granules contain
* Lysosomal enzymes (to destroy ingested pathogens)
* Bactericides (hydrogen peroxide and superoxide)
* Engulfs and digests pathogens (phagocytosis)
* Has Granulocytes
* Phagocytic
* Constitutes 50-70% of circulating WBC’s
* Has Pale cytoplasm granules contain
* Lysosomal enzymes (to destroy ingested pathogens)
* Bactericides (hydrogen peroxide and superoxide)
* Engulfs and digests pathogens (phagocytosis)

67
New cards
Give a description of a Eosinophil.
* Polymorphonuclear (Bi-lobed)
* Contains Granulocytes
* The granules stain orange/reddish color
* 2-4% of circulating WBC’s
* Attacks large parasites(worms) and controls inflammation with enzymes that reduce inflammatory effects.
* Contains Granulocytes
* The granules stain orange/reddish color
* 2-4% of circulating WBC’s
* Attacks large parasites(worms) and controls inflammation with enzymes that reduce inflammatory effects.
68
New cards
Give a description of a Basophil.
* Polymorphonuclear
* Contains Granulocytes
* Granules stain dark/purple
* .5-1% of circulating WBC’s (least amount)
* Release histamine which dilates blood vessels and releases Heparin which prevents blood clotting
* Contains Granulocytes
* Granules stain dark/purple
* .5-1% of circulating WBC’s (least amount)
* Release histamine which dilates blood vessels and releases Heparin which prevents blood clotting
69
New cards
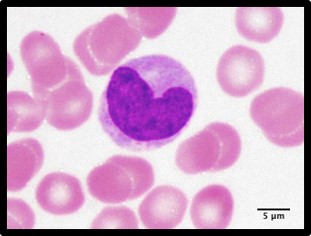
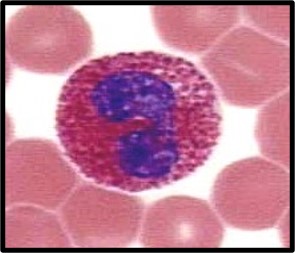
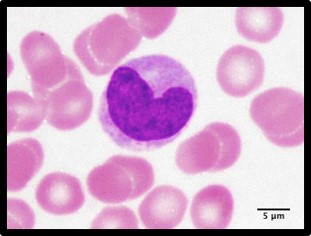
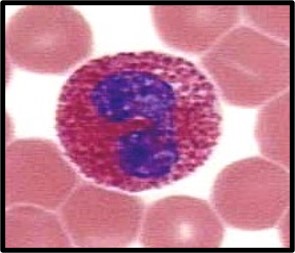
Give a description of Monocytes
* Agranulocyte(contains no cytoplasmic granules)
* Phagocytic cells
* 2-8% of circulating WBC’s
* Very large with U-shaped nucleus
* It enters peripheral tissues and becomes Macrophages that secretes substances to attract immune system cells and fibrocytes to injured area
* Increases in numbers during viral and bacterial infections to those viruses and bacteria
* Phagocytic cells
* 2-8% of circulating WBC’s
* Very large with U-shaped nucleus
* It enters peripheral tissues and becomes Macrophages that secretes substances to attract immune system cells and fibrocytes to injured area
* Increases in numbers during viral and bacterial infections to those viruses and bacteria
70
New cards
Give a description of Lymphocytes.
* 20%-30% of circulating WBC’s (these are what keep you immune)
* Agranulocytes(no cytoplasmic granules)
* Nucleus takes up most of the cell
* Mostly in Connective Tissues and lymphoid organs(lymph nodes and spleen)
* Part of the body’s specific defense system (immunity, T-cells and B-cells)
* Agranulocytes(no cytoplasmic granules)
* Nucleus takes up most of the cell
* Mostly in Connective Tissues and lymphoid organs(lymph nodes and spleen)
* Part of the body’s specific defense system (immunity, T-cells and B-cells)
71
New cards
How is the lymphatic system related to the Circulatory system?
In order for there to be lymph, plasma from the cardiovascular system is pushed into the capillaries, plasma will leak out becoming interstitial fluid about 10% and go into the lymphatic system up to the cardiovascular system. Most of the plasma, about 90% goes back to cardiovascular system by the venous system
72
New cards
Trace the general pathway of lymph
1. We start off with the heart and the heart sends the blood out through the arterial system and gets down to a capillary bed (site of exchange).
2. Once in capillary bed, plasma will leak out of the capillary bed and go into the spaces around the cells and **become interstitial fluid.**
1. Some of that fluid is reabsorbed and put back into the venule end which returns to the heart. However, not all of it was put back into the venule end and still in the interstitial space which needs to be taken back up by the Lymphatic system.
3. Interstitial fluid goes into the **Lymphatic capillary** turning it into the fluid known as Lymph.
4. The fluid is then transported to the Lymph node, they are packed with WBC’s which filters the lymph and transports it to the **lymphatic vessels**
5. The lymphatic vessels merge into the vessels of the **Cardiovascular system** to return the lymph back to the blood becoming plasma again
6. There are lymphatic organs that help filter in this process which is the **liver, spleen, bone marrow and thymus**
73
New cards
How is lymph returned against gravity?
After plasma from the cardiovascular system is forced into capillaries, plasma leaks out and goes into the lymphatic system and it goes along with the venous system which both have to work its way back up to the cardiovascular system against gravity.
74
New cards
What are the primary functions of lymph?
To return the proteins to the bloodstream that has leaked out of the blood capillaries and to transport bacteria and other foreign particles to the lymph node to be filtered.
75
New cards
What is lymph composed of?
White blood cells, especially lymphocytes, the cells that attack bacteria in the blood and body tissues. Fluid from the intestines called chyle, which contains proteins and fats.
76
New cards
What is the structure of and function of the Thymus?
Located in mediastinum (right above heart)
Atrophies(shrink) after puberty which diminishes the effect of your immune system and produces a hormone called Thymosin which stimulates mature T-cell development.
Atrophies(shrink) after puberty which diminishes the effect of your immune system and produces a hormone called Thymosin which stimulates mature T-cell development.
77
New cards
What is the structure of the spleen?
Attached to stomach by gastrosplenic ligament
Contacts diaphragm and left kidney
Splenic veins, arteries and lymphatic vessels that communicate with spleen at hilum (indentation)
Contacts diaphragm and left kidney
Splenic veins, arteries and lymphatic vessels that communicate with spleen at hilum (indentation)
78
New cards
What is the function of the spleen?
Very important in Blood cell recycling
1. Removal of abnormal blood cells and other blood components (platelets) by phagocytosis
2. Storage of iron recycled from RBC
3. Initiation of immune responses by Bcells and Tcells in response to antigens circulating blood
4. Blood reservoir , stores blood
1. Removal of abnormal blood cells and other blood components (platelets) by phagocytosis
2. Storage of iron recycled from RBC
3. Initiation of immune responses by Bcells and Tcells in response to antigens circulating blood
4. Blood reservoir , stores blood
79
New cards
What is Nonspecific defense?
Innate, what you have since birth
Defenses that help protect you from a wide range of possible pathogen invaders and toxins UNTIL immunity can be activated!
Defenses that help protect you from a wide range of possible pathogen invaders and toxins UNTIL immunity can be activated!
80
New cards
What is Specific defense?
When you need to develop immunity by being exposed to it. Therefore, you’ve been exposed to something and the body has responded and has made defense cells to be able to recognize it. Thus, if you get it again later on you won’t get sick, you’ll be immune.
81
New cards
What is the inflammation response?
* It’s localized tissue response that produces, local swelling, redness, heat, and pain.
* Can be triggered by cells that are damaged from any source release prostaglandins, proteins and potassium ions
* Foreign proteins or pathogens could also activate inflammatory response
* Can be triggered by cells that are damaged from any source release prostaglandins, proteins and potassium ions
* Foreign proteins or pathogens could also activate inflammatory response
82
New cards
What are the nonspecific defenses mechanism?
1. Species Resistance
1. (if we didn’t have the receptor for that virus, it couldn’t get in, however if immunity is low it can get by crossing species barrier)
2. Racial Immunity
1. (Genetic Resistance, everyone has different genetics)
3. Physical Barriers
4. Skin first line of physical defense, oil washes away microorganisms, hair provides protection. Epithelial linings of the body, secretions of mucus, enzymes and stomach acid. Phagocytes (neutrophils, eosinophils and macrophages derived from monocytes) that engulf and destroy foreign compounds and pathogens
5. Positive Flow/ Mechanical Processes
1. (puking and pooping, we put something in the body that the body wants to get rid of)
6. Chemical Barriers
1. (Saliva/tears, mucus, defensins/sebum, sweat, gastric juice, bile, small intestinal enzymes, urine, cerumen, and normal microflora secretions)
7. Phagocytes
1. Neutrophils, Eosinophils and macrophages
8. Immunological surveillance
1. Constant monitoring for abnormal cells by NK cells. Immunological escape by detecting capsule which causes cancer cells to spread
9. Interferons
1. (interferes with the replication of the virus, slows it down to stimulate macrophages and NK cells 2. Alpha interferon (virus infected cells), Beta interferon (secreted by fibroblasts to slow inflammation), Gamma interferons(secreted by Tcells and NK cells)
10. Complement
1. (System that complements specific immunity, they’re going to work together
11. Inflammatory Response
1. (Rubor, tumor/edema, calor and dolar)
12. Fever
83
New cards
What is Species Resistance?
* If we don’t have the receptor for that virus it couldn’t get in such as Avian bird flu, it didn’t affect humans, it affected birds. We humans don’t provide the right environment for most microbes they would die.
* However, if immunity is low, it can get by “crossing species barrier” for example Avian bird flu didn’t affect humans however, all of our viruses originate from animals , they cross the species barrier in a period of suppressed immunity.
* However, if immunity is low, it can get by “crossing species barrier” for example Avian bird flu didn’t affect humans however, all of our viruses originate from animals , they cross the species barrier in a period of suppressed immunity.
84
New cards
What is Racial/Genetic Immunity?
* We all have different genetics even our immune system is a little bit unique to us and some of us can recognize a specific antigen where areas some of us might not bc we develop our Tcells and Bcells in a random fashion.
* Ex: Majority of African descent have a sickle cell anemia mutation that helped them survive Malaria, macrophages see it as damaged RBC and eat it causing less Malaria so you can survive.
* Ex: CD4 receptor mutation which is a receptor on your WBC’s that lets HIV in. This could lead to AIDS but you could have HIV infection without AIDS bc the virus can’t get to the Tcells which means it can’t give you aids
* Ex: Majority of African descent have a sickle cell anemia mutation that helped them survive Malaria, macrophages see it as damaged RBC and eat it causing less Malaria so you can survive.
* Ex: CD4 receptor mutation which is a receptor on your WBC’s that lets HIV in. This could lead to AIDS but you could have HIV infection without AIDS bc the virus can’t get to the Tcells which means it can’t give you aids
85
New cards
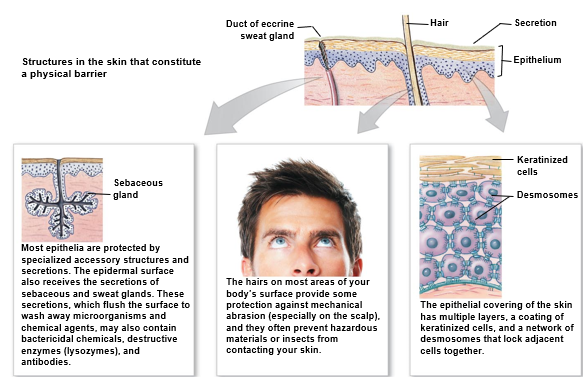
What are the Physical barriers of nonspecific defense?
* Integumentary system(skin)
* First line of physical defense!
* Multiple layers of dead water proof keratin cells linked very tightly together with desmosomes and tight junctions forming a permeability barrier to not allow things to get in
* Hair
* Provides protection from mechanical abrasion(not as much as animals) and prevents hazardous materials or insects from contacting skin
* Secretions from Sebaceous and Sweat glands
* Destroy or Wash away pathogenic and chemical agents. (contains bactericidal chemicals, destructive enzymes(lysozymes) and antibodies
* Orifices open to the outside that are all lined with an epithelial tissue that’s a mucous membrane
* oral, anal, ears, eyes, nose and genital openings
* First line of physical defense!
* Multiple layers of dead water proof keratin cells linked very tightly together with desmosomes and tight junctions forming a permeability barrier to not allow things to get in
* Hair
* Provides protection from mechanical abrasion(not as much as animals) and prevents hazardous materials or insects from contacting skin
* Secretions from Sebaceous and Sweat glands
* Destroy or Wash away pathogenic and chemical agents. (contains bactericidal chemicals, destructive enzymes(lysozymes) and antibodies
* Orifices open to the outside that are all lined with an epithelial tissue that’s a mucous membrane
* oral, anal, ears, eyes, nose and genital openings
86
New cards
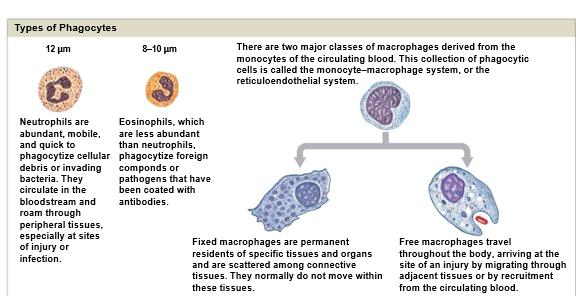
Explain phagocytes of nonspecific defenses
* Phagocytes cells roam all throughout the body
* Engulfs and destroys foreign compounds and pathogens which is the **First line of cellular defense against pathogenic invasion**
* 3 types
* Neutrophils (in bloodstream and tissues)
* Phagocytize cellular debris or bacteria
* Eosinophils (less abundant)
* Phagocytize foreign compounds and antibody-coated pathogens
* Macrophages (derived from monocytes)
* Fixed (permanent residents of certain organs, dendritic langar Hans on the skin and Kupffer cells in the liver)
* Free (travel throughout the body)
* Engulfs and destroys foreign compounds and pathogens which is the **First line of cellular defense against pathogenic invasion**
* 3 types
* Neutrophils (in bloodstream and tissues)
* Phagocytize cellular debris or bacteria
* Eosinophils (less abundant)
* Phagocytize foreign compounds and antibody-coated pathogens
* Macrophages (derived from monocytes)
* Fixed (permanent residents of certain organs, dendritic langar Hans on the skin and Kupffer cells in the liver)
* Free (travel throughout the body)
87
New cards
What are the Chemical Barriers of Nonspecific defense?
* Saliva/tears
* Mucus
* Defensins/ Sebum
* Sweat
* Gastric Juice
* Bile
* Small Intestine Enzymes
* Urine
* Cerumen
* Normal Microflora Secretions
* Mucus
* Defensins/ Sebum
* Sweat
* Gastric Juice
* Bile
* Small Intestine Enzymes
* Urine
* Cerumen
* Normal Microflora Secretions
88
New cards
Describe the chemical barrier Saliva/tears
* Primary enzyme, lysozyme(digestion) works on Gram + bacteria on skin and had are Gram + .
* Saliva/teas have lysozyme in them which is why we don’t get as many eye infections bc the tears are constantly rinsing lysozyme over your eyes.
* Lysozyme isn’t protective against E.coli bc it’s a Gram - bacteria which is why kids are more prone to pink eye.
* Saliva/teas have lysozyme in them which is why we don’t get as many eye infections bc the tears are constantly rinsing lysozyme over your eyes.
* Lysozyme isn’t protective against E.coli bc it’s a Gram - bacteria which is why kids are more prone to pink eye.
89
New cards
Describe the chemical barrier Mucus
Mucus is being produced by all the Goblet cells which also has lysozyme in it.
90
New cards
Describe the Chemical barrier, Defensins/Sebum
Sebum is Oil produced in sebaceous glands, defensive chemical effective in destroying some bacteria and some viruses
91
New cards
Describe the chemical barrier, Sweat.
“salty”, makes skin dry which sucks out all the water out of possible microbes(hypertonic). Salt is used to preserve food for it not to spoil since it sucks all the water out of possible microbes.
92
New cards
Describe the Chemical barrier, Gastric Juice
What’s being produced in the stomach, acids and enzymes. The enzyme in the stomach Pepsin (digests protein). All lot of bacteria we ingest are destroyed by stomach acid. Foods that we eat can let microbes pass like ice cream that can neutralize the acidic stomach.
93
New cards
Describe the chemical barrier, Bile
Produced by your liver from the breakdown of hemoglobin. Antimicrobial, but we don’t secret a lot of Bile unless were digesting very fatty foods, so its released to help with fat digestion.
94
New cards
Describe the chemical barrier, small intestinal enzymes.
Inside intestinal tract, in order to breakdown your nutrients you have to produce, all sorts of enzymes. Enzymes breakdown sugars, fats, proteins. Sometimes we end up digesting the microbes before they can make you sick, it protects you.
95
New cards
Describe the chemical barrier, Urine
Can be acidic especially if you eat a lot of acidic foods, which can kill bacteria.
The Ph of the vagina is important the more acidic it is will protect the vagina from the bacteria killing it.
The Ph of the vagina is important the more acidic it is will protect the vagina from the bacteria killing it.
96
New cards
How can we get a UTI?
Since there isn’t much space between the rectum and urethra, when having intercourse the bacteria (E.coli) is motile and can go into the urethra and into the bladder starting to grow causing a bladder infection.
97
New cards
Describe the chemical barrier, Cerumen
Ear wax, protects us from insects and preventing anything from entering.
98
New cards
Describe the chemical barrier, normal microflora secretions
Bacteria that is on your body that is suppose to be there! Bacteria can produce Antibiotics. Honey has Clostridium botulinum spores that can produce a neurotoxin therefore Infants can’t have honey bc they don’t have normal microflora like adults have and can paralyze the infants (SIDS, sudden infant death syndrome)
99
New cards
What is phagocytosis?
Engulfing/eating bacteria to get rid of it.
100
New cards
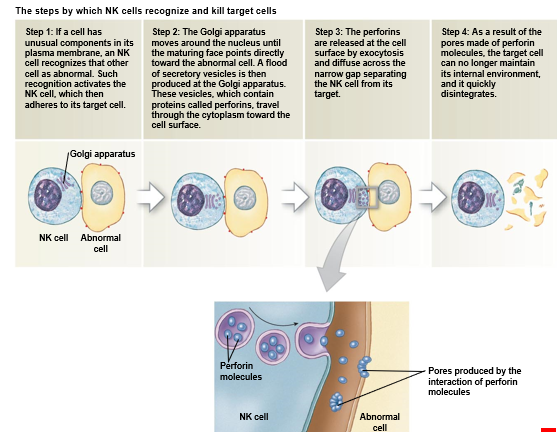
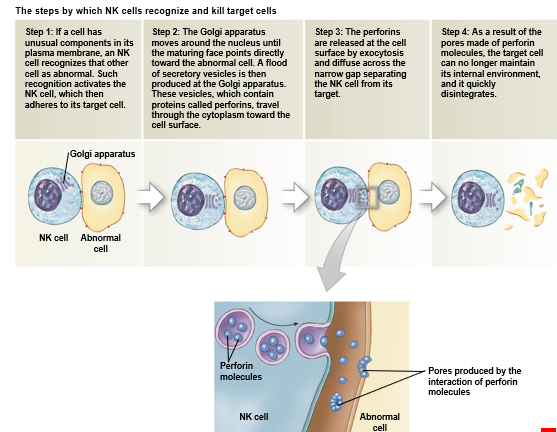
Describe the nonspecific defense, Immunological Surveillance
Constant monitoring of normal tissues by NK cells. NK cells recognize bacteria, foreign cells, virus infected cells and cancer cells. NK cells also destroy abnormal cells.
Cancer cells often contain tumor specific antigens (they have a protein on their surface that indicates its a cancerous cell) NK cells recognize them as abnormal and destroy them
Cancer cells often contain tumor specific antigens (they have a protein on their surface that indicates its a cancerous cell) NK cells recognize them as abnormal and destroy them