Ch. 27 - Male Reproductive System
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
58 Terms
External Genitalia of Males
scrotum and penis
Occupy the perineum
Bordered by the pubic symphysis, ischial tuberosities, and coccyx
Main function is to deliver gametes
Scrotum
pouch of skin, muscle, and fibrous connective tissue containing the testes
Left testicle usually hangs lower than the right so the two are not compressed against each other
Skin has sebaceous glands, sparse hair, rich sensory innervation, and dark pigmentation
Internal median septum divides scrotum into right and left sides
left side has the longer testicular vein, so it is very prone to having circulatory issues
Spermatic Cord
bundle of fibrous connective tissue containing the ductus deferens, blood and lymphatic vessels, and testicular the nerve
Continues through the inguinal opening into the pelvic cavity
External inguinal ring: inferior entrance to inguinal canal
Internal inguinal ring: superior exit to pelvic cavity
Why are testes in the scrotum?
Human testes reside in the scrotum because of its cooler environment
Cannot produce sperm at core body temperature of 37°C
Must be held at about 35°C (95 degreees F)
Testes (testicles)
combined endocrine and exocrine glands that produce sex hormones and sperm
Each teste is oval and slightly flattened
white in color
covered by tunica albunginea (white fibrous capsule) which has another membrane around it called the tunica vaginalis, forming a serous membrane with a bit of fluid between
testes have septa that divide them into 250-300 lobes
testes secrete high levels of testosterone throughout their life
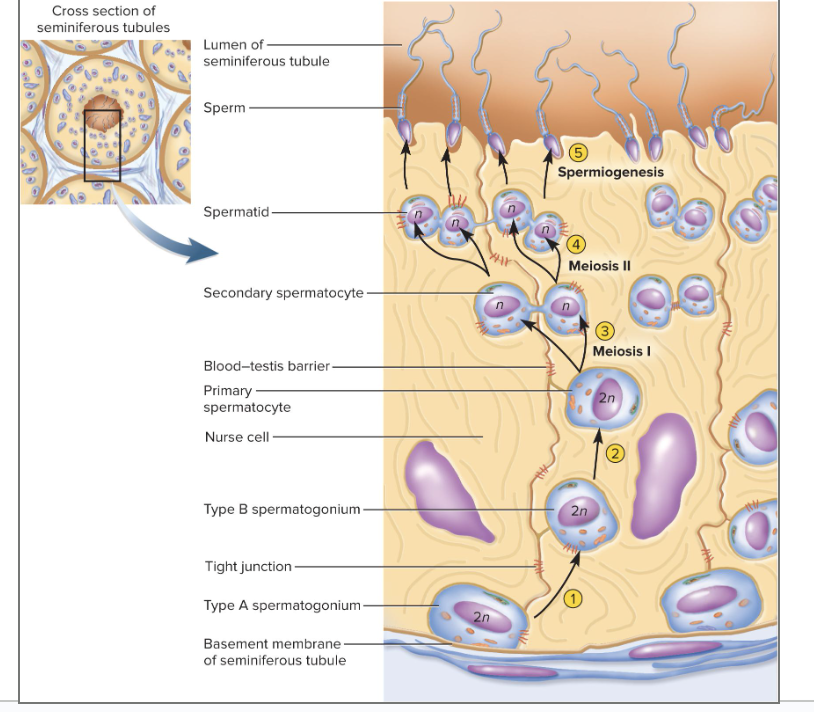
Seminiferous Tubules
Ducts in the testes where sperm are produced
One to three in each lobule
Each tubule is lined with a thick epithelium of germ cells and nurse cells
germ cells become sperm
surrounded by interstitial endocrine cells
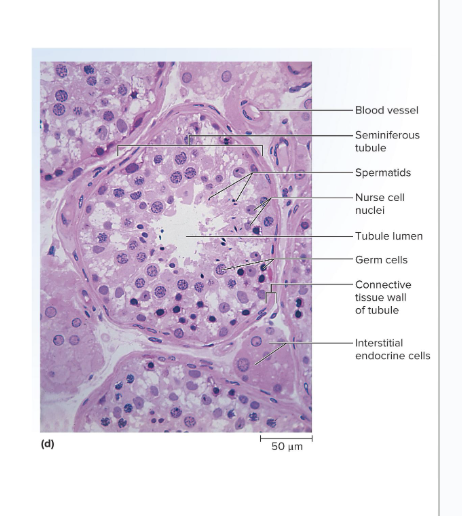
Nurse Cells in Seminiferous Tubules
Nurse cells are in between the germ cells
Protect the germ cells, and promote their development
Germ cells depend on them for nutrients, waste removal, growth factors, and other needs
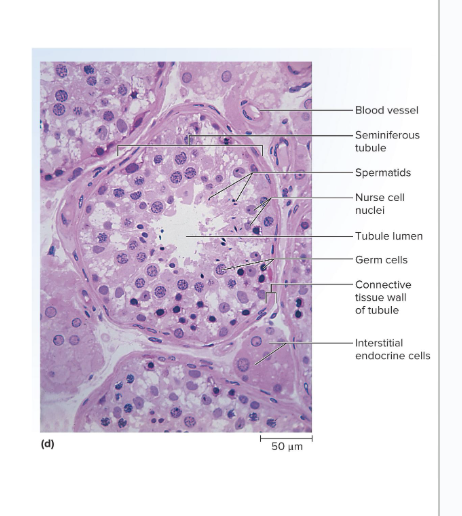
Interstitial Endocrine (Leydig) Cells
Clumps of cells that are between the tubules that produce testosterone
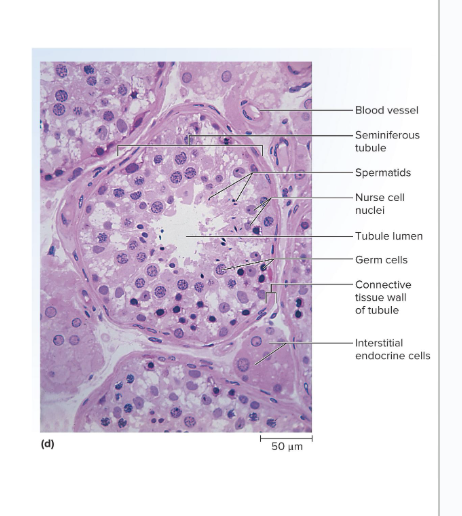
Blood–Testis Barrier (BTB)
formed by tight junctions between nurse cells
protects sperm from pathogens and the immune system
Why do we need to protect germ cells from our immune system?
Germ cells are immunologically different from body cells and would be attacked by the immune system if we did not have this barrier
Spermatic Ducts
Carry sperm from testis to the urethra
includes:
Efferent Ductules
Epididymis
ductus deferens
ejaculatory duct
Efferent Ductules
12 small ciliated ducts that collect sperm from the testes and transport it to the epididymis
start in the testes
connects testes to epididymis
Epididymis
Is a single coiled duct, (6 m long), that attaches to the back of the testes
Site of sperm maturation and storage (fertile for 40 to 60 days)
Sperm mature as they travel through the duct
If not ejaculated in the 40-60 days, they disintegrate and the epididymis reabsorbs them
includes a head, body, and tail
Ductus (vas) Deferens
Muscular tube passing up from the scrotum through the inguinal canal to the back of the bladder
Duct widens behind the bladder and widens into the terminal ampulla
Duct ends by uniting with the duct of the seminal vesicle
Has a thick wall of smooth muscle well innervated by sympathetic nerve fibers
causes parastaltic waves that moves sperm up through the inguinal opening to the back of the bladder
widens at the back of bladder to store sperm
during arousal, smooth muscle contractions will push the sperm to the ejaculatory duct
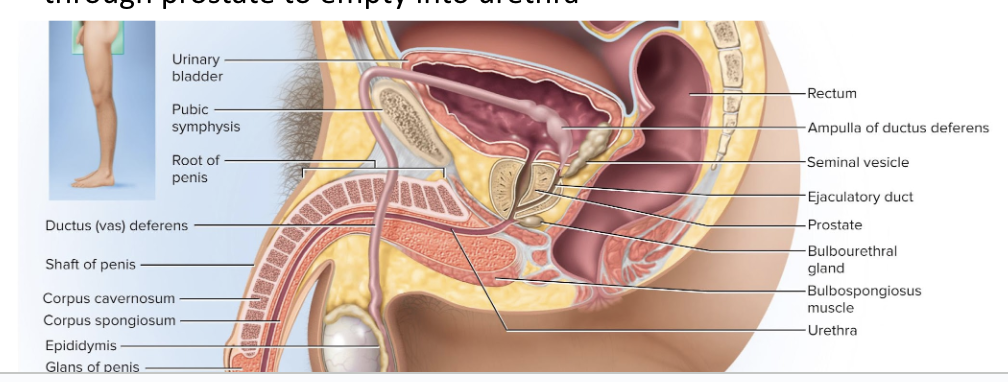
Ejaculatory Duct
Short duct formed from the ductus deferens and seminal vesicle
passes through prostate to empty into the urethra
allows secretions from seminal vesicle and sperm to mix and create semen
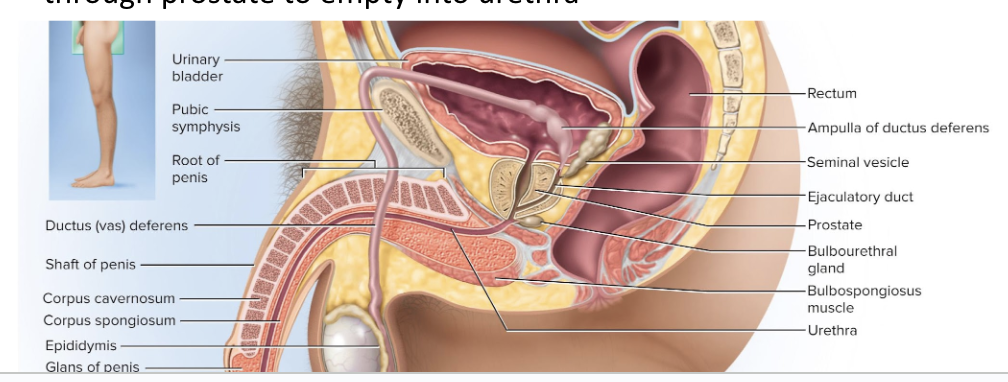
Seminal Vesicles
Pair of glands posterior to bladder
Empties into ejaculatory duct
Forms 60% of semen
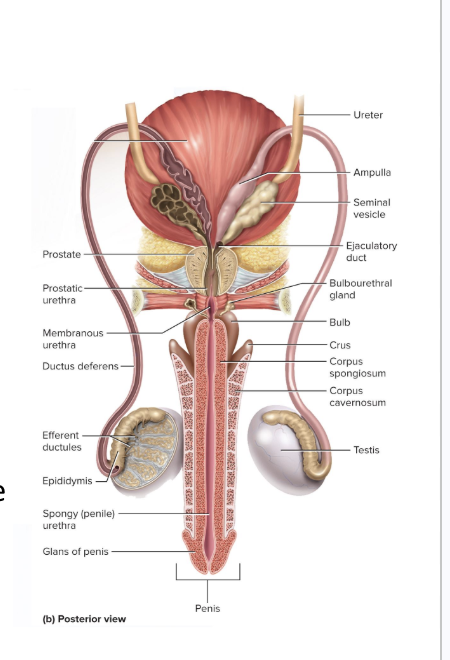
Prostate Gland
Single gland
Surrounds urethra and ejaculatory duct just below the bladder
Empty through about 20 pores in the prostatic urethra
Thin milky secretion forms 30% of semen
Bulbourethral glands
Near bulb of penis, right on either side of the midsaggital plane
During sexual arousal, they produce a clear, alkaline, slippery fluid that lubricates the head of the penis in preparation for intercourse
Protects the sperm by neutralizing the acidity of residual urine in the urethra
Penis
Penis serves to deposit semen in the vagina
Half of the penis is an internal root
Half is an externally visible shaft and glans (head)
External portion is about 4 in. long when flaccid
5 to 7 in. long when erect
Skin over shaft loosely attaches to allow expansion
Extends over the head as a prepuce (foreskin) that is removed by circumcision
What can circumcision lead to?
leads to development of less sensitive epidermis on the glans (head)
pros is that it leads to less STIs
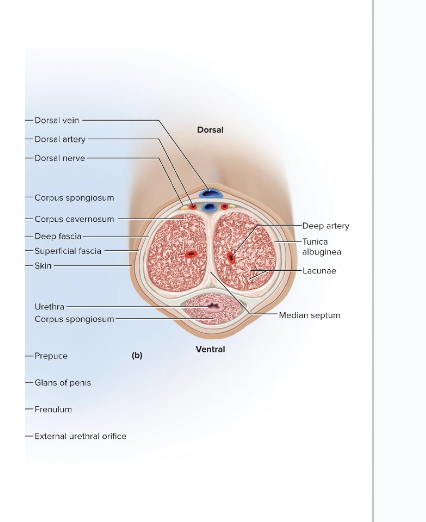
Internal Structure of the Penis
Has 3 cylindrical bodies of erectile tissue that fill with blood during sexual arousal and create an erection
the 3 bodies are…
one corpus spongiosum along the ventral side of penis
Two corpora cavernosa
Prepubescent boys only have 2 bodies of erectile tissue instead of 3
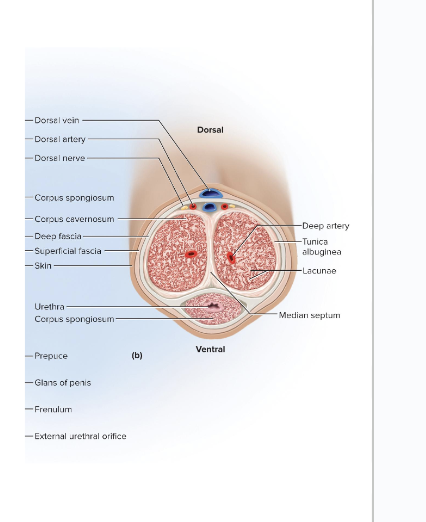
Corpus Spongiosum
Erectile tissue that runs along the front side of the penis
Encloses the spongy (penile) urethra
Distal end enlarges and forms the glans penis (penis head)
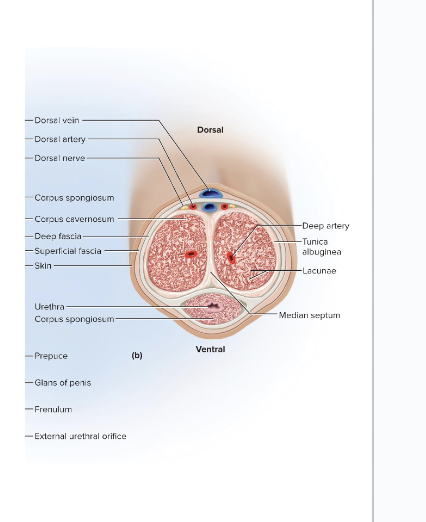
Corpora Cavernosa
erectile tissue that makes up the rest of the penis
Diverge like arms of a Y from the corpus spongiosum
Each arm, called a crus, attaches the penis to the pubic arch
is covered with ischiocavernosus muscle
What state is the reproductive system in for several years after birth?
Reproductive system remains dormant for several years after birth
10 to 12 years in most boys
8 to 10 years in most girls
Surge of pituitary gonadotropins awakens the reproductive system, leading to onset of puberty
Adolescence
The period from the onset of gonadotropin secretion and reproductive development to when a person attains full adult height
adolescence ends when person stops growing taller
for most males, adolescence ends at around 18 years old
Puberty
first few years of adolescence, until the first menstrual period in girls or the first ejaculation of viable sperm in boys
Typically around age 14 in boys and age 12 in girls
How does the concentration of testosterone fluctuate from utero to adult male?
The testes secrete testosterone in utero at levels about as high as they are midpuberty
Then testes becomes dormant until puberty
From puberty through adulthood, reproductive function is regulated by hormonal links between the hypothalamus, pituitary gland, and gonads
Gonadotropin-Releasing Hormone (GnRH)
produced by the hypothalamus
stimulates the anterior pituitary to secrete FSH and LH which will go to the testes do serve different functions
Follicle-Stimulating Hormone (FSH)
Stimulates nurse cells to secrete androgen-binding protein that binds testosterone,
this keeps testosterone in the seminiferous tubule to stimulate spermatogenesis
Luteinizing hormone (LH)
LH goes to interstitial endocrine cells and stimulate testosterone production
sometimes called interstitial cell–stimulating hormone (ICSH)
What hormone do nurse cells release and what does it do?
Inhibin
inhibin down-regulates FSH, which down-regulates androgen binding proteins so we maintain homeostasis for sperm production
What does testosterone do in the male reproductive system?
testosterone down-regulates GNRH and gonadotropin release
testosterone also has potent secondary sex characteristics
What does testosterone do during puberty (5 things)?
Stimulates growth of sex organs
Penis, testes, scrotum, ducts, glands
Testosterone stimulates generalized body growth
Limbs elongate, muscle mass increases, and larynx enlarges
Stimulates erythropoiesis, basal metabolic rate, and appetite
Pubic hair, axillary hair, and facial hair develop in response to dihydrotestosterone (DHT)
apocrine and sebaceous glands also develop
Stimulates sperm production and libido
What do hormones do during adulthood?
Testosterone sustains the male reproductive tract, sperm production, and libido
gradual decline in libido as testosterone declines
Inhibin from nurse cells suppresses FSH output, reducing sperm production without reducing LH and testosterone secretion
Spermatogenesis
process of sperm production in the seminiferous tubules
Involves 3 principal events
Division and remodeling of large germ cells into small, mobile sperm cells with flagella
Reduction of chromosome number by half
Shuffling of genes (crossing over) so each chromosome contains new gene combinations that did not exist in the parent
Ensures genetic variation in the offspring
Meiosis produces 4 haploid daughter cells that will become sperm
6 steps from spermatogonium to sperm
Spermatogonium
Primary Spermocyte
Secondary Spermocyte
Early Spermatid
Late Spermatid
Sperm
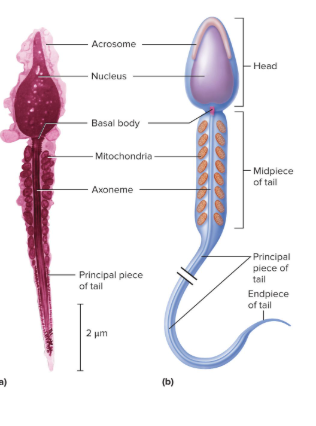
Spermatozoon (Sperm Cell)
Has two parts: head and tail
Head is pear-shaped
contains the nucleus
has haploid set of chromosomes
has the acrosome
enzyme cap that contains enzymes that will help it penetrate the egg
Tail is divided into 3 regions:
Midpiece
contains mitochondria
produces ATP for flagellar movement
Principal piece
the middle axoneme portion surrounded by supporting fibers
Constitutes most of tail
Endpiece
very narrow tip of flagella
Semen (seminal fluid)
Fluid expelled during orgasm
2 to 5 mL of fluid is expelled during ejaculation
Semen is 60% seminal vesicle fluid, 30% prostatic fluid, and 10% sperm and spermatic duct secretions
Normal sperm count is 50 to 120 million/mL
Anything lower than 20 to 25 million/mL indicates infertility
To help make semen, what does the prostate produce?
Prostate produces a thin, milky white fluid
Contains calcium, citrate, and phosphate ions
also contains a clotting enzyme
this causes semen to grow a thick coagulated mask to keep the sperm together to make it easier for it to reach female reproductive tract
also contains a protein-hydrolyzing enzyme called serine protease (prostate-specific antigen) to break that thick mask and release the sperm freely
To hep make semen, what do the seminal vesicles produce?
Seminal vesicles produces a viscous yellowish fluid
Contains fructose and other carbohydrates, citrate, prostaglandins, and protein called proseminogelin
the prostaglandins help stimulate smooth muscle contractions to help move sperm
How does the stickiness of semen promote fertilization?
Clotting enzyme from prostate activates proseminogelin and converts it to a sticky fibrin-like protein called seminogelin
This entangles the sperm and causes it to stick to the inner wall of the vagina and cervix
This ensures semen does not drain back into vagina
Promotes the uptake of sperm-filled clots of semen into the uterus
20 to 30 minutes after ejaculation, serine protease from prostatic fluid breaks down seminogelin, and liquifies the semen so it can swim freely up the tract
2 requirements for sperm motility:
elevated pH and an energy source
Prostatic fluid buffers vaginal acidity from pH 3.5 to 7.5
Seminal vesicles provide fructose and other sugars to the mitochondria of sperm for ATP production
How do semen make it to the female reproductive tract?
Active sperm crawl up vagina and uterus
Prostaglandins in semen may thin the mucus of the cervical canal and can stimulate waves of contractions in the uterus to help move the semen
female orgasm also gives sperm a kickstart in moving
4 Phases of Male Sexual Response
Excitement
Plateau
Orgasm
Resolution
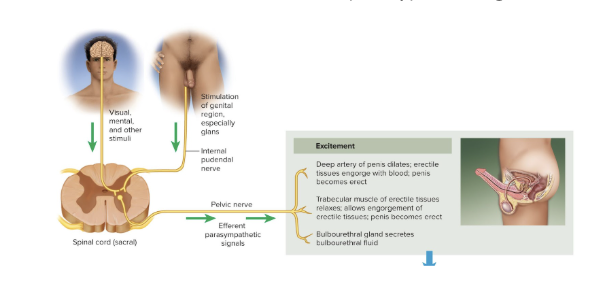
Excitement Phase
characterized by vasocongestion (swelling of genitals with blood), myotonia (muscle tension), and increases in heart rate, blood pressure, and pulmonary ventilation
Bulbourethral glands secrete fluid
Erection is primarily due to parasympathetic NS triggering the secretion of nitric oxide (NO)
NO is a potent vasodilator
arteries dilate and fill erectile tissue with blood
penile veins constrict so less can flow out
Erection allows for entry into vagina
Plateau Phase
variables such as respiratory rate, heart rate, and blood pressure stay increased
increase in engorged tissue and muscle tension
Lasts for a few seconds or a few minutes before orgasm
Orgasm
a short but intense reaction that is usually marked by the discharge of semen
Lasts 3 to 15 seconds
Heart rate, blood pressure, and breathing greatly elevate
tightening of skeletal muscles can occur
2 Stages of Ejaculation
Emission:
when the different ingredients of semen are being premixed
sympathetic nervous system stimulates peristalsis which propels sperm through the ducts once mixed
Expulsion:
also stimulated by sympathetic nervous system
semen in urethra activates reflexes that stimulate muscular contractions that lead to expulsion
internal urethral sphincter constricts so urine cannot enter urethra and semen cannot enter bladder
*Ejaculation and orgasm are not the same
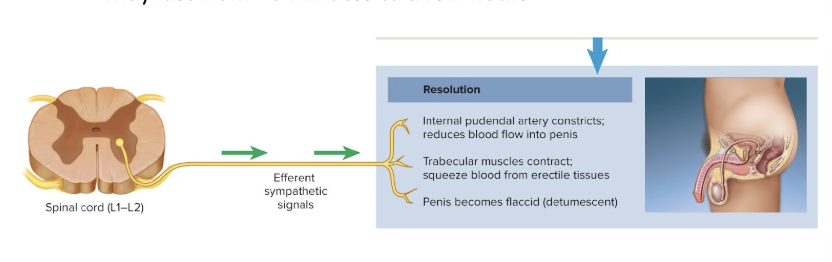
Resolution Phase
body variables return to their preexcitement state
Sympathetic signals constrict arteries to reduce blood flow to penis
Penis becomes soft and flaccid
Cardiovascular and respiratory functions return to normal
important bc stagnant blood can lead to blood clotting
Refractory Period
period following resolution where it is usually impossible for a male to attain another erection or orgasm
May last from 10 minutes to a few hours
Senescence of Male Reproductive System
Gradual decline in testosterone secretion, sperm count, and libido
Men are fertile into old age, but ED may occur due to atherosclerosis, hypertension, medication, or psychological reasons
Testosterone secretion declines with age
bc of decline in number and activity of interstitial endocrine cells
Andropause (male climacteric) may occur
Andropause
A period of declining reproductive function that may be first seen in early 50s
Although sperm counts decline, men can still father children throughout old age
not all men experience andropause
What do drops in testosterone and inhibin from age trigger?
An age-related drop in testosterone and inhibin triggers a rise in FSH and LH
Although most men do not notice this, some experience mood changes, hot flashes, “illusions of suffocation”
Erectile Dysfunction (impotence)
the inability to produce or maintain an erection sufficient for intercourse
20% of men in 60s to 50% of those in 80s
What age range has the highest rate of ED?
highest rate of ED currently is in males in their 30s
this change is due to smartphones and overconsumption of sexually explicit material
Treatments for ED
Viagra, Levitra, and Cialis
These are all phosphodiesterase inhibitors
How does the ED medication work in the body?
Sexual stimulation triggers nitric oxide secretion, which activates cGMP, which then increases blood flow into erectile tissue
These drugs slow the breakdown of cGMP by phosphodiesterase to prolong the duration of the erection
When should you not take ED meds?
if taking meds for High BP, then you shouldn’t take meds for ED bc both meds lower BP