Topic 6 Homeostatsis
0.0(0)
Card Sorting
1/114
Last updated 10:11 AM on 4/7/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
115 Terms
1
New cards
Taxes
Simple response in which an organism will move its entire body towards a favourable stimulus or away from an unfavourable stimulus → directional stimulus
Towards stimulus = positive taxis
Away from stimulus = negative taxis
Towards stimulus = positive taxis
Away from stimulus = negative taxis
2
New cards
Kinesis
An organism changes the speed of movement and rate due to non-directional stimulus
Positive area - less movement to stay where they are
Negative area - more movement to leave area to get positive
Positive area - less movement to stay where they are
Negative area - more movement to leave area to get positive
3
New cards
Plant tropism
Plant response via growth to stimulus
Positive = growth towards stimulus
Negative = growth away from stimulus
Responds to light, gravity and water
Positive = growth towards stimulus
Negative = growth away from stimulus
Responds to light, gravity and water
4
New cards
Indoleacetic acid (IAA)
Type of auxin, produced in the tips of shoots in flowering plants
Can diffuse to other cells
Can diffuse to other cells
5
New cards
Phototropism positIve
IAA diffuses to the shaded side of the shoot resulting in high conc. of IAA on shaded side
IAA causes the cells on the shaded side to elongate and shoot bends towards the light
IAA causes the cells on the shaded side to elongate and shoot bends towards the light
6
New cards
Phototropism negative
IAA diffuses to the shaded side of the root, so high conc. of IAA there
IAA causes cell elongation to be inhibited so root bends away from light
IAA causes cell elongation to be inhibited so root bends away from light
7
New cards
Gravitropism positive
IAA moves to the lower side of the root so high conc. of IAA there
Causes the upper side to elongate as IAA inhibits growth on the lower side so root bends down towards gravity and anchors in
Causes the upper side to elongate as IAA inhibits growth on the lower side so root bends down towards gravity and anchors in
8
New cards
Gravitropism negative
IAA diffuses to the underside of the shoots so there is high conc. of IAA there
Causes the cells to elongate so shoot bends upwards away from gravity
Causes the cells to elongate so shoot bends upwards away from gravity
9
New cards
IAA stimulating growth
1. binding to a receptor in the target cell zone of cell elongation in shoots/roots membranes and activating a proton pump
2. These pump protons (H+) from the cytoplasm to their cell walls
3. The resulting decrease in pH activates an enzyme that breaks the bonds between cellulose microfibrils
4. This loosens the cell wall and so allows the cell to elongate under internal turgor pressure - Ψ more negative in cytoplasm than outside so water enters via osmosis so cell grows
10
New cards
Central Nervous System
CNS
brain and spinal cord
brain and spinal cord
11
New cards
Peripheral Nervous System
PNS
Neurones that connect CNS to body
Splits into 2: somatic and autonomic nervous systems
Neurones that connect CNS to body
Splits into 2: somatic and autonomic nervous systems
12
New cards
Somatic nervous system
Controls conscious activities
13
New cards
Autonomic Nervous System
Controls unconscious activities
Splits into 2: sympathetic and parasympathetic
Splits into 2: sympathetic and parasympathetic
14
New cards
Sympathetic nervous system
Ready for action
Flight or fight
Flight or fight
15
New cards
Parasympathetic nervous system
Calms
Rest and digest
Rest and digest
16
New cards
Reflex arc
Body response to stimulus without making a conscious decision
Stimulus → receptors → sensory neurone → relay neurone → motor neurone → effectors → response
Stimulus → receptors → sensory neurone → relay neurone → motor neurone → effectors → response
17
New cards
Sensory neurone
Transmits electrical impulses from receptors to CNS
18
New cards
Relay neurone
Transmits electrical impulses between sensory and motor neurones
19
New cards
Motor neurone
Transmits electrical impulses from CNS to effectors
20
New cards
Resting potential
Neurone not conducting a nerve impulse
Difference between electrical charge inside and outside of neurone
At -70mV → outside is positively charged compared to inside as there are more positive ions outside than inside
Difference between electrical charge inside and outside of neurone
At -70mV → outside is positively charged compared to inside as there are more positive ions outside than inside
21
New cards
Establishing a resting potential
Maintained by sodium-potassium pumps → active transport using ATP
Pump moves:
* 2K+ into axon
* 3Na+ out of axon
This creates an electrochemical gradient
The membrane is more permeable to K+ so more are moved out via K+ channels via facilitated diffusion
* results in -70mV
* membrane becomes polarised
Pump moves:
* 2K+ into axon
* 3Na+ out of axon
This creates an electrochemical gradient
The membrane is more permeable to K+ so more are moved out via K+ channels via facilitated diffusion
* results in -70mV
* membrane becomes polarised
22
New cards
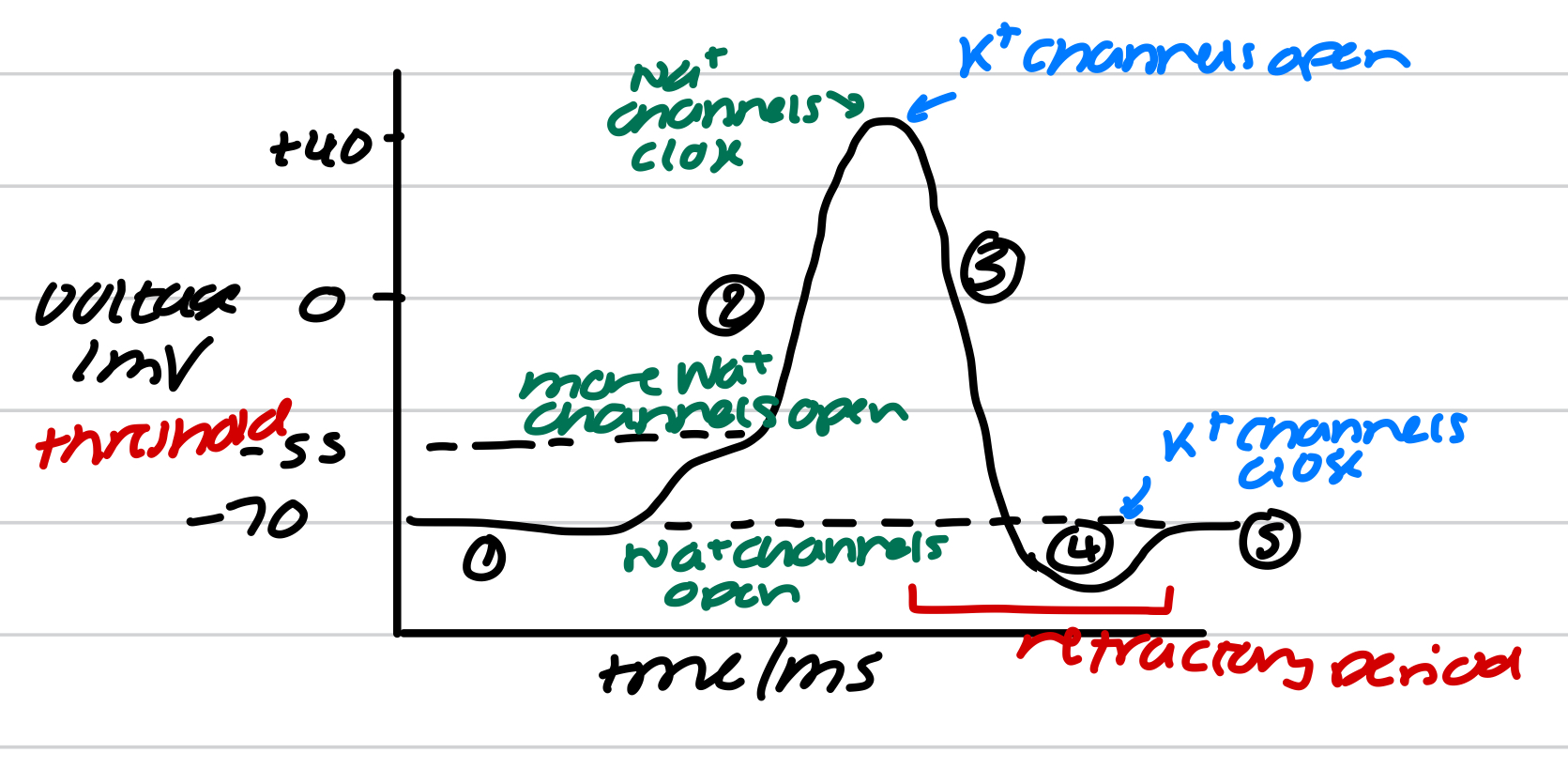
Action potential
Neurone voltage increases beyond a set point from the resting potential → this generates a nerve impulse
Increase in voltage (depolarisation) is due to membrane becoming more permeable to Na+
Increase in voltage (depolarisation) is due to membrane becoming more permeable to Na+
23
New cards
Action potential method
1. stimulus - excites the neurone cell membrane → Na+ channels open. The membrane becomes more permeable to Na+ so Na+ diffuses into neurone down Na+ electrochemical gradient. Makes the inside of neurone less negative
2. Depolarisation - if voltage reaches threshold of -55mV, more Na+ channels open causing more Na+ to diffuse rapidly into neurone
3. Repolarisation - at voltage +40mV, Na+ channels close and K+ channels open. Membrane is more permeable to K+ so K+ diffuse out of neurone down K+ concentration gradient. Membrane is back at resting
4. Hyperpolarisation - K+ channels are slow to close so slight ‘overshoot’, where too many K+ diffuse out of neurone. Voltage becomes more negative than the resting potential
5. Resting potential - ion channels reset. Na+/K+ pump returns membrane back to resting potential and maintains it until another stimulus
24
New cards
Refractory period
Neurone membrane can’t be excited straight away after an action potential due to ion channels recovering and can’t be made to open up again
So action potential can’t be regenerated
Act as a time delay between 1 action potential and next so:
* action potentials do not overlap but pass along as discrete (separate) impulses
* there is a limit to the frequency at which the nerve impulses can be transmitted
* action potentials are unidirectional
So action potential can’t be regenerated
Act as a time delay between 1 action potential and next so:
* action potentials do not overlap but pass along as discrete (separate) impulses
* there is a limit to the frequency at which the nerve impulses can be transmitted
* action potentials are unidirectional
25
New cards
Propagation/wave of depolarisation
When action potential happens, some Na+ that enter neurone diffuse sideways
Causes Na+ channels in the next part of the neurone to open and Na+ diffuses in
Causes a wave of depolarisation to travel along the neurone
Waves move along from parts of membrane in the refractory period as these parts can’t have an action potential
Causes Na+ channels in the next part of the neurone to open and Na+ diffuses in
Causes a wave of depolarisation to travel along the neurone
Waves move along from parts of membrane in the refractory period as these parts can’t have an action potential
26
New cards
All-or-nothing principle
If threshold isn’t reached, the action potential and the impulse are not produced - nothing
Any stimulus that reaches threshold will peak at the same voltage - all → bigger the stimulus increases the frequency of action potentials
Any stimulus that reaches threshold will peak at the same voltage - all → bigger the stimulus increases the frequency of action potentials
27
New cards
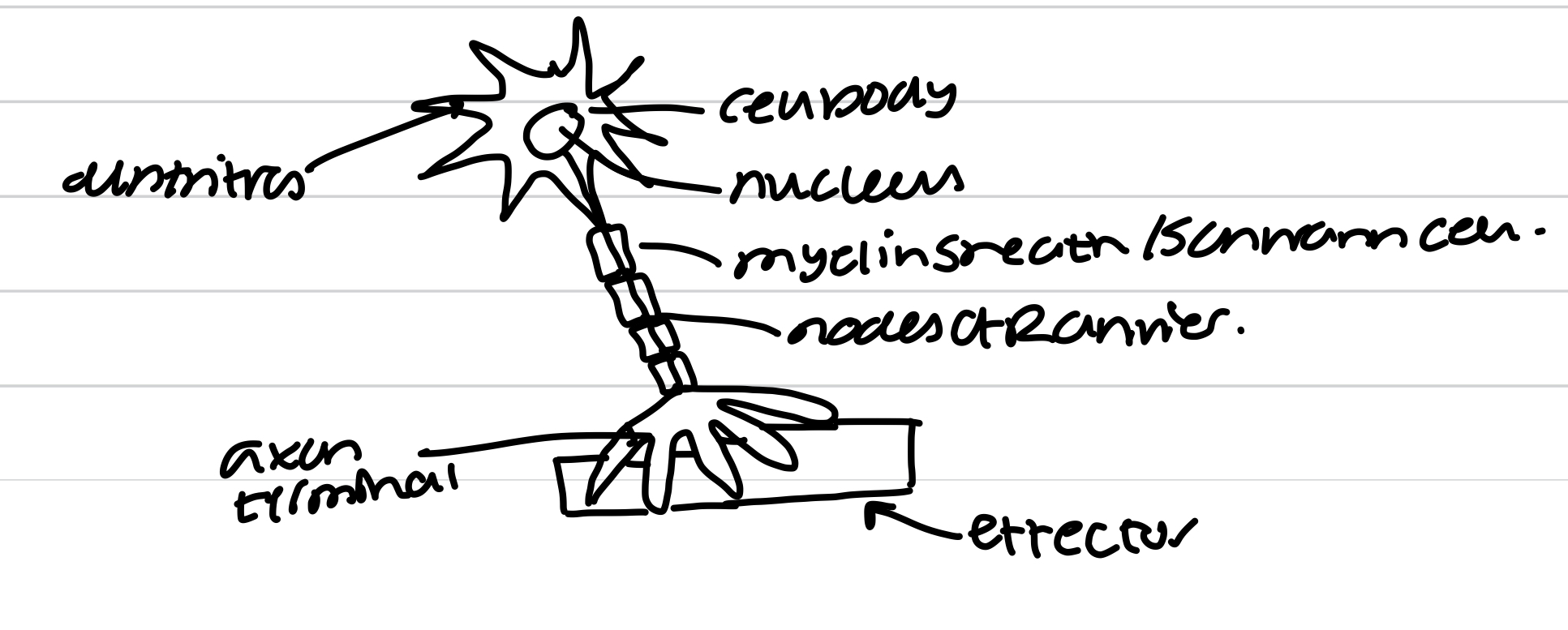
Myelinated motor neurone
28
New cards
Factors affecting speed of conduction - myelination
Neurones have myelin sheath or Schwann cell which is an electrical insulator
Gaps between Schwann cells are nodes of Ranvier. Na+ channels are concentrated at nodes
In myelinated neurone, depolarisation only happens at the nodes of Ranvier
Saltatory conduction - neurone’s cytoplasm conducts enough electrical charge to depolarise the next node, so impulse jumps node to node
In a non-myelinated neurone, the impulse travels as a wave along whole of axon membrane so depolarisation occurs along the whole length of the membrane and is slower than saltatory conduction
Gaps between Schwann cells are nodes of Ranvier. Na+ channels are concentrated at nodes
In myelinated neurone, depolarisation only happens at the nodes of Ranvier
Saltatory conduction - neurone’s cytoplasm conducts enough electrical charge to depolarise the next node, so impulse jumps node to node
In a non-myelinated neurone, the impulse travels as a wave along whole of axon membrane so depolarisation occurs along the whole length of the membrane and is slower than saltatory conduction
29
New cards
Factors affecting speed of conduction - axon diameter
Wider diameter of axon, speed of conduction increases due to less resistance of flow of ions and less leakage so action potential travels faster
30
New cards
Factors affecting speed of conduction - temperature
A higher temperature increases the speed of conductance as ions diffuse faster as enzymes involved in respiration work faster → more ATP for active transport
31
New cards
Synapse
Junction between a neurone cell and another neurone or neurone and effector
Gap is synaptic cleft
Action potential is transmitted as neurotransmitters that diffuse across the synapse
Gap is synaptic cleft
Action potential is transmitted as neurotransmitters that diffuse across the synapse
32
New cards
Function of synapse
1. an action potential arrives at the synaptic knob. This causes depolarisation of synaptic knob leading to the opening of Ca2+ voltage-gated channels and Ca2+ diffuses into synaptic knob
2. This causes synaptic vesicles to move and fuse to presynaptic membrane. This releases acetylcholine into synaptic cleft
3. acetylcholine diffuses down concentration gradient, across the synaptic cleft to the postsynaptic membrane. This binds to specific cholinergic receptors on postsynaptic membrane
4. This causes Na+ channels to open on the postsynaptic membrane. The influx of Na+ causes depolarisation. If threshold is reached, this generates a new action potential in postsynaptic membrane
5. acetylcholine is hydrolysed by acetylcholinesterase into ethanoic acid and choline. These diffuse into synaptic cleft into presynaptic neurone. Na+ channels close and postsynaptic membrane can re-establish the resting potential
6. ATP released by mitochondria is used to recombine choline and ethanoic acid, stored in synaptic vesicles for future
33
New cards
Neuromuscular junction
Postsynaptic cleft is the muscle fibre membrane and depolarisation leads to contraction of muscle fibre
34
New cards
Neuromuscular junction features
Only excitatory synapse
Linkes neurone to muscle
Action potential ends here
Only motor neurones
Acetylcholine binds to receptors on muscle membrane
Linkes neurone to muscle
Action potential ends here
Only motor neurones
Acetylcholine binds to receptors on muscle membrane
35
New cards
Cholinergic synapse features
Can be excitatory or inhibitory
Links neurones to neurones or neurone to effector
Another action potential may be generated along postsynaptic
Most neurones
Acetylcholine binds to receptors on postsynaptic membrane
Links neurones to neurones or neurone to effector
Another action potential may be generated along postsynaptic
Most neurones
Acetylcholine binds to receptors on postsynaptic membrane
36
New cards
Excitatory neurotransmitter
Post synaptic neurone is depolarised, triggering an action potential
37
New cards
Inhibitory neurotransmitter
Hyperpolarisation of postsynaptic neurone so no action potential is triggered
38
New cards
Inhibitory synapse
The presynaptic neurone releases an inhibitory neurotransmitter which binds to Cl- channels
Channels open causing facilitated diffusion of Cl- into postsynaptic neurone
May cause the opening of nearby K+ channels causing K+ to diffuse out
Cause an effect of more negative ions and less positive ions in cytoplasm of postsynaptic neurone causing hyperpolarisation
If an excitatory neurotransmitter was released at the same time, wouldn’t result in sufficient generator potential to reach threshold → no action potential is generated in postsynaptic neurone
Channels open causing facilitated diffusion of Cl- into postsynaptic neurone
May cause the opening of nearby K+ channels causing K+ to diffuse out
Cause an effect of more negative ions and less positive ions in cytoplasm of postsynaptic neurone causing hyperpolarisation
If an excitatory neurotransmitter was released at the same time, wouldn’t result in sufficient generator potential to reach threshold → no action potential is generated in postsynaptic neurone
39
New cards
Summation
The rapid build up of neurotransmitter in the synapse to help generate an action potential
This is needed as some action potentials do not result in sufficient concs of neurotransmitters being released to generate a new action potential
This is needed as some action potentials do not result in sufficient concs of neurotransmitters being released to generate a new action potential
40
New cards
Spatial summation
Many different neurones collectively trigger a new action potential by combining the neurotransmitters they released to exceed threshold
41
New cards
Temporal summation
The neurone releases neurotransmitter repeatedly over a short period of time to add up to enough to exceed threshold
42
New cards
Effects of stimulating drugs
Enhanced response
Can mimic the shape of the neurotransmitter, triggering action potentials
Stimulate the release of more neurotransmitters
Inhibits enzymes which breakdown neurotransmitters causing prolonged stimulation
Can mimic the shape of the neurotransmitter, triggering action potentials
Stimulate the release of more neurotransmitters
Inhibits enzymes which breakdown neurotransmitters causing prolonged stimulation
43
New cards
Effect of inhibitor drugs
Reduced response
Block response to stop neurotransmitters triggering action potentials
Bind to receptors and change their shape
Block response to stop neurotransmitters triggering action potentials
Bind to receptors and change their shape
44
New cards
Acetylcholine neurotransmitter
Parasympathetic nervous system
45
New cards
Noradrenaline neurotransmitters
Sympathetic nervous system
46
New cards
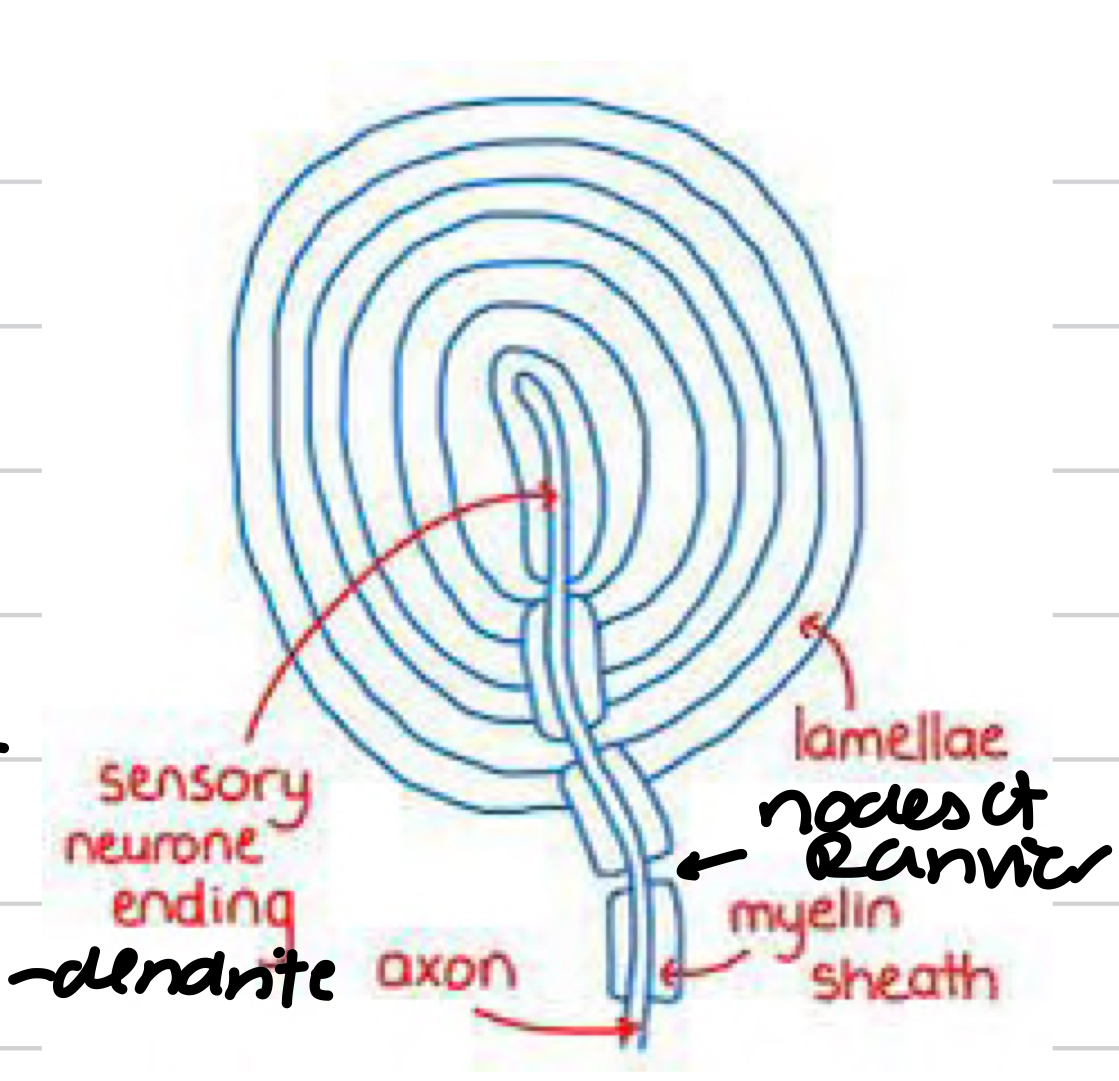
Pacinian Corpuscles
responds to changes in pressure
occur deep in skin, mainly feet and hands
consists of a single sensory neurone wrapped with layers of tissue separated by gel
Sensory neurone has special channel proteins in plasma membrane
* allows ion transportation
* Membranes surrounding sensory neurone have stretched-mediated Na+ channels
* Only open and allow Na+ to enter sensory neurone when stretched and deformed
occur deep in skin, mainly feet and hands
consists of a single sensory neurone wrapped with layers of tissue separated by gel
Sensory neurone has special channel proteins in plasma membrane
* allows ion transportation
* Membranes surrounding sensory neurone have stretched-mediated Na+ channels
* Only open and allow Na+ to enter sensory neurone when stretched and deformed
47
New cards
Pacinian Corpuscles structure
48
New cards
At resting of pacinian corpuscles
Na+/K+ pumps move Na+ away from dendrite. Therefore high diffusion gradient for Na+
Na+ channels are too narrow for Na+ to diffuse into sensory neurone so resting potential maintained
Na+ channels are too narrow for Na+ to diffuse into sensory neurone so resting potential maintained
49
New cards
Pressure applied on pacinian corpuscles
When pressure is applied, membrane stretches and deforms
Causes Na+ channels to open so Na+ diffuses into dendrite → this causes the generator potential
The greater the pressure, the more Na+ channels open so larger generator potential
If threshold is reached, an action potential occurs
Causes Na+ channels to open so Na+ diffuses into dendrite → this causes the generator potential
The greater the pressure, the more Na+ channels open so larger generator potential
If threshold is reached, an action potential occurs
50
New cards
Rod cells
Can’t distinguish between different wavelengths of light
Processes images in black and white
Can detect light at very low light intensities → many rod cells to 1 sensory neurone → retinal convergence
Contains light sensitive pigment, rhodopsin
* breaks down into opsin (protein) and retinal (vitamin A)
High visual sensitivity as spatial summation occurs
Low visual acuity as light from two close point aren’t able to be distinguished between
Processes images in black and white
Can detect light at very low light intensities → many rod cells to 1 sensory neurone → retinal convergence
Contains light sensitive pigment, rhodopsin
* breaks down into opsin (protein) and retinal (vitamin A)
High visual sensitivity as spatial summation occurs
Low visual acuity as light from two close point aren’t able to be distinguished between
51
New cards
Rod cells generating action potential
1. rhodopsin is broken down by light - bleaching
2. Must be enough energy from low-intensity light to cause breakdown
3. Enough pigment needs to be broken down for threshold to be met in the bipolar cell - become hyperpolarised and causes an action potential
Threshold can be reached in low light as many rod cells are connected to a single bipolar cell - spatial summation
Rhodopsin is reformed in the dark → dark adaption occurs from light to dark
52
New cards
Visual acuity
Measure of the ability of the eye to distinguish shapes and the details of objects at a given distance
53
New cards
Cone cells
Three types: red, green, blue
Contain pigment iodopsin
Each detects a different range of wavelengths
Stimulated by very high light intensities and sensitive to different wavelengths of light
A single cone cell contains 1 type of iodopsin
Colour vision
Low visual sensitivity → temporal summation
Can determine exact source of stimulus due to temporal summation → high visual acuity
Iodopsin is only broken down by high light intensities so generator potential can only be generated with enough light
Contain pigment iodopsin
Each detects a different range of wavelengths
Stimulated by very high light intensities and sensitive to different wavelengths of light
A single cone cell contains 1 type of iodopsin
Colour vision
Low visual sensitivity → temporal summation
Can determine exact source of stimulus due to temporal summation → high visual acuity
Iodopsin is only broken down by high light intensities so generator potential can only be generated with enough light
54
New cards
Fovea
Receives most light
Cone cells near
Rod cells far away at low light intensities
Cone cells near
Rod cells far away at low light intensities
55
New cards
Blind spot
No rod or cone cells
Not sensitive to light
Optic nerve
Not sensitive to light
Optic nerve
56
New cards
Heart
57
New cards
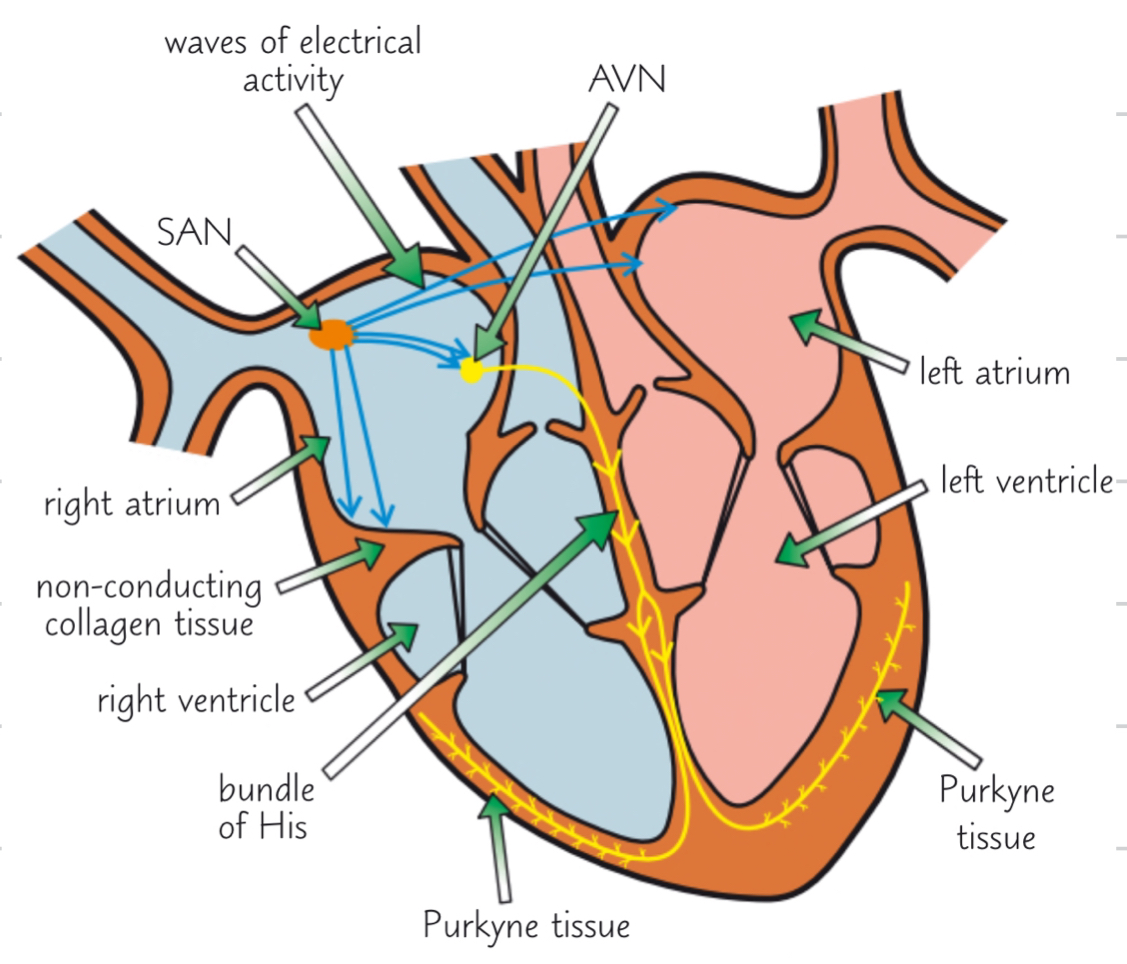
Cardiac muscle
Myogenic:
* contracts without stimulus
* rate of contraction is controlled by wave of electrical activity
Sinoatrial node:
* located in right atrium
* known as pacemaker → sets rhythm of heart beat by sending out regular electrical activity to atrial walls
Atrioventricular node:
* near border of left and right ventricle still within atria
Bundle of His:
* conductive tissue that runs through septum and up the walls of the ventricles
Purkyne tisse
* conductive tissues that go through ventricle walls
* contracts without stimulus
* rate of contraction is controlled by wave of electrical activity
Sinoatrial node:
* located in right atrium
* known as pacemaker → sets rhythm of heart beat by sending out regular electrical activity to atrial walls
Atrioventricular node:
* near border of left and right ventricle still within atria
Bundle of His:
* conductive tissue that runs through septum and up the walls of the ventricles
Purkyne tisse
* conductive tissues that go through ventricle walls
58
New cards
Regular beating of heart
1. SAN sends out a wave of electrical activity (depolarisation) across atria, causing both atria to contract at the same time
2. Band of non-conductive collagen tissue prevents the waves from being passed directly to ventricles from atria
3. waves go to AVN
4. AVN is responsible for passing the waves onto the Bundle of His → there is a slight delay before AVN reacts to make sure atria have empties before ventricles contract
5. Bundle of His conducts the waves down the septum to purkyne tissue
6. Purkyne tissue carries the waves into muscular walls of right and left ventricles causing them to contract simultaneously from bottom up
59
New cards
Control of heart rate
1. SAN generates electrical impulses that cause cardiac muscle to contract
2. the rate at which the SAN fires is unconsciously controlled by medulla oblongata
3. stimuli are detected by internal receptors
1. pressure receptors, baroreceptors, in aorta or carotid arteries, stimulated by blood pressure
2. chemical receptors, chemoreceptors, in aorta, carotid arteries or medulla, stimulated by O2 and CO2 levels and pH
4. electrical impulses from receptors are sent to medulla along sensory neurones
5. medulla processes the information and sends impulses along sympathetic neurones (increases heart rate) or parasympathetic neurones (decreasing heart rate), part of autonomic nervous system
60
New cards
High blood pressure
Baroreceptor
Impulses are sent to medulla, then send impulses along parasympathetic neurones. They secrete acetylcholine which binds to receptors on SAN
Cardiac muscle
Heart rate slows to reduce blood pressure back to normal
Impulses are sent to medulla, then send impulses along parasympathetic neurones. They secrete acetylcholine which binds to receptors on SAN
Cardiac muscle
Heart rate slows to reduce blood pressure back to normal
61
New cards
Low blood pressure
Baroreceptor
Impulses are sent to medulla, then send impulses along sympathetic neurones. They secrete noradrenaline which binds to receptors on SAN
Cardiac muscle
Heart rate speeds up to increase blood pressure back to normal
Impulses are sent to medulla, then send impulses along sympathetic neurones. They secrete noradrenaline which binds to receptors on SAN
Cardiac muscle
Heart rate speeds up to increase blood pressure back to normal
62
New cards
High O2, low CO2, high pH
Chemoreceptors
Impulses are sent to medulla, then send impulses along parasympathetic neurones. They secrete acetylcholine which binds to receptors on SAN
Cardiac muscle
Heart rate decreases so O2, CO2 and pH return back to normal
Impulses are sent to medulla, then send impulses along parasympathetic neurones. They secrete acetylcholine which binds to receptors on SAN
Cardiac muscle
Heart rate decreases so O2, CO2 and pH return back to normal
63
New cards
Low O2, high CO2, low pH
Chemoreceptors
Impulses are sent to medulla, then sends impulses along sympathetic neurones. They secrete noradrenaline, which binds to receptors on SAN
Cardiac muscle
Heart rate increases to return O2, CO2 and pH back to normal
Impulses are sent to medulla, then sends impulses along sympathetic neurones. They secrete noradrenaline, which binds to receptors on SAN
Cardiac muscle
Heart rate increases to return O2, CO2 and pH back to normal
64
New cards
Muscle structure
sarcolemma
sarcoplasm
invaginations
sarcoplasmic reticulum
lots of mitochondria and nuclei for ATP for contraction
contains myofibrils
sarcoplasm
invaginations
sarcoplasmic reticulum
lots of mitochondria and nuclei for ATP for contraction
contains myofibrils
65
New cards
Sarcolemma
cell membrane of muscle fibre cells
66
New cards
Invaginations
parts of sarcolemma folding inwards
they stick to sarcoplasm forming transverse (T) tubules
* help spread electrical impulses in sarcoplasm to reach all of muscle fibres
they stick to sarcoplasm forming transverse (T) tubules
* help spread electrical impulses in sarcoplasm to reach all of muscle fibres
67
New cards
Sarcoplasmic reticulum
Network of internal membrane through sarcoplasm
Stores and releases Ca2+ needed for contraction
Stores and releases Ca2+ needed for contraction
68
New cards
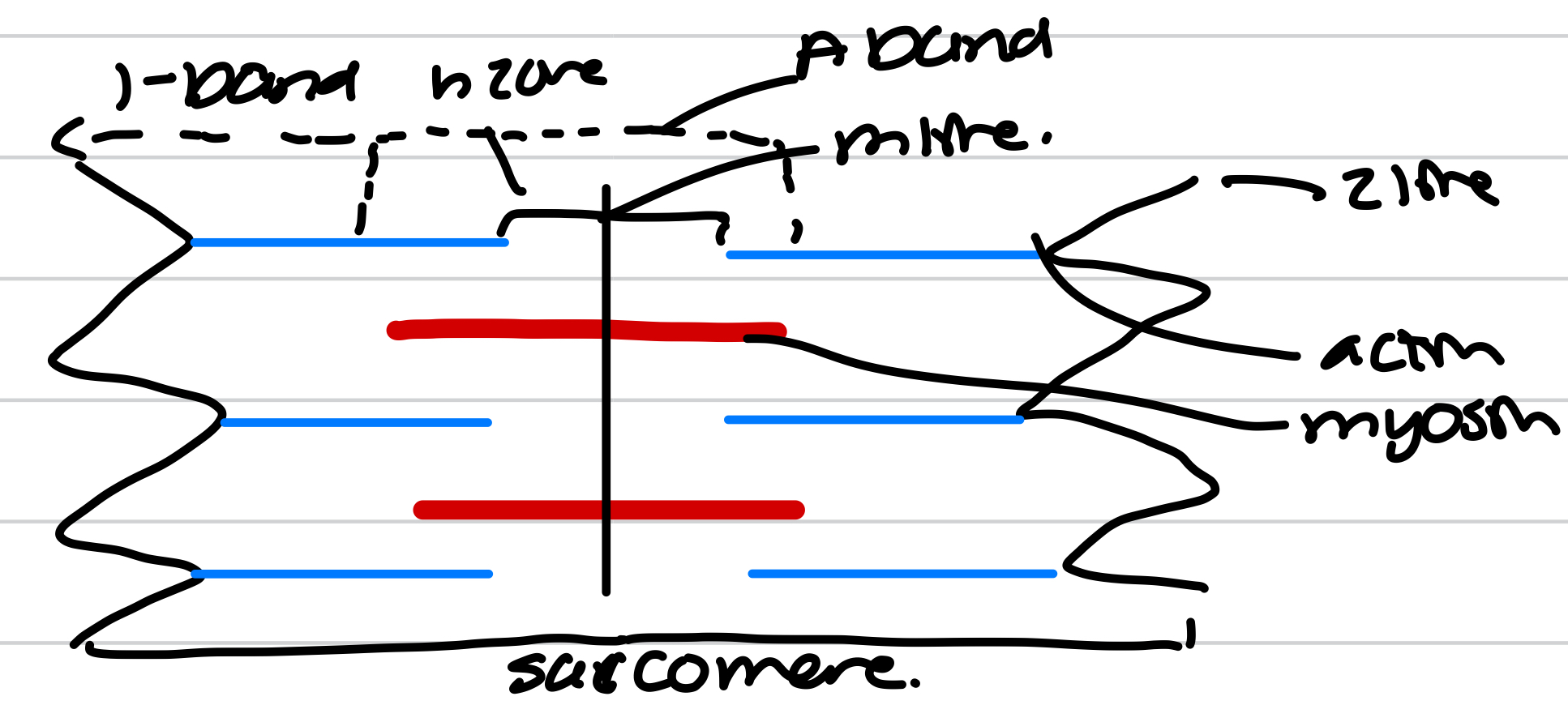
Myofibrils
Made up of thick myosin and thin actin filaments
Myosin: 2 heads and form cross bridges
Actin: troponin and tropomyosin
Under electron microscope:
* dark bands = A-bands = thick myosin and some overlapping actin
* light bands = I-bands = thin actin only
Made of many short sarcomeres
Myosin: 2 heads and form cross bridges
Actin: troponin and tropomyosin
Under electron microscope:
* dark bands = A-bands = thick myosin and some overlapping actin
* light bands = I-bands = thin actin only
Made of many short sarcomeres
69
New cards
Muscle contraction with bands
A-bands = stay the same length
I-bands = get shorter
H-zones = get shorter
Sarcomeres get shorter
I-bands = get shorter
H-zones = get shorter
Sarcomeres get shorter
70
New cards
Sliding filament theory
Myosin and actin filament slide over one another to make the sarcomere contract
Simultaneous contraction of lots of sarcomere means myofibrils and muscle fibres contract
Sarcomere return to original length as muscle relaxes
Simultaneous contraction of lots of sarcomere means myofibrils and muscle fibres contract
Sarcomere return to original length as muscle relaxes
71
New cards
Cross-bridge cycle
1. ATP binds to myosin head, causes the myosin head to be released from actin
2. ATP is hydrolysed while myosin head is unattached. ADP + Pi is formed and remain bound to myosin head
3. Energy released by hydrolysis of ATP is absorbed by myosin head changes shape. ADP + Pi are released from myosin head
4. Power stroke occurs, myosin head changes shape. This draws actin filament over myosin filament. Then binds to actin filament
72
New cards
Muscle contraction method
1. action potential arrives at the presynaptic neurone and this causes depolarisation of the membrane
2. Ca2+ channels open and Ca2+ diffuse in
3. This causes vesicles to move and fuse with presynaptic membrane. Vesicles release acetylcholine
4. Acetylcholine diffuses across the synaptic cleft and binds to receptors on sarcolemma of muscle
5. Causes Na+ channels to open and diffuse in. This causes depolarisation
6. Action potential is carried quickly into t-tubules and causes Ca2+ to be released from sarcoplasmic reticulum
7. Ca2+ binds to tropomyosin and causes to change shape
8. This exposes myosin binding site on actin
9. Myosin heads bind to actin filament forming actinomyosin cross bridges
10. Myosin heads bends pulling the actin filaments
11. ATP binds to myosin head breaking actinomyosin cross bridges
12. Hydrolysis of ATP releases energy used to recock the myosin head so it can bind to another binding site further away
73
New cards
Muscle relaxation
1. repolarisation of sarcolemma and sarcoplasmic reticulum
2. Causes Ca2+ channels to close and Ca2+ pumps remove Ca2+ into sarcoplasmic reticulum by active transport using ATP
3. Ca2+ dissociates from ATP hydrolase on myosin heads and this prevents ATP from binding so cross bridge stops
4. Ca2+ dissociates from tropomyosin causing it to change shape, covering up the myosin binding site on actin, dislodging the myosin head so cross bridges are broken
5. Actin filaments slide back and sarcomere lengthens
74
New cards
Phosphocreatine (PCr)
Serves as a high-energy phosphate reservoir for rapid regeneration of ATP
Creatine is phosphorylated during rest by ATP produced by respiration
Replaces ADP’s lost phosphate to reform ATP
Process is much faster than making new ATP
Creatine is phosphorylated during rest by ATP produced by respiration
Replaces ADP’s lost phosphate to reform ATP
Process is much faster than making new ATP
75
New cards
Slow twitch muscles
Aerobic respiration, limited by rate of O2 supply
Long periods of contraction
Slow contraction speeds
No lactate produced, not susceptible to fatigue
Lots of mitochondria and myoglobin → red colour
Heart, leg and back
Long periods of contraction
Slow contraction speeds
No lactate produced, not susceptible to fatigue
Lots of mitochondria and myoglobin → red colour
Heart, leg and back
76
New cards
Fast twitch muscles
Anaerobic respiration → not limited by blood supply
Only short bursts of energy
Fast contraction speed
Lots of glycogen but few mitochondria and myoglobin → white
Lactate produced
pH is low and muscle fatigue
Only short bursts of energy
Fast contraction speed
Lots of glycogen but few mitochondria and myoglobin → white
Lactate produced
pH is low and muscle fatigue
77
New cards
Rigor mortis
Soon after death, aerobic respiration is inhibited
ATP not available for repolarisation of sarcoplasmic reticulum and Ca2+ pumps to remove Ca2+ from myofibrils
Ca2+ remains bound to tropomyosin so binding sites are not broken down
Slowly Ca2+ diffuses out of muscle cell into surrounding tissue, decreasing conc of Ca2+ in myofibrils
Ca2+ will eventually dissociate from tropomyosin ending rigor mortis
ATP not available for repolarisation of sarcoplasmic reticulum and Ca2+ pumps to remove Ca2+ from myofibrils
Ca2+ remains bound to tropomyosin so binding sites are not broken down
Slowly Ca2+ diffuses out of muscle cell into surrounding tissue, decreasing conc of Ca2+ in myofibrils
Ca2+ will eventually dissociate from tropomyosin ending rigor mortis
78
New cards
Homeostasis
In mammals involves physiological control system that maintain the internal environmental within restricted limits
79
New cards
Negative feedback
Restores system to their original level
80
New cards
Control of body temperature - too hot
Increase in temperature
Detected by thermoreceptors
Sweating and vasodilation
Decrease in temperature
Negative feedback for heat loss and positive feedback for heat gain
Detected by thermoreceptors
Sweating and vasodilation
Decrease in temperature
Negative feedback for heat loss and positive feedback for heat gain
81
New cards
Control of body temperature - too cold
Decrease in temperature
Detected by thermoreceptors
Shivering and vasoconstriction
Increase in temp
Negative feedback for heat gain and positive feedback for heat loss
Detected by thermoreceptors
Shivering and vasoconstriction
Increase in temp
Negative feedback for heat gain and positive feedback for heat loss
82
New cards
Control of blood glucose
Pancreas detects changes in the blood glucose levels
* contain endocrine cells in the Islet of Langerhans which release the hormones insulin and glucagon to bring levels back to normal
Islets of Langerhans contain 2 different types of secretory cells:
* alpha cells which secrete glucagon
* beta cells which secrete insulin
Adrenaline is released by adrenal glands when your body anticipates danger
* this results in more glucose being released from stores of glycogen in the liver
* contain endocrine cells in the Islet of Langerhans which release the hormones insulin and glucagon to bring levels back to normal
Islets of Langerhans contain 2 different types of secretory cells:
* alpha cells which secrete glucagon
* beta cells which secrete insulin
Adrenaline is released by adrenal glands when your body anticipates danger
* this results in more glucose being released from stores of glycogen in the liver
83
New cards
Blood glucose levels increase
Blood glucose levels increase
Detected by beta cells in Islets of Langerhans
Liver cells become more permeable to glucose and enzymes are activated to convert glucose to glycogen
Glucose is removed from the blood and stored as glycogen in cells
Normal blood glucose levels
Detected by beta cells in Islets of Langerhans
Liver cells become more permeable to glucose and enzymes are activated to convert glucose to glycogen
Glucose is removed from the blood and stored as glycogen in cells
Normal blood glucose levels
84
New cards
Blood glucose levels decrease
Blood glucose levels decrease
Detected by alpha cells in the Islets of Langerhans
Alpha cells release glucagon and adrenal gland releases adrenaline
Second messenger model occurs to activate enzymes to hydrolyse glycogen
Glycogen is hydrolysed to glucose and more glucose is released back into the blood
Normal blood glucose levels
Detected by alpha cells in the Islets of Langerhans
Alpha cells release glucagon and adrenal gland releases adrenaline
Second messenger model occurs to activate enzymes to hydrolyse glycogen
Glycogen is hydrolysed to glucose and more glucose is released back into the blood
Normal blood glucose levels
85
New cards
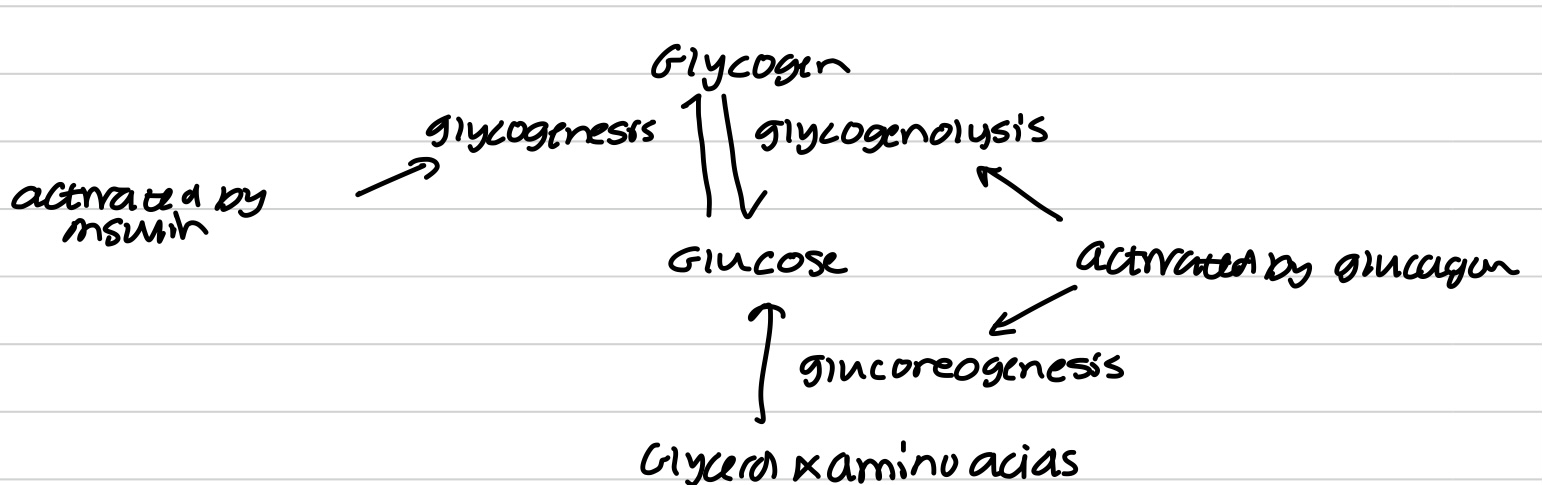
Glycogenesis
The process of excess glucose being converted to glycogen when blood glucose is higher than normal
Occurs mainly in the liver
Occurs mainly in the liver
86
New cards
Glycogenolysis
The hydrolysis of glycogen back into glucose in the liver
Occurs when blood glucose levels are lower than normal
Occurs when blood glucose levels are lower than normal
87
New cards
Gluconeogenesis
The process of creating glucose from non-carbohydrate stores in the liver
Occurs if all glycogen has been hydrolysed into glucose and body still needs more glucose
Occurs if all glycogen has been hydrolysed into glucose and body still needs more glucose
88
New cards
Action of insulin
1. Insulin binds to specific receptors on the cell membrane of liver and muscle cells. This changes the tertiary structure of the channel proteins resulting in more glucose being absorbed by facilitated diffusion
2. It increases the permeability of muscle cell membrane to glucose so takes up more glucose. This involves increasing the number of channel proteins in the cell membrane
3. Insulin also activates enzymes in the liver and muscle cells that convert glucose into glycogen
4. The cells are able to store glycogen in their cytoplasm, as an energy store → glycogenesis
5. Insulin also increase the rate of respiration of glucose, especially in muscle cells
89
New cards
Action of glucagon
1. Glucagon binds to specific receptors on cell membranes of liver cells
2. Glucagon activates enzymes in liver cells that breakdown glycogen into glucose. The glucagon binding causes a protein to be activated into adenyl cyclase and to convert ATP in a molecule, cyclic AMP (cAMP). CAMP activates an enzyme, protein kinase, that can hydrolyse glycogen into glucose → glycogenolysis
3. Glucagon also activates enzymes that are involved in the formation of glucose from glycerol and amino acids → gluconeogenesis
4. Glucagon decreases the rate of respiration of glucose in cells
90
New cards
Action of insulin and glucagon
91
New cards
Second messenger model
1. Glucagon binds to glucagon receptors
2. Once bound, it causes a change in shape to the enzyme adenyl cyclase, which activates it
3. Activated adenyl cyclase enzymes convert ATP into cyclic AMP (cAMP). CAMP is the second messenger
4. CAMP activates an enzyme, protein kinase A. Protein kinase A activates a cascade (a chain of reactions) of glycogenolysis
92
New cards
Role of adrenaline in second messenger model
Increases blood glucose levels
1. Adrenaline attaches to receptors on surface of target cells. This causes G protein to be activated and to convert ATP into cAMP
1. Adrenaline attaches to receptors on surface of target cells. This causes G protein to be activated and to convert ATP into cAMP
93
New cards
Other hormones influencing plasma glucose conc.
Thyroxine → increases the basal metabolic rate, so and increase rate of energy release is required
Corticosteroids → promote reactions that result in the synthesis of glucose from non-carbohydrate sources → glucogenesis
Corticosteroids → promote reactions that result in the synthesis of glucose from non-carbohydrate sources → glucogenesis
94
New cards
Diabetes Type I
Body is unable to produce insulin
Starts in childhood and could be result of an autoimmune disease where the beta cells were attacked
Treatment involves injections of insulin
Starts in childhood and could be result of an autoimmune disease where the beta cells were attacked
Treatment involves injections of insulin
95
New cards
Diabetes Type II
Due to receptors on target cells losing their responsiveness to insulin
Develops in adults because of obesity and poor diet
Controlled by regulating in take of carbohydrates, increasing exercise and sometimes insulin injections
Develops in adults because of obesity and poor diet
Controlled by regulating in take of carbohydrates, increasing exercise and sometimes insulin injections
96
New cards
Hyperglycaemic coma
Too much glucose
Excessive ketone production
Insulin treatment
Excessive ketone production
Insulin treatment
97
New cards
Hypoglycaemic coma
Low glucose
Brain cells starved
Treated by glucose or adrenaline
Brain cells starved
Treated by glucose or adrenaline
98
New cards
Kidneys
Osmoregulation occurs within nephrons
Nephrons are long tubules surrounded by capillaries
Approx 1 million nephrons in each kidney
Nephrons are long tubules surrounded by capillaries
Approx 1 million nephrons in each kidney
99
New cards
Nephron structure
1. Renal capsule with glomerulus
2. Proximal convoluted tubule
3. Loop of Henle
4. Distal convoluted tubule
5. Collecting ducts
100
New cards
Function of nephron
Filter blood to remove waste and selectively reabsorb useful substances back into blood