women repro
1/30
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
31 Terms
order of the phases
Phases/ Events
Menstruation
Follicular Phase
Ovulation
Luteal Phase
Menstruation

Marks the first day of a new menstrual cycle
Discharge of bloody fluid containing endometrial and blood cells
Typically lasts 3-5 days
Triggered by decline in estrogen and progesterone (especially progesterone) from the last cycle
Vasoconstriction causes endometrial tissue to die
Uterine contractions cause it to be expelled
The Early Follicular Phase

Follicles contained in the ovaries are small
Because of this, estradiol levels are very low
Cervical mucus is dry
The Late Follicular Phase

The Late Follicular Phase
Gradual rise in FSH stimulates the ovarian follicles
Follicles compete with each other for dominance
A dominant follicle (occasionally 2) will mature, becoming a fluid-filled Graafian follicle, which contains an ovum (egg)
As follicles grow, they release more and more estradiol
Estradiol stimulates the thickening of the endometrium (lining of the uterus)
Estradiol also stimulates the cervix to produce increasing amounts of cervical mucus
ovulation
Once estradiol levels reach a certain threshold, a surge of LH is triggered (related to the frequency of GnRH pulses)
LH matures the egg and weakens the follicular wall, facilitating ovulation
Once released, the ovum is swept up into the fallopian tube
The Luteal Phase

Corpus luteum: solid body formed after the ovum is released into the fallopian tube
Produces significant amounts of progesterone, which is critical to making the endometrium receptive to implantation of a blastocyst (i.e. pre-embryo)
High estradiol & progesterone inhibit FSH & LH
High progesterone causes cervical mucus to dry up
If ovum is not fertilized, corpus luteum disintegrates after 14ish days, resulting in a drop of estradiol and progesterone (resulting in menstruation)
Why is the Average Age of Menarche Declining???

In the past:
Improving living standards, nutrition
More recent:
Higher rates of obesity
Exposure to endocrine-disrupting chemicals (https://www.endocrine.org/topics/edc)
Greater exposure to light
Consequences: increased risk of estrogen-dependent cancers
How do I know when/ if I’m ovulating?

Signs of ovulation
Lots of “egg-white” cervical mucus followed by sudden drying up
Increase in libido leading up to ovulation
Ovarian pain during ovulation (also known as “mittelschmertz”)
Mid-cycle increase in basal body temperature
Period begins 12-15 days after suspected ovulation
Note that in healthy women, about 10% of menstrual cycles are anovulatory (i.e. ovulation doesn’t occur)
What about the Pill?

Most birth control pills contain both synthetic estrogen and progesterone (called progestogen)
Estrogen and progesterone feed back in the HPG axis to prevent FSH and LH release
Result: no ovulation
The progestogen also prevents the production of fertile cervical mucus
During pill-free intervals, you experience withdrawal from estrogen and progestogen, resulting in bleeding
How do IUDs work?

Both types of IUDs are inserted in the uterus
The presence of an IUD in the uterus creates an inflammatory reaction that prevents fertilization of the ovum by sperm
All phases of the menstrual cycle still occur
Hormonal IUDs also release a progestogen, which prevents fertile cervical mucus and prevents thickening of the uterine lining
Why aren’t my periods regular?

Occasional irregularity is nothing to worry about but chronically irregular periods is something to look into
Possible causes of menstrual irregularity
Stress can cause occasional irregularity
Thyroid dysfunction
Excessive exercise
Eating disorders
Uncontrolled diabetes
Primary ovarian insufficiency
Most common: polycystic ovarian syndrome
Polycystic Ovarian Syndrome (PCOS)
5-10% of women
Symptoms:
2 out of 3 of the following criteria:
1.Menstrual irregularity
2.Signs of elevated testosterone (e.g. acne, excess body hair, hair loss)
3.Polycystic ovaries (via ultrasound)
Responds well to low glycemic index diet & exercise
The History of PMS

1931: Karen Horney writes a paper entitled “Premenstrual Tensions”
1953: Dr. Katharina Dalton, British gynecologist, coined the term “premenstrual syndrome”
Devoted her career to researching, writing about and treating PMS
Believed PMS was due to deficient progesterone
Estimated rate to be 30%
Testified in over 50 trials in which the defendant had committed crimes in the premenstrual phase
1931: Karen Horney writes a paper entitled “Premenstrual Tensions”
1953: Dr. Katharina Dalton, British gynecologist, coined the term “premenstrual syndrome”
1987: “Late luteal phase disorder” appears in the Appendix of the Diagnostic and Statistical Manual of Mental Disorders (DSM)
2012: Premenstrual Dysphoric Disorder (PMDD) ‘upgrades’ to the front of the DSM
Inclusion of PMDD in the DSM:
A Controversial Decision

ARGUMENTS AGAINST |
Pathologizes normal variations in mood |
Allows big pharma to re-patent old antidepressants for this new purpose |
Encourages the depiction of women as highly emotional and irrational |
Inclusion of PMDD in the DSM:
A Controversial Decision

ARGUMENTS FOR |
Existence is supported by a large body of research |
Facilitates diagnosis, treatment, and research |
Validates the experiences of many women |
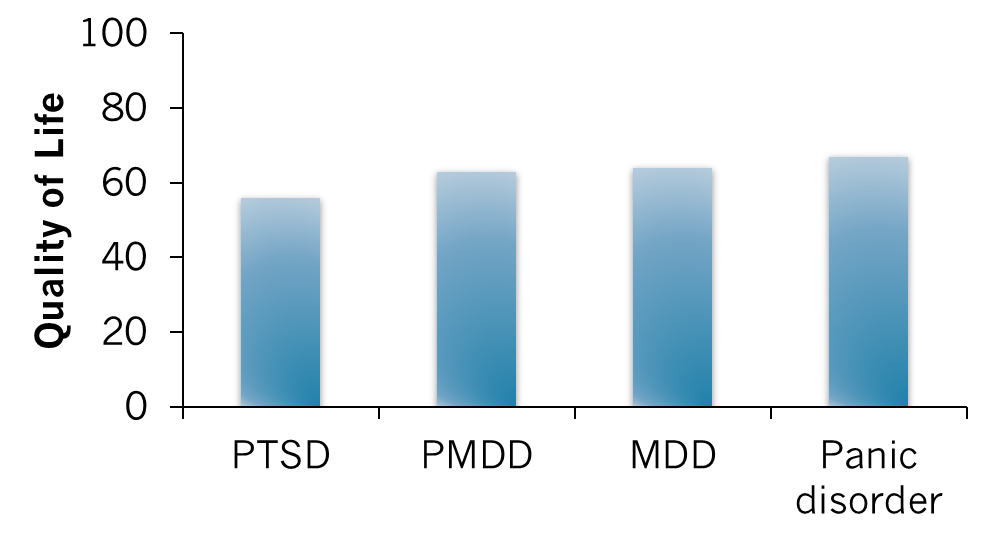
Quality of Life in PMDD

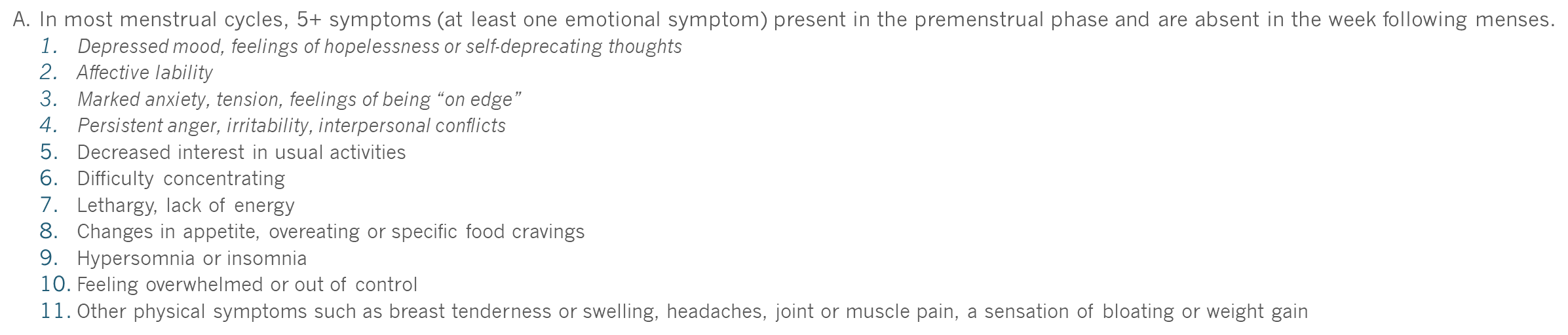
DSM-5 Criteria for PMDD

A. In most menstrual cycles, 5+ symptoms (at least one emotional symptom) present in the premenstrual phase and are absent in the week following menses.
1.Depressed mood, feelings of hopelessness or self-deprecating thoughts
2.Affective lability
3.Marked anxiety, tension, feelings of being “on edge”
4.Persistent anger, irritability, interpersonal conflicts
5.Decreased interest in usual activities
6.Difficulty concentrating
7.Lethargy, lack of energy
8.Changes in appetite, overeating or specific food cravings
9.Hypersomnia or insomnia
10.Feeling overwhelmed or out of control
11.Other physical symptoms such as breast tenderness or swelling, headaches, joint or muscle pain, a sensation of bloating or weight gain
●
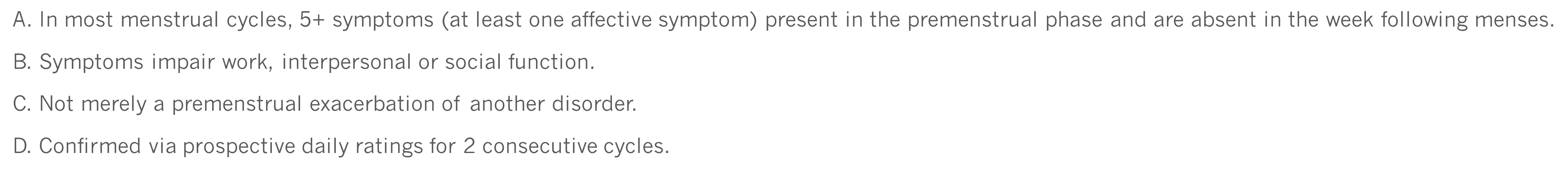
DSM-5 Criteria for PMDD

A. In most menstrual cycles, 5+ symptoms (at least one affective symptom) present in the premenstrual phase and are absent in the week following menses.
B. Symptoms impair work, interpersonal or social function.
C. Not merely a premenstrual exacerbation of another disorder.
D. Confirmed via prospective daily ratings for 2 consecutive cycles.
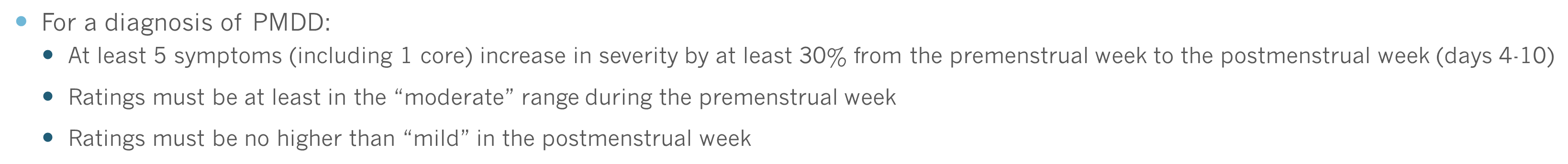
Interpreting Daily ratings

For a diagnosis of PMDD:
At least 5 symptoms (including 1 core) increase in severity by at least 30% from the premenstrual week to the postmenstrual week (days 4-10)
Ratings must be at least in the “moderate” range during the premenstrual week
Ratings must be no higher than “mild” in the postmenstrual week
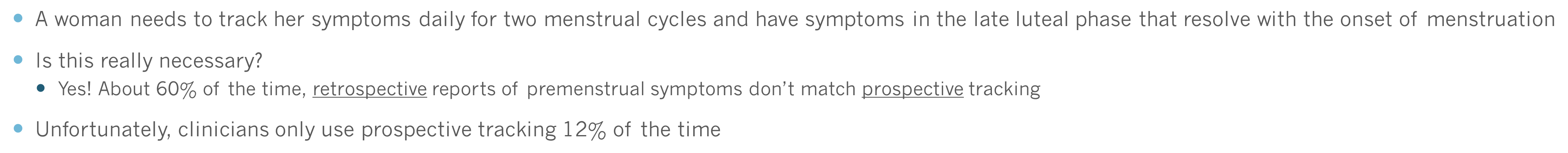
PMDD Assessment:
Why Prospective Ratings are Critical

A woman needs to track her symptoms daily for two menstrual cycles and have symptoms in the late luteal phase that resolve with the onset of menstruation
Is this really necessary?
Yes! About 60% of the time, retrospective reports of premenstrual symptoms don’t match prospective tracking
Unfortunately, clinicians only use prospective tracking 12% of the time

PMDD Prevalence
Strict DSM-5 diagnosis
1-2%1
Clinically significant but sub-threshold symptoms:
13-19%2
E.g. <5 symptoms
Prevalence of PMDD Symptoms


Suicidality & PMDD

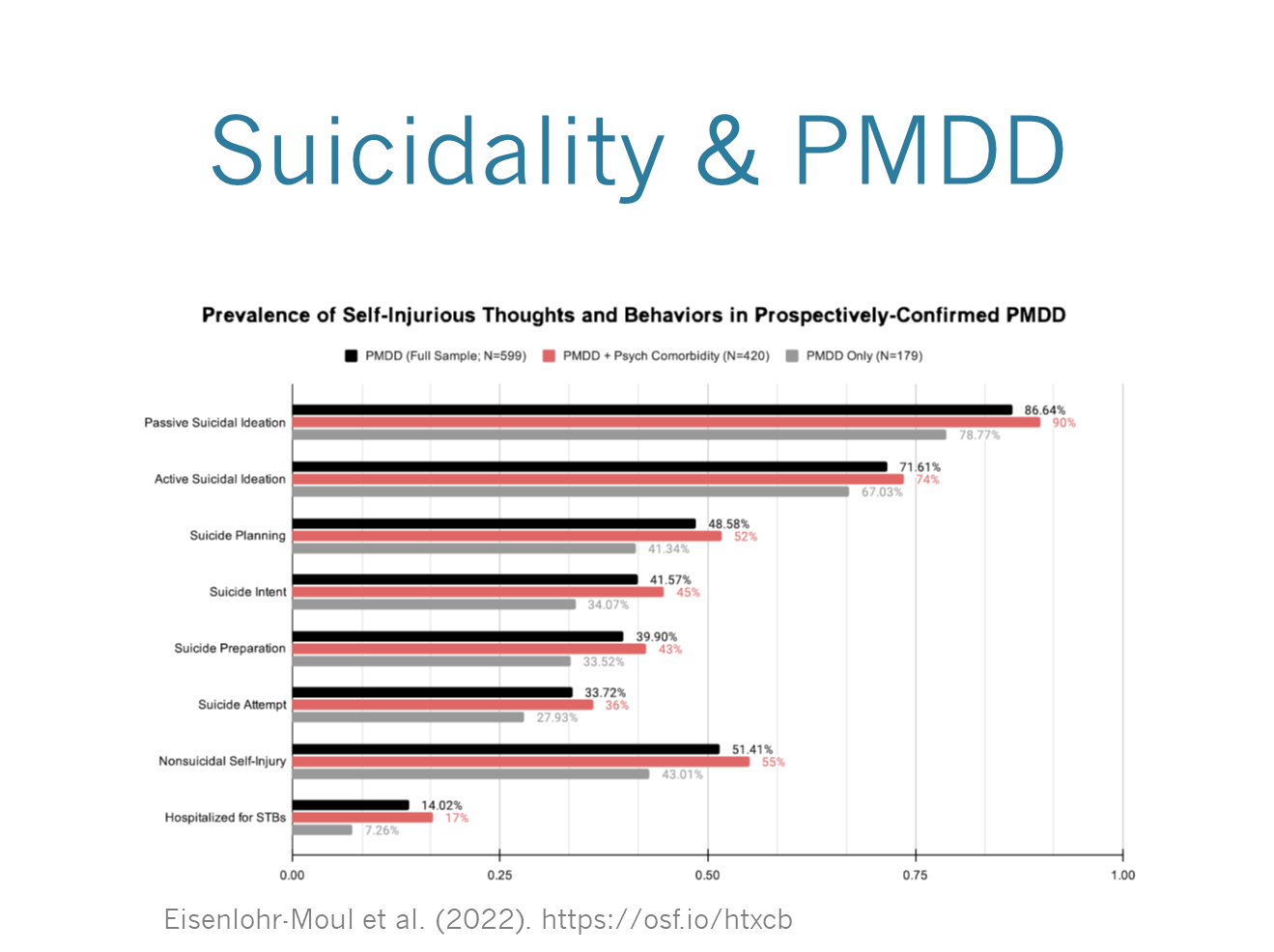
The Argument For Including Suicidality in the DSM

Seems to be highly prevalent in those with PMDD
Would encourage clinicians to assess suicidal risk
Identify the need for intervention
Would prevent misdiagnosis of other conditions in which suicidality is listed (major depression, bipolar, borderline personality disorder)
The Argument Against Including Suicidality in PMDD

Limitations of current research
Not prospectively-confirmed PMDD
Suicidality not tracked across the cycle
Questions to be answered
What is the prevalence of suicidality in prospectively-confirmed PMDD?
Does it follow the same on-off pattern as other PMDD symptoms?
How is the prevalence of PMDD affected by including it?
What is the clinical utility of adding it? Does it lead to improved diagnosis and treatment?
PMDD Subtypes?
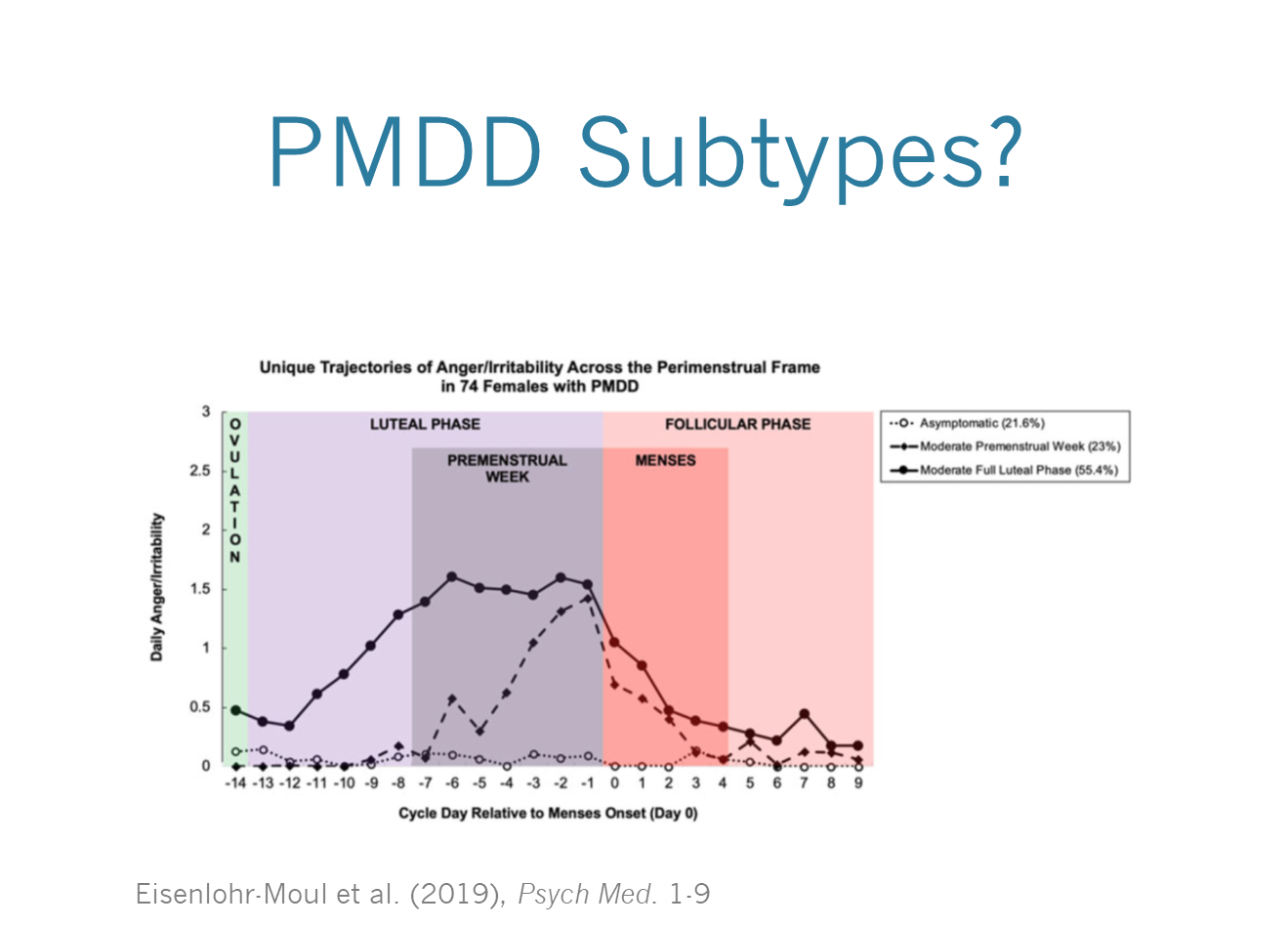
PMDD Subtypes
Onset of symptoms could occur:
At the start of the luteal phase
One week into the luteal phase
Offset of symptoms could occur:
At the start of the follicular phase
One week into the follicular phase
Suggests the neurobiological effects of hormones may be delayed or slow to resolve in some women
Also, prominent symptoms may differ from person to person or cycle to cycle
PMDD & Hormonal Levels

One thing that these researchers have pretty clearly established so far: women with PMDD do not have abnormal hormone levels
Estradiol
Progesterone
LH, FSH
Sex hormone binding globulin
Instead, it’s thought that PMDD is an abnormal response to normal hormonal changes
Leuprolide Study: Part 1

20 women with PMS (age 21-45)
Confirmed with prospective mood ratings for 3 consecutive cycles showing 30%+ increase in symptoms during premenstrual phase
Randomly assigned to receive 3 monthly injections of
Leuprolide acetate (GnRH agonist) OR
Saline placebo
PMS symptoms rated daily using a visual analog scale and Daily Rating Form
Blood samples drawn every 2 weeks
What is Leuprolide?

Results

A GnRH agonist
Results in a big increase in estrogen in the short-term
High estrogen feeds back to shut down the axis
Result: HPG axis shutdown
At baseline (before receiving either Leuprolide or placebo), both groups show an increase in symptoms during the premenstrual phase

After treatment, only the placebo group shows an increase in symptoms during the premenstrual phase

Conclusion: no reproductive hormones = no PMS
