GI Lecture Bio 221
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
What are the main functions of the gastrointestinal (GI) tract, including its immune and liver-related roles?
Ingestion – takes in food.
Secretion – releases enzymes, acid, bile, and mucus into the lumen.
Motility – mixes and propels contents (peristalsis and segmentation).
Digestion – breaks food down mechanically and chemically.
Absorption – moves nutrients, water, and electrolytes into blood/lymph.
Excretion – eliminates undigested material and metabolic wastes as feces.
Immune functions – gut-associated lymphoid tissue (GALT), microbiota, and mucosal barrier help protect against pathogens.
Liver functions (related to GI) – produces bile for fat digestion, processes and stores absorbed nutrients, detoxifies substances, and helps regulate blood glucose and plasma proteins.
How is the gastrointestinal (GI) tract assisted in digestion?
Accessory digestive organs:
Salivary glands: Produce saliva and enzymes for initial digestion
Liver: Produces bile for fat emulsification
Gallbladder: Stores and releases bile
Pancreas: Produces digestive enzymes and bicarbonate
GI secretions:
Enzymes: Break down carbohydrates, proteins, and fats
Mucus: Lubricates and protects GI lining
Acid: Aids protein digestion and kills pathogens
Bile: Emulsifies fats for absorption
Hormones: Regulate digestive processes
What are the two neural pathways that regulate gastrointestinal processes?
GI processes are regulated by:
Enteric nervous system (ENS): Local control of GI motility and secretions
Autonomic nervous system (ANS):
Parasympathetic: Stimulates GI activity
Sympathetic: Inhibits GI activity
Which neural pathway that regulates gastrointestinal processes does not involve the central nervous system?
The enteric nervous system (ENS) mediates short reflexes entirely within the gut wall without requiring input from the central nervous system (CNS).
Name at least three hormones that regulate gastrointestinal processes.
GI-regulating hormones include:
Gastrin – stimulates gastric acid secretion and motility
Secretin – stimulates bicarbonate release from the pancreas
Cholecystokinin (CCK) – stimulates bile and pancreatic enzyme release
Gastric inhibitory peptide (GIP) – inhibits gastric motility and secretion
Motilin – stimulates migrating motor complexes for intestinal motility
What are the three phases of control of gastrointestinal regulatory processes?
GI regulatory control occurs in three phases:
Cephalic phase: Triggered by sight, smell, thought, or taste of food
Gastric phase: Triggered by food entering the stomach
Intestinal phase: Triggered by chyme entering the small intestine
What are the four layers of the wall of many gastrointestinal organs, from innermost to outermost?
The four layers of the wall of many gastrointestinal organs are:
Mucosa – the innermost layer, responsible for secretion, absorption, and protection.
Submucosa – a connective tissue layer containing blood vessels, lymphatics, and nerves.
Muscularis externa – smooth muscle layer responsible for peristalsis and segmentation.
Serosa (or adventitia in some regions) – the outermost layer; the serosa forms the peritoneum, while the adventitia is a connective tissue layer that anchors organs.
What are the two layers of the peritoneum formed by the tunica serosa?
The tunica serosa forms the peritoneum, which has two layers: the parietal peritoneum, which lines the abdominal cavity, and the visceral peritoneum, which covers the abdominal organs.
What are the functions of the tongue?
Functions of the tongue:
Mechanical digestion: Helps chew and mix food, forming it into a bolus
Swallowing: Pushes food into the pharynx to initiate swallowing
Taste: Houses taste buds to detect flavors
Speech: Assists in articulation and sound formation
What is the medical term for chewing?
The medical term for chewing is mastication.
What are the main functions of saliva?
Saliva lubricates and moistens food, begins the digestion of carbohydrates, contributes to the digestion of fats, protects the oral cavity and teeth, and aids the process of tasting food.
What are the functions of saliva in digestion, oral health, and other processes?
Saliva functions:
Lubrication & swallowing:
Water and mucus moisten food for easier swallowing
Mucin helps form the bolus
Aids in speech
Helps disperse molecules over the tongue for taste
Digestion:
Salivary amylase: Begins starch digestion
Lingual lipase: Initiates fat digestion
pH balance:
Bicarbonate: Buffers oral pH
Protection & immune defense:
Lysozyme: Antimicrobial enzyme
Immunoglobulin A (IgA): Provides immune defense
What controls the secretion of saliva?
Salivary secretion is primarily controlled by the parasympathetic division of the autonomic nervous system, which increases saliva production in response to stimuli such as:
Taste
Smell
Chewing
Thought of food
What is the medical term for swallowing?
The medical term for swallowing is deglutition.
What initiates the swallowing process?
The swallowing process is initiated voluntarily when the tongue pushes the bolus of food from the mouth into the oropharynx.
What type of motility is swallowing considered to be?
Swallowing is considered a motility process that begins with a voluntary phase and then continues as an involuntary reflex involving coordinated peristaltic contractions.
What are the main functions of the stomach?
Stomach functions:
Storage: Holds ingested food
Mechanical digestion: Mixes food with gastric secretions to form chyme
Chemical digestion: Begins protein digestion
Secretion: Produces intrinsic factor for vitamin B₁₂ absorption
Regulation: Controls the rate at which chyme empties into the small intestine
What is the importance of intrinsic factor?
Intrinsic factor is important because it is required for the absorption of vitamin B₁₂ in the ileum, and vitamin B₁₂ is necessary for normal red blood cell production.
What regulates hydrochloric acid (HCl) secretion in the stomach?
Stimulation of HCl secretion:
Neural: Acetylcholine from vagal nerves
Hormonal: Gastrin and histamine
Mechanical/Chemical: Food in the stomach, distension, presence of proteins
Inhibition of HCl secretion:
Low stomach pH
Intestinal signals: Secretin and cholecystokinin (CCK)
What are two ways the stomach is protected from damage by hydrochloric acid?
The stomach is protected by a thick mucus and bicarbonate barrier that coats the mucosa and by tight junctions and rapid turnover of the epithelial cells lining the stomach.
What converts pepsinogen to pepsin, and what is the action of pepsin?
Pepsinogen is converted to pepsin by hydrochloric acid and by already formed pepsin, and pepsin acts as a proteolytic enzyme that digests proteins by breaking peptide bonds.
What is gastrin, where is it released from, what stimulates and inhibits it, and what are its major digestive functions?
Gastrin is a hormone released by G cells in the stomach during the gastric phase of digestion. It is stimulated by stomach distension, the presence of proteins and amino acids, and vagal (parasympathetic) stimulation, and is inhibited by very low pH (high acidity). Gastrin increases secretion of Hydrochloric acid (HCl) from parietal cells, stimulates gastric motility to mix and move food, promotes growth and repair of the gastric mucosa, and increases motility in the lower GI tract to coordinate digestion. Overall, gastrin prepares the stomach for efficient chemical and mechanical digestion.
What causes the release of gastrin?
Gastrin release is stimulated by distension of the stomach, by the presence of peptides and amino acids in the stomach, by vagal stimulation, and by a relatively high stomach pH.
In which direction does the peristaltic wave of contraction occur in the stomach?
The peristaltic wave of contraction in the stomach begins in the fundus and body and passes toward the pylorus.
When the stomach contracts, the stomach contents are moved into which structure?
When the stomach contracts, the stomach contents are moved into the duodenum through the pyloric sphincter.
Which factors influence gastric motility and gastric emptying?
Gastric motility and emptying are influenced by multiple factors:
Stomach factors: the volume and composition of stomach contents.
Duodenal factors: distension, pH, fat content, and osmolarity in the duodenum.
Hormonal factors: cholecystokinin (CCK), secretin, and gastric inhibitory peptide (GIP).
Neural factors: autonomic and enteric nervous system reflexes.
These factors work together to regulate the rate and strength of gastric contractions and chyme emptying into the duodenum.
What are the major functions of the liver?
he liver produces bile, metabolizes and stores carbohydrates, lipids, and proteins, detoxifies drugs and toxins, synthesizes plasma proteins, stores vitamins and iron, and helps regulate blood glucose levels.
What are the liver cells called?
The liver cells are called hepatocytes.
Which two blood vessels bring blood into the liver?
Blood is brought into the liver by the hepatic artery and the hepatic portal vein.
Where does the blood from the hepatic artery and hepatic portal vein mix, and into which vessels does it flow before reaching the inferior vena cava?
Blood from the hepatic artery and hepatic portal vein mixes in the liver sinusoids, then flows into central veins, then into hepatic veins, and finally drains into the inferior vena cava.
What is the importance of cytochrome P450 enzymes in the liver?
Cytochrome P450 enzymes are produced in the liver (mainly in hepatocytes) and they detoxify many drugs, toxins, and hormones, metabolize medications, and convert fat-soluble substances into water-soluble forms so they can be excreted, mainly in urine or sometimes in bile.
What are the major components of bile?
Bile is composed mainly of bile salts, bile pigments such as bilirubin, cholesterol, phospholipids, and various electrolytes.
What is the source of bilirubin?
Bilirubin is produced from the breakdown of heme, which comes from old red blood cells.
Where is bilirubin conjugated?
Bilirubin is conjugated in the liver by hepatocytes.
In this context, “conjugated” means that a chemical group (glucuronic acid) is added to bilirubin, which:
Makes it water-soluble
Allows it to be secreted into bile and pass safely through the intestines
Facilitates excretion in feces
Where are bilirubin and urobilinogen excreted?
Conjugated bilirubin is secreted into bile and delivered to the small intestine. In the intestine, bacteria convert it to urobilinogen. Most urobilinogen is further converted to stercobilin and excreted in feces, while a small portion is reabsorbed into the bloodstream and excreted by the kidneys as urobin in the urine.
What is the function of the gallbladder?
The gallbladder functions to store bile, concentrate it, and release it into the small intestine when needed for digestion.
What is the main stimulus for the release of bile from the gallbladder?
The main stimulus for bile release from the gallbladder is the hormone cholecystokinin (CCK), which is released from the small intestine in response to fats in the chyme.
What is the main action of bile in digestion?
The main action of bile is to emulsify fats, breaking large fat droplets into smaller ones to facilitate fat digestion and absorption.
What are the main components of pancreatic juice?
Pancreatic juice contains digestive enzymes for carbohydrates, proteins, fats, and nucleic acids, as well as bicarbonate and water.
Which pancreatic enzyme is involved in carbohydrate digestion?
The pancreatic enzyme involved in carbohydrate digestion is pancreatic amylase.
Which pancreatic enzymes are involved in lipid digestion?
Lipid digestion is carried out mainly by pancreatic lipase, with the assistance of colipase.
Which pancreatic enzymes are involved in protein digestion?
Protein digestion is carried out by trypsin, chymotrypsin, elastase, and carboxypeptidases.
Which pancreatic enzymes are involved in nucleic acid digestion?
Nucleic acid digestion is carried out by ribonuclease, which digests RNA, and deoxyribonuclease, which digests DNA.
What is the importance of trypsin?
Trypsin is important because it digests proteins and also activates other pancreatic zymogens, such as chymotrypsinogen and procarboxypeptidase.
Zymogens: inactive (non-working) forms of digestive enzymes that are produced and secreted by the pancreas.
What controls the secretion of pancreatic juice?
The secretion of pancreatic juice is controlled by the hormones secretin and cholecystokinin (CCK), which are released from the small intestine, and by parasympathetic stimulation through the vagus nerve.
What are the three segments of the small intestine?
The three segments of the small intestine are the duodenum, the jejunum, and the ileum.
What are brush border enzymes?
Brush border enzymes are digestive enzymes attached to the microvilli of small intestinal epithelial cells, and they perform the final steps of digestion of carbohydrates and proteins.
Besides enzymes, what else does the small intestine secrete?
Besides enzymes, the small intestine secretes mucus, water, and bicarbonate-rich intestinal juice.
How are carbohydrates and amino acids transported from the intestines to the bloodstream?
Carbohydrates → monosaccharides and proteins → amino acids in the small intestine.
Enter intestinal epithelial cells (enterocytes) via carrier-mediated transport, often coupled to sodium (secondary active transport).
Exit enterocytes into capillaries in the villi by facilitated diffusion.
Capillaries merge into the hepatic portal vein, carrying nutrient-rich blood directly to the liver for processing (glucose regulation, protein synthesis, detoxification).
Step-by-Step Flow:
Lumen → Enterocyte → Villi Capillary → Hepatic Portal Vein → Liver
Memory Trick:
“Sodium helps nutrients in → nutrients go to liver first.”
What are the main steps in the breakdown and absorption of fats?
Dietary fats are emulsified by bile salts in the small intestine. Pancreatic lipase then breaks triglycerides into fatty acids and monoglycerides. These combine with bile salts to form micelles, which deliver the lipids to enterocytes (intestinal epithelial cells). Inside the enterocyte the lipids are reassembled into triglycerides and packaged into chylomicrons, which exit the cell by exocytosis, enter the lacteals, travel through the lymphatic system, and eventually drain into the bloodstream through the thoracic duct into the left subclavian vein.
How do fats ultimately reach the bloodstream?
Fats reach the bloodstream when chylomicrons enter the lacteals of the intestinal villi, travel through the lymphatic system, and then drain into the venous circulation via the thoracic duct.
How do vitamins enter the bloodstream?
Water-soluble vitamins are absorbed directly into blood capillaries by diffusion or carrier-mediated transport, while fat-soluble vitamins are absorbed with dietary fats into chylomicrons and then enter the bloodstream via the lymphatic system.
What happens after these nutrient molecules are absorbed?
Water-soluble → portal vein → liver; fat-soluble → lymph → blood → liver later.
What are the two main forms of motility in the small intestine?
The two main forms of motility in the small intestine are segmentation, which mixes intestinal contents, and peristalsis, which propels contents forward through the intestine.
What controls motility in the small intestine?
Motility in the small intestine is controlled by the enteric nervous system, the autonomic nervous system, and gastrointestinal hormones such as cholecystokinin (CCK) and motilin.
What is the major function of the large intestine, also called the colon?
The major function of the large intestine is to absorb water and electrolytes, form and store feces, and provide a habitat for intestinal bacteria.
What are two types of motility in the colon?
The two types of motility in the colon are haustral contractions, which are segmenting movements that mix contents, and mass movements, which are powerful peristaltic waves that move feces toward the rectum.
The colon is the main portion of the large intestine.
What triggers the defecation reflex, and how can this reflex be inhibited?
The defecation reflex is triggered by distension (stretching or expansion of a hollow organ due to pressure from inside) of the rectum by feces. It can be voluntarily inhibited by contracting the external anal sphincter and the pelvic floor muscles.
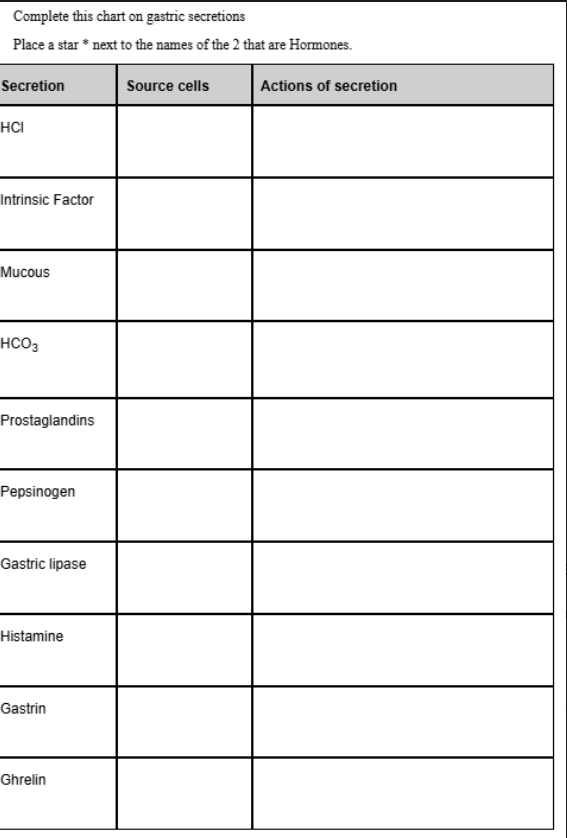
Fill in the blank.
Secretion | Source cells | Actions of secretion |
|---|---|---|
HCl | Parietal (oxyntic) cells of stomach | Creates acidic pH; activates pepsinogen → pepsin; denatures proteins; kills microbes. |
Intrinsic factor | Parietal cells | Binds vitamin B₁₂ in stomach → needed for B₁₂ absorption in ileum. |
Mucous | Surface mucous cells & mucous neck cells | Forms protective mucous layer that lubricates and shields epithelium from acid and pepsin. |
HCO₃⁻ (bicarbonate) | Surface mucous cells | Neutralizes acid at epithelial surface; helps maintain near-neutral pH at mucosa. |
Prostaglandins | Mucosal cells (and submucosal cells) | Increase mucous + HCO₃⁻ secretion, increase mucosal blood flow, and reduce acid secretion → protect gastric mucosa. |
Pepsinogen | Chief (peptic) cells | Inactive enzyme converted by HCl to pepsin → begins protein digestion. |
Gastric lipase | Chief cells | Begins digestion of triglycerides (fats) in the stomach. |
Histamine | Enterochromaffin-like (ECL) cells | Stimulates parietal cells to secrete HCl. |
Gastrin★ | G cells in antrum & duodenum | Hormone that increases HCl secretion, stimulates gastric motility, mucosal growth, and LES tone. |
Ghrelin★ | P/D₁ cells (A-like cells) in gastric fundus | “Hunger hormone”: increases appetite; stimulates growth hormone release; promotes gastric motility. |
What are the main regulators of gastrointestinal (GI) activity?
Hormonal:
CCK (Cholecystokinin): Stimulates bile and pancreatic enzyme secretion; slows gastric emptying.
Gastrin: Stimulates gastric acid secretion and gastric motility.
Motilin: Stimulates migrating motor complexes (intestinal motility).
Ghrelin: Stimulates appetite and gastric motility.
Somatostatin: Inhibits gastric acid secretion and other GI hormones.
Neural:
Autonomic nervous system:
Sympathetic: Generally inhibits GI activity.
Parasympathetic: Stimulates GI activity.
Reflexes:
Long reflexes: Involve CNS integration (e.g., sight, smell, thought of food).
What are the layers of the gastrointestinal (GI) organ walls and their main features?
GI wall layers (from inside to outside):
Tunica mucosa:
Epithelium lining the lumen
Functions in secretion, absorption, and protection
Tunica submucosa:
Connective tissue containing blood vessels, lymphatics, and nerves
Tunica muscularis:
Smooth muscle layers (usually inner circular & outer longitudinal)
Responsible for peristalsis and mixing
Tunica serosa/adventitia:
Connective tissue forming the outer layer
Serosa forms the peritoneum with two layers:
Visceral peritoneum (covers organs)
Parietal peritoneum (lines the abdominal wall)
How does swallowing (deglutition) work?
1. Voluntary phase: Tongue pushes the bolus from the mouth into the oropharynx.
2. Reflex phase: Pressure in the oropharynx triggers peristalsis, a series of waves of esophageal contractions that move the bolus toward the stomach.
What is the role of teeth in digestion?
Teeth (mastication): Chew and break down food into smaller pieces, aiding mechanical digestion.
What are the major stomach secretions, their sources, and functions?
Stomach secretions by cell type:
Parietal cells:
HCl: Acidifies stomach, activates pepsin
Intrinsic factor: Needed for vitamin B₁₂ absorption
Chief cells:
Pepsinogen: Converted to pepsin for protein digestion
Gastric lipase: Initiates fat digestion
Mucosal cells / Surface epithelial cells:
Mucus: Protects stomach lining
HCO₃⁻ (bicarbonate): Buffers stomach acid
Enteroendocrine cells:
G cells: Gastrin – stimulates HCl secretion
D cells: Somatostatin – inhibits HCl and gastrin
ECL (enterochromaffin-like) cells: Histamine – stimulates HCl
Fundus cells: Ghrelin – stimulates appetite
Prostaglandins: Protect mucosa, stimulate mucus and bicarbonate
What are the functions of hydrochloric acid (HCl) in the stomach, and how is it produced by parietal cells?
In the stomach, HCl:
Denatures proteins to help enzymes digest them.
Has antimicrobial effects, killing many ingested pathogens.
Converts pepsinogen to pepsin, activating this protein-digesting enzyme.
HCl is produced by parietal cells as follows:
CO₂ + H₂O form carbonic acid (H₂CO₃), which dissociates into H⁺ and HCO₃⁻ (bicarbonate).
H⁺ ions are pumped into the stomach lumen, creating acidity.
Chloride (Cl⁻) follows H⁺ into the lumen and combines with it to form HCl.
HCO₃⁻ is transported into the bloodstream, causing a temporary “alkaline tide” after meals.
Which factors increase the release of hydrochloric acid (HCl) in the stomach?
HCl release from parietal cells is increased by:
Parasympathetic stimulation from higher brain centers, such as the sight, smell, taste and thought of food.
Stretch (distension) of the stomach, which activates local and vagovagal reflexes.
Gastrin, a hormone released from G cells in the stomach, which stimulates parietal cells to secrete more HCl.
Histamine, released from enterochromaffin-like (ECL) cells, which binds to H₂ receptors on parietal cells and increases HCl secretion.
Caffeine, which can stimulate gastric acid secretion.
How do mucus, bicarbonate, and prostaglandins help protect the stomach from acid damage?
Mucus and bicarbonate (HCO₃⁻) coat the epithelial cells and protect the stomach wall from damage by hydrochloric acid (HCl).
Prostaglandins increase the secretion of bicarbonate and mucus, which strengthens this protective barrier.
Pepsiongoen-pepsin-proteolytic enzyme- catbolizes protein
What are the actions of gastrin, and what factors stimulate or inhibit its release?
Actions of gastrin:
Increases gastric secretions, including HCl, pepsinogen, and mucus.
Increases gastric motility.
Stimuli for gastrin release:
Increased parasympathetic activity.
Cephalic influences such as sight, smell, taste, or thought of food.
Presence of food in the stomach.
Inhibitors of gastrin release:
Acid in the duodenum.
Somatostatin, which suppresses gastrin secretion.
What is the direction and purpose of gastric motility, and why is intrinsic factor important?
Gastric motility:
Peristaltic waves of contraction travel from the fundus to the pylorus.
These waves mix stomach contents and allow a slow, controlled release of chyme into the duodenum.
Intrinsic factor:
Required for absorption of vitamin B₁₂ in the ileum.
Vitamin B₁₂ is necessary for normal red blood cell production.
What factors influence gastrointestinal motility?
Factors that increase gastrointestinal motility include motilin, parasympathetic activity, gastrin, stomach distension, and the presence of food in the stomach (especially proteins). Factors that inhibit motility include increased sympathetic activity, low pH, intestinal distension, somatostatin, and hormones such as CCK and secretin which slow gastric emptying.
What are the major functions of the liver?
The liver performs multiple essential functions:
Produces bile to aid in fat digestion and absorption.
Conjugates bilirubin, a product of hemoglobin breakdown, for excretion.
Detoxifies drugs, hormones, and neurotransmitters.
Synthesizes plasma proteins, such as albumin and clotting factors.
Converts ammonia (NH₃) to urea for excretion.
Stores glycogen for energy.
Stores vitamins (A, D, E, K, and B12) and minerals.
Contains Kupffer cells, which are phagocytic cells that remove pathogens and debris from the blood.
How does blood flow through the liver?
Blood from the hepatic artery and hepatic portal vein flows into the liver sinusoids, then into central veins, then into the hepatic veins, and finally drains into the inferior vena cava (IVC).
Describe the pathway of bilirubin from its formation to excretion.
Unconjugated bilirubin → liver → conjugated bilirubin → bile → intestine → urobilinogen → feces / urine
What is bile, what are its components, and what stimulates its release?
Production and Storage:
Bile is produced by the liver and stored and concentrated in the gallbladder.
Components:
Water
Bilirubin
Bile salts
Pigments
Cholesterol
Stimuli for Release:
Parasympathetic nervous system activation
Cholecystokinin (CCK)
The presence of fats in the chyme, which increases CCK release and triggers gallbladder contraction.
What is the role of cytochrome P450 (CYP450) enzymes in the liver?
Cytochrome P450 (CYP450) enzymes in the liver metabolize and break down drugs, neurotransmitters, hormones, and other toxins, making them easier to eliminate from the body.
What happens to NH₃ (ammonia) in the body?
The liver converts toxic NH₃ into urea, which is then transported to the kidneys and excreted in urine.
Pancreatic enzymes, activation, and lipases
Pancreatic Enzymes (from acinar cells):
Pancreatic lipase – digests fats
Pancreatic amylase – digests starch
Carboxypeptidase – digests peptides
RNase & DNase – digest nucleic acids
Activation of Pancreatic Enzymes:
Most are released as inactive zymogens
Trypsinogen → trypsin (activated by enterokinase in the small intestine)
Trypsin then activates the other pancreatic enzymes
Major Lipases in Digestion:
Lingual lipase – mouth
Gastric lipase – stomach
Pancreatic lipase – small intestine (LIPASE): enzyme that breaks down fats (lipids) into smaller molecule.
What is pancreatic juice and what does it do?
Pancreatic juice contains digestive enzymes, water, and bicarbonate. Digestive enzymes chemically break down carbohydrates, proteins, and fats. Water provides a fluid medium for digestion. Bicarbonate neutralizes the acidic chyme from the stomach by buffering hydrochloric acid, raising the pH of the small intestine to a level optimal for pancreatic enzyme activity and protecting the intestinal mucosa from acid damage.
Control of Pancreatic Juice Secretion
Increases Pancreatic Secretion:
Parasympathetic stimulation → overall increase in pancreatic juice
Secretin → increases HCO₃⁻-rich pancreatic juice
CCK → increases enzyme-rich pancreatic juice
Decreases Pancreatic Secretion:
Somatostatin → inhibits release of pancreatic juice
Intestinal Secretions & Control
Intestinal Secretions:
Water (H₂O)
Bicarbonate (HCO₃⁻)
Digestive enzymes (brush-border enzymes):
Maltase
Lactase
Sucrase
Aminopeptidase
Peptidase
Lipase
Control of Intestinal Secretion:
↑ Parasympathetic stimulation → increases secretion
How are monosaccharides and amino acids absorbed and transported out of the small intestine?
Monosaccharide Absorption:
Co-transported with Na⁺ into intestinal epithelial cells
Exit basolateral membrane into blood vessels of the villi
Amino Acid Absorption:
Also Na⁺-dependent co-transport (same mechanism as monosaccharides)
Exit basolaterally into villus blood vessels
How are fats digested and absorbed in the small intestine?
Fat Digestion & Absorption Steps:
Pancreatic lipase breaks down emulsified fats into micelles.
Micelles enter the intestinal epithelial cells.
Inside the cells, fatty acids are re-formed into triglycerides.
Triglycerides bind to proteins to form chylomicrons.
Chylomicrons enter the lacteals (lymph vessels).
Lacteals → thoracic duct → bloodstream (left subclavian vein).
What controls motility in the small intestine, and what are the motility patterns?
Patterns:
Segmentation
Segmentation consists of rhythmic contractions of the circular smooth muscle in the walls of the small intestine. These contractions move chyme back and forth (“sloshing”) rather than pushing it forward. This action:
Mixes chyme thoroughly with digestive enzymes and intestinal secretions
Enhances mechanical digestion
Improves chemical digestion by evenly distributing enzymes
Increases contact between chyme and the intestinal mucosa
Therefore, it maximises nutrient absorption
Segmentation is strongest when nutrients are present in the lumen and slows down as nutrients are absorbed. The alternating contractions occur at different points along the intestine, squeezing the middle and ends of intestinal segments, producing efficient mixing rather than propulsion.
Peristalsis
Peristalsis is a series of coordinated, wave-like muscular contractions that propels contents forward through the gastrointestinal tract. It occurs in any hollow, muscular organ (esophagus, stomach, small intestine, large intestine).
In peristalsis:
The circular muscle contracts behind the bolus/chyme
The circular muscle relaxes in front of it
The longitudinal muscle shortens the segment
This coordinated pattern pushes material aborally (forward)
Peristalsis:
Begins in the esophagus
Occurs in the stomach to move chyme toward the pylorus
Continues through the small intestine and into the large intestine
Is responsible for movement, not mixing
Key Contrast (Exam Gold)
Segmentation = mixing for digestion & absorption
Peristalsis = propulsion for movement
Control of Motility:
↑ Parasympathetic stimulation → increases motility
Motilin → increases MMC activity (more motilin = ↑ motility)
Reflexes:
Gastroileal Reflex:
↑ Stretch in stomach → ↑ motility in small intestine
Intestino-intestinal Reflex:
↑ Stretch in intestine → ↓ motility
How are vitamins absorbed in the small intestine?
Lipid-Soluble Vitamins (A, D, E, K)
Absorbed with dietary fats in the small intestine
Require bile salts for emulsification (breaking large fat droplets into tiny fat droplets)
Enter intestinal cells via micelles
Packaged into chylomicrons → enter lymphatic system
Stored in liver & adipose tissue
Higher risk of toxicity if overdosed
Water-Soluble Vitamins (B, C)
Absorbed directly into intestinal cells by diffusion or active transport
Enter bloodstream immediately (portal circulation)
Not stored extensively (except B₁₂)
Excess is excreted in urine
Low risk of toxicity, higher risk of deficiency
Water Absorption
Water is reabsorbed by osmosis
Follows the movement of electrolytes (Na⁺, Cl⁻)
Majority absorbed in the small intestine
Remaining water absorbed in the large intestine
What are the functions, motility patterns, and controls of the large intestine?
Functions of the Large Intestine (Colon):
Absorbs large amounts of water
Produces vitamins (from gut bacteria)
Secretes HCO₃⁻
Houses millions of bacteria that:
Digest cellulose
Produce gases
Motility:
Segmentation / Haustral shuttling: mixing movements
Mass movements:
Occur 3–4 times per day
Powerful contractions that move contents to the rectum
Control of Motility:
↑ Parasympathetic stimulation → increases motility
Motilin → increases motility
Gastrocolic reflex:
↑ Stomach distention → ↑ colonic motility
What happens during the defecation reflex, and how can it be delayed
Defecation Reflex:
Mass movements push feces into the rectum
Rectal stretch → urge to defecate
↑ Parasympathetic stimulation → contracts colon & rectum
↓ Action potentials to rectal sphincters → internal sphincter relaxes
External sphincter relaxes → defecation occurs (to pass solid waste (feces) out of the body through the rectum and anus.)
Delaying Defecation:
↓ Parasympathetic activity
↑ Sympathetic activity
Reverse peristalsis (moves stool upward)
Keep sphincters contracted
When is pancreatic juice released, what stimulates it, what does it contain, where does it work, and what does “secreted as inactive zymogens” mean?
Pancreatic juice is released from the pancreas into the duodenum during the intestinal phase of digestion when chyme enters the small intestine. Cholecystokinin (CCK) stimulates the release of enzyme-rich pancreatic juice, while Secretin stimulates the release of bicarbonate to neutralize stomach acid. Pancreatic juice contains enzymes for carbohydrates, proteins (proteases), fats (lipase), and nucleic acids, plus bicarbonate and water. These enzymes perform digestion in the duodenum and jejunum after the pH is neutralized. Proteases are released as **inactive Zymogens (e.g., Trypsinogen → Trypsin) to prevent the pancreas from digesting itself.