Role of Health Psychology in COVID-19 Pandemic
Health Psychology
- Too simplistic to call Health Psychology the child of medicine and psychology
- Intersection of biological, psychological, and socio-cultural factors in health and illness
- Health behaviors (e.g. hygiene, blood sugar testing, blood pressure monitoring)
Role of Health Psychology
- (Arden & Chilcot, 2020) “understand how people will respond and cope to the threat of COVID-19…how they will adhere and adapt to transmission related behaviors including hand washing and self-isolation”
- (Bish & Mishie, 2010) “…promote preventive behaviors (that are) targeted to specific demographic groups as well as focus on raising PERCEIVED THREAT and effectiveness of BEHAVIORAL MEASURES to reduce risk”
Health Behaviors
- Personal hygiene behaviors
- Pro-social behaviors: e.g. maintaining social distance, let people check your temperature
- Panic buying
- Communication
- Risk perception
- Impacts of isolation
Mental impact of the COVID-19 pandemic (Usher, Bhullar, & Jackson, 2020)
- Modern quarantine strategies and restrictions
- Psychological effects of modern quarantine strategies and restrictions:
- Feelings of being unsafe
- Anxiety
- Threatened sense of connectedness (Hawryluck et al., 2004 as cited in Usher et al., 2020)
- Social isolation + quarantine = acute stress disorders, irritability, insomnia, emotional distress and mood disorders including depressive symptoms, fear and panic, anxiety and stress because of financial concerns, frustration and boredom, loneliness, lack of supplies and poor communication
- Disease-fear-contagion nexus
- Post-traumatic stress disorder
- Other stressors (Brooks et al., 2020): irregular or less supplies of usual goods (such as food items and medicine) restriction of routine daily activities
Effects of the COVID-19 Pandemic
- Increased incidence of intimate partner violence, family violence, COVID-19 induced panic disorder.
- Because of isolation
- Who are more vulnerable to psychological distress or exacerbations of existing illness?
- Children and adolescents
- Older adults
- Minority groups
- Lower socio-economic status groups
- Females
- Individuals with pre-existing mental conditions
- Students may experience “reduced motivation towards studies, increased pressures to learn independently, abandonment of daily routines, potentially higher rates of dropout” (Grubic, Badovinac, & Johri, 2020).
- Physicians, nurses, family caregivers: burnout, compassion fatigue as a result of increased workload pressures and increased total health expenditures (Moazzami et al., 2020). Healthcare workers may also experience anxiety during the COVID-19 pandemic (Shanafelt, Ripp, and Trockel, 2020). Healthcare workers are also susceptible to vicarious traumatization (Li et al., 2020).
- ^^Major causes of psychological distress among healthcare workers ^^include: long work hours, sleep disturbances, debilitating fatigue, risk of getting infected and putting their own families at risk of a life-threatening condition.
- Major causes of anxiety among healthcare professionals:
- access to appropriate PPE;
- exposure to COVID-19 at work and taking the infection home to their family;
- not having rapid access to testing if they develop symptoms and concomitant fear of propagating infection at work;
- uncertainty that their organization will support/take care of their personal and family needs if they develop infection;
- access to childcare during increased work hours and school closures;
- support for other personal and family needs as work hours and demands increase;
- being able to provide competent medical care if deployed to a new area;
- lack of access to up-to-date information and communication
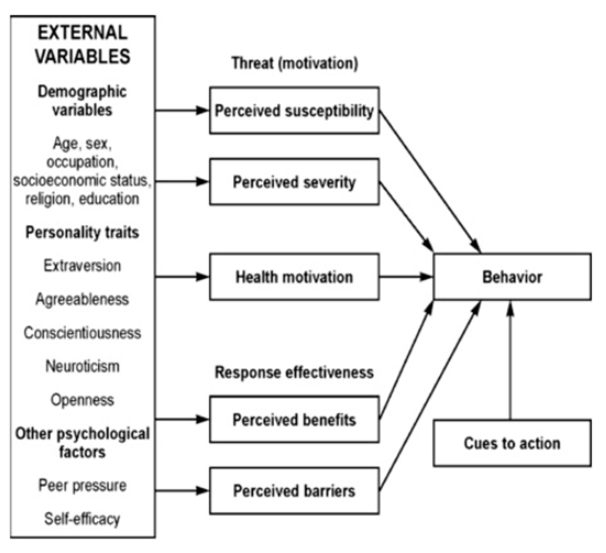
Health Belief Model
Increasing Resilience and Compliance to Public Health Measures
Resilience: “ability to maintain or quickly recover mental health during and after times of adversity” (Helmich & Bloem, 2020).
The COM-B Model: behaviors are influenced by how capable we are in doing the said behavior
- Why are you motivated to maintain said behavior?
- Do i have the opportunity to do said behavior?
Application of the COM-B Model to reduce SARS-CoV-2 transmission (West et al., 2020)
The Behavior Change Wheel
Using the APEASE criteria to evaluate intervention approaches or components (West et al., 2020)
What changes can we expect in mental health care delivery?
- As the number of cases increase, there is a very real possibility that there will be a decline in the workforce capacity of physicians, nurses, mental health practitioners/clinicians (Moazzami et al., 2020).
- It is recommended that pursuing developments and improvements in TELEMEDICINE and TELEPSYCHOLOGY delivery be seriously considered (Moazzami et al., 2020). \n