BSCI201: LEx2
1/109
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
110 Terms
The epidermis is composed of what?
keratinized stratified squamous epithelium
What are the five strata (deep to superficial) of the epidermis?
stratum basale, stratum spinosum, stratum granulosum, stratum lucidum (only in thick skin), and stratum corneum
What mnemonic is this? “Come Let’s Get Sun Burned”
Corneum, Lucidum, Granulosum, Spinosum, Basale
What is the prickly appearance of cells in the stratum spinosum is due to strong intercellular attachments provided by?
desmosomes
Keratinocytes
Produces keratin and is the precursor for vitamin D. Function is protection and waterproofing skin.
Melanocytes
Produces melanin. Found in the keratinocytes in the stratum spinosum to protect mitotic basal stem cells from UV rays
Dendritic cells (Langerhans cells)
provide immune surveillance in the epidermis through phagocytes
Merkel cells (Tactile cells)
sensory receptors located in the stratum basale and linked to sensory nerve fibers
What is the dermis composed of?
Fibrous CT
What layers are found in the Dermis?
Papillary layer and Reticular layer
Papillary layer
Composed of areolar CT, contains capillaries, sensory receptors like Tactile corpuscles and free nerve endings
Reticular layer
Composed of Dense Irregular CT, provides strength (collagen fibers) and stretch-recoil properties (elastic fibers). Contains pacinian (lamellar) corpuscles (vibration/pressure sensation)
Pacinian (lamellar) corpuscles
These sensory receptors for pressure and vibration are located in the reticular layer of the dermis, not the epidermis
What is the hypodermis composed of?
adipose tissue
Merocrine secretion
Products are secreted by exocytosis, substances released by cell
What are glands that are merocrine?
eccrine sweat glands and apocrine sweat glands
Holocrine secretion
Products secreted by rupture of the entire gland cell
What gland is of holocrine secretion?
Sebaceous glands
What are the sweat (sudoriferous) glands?
eccrine glands, apocrine glands, sebaceous (oil) glands
Eccrine glands
Uses merocrine secretion via duct to the skin surface. Used for thermoregulation
Apocrine glands
Uses merocrine secretion via duct to the hair follicle. Found in axilla and groin.
What are some modified apocrine glands?
ceruminous glands (ear wax) and mammary glands (milk)
Sebaceous glands
Uses holocrine secretion, producing an oily substance (sebum) that lubricates skin and hair - not associated with thermoregulation
Hair
The cells of the hair matrix, which undergo cell division, come from the epidermal stratum basale
Healing involves what?
regeneration and fibrosis
What is regeneration?
replacement of original tissue
What is fibrosis?
Formation of scar tissue, typical in the dermis
What is the first type of tissue to fill a large gap during healing?
granulation tissue (new CT and blood vessels)
Where does scar tissue result from?
Fibrosis, where fibroblasts proliferate and deposit collagen fibers. Scar tissue has decreased elasticity and fewer blood vessels.
First degree burn
Only epidermis is damaged, characterized by localized redness, edema, and pain
Superficial Second degree burn
Damage to the epidermis and superficial dermis. Characterized by blisters and extreme pain. Adnexa (Hair follicles and glands) remain and healing usually occurs by re-epithelialization with no scar.
Deep Second degree burn
Damage to deeper dermis. Less moist and pain. Heal by scar deposition, contraction, and limited re-epithelialization.
Third degree burn
Damage to the entire thickness of the skin. Permanent loss of adnexa. Often less painful because nerve endings are destroyed. Requires skin grafting.
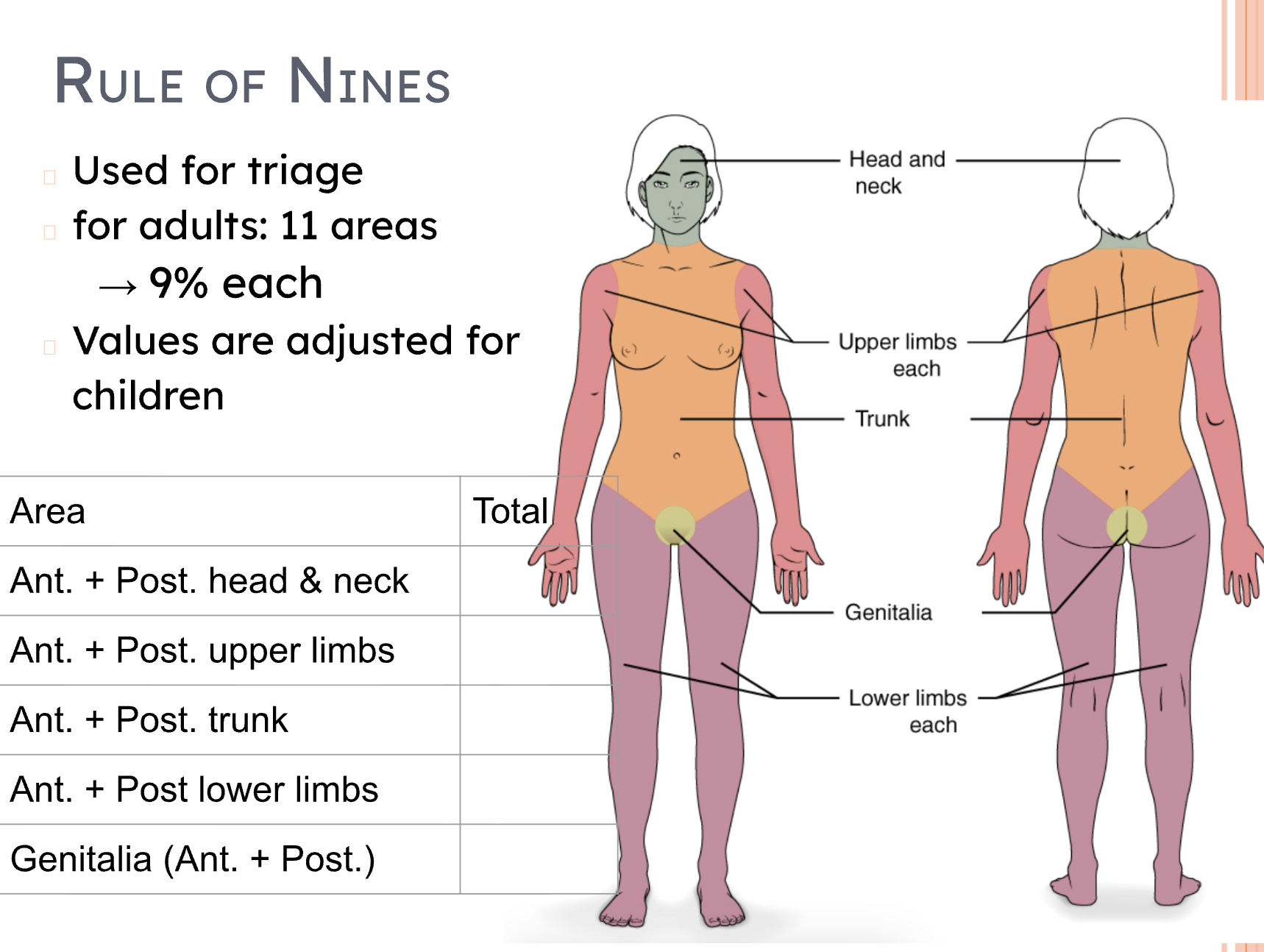
When are burns critical?
Over 25% of the body has second degree burns, over 10% of the body has third degree burns, or the third degree burns are on the face, genitalia, hands, or feet.
Fill in the blanks

Osteogenic cells (Mesenchymal Stem Cells)
differentiate into osteoblasts
Osteoblasts
deposits osteoid (organic matrix) and produce the hormone Osteocalcin
Osteocytes
Mature bone cells trapped in lacunae. Communicates with each other via gap junctions through extensions that travel in canaliculi
Osteoclasts
resorb (break down) bone matrix by secreting lysosomal enzymes and acid
Compact bone is organized into repeating structural units called what?
Osteons
Osteons consist of what?
Lamellae surrounding a central (haversian) canal containing blood vessels and nerves.
Adjacent osteons connect via what?
Perforating (volkmann’s) canals
Compact bones has high or low porosity?
low porosity
Spongy bone is composed of what?
taberculae
Spongy bone lacks what?
Osteons, central canals, and perforating canals
Spongy bones has high or low porosity?
high porosity
Hematopoiesis (blood cell formation)
occurs in the red bone marrow, which is found in the spongy bone throughout life
Intramembranous ossification
forms bone from fibrous membranes, forming flat bones
Endochondral ossification
forms bone by replacing a hyaline cartilage, forming all long bones, short bones, and irregular bones
Longitudinal Growth
Increases in length, occurs at the epiphyseal plate (metaphysis) throughout endochondral processes
What are the 4 zones of the epiphyseal plate?
Proliferation Zone, Hypertrophic Zone, Calcification Zone, and Ossification Zone
Proliferation Zone
Chondroblasts divide via mitosis (hyperplasia), pushing the epiphysis away from the diaphysis
Hypertrophic Zone
Older chondrocytes enlarge (hypertrophy)
Calcification Zone
Cartilage matrix calcifies, and chondrocytes die
Ossification Zone
Calcified cartilage is replaced by bone tissue, forming spongy bone
Appositional Growth
Increase in width/diameter, occurs in all bones. Involves addition of external bone layers by osteoblasts in the periosteum and the resorption of internal layers by osteoclasts in the endosteum
What are the hormones that help regulate bone growth?
Growth Hormone (GH), Thyroid hormone, Testosterone, and Estrogen
What does growth hormone and thyroid hormone do for bone growth?
stimulate epiphyseal plate activity
What does testosterone and estrogen do for bone growth?
promote osteoblast activity, inhibit osteoclast activity, promote calcification, and ultimately induce epiphyseal plate closure
What does menopause/estrogen cause for the bone?
Loss of estrogen in early menopause leads to the lifting of osteoclast inhibition, resulting in increased osteoclast activity and subsequent bone resorption, leading to bone mass reduction (osteoporosis). Woman likely to show hypocalcemia
Parathyroid hormone (PTH)
Released during hypocalcemia (low blood Ca2+). Promotes bone resorption (activates osteoclasts), increases Ca2+ reabsorption in the kidneys and stimulates calcitriol synthesis. Reduces calcium loss in urine
Calcitriol (active vitamin D3)
Expressed during hypocalcemia. Essential for Ca2+ homeostasis as it increases Ca2+ absorption in the gut (small intestine), increases Ca2+ reabsorption from kidneys and activates osteoclasts to resorb bone
Calcitonin
Expressed during hypercalcemia. Decreases osteoclast activity, promoting bone deposition
Osteomalacia
“bending” bones, softening of the bone is caused by decreased mineralization of the osteoid matrix
What is the purpose bone remodeling?
maintain Ca2+ homeostasis and adapt bone structure too mechanical stress
Wolff’s law
states that bone tissue adapts its structure and shape in response to the mechanical stresses placed upon it
Where do bones become thicker at?
attachment sites for active skeletal muscles
Lack of mechanical stress leads to what?
rapid loss of bone density (resorption exceeds deposition)
What are the stages of bone healing?
Hematoma forms, fibrocartilaginous callus forms, bony callus formation, bone remodeling
Hematoma forms
Torn vessels hemorrhages, and a clot forms
Fibrocartilaginous callus forms
fibroblasts secrete collagen and chondroblasts produce fibrocartilage to “glue” the sections (internal callus)
Boney callus formation
Osteoprogenitor cells differentiate into osteoblasts to produce new spongy bone (hard callus)
Bone remodeling
The bony callus is remodeled in response to mechanical stressors; compact bone replaces spongy bone, and the final structure resembles the original
What are the functional classifications for joints?
Synarthroses, Amphiarthroses, and Diarthroses
Synarthroses
Immovable joints, Synostoses (fused bone) are considered synarthrotic joints
Ampiarthroses
Slightly movable joints
Diarthroses
Freely movable joints
What are the structural classifications?
Fibrous joints, Cartilaginous joints, and Synovial joints
Fibrous joints
Bones united by fibrous CT
Cartilaginous joints
Bones united by cartilage, lacking a joint cavity
Synovial joints
Possess a joint cavity
Articular Cartilage
Hyaline cartilage covering the articulating surfaces of the bones.
Joint Cavity
Contains synovial fluid, which acts as a lubricant (reduces friction), provides nutrients to the cartilage, and absorbs shock (due to hyaluronic acid).
Articular Capsule
Double-layered structure forming the boundary of the synovial joint. It consists of an outer fibrous capsule and an inner synovial membrane which produces the synovial fluid
Ligament
A strong band of fibrous connective tissue (dense regular CT) that holds bones together
Tendon
Attaches muscle to bone; made of dense regular connective tissue
Bursa
A flattened, fibrous sac containing synovial fluid that prevents friction between skin/bone, or tendon/bone. Made of dense regular connective tissue
Sheath
An elongated bursa that wraps around a tendon
Plane Joint
Nonaxial, allows gliding, ie. intercarpals
Hinge Joint
Uniaxial, allows flexion/extension, ie. elbow, knee
Pivot Joint
Uniaxial, allows rotation, ie. Radioulnar joint, atlanto-axial joint (allows us to move head side to side, motion NO)
Condyloid Joint
Biaxial, allows flexion/extension, ab/adduction, circumduction, ie. knuckes
Saddle Joint
Biaxial, allows opposition, ie. thumb
Ball-and-socket Joint
multiaxial, allows flexion/extension, ab/adduction, rotation, circumduction, ie. shoulder, hip
Flexion
Decreases the angle of the joint
Extension
Increases the angle of the joint
Hyperextension
Excessive extension beyond the normal range of motion
ABduction
Movement away from the midline
ADduction
Movement toward the midline
Circumduction
Describes a cone in space (combination of F/E, Ab/Adduction)