Test 5 - Ischemic Heart Disease and Contrast
1/78
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
79 Terms
What is one of the most common indications for echocardiography?
Assessing left ventricular function in a patient with ischemic heart disease
What is ischemia?
Reduced blood flow, and thus oxygen, within an area
How is ischemic heart disease visually assessed?
From right and left ventricular wall thickening and wall motion by echo
Can you see the coronary arteries well by echo?
No
What is very important on patients in the ER with chest pain for diagnosis of coronary artery disease?
The presence or absence of wall motion abnormalities
Indications of ischemic heart disease are used….
to evaluate for other complications associated with CAD and with acute myocardial infarction
Diagnostic tests:
Electrocardiogram
Exercise stress test
Nuclear stress test
Cardiac MRI
Cardiac catheteriztion
Echocardiogram
Exercise stress echocardiogram
What is the gold standard out of the diagnostic tests?
Cardiac catheterization
Myocardial ischemia:
Lack of oxygen to the heart muscle caused by blockages in the coronary arteries
Greater than 70% narrowing
Increased demand for oxygen by exertion, emotional stress — the coronary arteries cannot supply enough blood to the muscle
Causes a change in wall motion in the affected area — hypokinesis
Does myocardial ischemia cause permanent damage?
No — wall motion will return to normal when demand for oxygen returns to normal
Angina:
Chest discomfort due to ischemia (lack of oxygen) to the heart muscle
Chest tightness or pressure, heaviness
Can radiate into the left arm, jaw, and back
Women and men’s symptoms can differ
What can women experience with angina? (4)
Nausea
Vomiting
Shortness of breath
General uneasiness
Sequence of events in myocardial ischemia: (4)
Describes what occurs within the heart when ischemia begins
Perfusion abnormalities are the first abnormalities that can be observed (observed by nuclear imaging)
Wall motion abnormalities are observed a little further into the cascade (observed by echocardiography)
ECG changes and finally angina occur later in the cascade
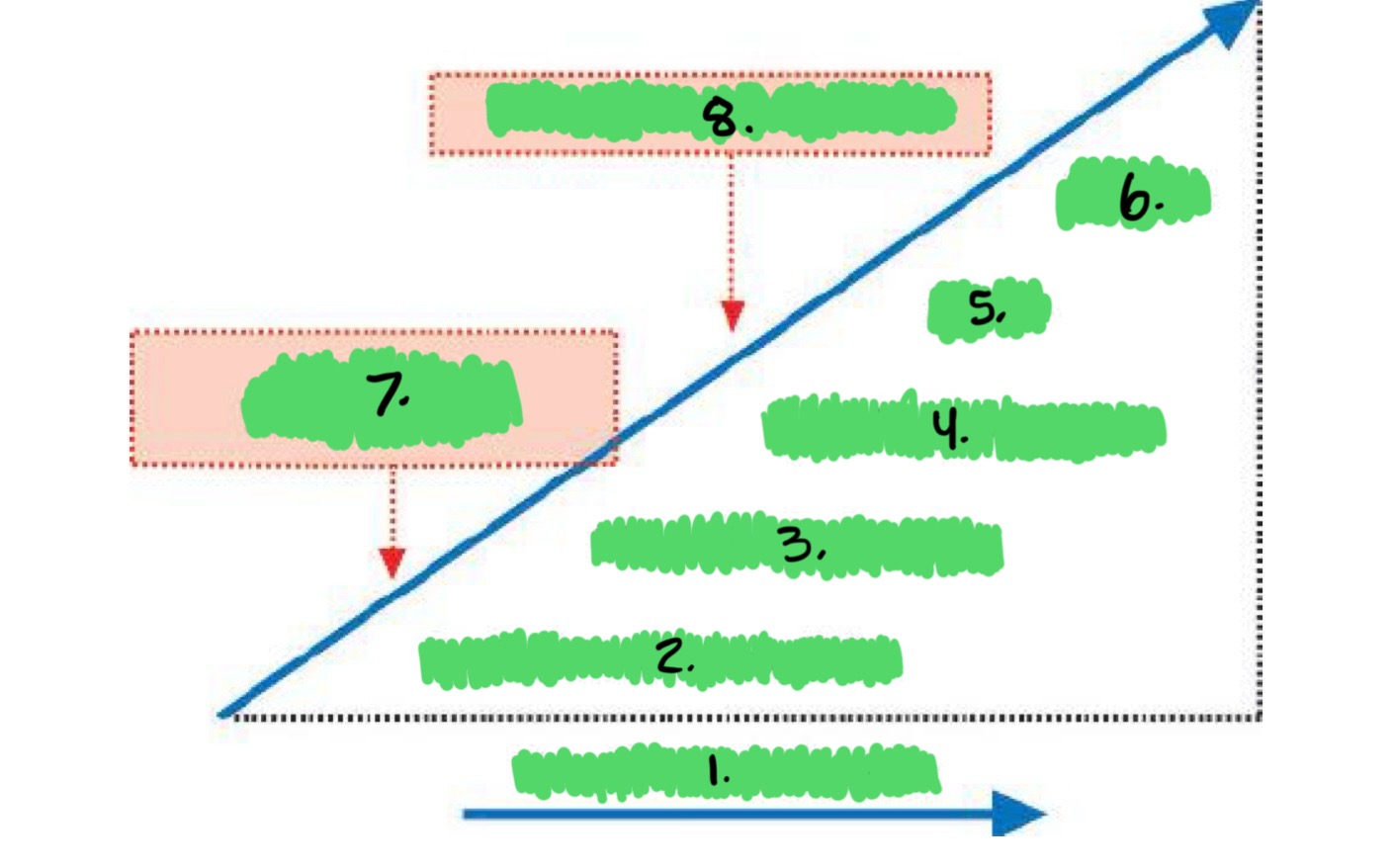
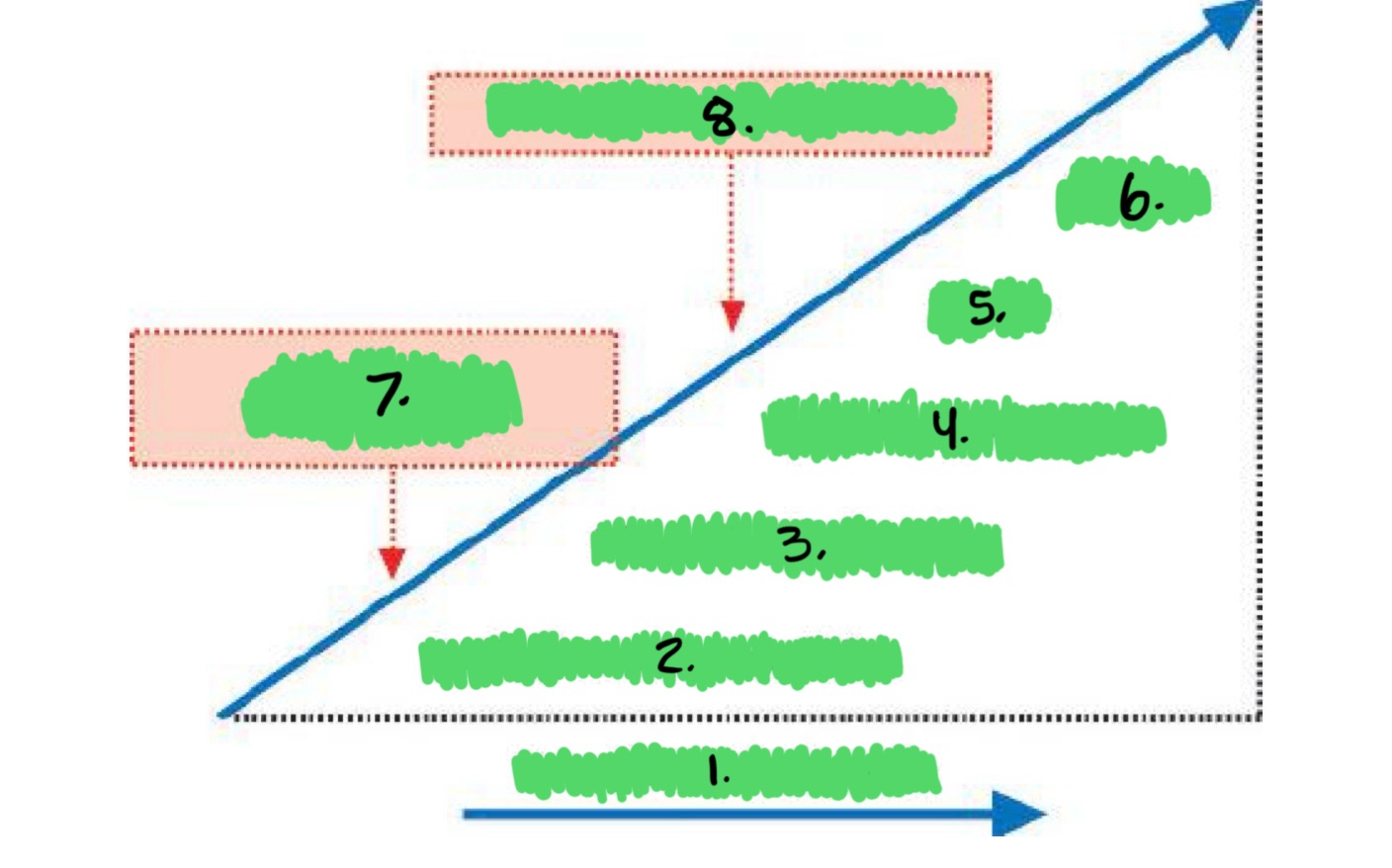
Label the sequence of events in myocardial ischemia: (8)
Duration of ischemia
Perfusion abnormalities
Diastolic dysfunction
Systolic dysfunction
∆ ECG
Angina
Nuclear imaging/MRI
Echocardiography/MRI
Myocardial infarction: (2)
When a blockage occurs in one the coronary arteries and the blood supply to heart muscle is completely occluded causing irreversible damage
Same as “heart attack”
Symptoms and signs of myocardial infarction:
Angina
Chest heaviness, aching, pinching, squeezing, tightness or pressure
Nausea, vomiting
Numbness
Dizziness/fainting
Diaphoresis
Palpitations
Radiating arm, back, shoulder, jaw pain
Dyspnea
Heart failure (SOB, edema, cough)
ECG changes
Causes of myocardial infarction: (3)
Rupture of atherosclerotic plaque
Spontaneous coronary artery dissection SCAD - more common in women
Coronary spasm
What is the leading cause of death in men and women?
Heart attack (myocardial infarction)
What do electrocardiograms show with MI? (2)
ST elevation with an acute MI
Q waves with an old MI
Acute infarction: (3)
Normal wall thickness
Reduced or absent endocardial motion and wall thickening
ST elevation on the electrocardiogram
Old myocardial infarction: (3)
Thinning and increased echogenicity due to scarring and fibrosis
Abnormal motion and absent wall thickening
Q waves on the electrocardiogram
Progression of MI: (2)
First, the heart muscle affected becomes hypokinetic or akinetic but the thickness remains normal
The heart muscle will become thin and scarred (fibrotic) over time and appear brighter on the echocardiogram
What does normal wall motion imply?
That there is no ischemia at the time images were acquired
Dressler’s syndrome: (3)
A form of pericarditis
A small pericardial effusion after a myocardial infarction
Usually 1 - 12 weeks post MI
What and why is the test of choice on a post MI patient with a murmur? (3)
Echo
Mitral regurgitation
Ventricular septal defect
Ventricular rupture with pseudoaneurysm
Ischemic mitral regurgitiation:
Functional mitral regurgitation — the leaflets are normal — includes mitral regurgitation caused by ischemia and dilated cardiomypathy
Caused by papillary muscle displacement and dilation of the annulus
Most common complication of a MI
Severe mitral regurgitation can occur with papillary muscle rupture
Tenting of the mitral valve leaflets (normal closure is at the annulus)
What is ischemic mitral regurgitation caused by?
Papillary muscle displacement and dilation of the annulus
What is the most common complication of a myocardial infarction?
Ischemic mitral regurgitation
What can occur with severe papillary muscle rupture?
Severe mitral regurgitation
Ventricular septal defect: (4)
Rupture of part of the IVS
Evaluate using color Doppler looking for high velocity flow on the right side
Left to right flow
Obtain peak velocity using continuous-wave Doppler in multiple windows
Pseudoaneurysm:
AKA contained rupture
An aneurysm caused by a rupture
Narrow neck (less than 0.5 cm) and lined with pericardium, not lined with myocardium
May have thrombus - perform off-axis, magnified imaging (improved near-field resolution)
Surgical repair recommended
What is a pseduoaneurysm lined with?
Pericardium
True aneurysm:
Diastolic contour abnormality - outward bulging of the wall in a severely infarcted area
Systolic dyskinesis - wall moves out while other walls contract in
Most common locations are apical or inferobasal
Lined by thin myocardium
Smooth transition from normal myocardium to thinned area
Wide neck (greater than 0.5 cm)
May have thrombus - perform off-axis, magnified imaging
What is a true aneurysm lined with?
Thin myocardium
Pericardial effusion:
Can occur after an MI - Dressler’s syndrome
Nonspecific response
Usually benign but could indicate pericarditis, possible dissection or LV rupture
Sometimes can develop tamponade physiology
Right ventricular infarcation:
Most often associated with an inferior MI
Right ventricular hypokinesis
Variable degrees of dilation
Left ventricular thrombi
Clotting information in areas of low flow
Low-flow examples that increase the likelihood of LV thrombi: (3)
Severely reduced akinetic area
An aneurysm
The appearance of spontaneous echo contrast (smoke)
LV thrombi; must perform careful imaging of the LV and apex…
Can be small or large
Can be confused with other structures - trabeculation, tendon, chord
Use high-resolution settings for better near-field resolution
Use off-axis imaging planes (short-axis apical views)
Use multiple imaging planes
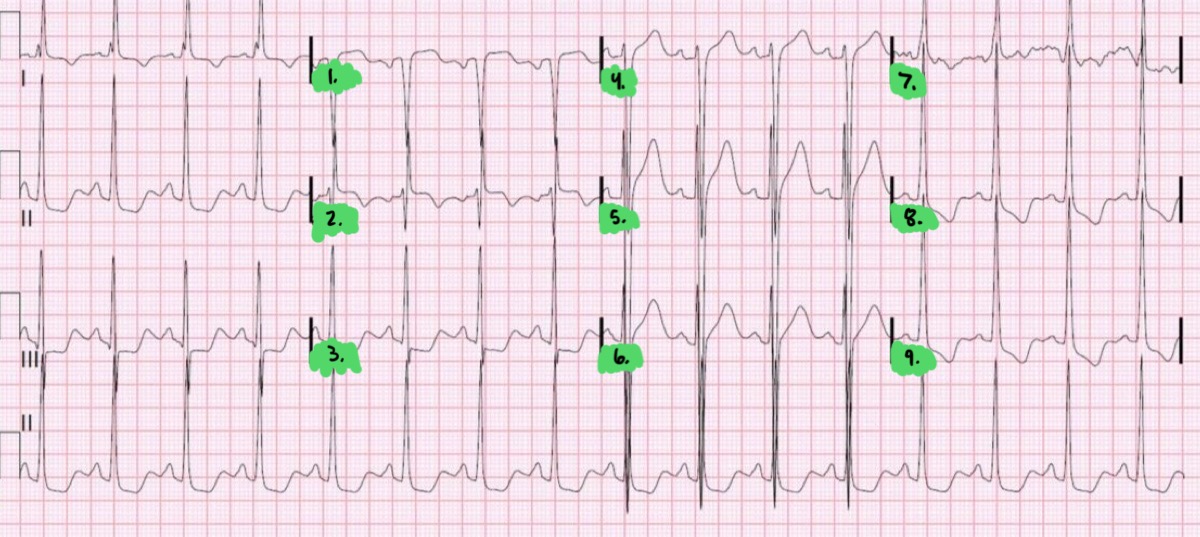
Electrocardiogram findings: (3)
ST depression - ischemia
ST elevation - acute MI
Q waves - old MI
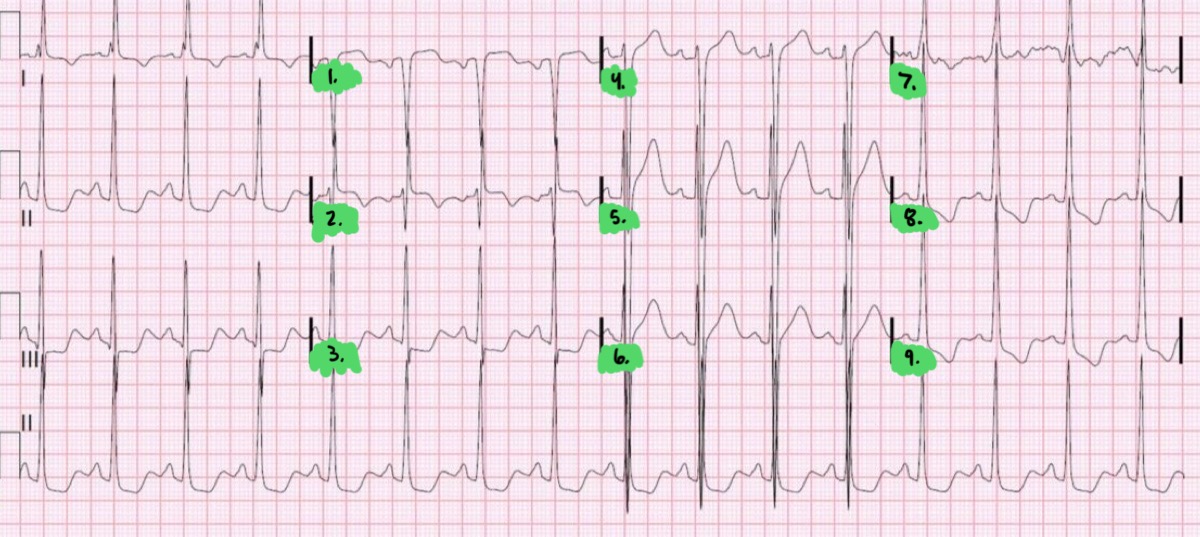
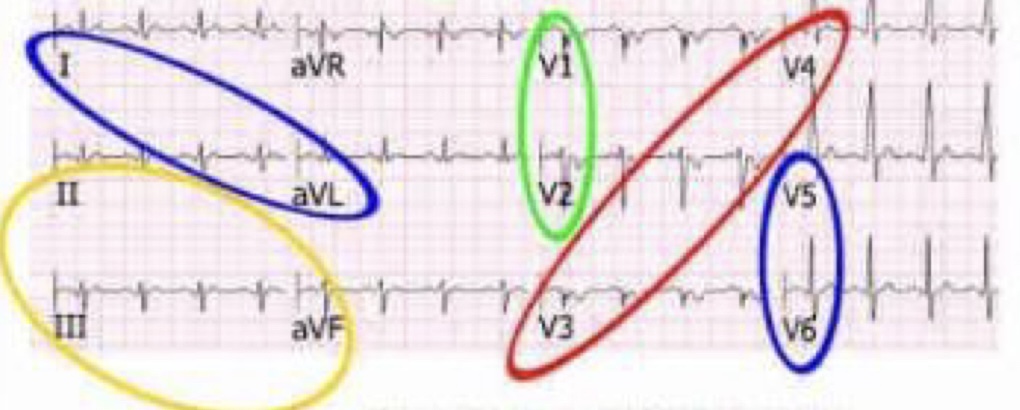
Label the EKG (Ischemia ST depression): (9)
aVR (augmented vector right)
aVL (augmented vector left)
aVF (augmented vector foot)
V1
V2
V3
V4
V5
V6
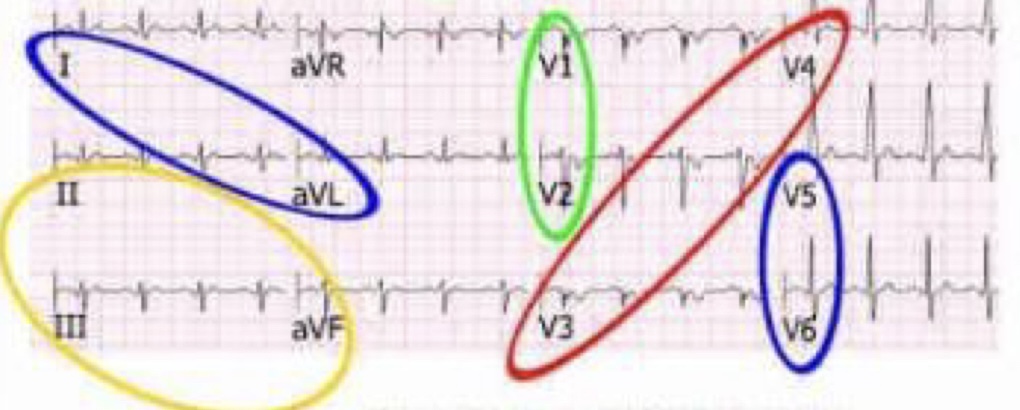
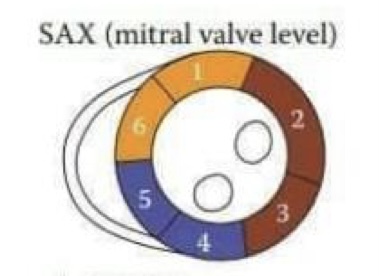
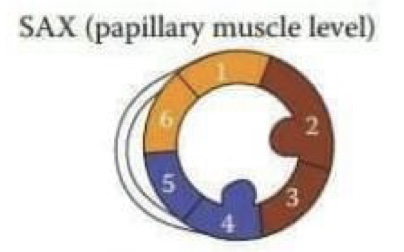
What do the colors mean within the diagram?
Blue- Lateral
Yellow- Inferior
Green- Septal
Red- Anterior
What do the wall segments on echocardiography correlate with?
They correlate closely with the coronary artery territories
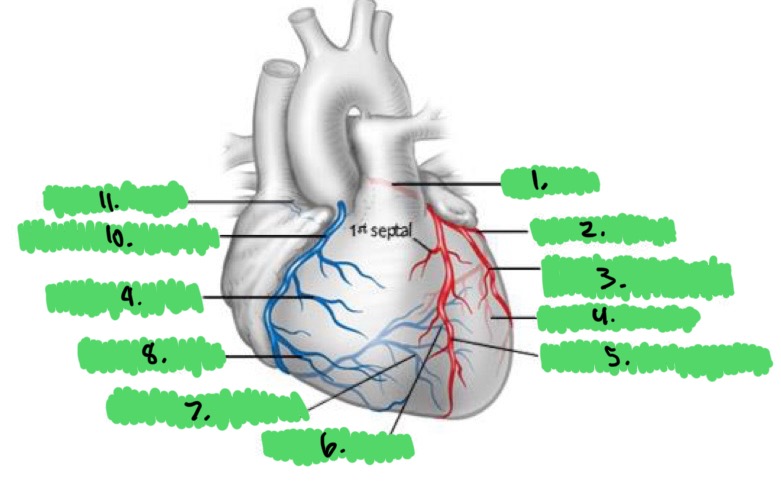
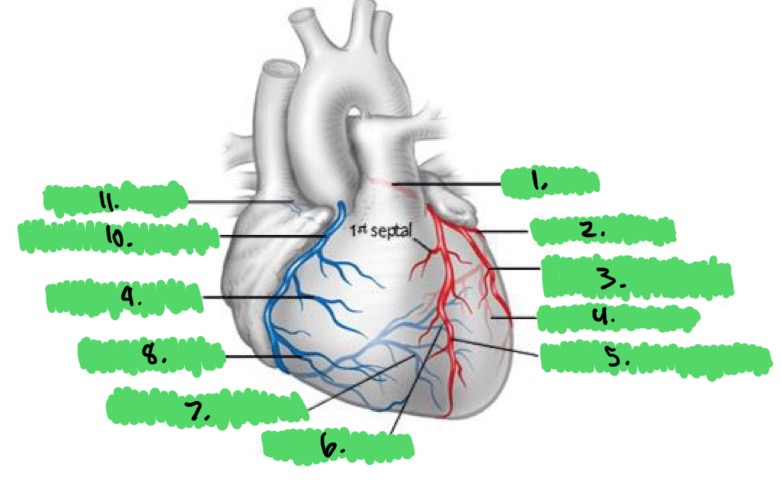
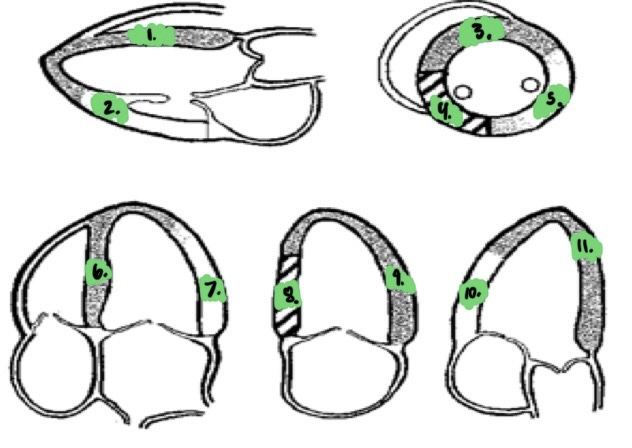
Label the coronary arteries: (11)
Left main
Left circumflex
Intermediate
Obtuse marginal
Left anterior descending
Posterior lateral
Posterior descending
Acute marginal
Right ventricular
Right coronary artery
Sinoatrial node
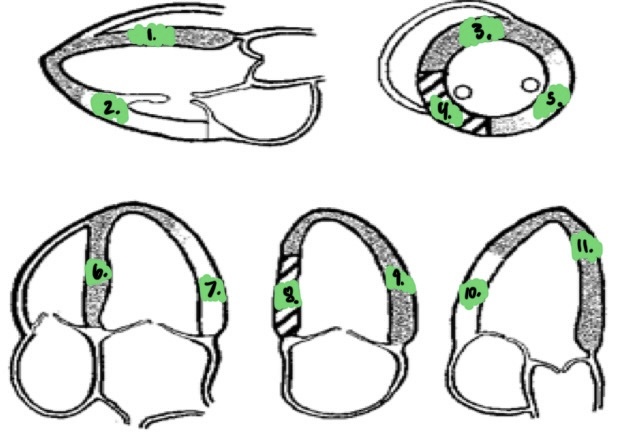
Label the coronary artery wall segments: (11)
LAD
LCx
LAD
RCA
LCx
LAD
LCx
RCA
LAD
LCx
LAD
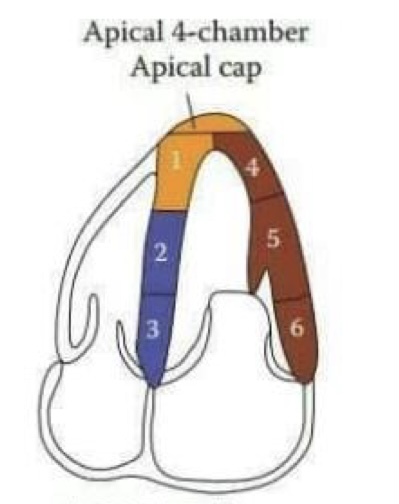
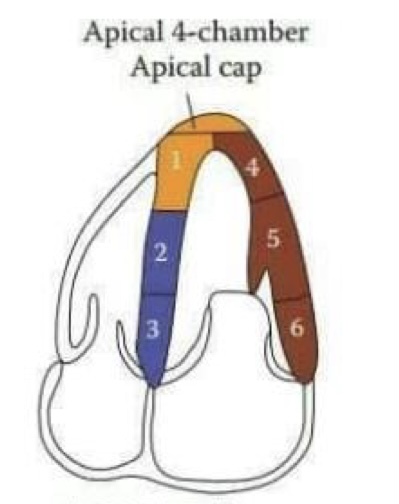
Label the Apical 4-Chamber diagram: (6)
Apical septal (LAD)
Mid inferoseptal (RCA)
Basal inferoseptal (RCA)
Apical lateral (LCx)
Mid anterolateral (LCx)
Basal anterolateral (LCx)
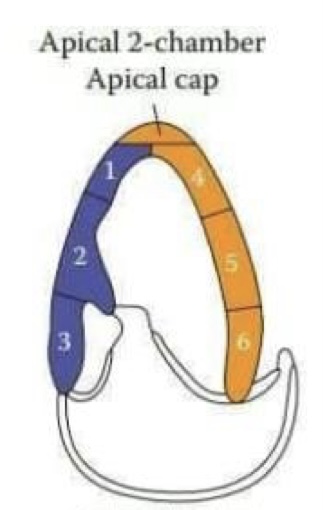
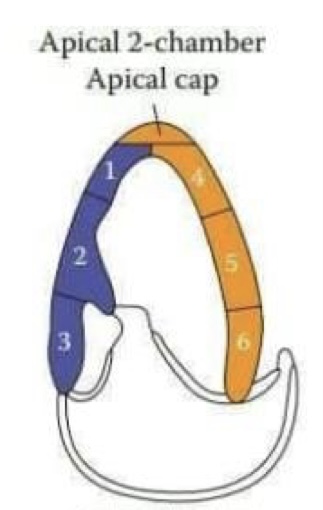
Label the Apical 2-Chamber diagram: (6)
Apical inferior (RCA)
Mid inferior (RCA)
Basal inferior (RCA)
Apical anterior (LAD)
Mid anterior (LAD)
Basal anterior (LAD)
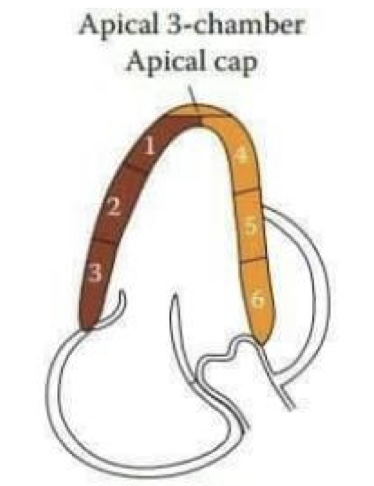
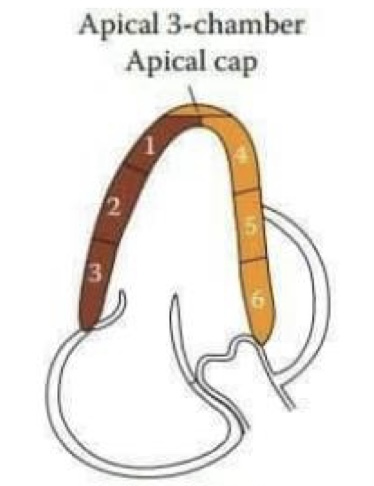
Label the Apical 3-Chamber diagram: (6)
Apical lateral (LCx)
Mid inferolateral (LCx)
Basal inferolateral (LCx)
Apical anterior (LAD)
Mid anteroseptal (LAD)
Basal anteroseptal (LAD)
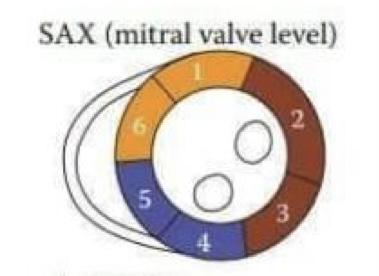
Label the SAX MV level diagram: (6)
Anterior (LAD)
Anterolateral (LCx)
Inferolateral (LCx)
Inferior (RCA)
Inferoseptal (RCA)
Anteroseptal (LAD)
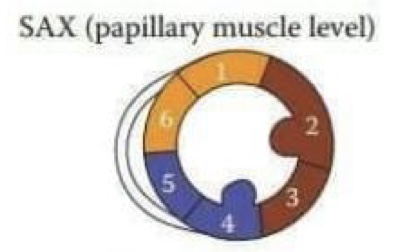
Label the SAX PAP level diagram: (6)
Anterior (LAD)
Anterolateral (LCx)
Inferolateral (LCx)
Inferior (RCA)
Inferoseptal (RCA)
Anteroseptal (LAD)
PAP
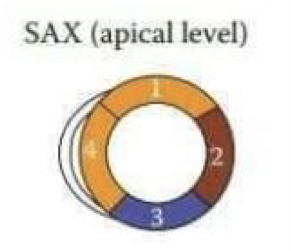
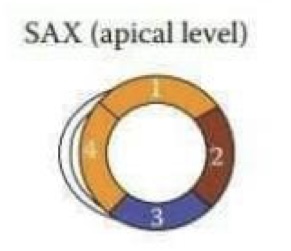
Label the SAX apical level diagram: (4)
Anterior (LAD)
Lateral (LCx)
Inferior (RCA)
Septal (LAD)
What will an occlusion of the left anterior descending artery result in?
A myocardial infarction and akinesis of the:
Anterior septum
Anterior wall
Apex
What will an occlusion of the right coronary artery result in?
A myocardial infarction and akinesis of:
Inferior septum - base and mid
Inferior wall
What will an occlusion of the circumflex artery result in?
A myocardial infarction and akinesis of:
Anterolateral wall
Inferolateral wall
Parasternal long-axis view evaluates wall motion of: (3)
Basal and mid segments of the anterior septum
Inferolateral wall (posterior wall)
Right ventricular free wall
Parasternal short-axis view evaluates wall motion of: (6)
Anterior septum
Anterior wall
Anterolateral wall
Inferolateral wall
Inferior wall
Inferoseptal wall
Apical four-chamber view evaluates wall motion of: (2)
Anterolateral wall
Inferior septum
Apical five-chamber view evaluates wall motion of: (2)
Anterolateral wall
Anterior septum
Apical two-chamber view evaluates wall motion of: (2)
Anterior wall
Inferior wall
Apical long-axis view evaluates wall motion of: (3)
Basal and mid segments of the anterior septum
Inferolateral wall (posterior wall)
Right ventricular free wall
Two-dimensional imaging tips: (5)
Avoid foreshortening in the apical views
Endocardial definition may be difficult due to attenuation from lung
Change patient position
Respiratory maneuvers
Obtain extra views and different depths
Perform off-axis views of the apex when wall motion abnormalities are present
Magnify on the apex using high resolution to evaluate for thrombus
Use contrast:
Aid in endocardial defitinion
Presence of a thrombus especially when wall motion abnormalities are present
Qualitative evaluation of global and regional function of CAD: (3)
Visually assess global and regional wall motion and systolic function
Estimate (eyeball) the ejection fraction
Use all windows and many tomographic views
Semi-quantitive evaluation - Wall Motion Score Index: (4; numbers correlate with scores)
Normal - endocardial inward motion and wall thickening in systole
Hypokinetic - reduced endocardial motion and wall thickening in systole
Akinetic - absence of inward endocardial motion or wall thickening in systole
Dyskinetic - outward motion or “bulging” of the segment in systole, usually associated with thin, scarred myocardium
Other information about Wall Motion Score Index:
Can be derived by dividing the sum of scores for each segment by the number of segments evaluated
Must be able to visualize the endocardium
Quantitative evaluation of global and regional function in CAD: (4)
Bi-plane tracing of the endocardium at end-systole and end-diastole in the apical views
Must have optimal endocardial definition
Method of Discs - Simpson’s
More accurate and preferred method as long as there is good imaging of the endocardium
Can echo alone assess for coronary artery disease?
No
Stress echocardiography:
Uses echocardiography (wall motion), rather than the electrocardiogram, to diagnose ischemia
Either exercise or dobutamine (pharmacologic) is used to attempt to raise the heart rate to produce ischemia
Observe LV wall motion before and after exercise or during pharmacologic exercise
Segmental wall motion abnormalities will develop with ischemia - reduced oxygen to the area
Need to evaluate wall motion during ischemia
Echocardiography in the Emergency Department:
Echocardiography is used very often to evaluate patients suspected of having an MI or patients with chest pain
Very easy to assess global and regional wall motion of the left and right ventricles
Echocardiography is useful in determining the location and severity of the wall motion abnormality
Echocardiography is also useful in re-evaluating global and regional function after a reperfusion procedure - CABG, Stent, balloon angioplasty
What do acute infarcts and ischemia usually have?
A wall motion abnormality with normal wall thickness
What do old infarcts have?
A wall motion abnormality with a thinning of the wall
End-stage ischemic cardiac disease:
Global left ventricular dysfunction develops due to multiple infarcts with some regional variation in wall motion
The presence of wall motion abnormalities will help distinguish CAD from a dilated cardiomyopathy
Once the end stage is reached, becomes difficult to differentiate from dilated cardiomyopathy
Dilated cardiomyopathy usually affects both ventricles
Usually preserved function at the base - basal inferolateral wall and lateral wall move best
What does dilated cardiomyopathy usually affect?
Both ventricles
Ischemic disease (end-stage): (2)
Definite areas of akinesis or wall thinning
Normal right ventricular size and function, unless there was an infarct
Purpose of contrast:
For use in patients with suboptimal echocardiograms
To opacify the LV to improve the delineation of the LV endocardium
To improve evaluation of LV systolic function
To enhance visualization or delineation of LV thrombus
To enhance tricuspid regurgitation Doppler jet for estimating PAP
Unlike agitated saline, the microspheres pass the capillary beds and opacify the LV
Helps answer questions; improves suboptimal images
Echo facts:
Inexpensive
Portable
Not selective
Ordered most often for LV function evaluation
25.7 million echocardiograms performed in 2006
Estimate that 20% of echocardiograms are non-diagnostic
Requires adequate delineation of endocardial borders
Regional wall motion abnormalities are associated with abnormalities of thickening and endocardial motion
Decreases the time needed to image technically difficult studies
Reproducible and accurate: Measurement of LV function provides prognostic and diagnostic information in patients with cardiovascular disease, which is why the ASE strongly supports the use of contrast
“See Better, Judge Better, Treat Better”
When to use contrast:
It is the responsibility of the sonographer to determine the need for contrast by determining the quality of the echocardiogram
Use contrast when unable to visualize two or more wall segments in the AP4C and AP2C views
Want to be able to see thickening of the myocardium, not movement
When less than 80% of endocardial border definition is visualized, contrast is strongly recommended
Use when wall motion abnormalities are present to rule out thrombus
Apical aneurysm, HCM
Possible complications after a myocardial infarction: (5)
Pericarditis
Dressler’s Syndrome
Pericardial effusion
Thinning and scarring of myocardium
VSD
Basic reasons to use contrast: (3)
To enhance suboptimal images
To enhance tricuspid valve regurgitation
To delineate a mass or thrombus
An ejection fraction over 75% is called?
Hyperkinesis