MD5 - Anti-androgens
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
26 Terms
Risk of prostate cancer
1 in 8 men will get prostate cancer
Risk increases with age
Typically > 50 and most common age is 65-69
Risk factors of prostate cancer
Family history
Father/ brother who has been diagnosed with prostate cancer previously means you’re 2.5x more likely to develop it
If mother/sister has had breast cancer
Ethnicity
black men risk is 1 in 4
Age
over 50
PSA
Prostate Specific Antigen
a specific protein made by the prostate, some of which enters the bloodstream and can be measured via a blood test.
An enlarged, inflamed or infected prostate can cause elevated PSA
Elevated PSA may also indicate cancer in the prostate (but may be other things)
Stages of Prostate Cancer: (T)NM
T1 – tumour is contained in the prostate, too small to be felt by digital rectal examination (DRE) or seen on a scan (may be diagnosed after elevated PSA then biopsy)
T2 – tumour still contained in the prostate but can be felt by DRE or seen on a scan
Divided in to:
T2a –tumour is only in half of 1 of the 2 lobes of the prostate
T2b – it is in more than half of 1 lobe
T2c – it is in both lobes
T3 – tumour has spread through the capsule surrounding the prostate and may be in nearby tissues
T3a – spread through the capsule
T3b – spread to the seminal vesicles that produce fluid for semen
T4 – spread into areas close by such as the bladder, rectum or the muscle that controls urination
Stages of Prostate Cancer: T(N)M
N0 – means there is no cancer in the lymph nodes near the prostate
N1 - means there is cancer in 1 or more lymph nodes close by
Stages of Prostate Cancer: TN(M)
M0 – means the cancer has not spread to another part of the body (hence locally advanced prostate cancer is ALWAYS M0)
M1 – means the cancer has spread to another part of the body
So advanced prostate cancer is ALWAYS M1
Numbered staging of Prostate Cancer
Stage 1 – Tumour contained in the prostate
Stage 2 – Tumour is bigger but still contained in the prostate
Stage 3 – Tumour has started to break out of the outer capsule and may be in the seminal vesicles
Stage 4 – Tumour has spread outside the prostate – maybe local, such as the bladder, but may be further, e.g. to bones
Gleason Scale
based on taking a biopsy of the prostate and looking at the morphology of the cells
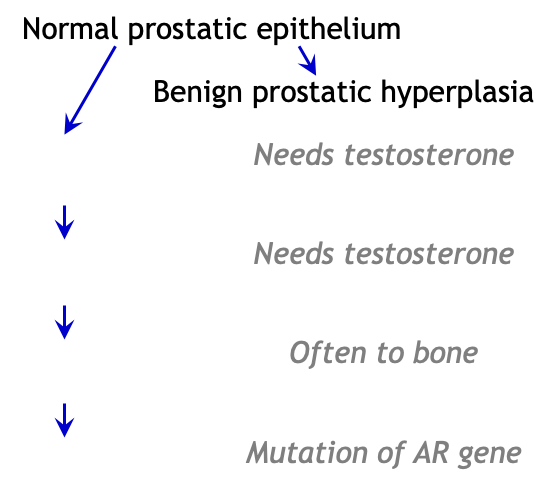
Androgen Independence
prostate cancer always starts out needing the testosterone when it no longer needs the testosterone signal it is androgen independent (very bad)
How does Prostate cancer develop from prostatic epithelium?
Options for treatment of prostate cancer
watchful waiting - mainly for frail older men with slow-growing tumours
active surveillance - small tumours confined to prostate
surgery - frequently used but major side effets
hormone therapy - ONLY for hormone dependent tumours
chemotherapy - for hormone independent/relapsed cancer
high-intensity focused ultrasound - energy into prostate cancer to “de-bulk” aka break it up
External beam radiotherapy - for small tumours confined to the prostate
Permanent seed brachytherapy - permanent source of radiation which is implanted into the tumour itself and will damage it because it’s sat inside the tumour
How does testosterone promote proliferation?
binds to androgen receptor (with hydrophobic interactions) outside cell
causes a conformation change
AR+T complez translocates to the cell’s nucleus where it signals for proliferation
First gen AR inhibitors
flutamide - originally antibacterial and then used for anti-androgen activity - - hepatotoxic so little use in prostate cancer atm
Possible due to mitochondrial toxicity
nilutamide - made from flutamide and a little less hepatotoxic
selective antagonist
bicalutamide - binding mode is known and this drug is widely used
Often used with gonadotropin releasing hormone (GnRH) or castration
Common structural components of 1st generation anti-androgens
CF3
aromatic ring
amide bond
2nd generation anti-androgens
Enzalutamide
good in vivo efficacy
good PK
high steady state brain tissue level - rare cns toxicity
Apalutamide
good in vivo efficacy
good PK
low steady state brain tissue level (good)
Darolutamide
short t1/2
When is Apalutamide used?
non metastatic castrate resistant prostate cancer
Bicalutamide MOA
binds to AR (via H-bonds) but doesn’t cause conformational change
acts as competititve inhibitor
bicalutamide complex is internalised but cannot be translocated to the nucleus
some agonist activity especially at mutant AR
How does bicalutamide bind to AR?
binds using nitrile of the bicalutamide and forms a H-bond with the amine of the Arg 752
No Thr877 binding
on the other end of it’s molecule it has another with Asn705 and forms a hydrogen bond at the hydroxyl group of the bicaludamine with the carboxyl of the Asn705
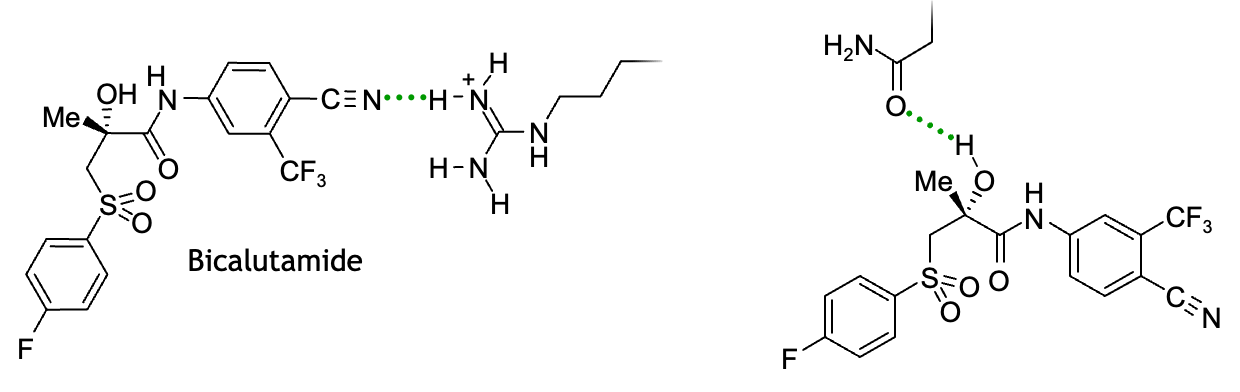
How does Testosterone bind to AR?
it forms a H-bond with the receptor at the carboxyl group and binds with the amine of the Arg 752 (part of the binding site)
On the other end it also picks up a Thr877 at the hydroxyl group
Mechanism of resistance to enzulatamide
primary/acquired resistance is usually developed from cancer reccurance and progression
but the other methods of resistance are:
AR signalling pathways are altered - typically AR gene amplification which increases the no. of AR so not all blocked by drug
AR mutation - converts drug from antagonist to agonist
AR (splice) variant - typically after castration but role in resistance is not very clear
Metabolic changes - increased androgen synthesis to overwhelm the inhibition as it is only competitive
lineage plasticity - cell line becomes AR independent via epigenetic changes so testosterone is no longer needed
How much does enzalutamide extend life by?
4-5 months for castrate resistant metastatic prostate cancer
Biosynthesis of testosterone
Cholesterol
Pregnenolone → progesterone
either make Androtenediol (pregnenolone) or Androstenedione (progesterone) which can both be converted into testosterone
CYP17A1
exists as tetramer therefore 4 binding sites
it is an oxidising enzyme (has an iron in the centre of it)
converts progesterone to 17a hydroxyprogesterone (intermediate before androtenedione)
Drugs that inhibit CYP17A1
Need something that is a ligand for metals - has a lp and will bind to the iron e.g.
Ketoconazole (non-specific inhibitor of CYPs)
Abiraterone - selective inhibitor of CYP17A1
Abiraterone acetate - prodrug of abiraterone
How does progesterone bind to CYP17A1?
C=O forms a h-bond to the Asn202 of CYP17A1
hydrocarbon part sticks to the hydrophobic side-chain
How does abiraterone bind to CYP17A1?
OH forms a h-bond to the Asn 202