Muscle Physiology
5.0(1)
Card Sorting
1/110
Earn XP
Description and Tags
Last updated 6:26 AM on 2/24/23
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
111 Terms
1
New cards
What are the three types of muscle tissue is the muscular system?
Skeletal, Cardiac, and Smooth
2
New cards
What is skeletal muscle?
* Attached to bones of skeleton
* Voluntary (consciously controlled)
* Voluntary (consciously controlled)
3
New cards
What is cardiac muscle?
* Makes up most of the wall of the heart
* Involuntary (non-consciously controlled)
* Responsible for pumping action of the heart
* Involuntary (non-consciously controlled)
* Responsible for pumping action of the heart
4
New cards
What is smooth muscle?
* Found in walls of internal organs, such as those of digestive tract.
* Involuntary (non-consciously controlled)
* Involuntary (non-consciously controlled)
5
New cards
Skeletal muscles
* Over 600 skeletal muscles in the body
* Attached to bones, and skin of face
* Under conscious control (voluntary)
* Are organs of the muscular system
* Attached to bones, and skin of face
* Under conscious control (voluntary)
* Are organs of the muscular system
6
New cards
What is skeletal muscle composed of?
* Skeletal muscle tissue
* Nervous tissue
* Blood
* Connective tissue
* Nervous tissue
* Blood
* Connective tissue
7
New cards
What is Fascia?
Thin covering of connective tissue around a muscle.
8
New cards
What are tendons?
Cord-like mass of connective tissues that connect muscles to a bone.
9
New cards
What is Aponeurosis?
Sheet-like mass of connective tissue that connects a muscle to bone, skin, or another muscle.
10
New cards
What does the Epimysium surround?
Surrounds whole muscles; lies beneath fascia.
11
New cards
What does the Perimysium surround?
Surrounds fascicles within a muscle.
12
New cards
What does the Endomysium surround?
Surrounds muscle fibers (cells) within a fascicle.
13
New cards
What is a compartment?
Space containing groups of muscles, blood vessels, and nerves enclosed by fascia.
14
New cards
What is Compartment Syndrome?
* It’s fluid accumulation with a compartment which results in the increase of pressure in the compartments.
* It leads to deficiency of oxygen and nurtients.
* Also causes severe pain.
* It leads to deficiency of oxygen and nurtients.
* Also causes severe pain.
15
New cards
Fascia
* Fascia of each muscle is part of network of fasciae
* Portion surrounding muscles is deep fascia, which connects to subcutaneous fascia under skin
* Network also connects to subserous fascia of serous membranes
* Portion surrounding muscles is deep fascia, which connects to subcutaneous fascia under skin
* Network also connects to subserous fascia of serous membranes
16
New cards
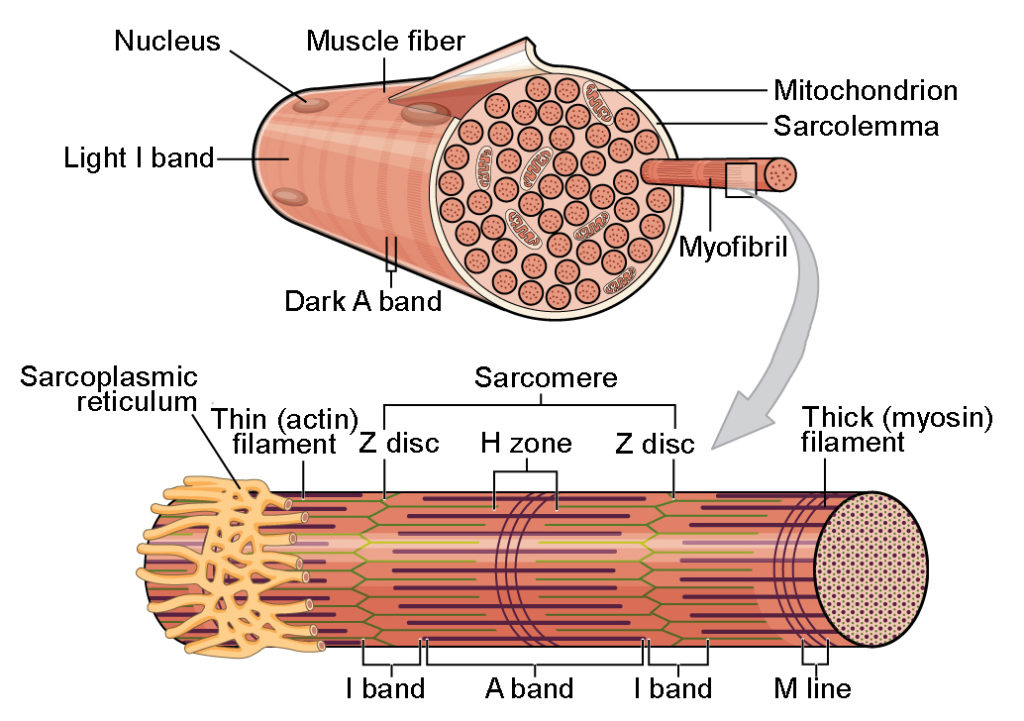
Skeletal muscle fiber (cell) are…
Multinucleated
17
New cards
What is sarcolemma?
Cell membrane of muscle fiber
18
New cards
What is the sarcoplasm?
Cytoplasm of muscle fiber
19
New cards
Myofribils consist what?
Thin actin filaments and thick myosin filaments.
20
New cards
What is sarcomeres?
Units that connect end-to-end, to make up myofibrils. (Functional unit of the muscular system)
21
New cards
What is the Sarcoplasmic reticulum (SR) and what does it store?
It is the endoplasmic reticulum of muscles and it stores calcium.
22
New cards
What is the transverse (“T”) tubule responsible for?
It relays electrical impulses to the SR.
23
New cards
What does the Triad consist of?
1 T tubule and 2 SR cisternae
24
New cards
What does myofibrils consist of that connect from end-to-end?
Sarcomeres
25
New cards
How are Striation patterns made?
They’re made by the arrangement of myofilaments in the myofibrils.
26
New cards
The A sarcomere consists of what structures?
I band- Light band; composed of thin actin filaments
A band- Dark band; composed of thick myosin filaments with portions overlapped with thin actin filaments.
H zone- Center of A band; composed of thick myosin filaments.
Z line (Z disc)- Sarcomere boundary; in center of I band which anchors filaments in place.
M line- Center of sarcomere and A band; anchors thick filaments
A band- Dark band; composed of thick myosin filaments with portions overlapped with thin actin filaments.
H zone- Center of A band; composed of thick myosin filaments.
Z line (Z disc)- Sarcomere boundary; in center of I band which anchors filaments in place.
M line- Center of sarcomere and A band; anchors thick filaments
27
New cards
Thick filaments
* Composed of myosin proteins
* Heads form cross-bridges with thin filaments
* Heads form cross-bridges with thin filaments
28
New cards
Thin filaments
* Composed of actin protein
* Associated with troponin and tropomyosin, which prevent cross-bridge formation when muscle is not contracting.
* Associated with troponin and tropomyosin, which prevent cross-bridge formation when muscle is not contracting.
29
New cards
Heavy chains and light chains form what?
Heavy chains intertwine to form myosin tail
Light chains form myosin globurlar head
Light chains form myosin globurlar head
30
New cards
Actin filaments made up of what?
G actin (globular) subunits
* G actin subunits bears active sites for myosin head attachment during contraction.
* G actin subunits bears active sites for myosin head attachment during contraction.
31
New cards
G actin subunits link together to form what?
Long fibrous F actin (filamentous)
32
New cards
____ F actin strands twist together to form a thin filament.
Two
33
New cards
What does tropomyosin and troponin do?
They regulate proteins bound to actin.
34
New cards
Contraction of a skeletal muscle fiber
* Requires interaction from several chemical and cellular components.
* Results from a movement within the myofibrils, in which the actin and myosin filaments slide past each other, shortening the sarcomeres
* Muscle fiber shortens and pulls on attachment points.
* Results from a movement within the myofibrils, in which the actin and myosin filaments slide past each other, shortening the sarcomeres
* Muscle fiber shortens and pulls on attachment points.
35
New cards
Neuronmuscular Junction (NMJ)
* A type of Synapse
* Also called a myoneural junction
* Site where an axon of motor neuron and skeletal muscle fiber interact
* Skeletal muscle fibers contract only when stimulated by a motor neuron
* Also called a myoneural junction
* Site where an axon of motor neuron and skeletal muscle fiber interact
* Skeletal muscle fibers contract only when stimulated by a motor neuron
36
New cards
Parts of a Neuromuscular Junction consist of..
* Motor neurons
* Motor end plates
* Synaptic Cleft
* Synaptic vesicles
* Neurotransmitters
* Motor end plates
* Synaptic Cleft
* Synaptic vesicles
* Neurotransmitters
37
New cards
Motor neuron
Neuron that controls skeletal muscle fibers
38
New cards
Motor end plate
Specialized folded portion of skeletal muscle fiber, where fiber binds to neurotransmitter.
39
New cards
Synaptic Cleft
Space between neuron and muscle fiber, across which neurotransmitter travels.
40
New cards
Synaptic vesicles
Membrane-bound sacs containing neurotransmitters
41
New cards
Neurotransmitters
Chemical released by motor neuron to deliver message to muscle fiber
42
New cards
Steps for contraction at neuromuscular junction
* Action potential arrives at the end of a motor neuron
* Action potential sends an electrical signal which opens a voltage channel
* Calcium rushes into end of motor neuron and stimulates release of ACh from synaptic vesicles
* ACh diffuses arcross synaptic cleft and bind to receptors
* AcH receptors open a channel where Na ions enter and K ion exits.
* A change occurs in the membrane potential called the end plate potential
* Action potential sends an electrical signal which opens a voltage channel
* Calcium rushes into end of motor neuron and stimulates release of ACh from synaptic vesicles
* ACh diffuses arcross synaptic cleft and bind to receptors
* AcH receptors open a channel where Na ions enter and K ion exits.
* A change occurs in the membrane potential called the end plate potential
43
New cards
Generations of an Action Potential Across the Sarcolemma
* Resting sarcolemma is polarized, meaning a voltage exists across membrane
* Action potential is caused by changes in electrical charges
* Action potential is caused by changes in electrical charges
44
New cards
Three steps of action potential across the sarcolemma.
* End plate potential- generated at the neuromuscular junction
* Depolarization- generating and propagating an action potential
* Repolarization- restoring the sarcolemma to its initial polarized state (negative inside, positive outside)
* Depolarization- generating and propagating an action potential
* Repolarization- restoring the sarcolemma to its initial polarized state (negative inside, positive outside)
45
New cards
Refractory period
Muscle fiber cannot be stimulated for a specific amount of time, until repolarization is complete.
46
New cards
What is excitation-contractions coupling?
Connnection between muscle fiber stimulation and muscle contraction.
47
New cards
During muscle relaxation:
* Calcium ions are stored in sarcoplasmic reticulum
* Troponin-tropomyosin complexes cover binding sites on actin filaments
* Troponin-tropomyosin complexes cover binding sites on actin filaments
48
New cards
Upon muscle stimulation:
* Muscle impulses travel down the T-tubules causes SR to release
* Calcium ions binds to troponin to change its shape
* Each tropomyosin is held in place by a troponin molecule; change in shape of troponin alters the position of tropomyosin
* Binding sites on actin are now exposed
* Myosin heads bind to actin, forming cross-bridges
* Calcium ions binds to troponin to change its shape
* Each tropomyosin is held in place by a troponin molecule; change in shape of troponin alters the position of tropomyosin
* Binding sites on actin are now exposed
* Myosin heads bind to actin, forming cross-bridges
49
New cards
Cross-Bridge Cycling in order
1. Myosin head attaches to actin binding site, forming cross-bridge
2. Myosin cross-bridge pulls thin filaments towards center of sarcomere
3. ADP and Phosphate are released from myosin
4. New ATP binds to myosin
5. Linkage between actin and myosin cross-bridge break
6. ATP splits
7. Myosin cross-bridge goes back to original position, ready to bind to another binding site on actin.
50
New cards
Relaxation
* Acetylcholinesterase rapidly decomposes ACh remaining the synapse
* Muscle impulse stops when ACh is decomposed
* Stimules to sarcolemma and muscle fiber membrane ceases.
* Calcium pumps calcium ions back into sarcoplasmic reticulum
* Troponin-tropomyosin complex again covers binding sites on actin.
* Myosin and actin binding are now prevented.
* Muscle fiber relaxes.
* Muscle impulse stops when ACh is decomposed
* Stimules to sarcolemma and muscle fiber membrane ceases.
* Calcium pumps calcium ions back into sarcoplasmic reticulum
* Troponin-tropomyosin complex again covers binding sites on actin.
* Myosin and actin binding are now prevented.
* Muscle fiber relaxes.
51
New cards
Sliding Filament Model of Muscle Contraction:
* When sarcomeres shorten, thick and thin filaments slide past each other
* H zones and I bands narrow (some texts state the H zones will disappear and I bands shorten)
* Z lines move closer together (pulled toward M line)
* A bands move closer to each other
* Thin and thick filaments do not change length
* Overlap between filaments increases
* H zones and I bands narrow (some texts state the H zones will disappear and I bands shorten)
* Z lines move closer together (pulled toward M line)
* A bands move closer to each other
* Thin and thick filaments do not change length
* Overlap between filaments increases
52
New cards
Myasthenia Gravis (MG)
* An autoimmune disorder, which antibodies attack acetylcholine receptors on skeletal muscle fibers (motor end plates) in neuromuscular junctions.
* Person may have only one-third normal number of ACh receptors
* May lead to widespread muscle weakness and muscle fatigue
* Treatments for it include drugs that inhibit acetylcholinesterase and immunosuppressant drugs
* Person may have only one-third normal number of ACh receptors
* May lead to widespread muscle weakness and muscle fatigue
* Treatments for it include drugs that inhibit acetylcholinesterase and immunosuppressant drugs
53
New cards
Muscular Dystrophy
* Deficiency or abnormality/mutation in scarce muscle protein called dystrophin.
* Dystrophin binds to internal side of muscle cell membrane, and holds them together during contraction.
* In absence of normal dystrophin, cells lose normal structure and die.
* Dystrophin binds to internal side of muscle cell membrane, and holds them together during contraction.
* In absence of normal dystrophin, cells lose normal structure and die.
54
New cards
Clostridium Botulinum
* Anaerobic bacteria that produces a toxin that caused food poisoning.
* Grows in food that is not properly preserved
* Causes digestive, muscular, and respiratory symptoms.
* Treated with an antitoxin
* Used in small doses as Botox to smooth wrinkles, treat mirgraines. Blocks the release of Ach causing paralysis.
* Grows in food that is not properly preserved
* Causes digestive, muscular, and respiratory symptoms.
* Treated with an antitoxin
* Used in small doses as Botox to smooth wrinkles, treat mirgraines. Blocks the release of Ach causing paralysis.
55
New cards
ATP reserves
* First source of energy for muscle contraction
* Muscle cells store only a small amount-must be able to regenerate ATP
* Muscle cells store only a small amount-must be able to regenerate ATP
56
New cards
Creatine Phosphate
* Initial source of energy to regenerate ATP from ADP and P.
* Stores energy in phosphate bond
* Stores energy in phosphate bond
57
New cards
Cellular respiration
* Must be used to fuel longer periods of muscle contraction
* Breaks down glucose to produce ATP
* Glucose stored as glycogen in muscle cells
* Breaks down glucose to produce ATP
* Glucose stored as glycogen in muscle cells
58
New cards
Types of phases of cellular respiration:
* Anaerobic Phase
* Aerobic Phase
* Aerobic Phase
59
New cards
Anaerobic (does NOT require O2) Phase
* Glycolysis
* Occurs in cytoplasm/cytosol
* Produces little ATP- 2 ATP
* Occurs in cytoplasm/cytosol
* Produces little ATP- 2 ATP
60
New cards
Aerobic Phase
* Citric acid cycle and electron transport chain system
* Occurs in the mitochondria
* Produces the most ATP (max is 30 in a muscle cell)
* Occurs in the mitochondria
* Produces the most ATP (max is 30 in a muscle cell)
61
New cards
What does myoglobin do?
It stores extra oxygen in muscles (increases the amount of oxygen available in the muscle cells to support aerobic respiration.
* Important because blood flow may decrease when contracting muscle fibers compress blood vessels.
* Important because blood flow may decrease when contracting muscle fibers compress blood vessels.
62
New cards
Oxygen Debt
The amount of oxygen needed by liver cells to convert the accumulated lactic acid to glucose, and to restore muscle ATP and creatine phosphate concentrations.
63
New cards
Anaerobic (Lactic Acid) Threshold
* Shift in metabolism from aerobic to anaerobic, during strenuous muscle activity, when the above systems cannot supply the necessary O2
* Lactic acid is produced which goes to the liver to be converted to glucose. (Requires ATP)
* Lactic acid is produced which goes to the liver to be converted to glucose. (Requires ATP)
64
New cards
Muscle Fatigue
Inability to contract muscles (For example, during prolonged exercise)
* Common causes of muscle fatigue
* Decreased blood flow
* Ion imbalances across the sarcolemma
* Loss of desire to continue exercise (psychological)
* Accumulation of lactic acid (controversial)
* Common causes of muscle fatigue
* Decreased blood flow
* Ion imbalances across the sarcolemma
* Loss of desire to continue exercise (psychological)
* Accumulation of lactic acid (controversial)
65
New cards
Muscle Cramp
* Not fully understood
* Sustained, involuntary muscle contraction
* May be caused by changes in electrolytes concentration in extracellular fluids in the area
* Sodium
* Chlorine
* Magnesium
* Potassium
* Calcium
* Sustained, involuntary muscle contraction
* May be caused by changes in electrolytes concentration in extracellular fluids in the area
* Sodium
* Chlorine
* Magnesium
* Potassium
* Calcium
66
New cards
Heat production
* Heat is a byproduct of cellular respiration in active cells. In other words, active cells generate heat.
* Muscle contraction will release heat
* Muscle cells are a major source of body heat. Muscle tissue is a large portion of body mass.
* More than half the energy release in cellular respiration becomes heat; less than half is transferred to ATP.
* Blood transports heat throughout body core.
* Muscle contraction will release heat
* Muscle cells are a major source of body heat. Muscle tissue is a large portion of body mass.
* More than half the energy release in cellular respiration becomes heat; less than half is transferred to ATP.
* Blood transports heat throughout body core.
67
New cards
Threshold Stimulus
Minimum strength of stimulation of a muscle fiber required to cause contractions
68
New cards
What is a twitch?
* A contractile response of a single muscle fiber to a single impulse
* Twitches vary in strengths (contributing factors):
* Development of fatigue
* Length to which fiber is stretched before stimulation
* Twitches vary in strengths (contributing factors):
* Development of fatigue
* Length to which fiber is stretched before stimulation
69
New cards
Period of times associated with a twitch
* Latent period- Delay between stimulation and start of contraction (approximately 2 milliseconds)
* Period of contraction- Fiber pulls at attachments
* Period of relaxation- Pulling forces decrease
* Period of contraction- Fiber pulls at attachments
* Period of relaxation- Pulling forces decrease
70
New cards
What does a myogram do?
It records events of a muscle twitch.
71
New cards
Length-Tension Relationship
* The length of muscle fiber before stimulation determines the amount of force it can develop.
* Optimum starting length is resting length of the fiber which allows the greatest force to develop.
* Stretched muscle fiber develop less force, since some myosin heads cannot reach binding sites on actin.
* Shortened muscle fiber also develop less force, since compressed sarcomeres cannot shorten further.
* Optimum starting length is resting length of the fiber which allows the greatest force to develop.
* Stretched muscle fiber develop less force, since some myosin heads cannot reach binding sites on actin.
* Shortened muscle fiber also develop less force, since compressed sarcomeres cannot shorten further.
72
New cards
Whole muscle contraction
* The actions we perform usually require the contribution of multiple muscle fibers simultaneously.
* We can electrically stimulate the whole muscle which contracts the muscle.
* When contracted muscles will pull on levers (bones).
* We can electrically stimulate the whole muscle which contracts the muscle.
* When contracted muscles will pull on levers (bones).
73
New cards
Summation
* Process by which the force of individual muscle fiber twitch combine, when frequency of stimulation increases.
* Produces sustained contractions and can lead to partial or complete tetanic contractions
* Produces sustained contractions and can lead to partial or complete tetanic contractions
74
New cards
What are the types of Tetanus?
Partial Tetany and Complete Tetany
75
New cards
What is Partial Tetany and Complete Tetany?
Partial Tetany
* Occurs at higher frequencies of stimulation
* Time spent in relaxation between twitches become very brief
Complete Tetany
* Occurss at very high frequencies of stimulation
* Does not occur in body, only in laboratories
* Forceful sustained contraction has no relaxation between twitches.
* Occurs at higher frequencies of stimulation
* Time spent in relaxation between twitches become very brief
Complete Tetany
* Occurss at very high frequencies of stimulation
* Does not occur in body, only in laboratories
* Forceful sustained contraction has no relaxation between twitches.
76
New cards
What is a motor unit?
A motor neuron plus all of the muscle fibers it controls.
(Most muscle fibers have only one motor end plate)
* A whole muscle consists of many motor units
(Most muscle fibers have only one motor end plate)
* A whole muscle consists of many motor units
77
New cards
Precise movements of motor units
Produced with fewer muscle fibers in a motor unit.
* Example: the motor unit of the muscle that moves the eye including fewer than 10 muscle fibers per motor unit and can produce very slight movements
* Example: the motor unit of the muscle that moves the eye including fewer than 10 muscle fibers per motor unit and can produce very slight movements
78
New cards
Coarse movements of motor units
Produced with large numbers of fibers in a motor unit
* Motor units of the large muscle in the back may include a hundred or more muscle fibers. Movements are larger scale than the eye.
* Motor units of the large muscle in the back may include a hundred or more muscle fibers. Movements are larger scale than the eye.
79
New cards
Sustained contractions
* Smaller motor units (smaller diameter axons)- recruited first
* Large motor units (larger diameter axons)- recruited later and with greater force
* Summation and recruitment can produce sustained contractions of increasing strength
* Whole muscle contractions are smooth movements. Individuals twitches do not normally occur. Partial or tetanic contractions of muscle fibers are common.
* Large motor units (larger diameter axons)- recruited later and with greater force
* Summation and recruitment can produce sustained contractions of increasing strength
* Whole muscle contractions are smooth movements. Individuals twitches do not normally occur. Partial or tetanic contractions of muscle fibers are common.
80
New cards
What is muscle tone (tonus)?
Continuous state of partial contractions in resting muscles.
* Contributes to maintaining posture
* Taught neck, head, trunk, and lower limbs enable a person to sit up, stand, hold up head etc.
* Lose consciousness and the body collapses
* Contributes to maintaining posture
* Taught neck, head, trunk, and lower limbs enable a person to sit up, stand, hold up head etc.
* Lose consciousness and the body collapses
81
New cards
What happens in isotonic contractions?
Muscle contracts and changes length. (Means equal force)
82
New cards
Types of Isotonic contractions
* Concentric- shortening contraction; occurs when lifting an object
* Eccentric- lengthening contraction; occurs when force not sufficient to lift object (lowering a hand weight)
* Eccentric- lengthening contraction; occurs when force not sufficient to lift object (lowering a hand weight)
83
New cards
Isometric contractions
* Muscle contracts but does NOT change length
* Means “equal length”
* Tension develops, but parts attached to muscle do not move (no movement-holding object in place)
* Means “equal length”
* Tension develops, but parts attached to muscle do not move (no movement-holding object in place)
84
New cards
Muscles vary in the following ways:
* Contraction speed: Slow or Fast
* Method of ATP production: Oxidatively or Glycolytically
* Method of ATP production: Oxidatively or Glycolytically
85
New cards
Three types of muscle fibers found in human:
* Slow Twitch fibers (Type I)
* Fast-twitch fatigue-resistant fibers (Type IIa)
* Fast-twitch glycolytic fibers (Type IIb)
* Fast-twitch fatigue-resistant fibers (Type IIa)
* Fast-twitch glycolytic fibers (Type IIb)
86
New cards
Slow-twitch fibers (Type I) (Will be on test)
* Always oxidative
* Resistant to fatigue (due to high ATP production)
* Red fibers (High myoglobin)
* Abundant myoglobin (stores oxygen in muscles)
* Good blood supply
* Many mitochondria
* Slow ATPase activity; slow to contract
* Resistant to fatigue (due to high ATP production)
* Red fibers (High myoglobin)
* Abundant myoglobin (stores oxygen in muscles)
* Good blood supply
* Many mitochondria
* Slow ATPase activity; slow to contract
87
New cards
Fast-twitch fatigue-resistant fibers (Type IIa) (Might be on test so still know it)
* Intermediate twitch fibers
* Intermediate oxidative capacity
* Intermediate amount of myoglobin
* White fibers (have less myoglobin)
* Resistant to fatigue
* Rapid ATPase activity
* Intermediate oxidative capacity
* Intermediate amount of myoglobin
* White fibers (have less myoglobin)
* Resistant to fatigue
* Rapid ATPase activity
88
New cards
Fast-twitch glycolytic fibers (Type IIb) (Will be on test)
* Anaerobic respiration (glycolysis)
* White fibers (less myoglobin)
* Poorer blood supply than slow-twitch fibers
* Fewer mitochondria than slow twitch
* More SR than slow-twitch (SR to store and absorb calcium ions)
* Susceptible to fatigue
* Fast ATPase activity; contract rapidly
* White fibers (less myoglobin)
* Poorer blood supply than slow-twitch fibers
* Fewer mitochondria than slow twitch
* More SR than slow-twitch (SR to store and absorb calcium ions)
* Susceptible to fatigue
* Fast ATPase activity; contract rapidly
89
New cards
What is hypertrophy and atrophy?
* Hypertrophy- enlargement of skeletal muscle that is exercised
* Atrophy- decrease in size (actin and myosin filaments) and strength of skeletal muscle that is unused. Can happen if neurons no longer supply a signal.
* Atrophy- decrease in size (actin and myosin filaments) and strength of skeletal muscle that is unused. Can happen if neurons no longer supply a signal.
90
New cards
What does Aerobic and Forceful exercise stimulate?
* Aerobic exercise simulates slow-twitch fibers; in response, fibers increase their capillaries and mitochondria
* Forceful exercise simulates mainly fast-twitch fibers; in response, fibers produce new actin and myosin filaments, and the muscle enlarges.
* Forceful exercise simulates mainly fast-twitch fibers; in response, fibers produce new actin and myosin filaments, and the muscle enlarges.
91
New cards
Smooth muscle
Compared to skeletal muscle fibers, smooth muscle fibers are:
* Shorter
* Single, centrally located nucleus
* Elongated with tapering ends (tissue looks like spindles)
* Myofilaments randomly organized (so they have actin, myosin, and myofibrils)
* Lack striations
* Lack transverse tubules
* Sarcoplasmic reticulum (SR) not well developed
* Shorter
* Single, centrally located nucleus
* Elongated with tapering ends (tissue looks like spindles)
* Myofilaments randomly organized (so they have actin, myosin, and myofibrils)
* Lack striations
* Lack transverse tubules
* Sarcoplasmic reticulum (SR) not well developed
92
New cards
Smooth muscle SIMILARITIES to skeletal muscle
* Mechanisms reflect reactions to actin and myosin
* Triggered by membrane impulses and release of calcium ions
* Both use energy from ATP molecules (have mitochondria)
* Neurotransmitters: acetylcholine
* Triggered by membrane impulses and release of calcium ions
* Both use energy from ATP molecules (have mitochondria)
* Neurotransmitters: acetylcholine
93
New cards
Smooth muscle DIFFERENCES to skeletal muscle
* Does not have troponin; instead has calmodulin-binds to calcium activating contraction
* Calcium needed diffuses into the cell from extracellular fluid not SR
* Neurotransmitters: norepinephrine SO SMOOTH MUSCLE HAS BOTH ACETYLCHOLINE AND NOREPINEPHRINE
* Calcium needed diffuses into the cell from extracellular fluid not SR
* Neurotransmitters: norepinephrine SO SMOOTH MUSCLE HAS BOTH ACETYLCHOLINE AND NOREPINEPHRINE
94
New cards
What are the two types of smooth muscle?
* Multi-unit smooth muscle
* Visceral smooth muscle
* Visceral smooth muscle
95
New cards
Multi-unit smooth muscle
* Cells are less organized
* Function as separate units
* Fibers function independently
* Iris of eye, walls of blood vessels
* Stimulated by neurons, hormones
* Function as separate units
* Fibers function independently
* Iris of eye, walls of blood vessels
* Stimulated by neurons, hormones
96
New cards
What role does hormones play in multi-unit smooth muscles?
It can stimulate or inhibit contractions or may alter the degree of response to neurotransmitters.
97
New cards
Visceral smooth muscles
* Single-unit smooth muscle; cells respond as a unit
* Sheets of spindle-shaped muscle fibers
* Fibers held together by gap junctions
* Exhibit rhythmicity
* Conduct peristalsis
* Walls of most hollow organs (intestines, stomach, etc.)
* More common type of smooth muscle
* Sheets of spindle-shaped muscle fibers
* Fibers held together by gap junctions
* Exhibit rhythmicity
* Conduct peristalsis
* Walls of most hollow organs (intestines, stomach, etc.)
* More common type of smooth muscle
98
New cards
Smooth muscle contractions RESEMBLE skeletal muscle contractions in the following ways:
* Interaction between actin and myosin
* Both use calcium and ATP
* Both are triggered by membrane impulses
* Both use calcium and ATP
* Both are triggered by membrane impulses
99
New cards
Smooth muscle contractions DIFFER from skeletal muscle contraction in the following ways:
* Smooth muscle lacks troponin; used calmodulin instead
* Two neurotransmitters affect smooth muscle: Acetylcholine (Ach) and norepinephrine (NE)
* Hormones can stimulate or inhibit smooth muscle
* Stretching can trigger smooth muscle contractions
* Smooth muscle slower to contraction and relax
* Smooth muscle more resistant to fatigue
* Smooth muscles can change length without changing tautness.
* Two neurotransmitters affect smooth muscle: Acetylcholine (Ach) and norepinephrine (NE)
* Hormones can stimulate or inhibit smooth muscle
* Stretching can trigger smooth muscle contractions
* Smooth muscle slower to contraction and relax
* Smooth muscle more resistant to fatigue
* Smooth muscles can change length without changing tautness.
100
New cards
Cardiac Muscle
* Located only in the heart
* Striated muscle cells
* Muscle fiber joined together by intercalated discs
* Fibers branch, contains a single nucleus; has many mitochondria
* Network of fibers contracts as a unit (syncytium)
* Self-exciting and rhythmic
* Does not require stimulation from neurons
* Longer refractory period (muscle fiber cannot be stimulated until repolarization is complete) than skeletal muscle.
* No sustained or tetanic contractions
* Striated muscle cells
* Muscle fiber joined together by intercalated discs
* Fibers branch, contains a single nucleus; has many mitochondria
* Network of fibers contracts as a unit (syncytium)
* Self-exciting and rhythmic
* Does not require stimulation from neurons
* Longer refractory period (muscle fiber cannot be stimulated until repolarization is complete) than skeletal muscle.
* No sustained or tetanic contractions