Cardiac Physiology
1/87
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
88 Terms
What is the heart's main function, and how is it assessed?
Maintain blood circulation. Assessed using heart rate, stroke volume, and cardiac output. Summary 1
What are the two phases of the cardiac cycle?
Systole (blood pumped from heart) and diastole (heart fills with blood). Summary 2
What initiates and coordinates heart muscle contraction?
Conduction system, a collection of nodes and specialized conduction cells. Summary 3
What is the role of pacemaker cells (e.g., sinus node)?
Autonomously generate action potentials (APs). Summary 4
What happens after the conduction system transmits the AP throughout the myocardium?
Electrical excitation leads to myocardial contraction (electromechanical coupling). Summary 5
What prevents immediate re-excitation after contraction?
Refractory period. Summary 6
How does the Frank-Starling mechanism maintain cardiac output?
Increases myocardial contractility (and stroke volume) in response to increased preload (end-diastolic volume). Summary 7
How does the autonomic nervous system regulate the heart?
Regulates heart rate, excitability, conductivity, relaxation, and contractility. Summary 8
What is heart rate (HR)?
Number of heart contractions per minute (bpm). Normal: 60-100 bpm at rest. Definitions 9
What is stroke volume (SV)?
Volume of blood pumped by left or right ventricle in a single beat. SV = EDV - ESV. Definitions 10
What is ejection fraction (EF)?
Proportion of EDV ejected from ventricle. EF = SV/EDV = (EDV-ESV)/EDV. Normal: 50-70%. Index of myocardial contractility. Definitions 11
What is venous return?
Rate at which blood flows back to the heart, typically equals cardiac output. Definitions 12
What is cardiac output (CO)?
Volume of blood pumped through circulatory system per minute (~5 L/min at rest). CO = HR x SV. Definitions 13
How does increased heart rate affect cardiac output during physical activity?
Increase in CO is mediated by increasing heart rate (SV becomes constant). Definitions 14
How is cardiac output measured via the Fick principle?
CO = (O2 consumption)/(arterial O2 content - venous O2 content). Definitions 15
How is cardiac output measured via mean arterial pressure (MAP)?
MAP = CO x TPR. MAP = (SP + 2 x DP)/3. Definitions 16
How does increased HR affect SV?
Diastole is shortened, which decreases SV due to less filling time. Definitions 17
How is maximum CO reached?
Reaches ≥160/bpm max CO & decreases, as SV declines faster than HR increases. Definitions 18
What is the cardiac index?
Cardiac output (L/min) in relation to body surface area (m2). Definitions 19
What is the volumetric flow rate?
Volume of blood that flows across a valve per second. Used to calculate flow across stenotic valves. Q = v x A Definitions 20
What factors affect myocardial oxygen demand?
Heart rate, contractility, wall tension (ventricular diameter), afterload. Definitions 21
Where does the coronary sinus drain?
Receives drainage from most epicardial ventricular veins & contains majority of deoxygenated blood. Definitions 22
What are normal cardiac blood pressures (measured via Swan-Ganz catheterization)?
Right atrium: < 5 mm Hg, Right ventricle: 25/5 mm Hg, Left atrium: < 12 mm Hg, Left ventricle: 130/10 mm Hg. Definitions 23
What is coronary perfusion pressure?
Driving pressure forcing blood into coronary arteries during diastole. Calculated as difference in pressure between aorta and left ventricle during diastole. Definitions 24
What are the two phases of the cardiac cycle?
Systole (blood pumped from the heart) and diastole (heart fills with blood). Cardiac cycle 25
What are the four phases of heart action?
Isovolumetric contraction, Systolic ejection, Isovolumetric relaxation, and Ventricular filling. Cardiac cycle 26
What is the main function of isovolumetric contraction?
Ventricular contraction. Cardiac cycle 27
What are the pressure and volume changes during isovolumetric contraction?
LV Pressure: 8 mm Hg → ∼ 80 mm Hg & RV Pressure: 5 mm Hg → 25 mm Hg; Ventricular volume remains constant (∼ 150 mL). Cardiac cycle 28
What characterizes isovolumetric contraction?
Ventricle contracts (pressure increases) with no corresponding ventricular volume change, AV valves close & semilunar valves are closed. Cardiac cycle 29
When does isovolumetric contraction occur?
Follows ventricular filling, Occurs in early systole, directly after AV valves close and before semilunar valves open. Cardiac cycle 30
When is O2 consumption at its highest?
Period of highest O2 consumption during isovolumetric contraction Cardiac cycle 31
What is the main function of systolic ejection?
Blood is pumped from the ventricles into the circulation and lungs. Cardiac cycle 32
What are the pressure and volume changes during systolic ejection?
Pressure: increases from ∼ 80 mm Hg to 120 mm Hg & then decreases until aortic/pulmonary valves close; Volume: ejection of ∼ 90 mL SV (150 mL → 60 mL). Cardiac cycle 33
When does systolic ejection occur?
Follows isovolumetric contraction; Occurs between the opening and closing of the aortic valve and pulmonary valve. Cardiac cycle 34
What is the main function of isovolumetric relaxation?
Ventricular relaxation. Cardiac cycle 35
What are the pressure and volume changes during isovolumetric relaxation?
Pressure: decreases to ∼ 10 mm Hg (LV) & ∼ 5 mm Hg (RV); Volume: remains constant at ∼ 60 mL. Cardiac cycle 36
What characterizes isovolumetric relaxation?
Ventricles relax (pressure decreases) with no ventricular volume change until ventricular pressure is lower than atrial pressure and AV valves open and all valves closed. Cardiac cycle 37
When does isovolumetric relaxation occur?
Follows systolic ejection; Occurs between aortic valve closing and mitral valve opening. Cardiac cycle 38
What is the dicrotic notch?
Slight increase of aortic pressure in early diastole that corresponds to closure of the aortic valve. Cardiac cycle 39
What occurs during early diastole with respect to coronary blood flow?
Coronary blood flow peaks & coronary arteries fill with blood. Cardiac cycle 40
What is the main function of ventricular filling?
Ventricles fill with blood Cardiac cycle 41
What are the two phases of ventricular filling?
Rapid and Reduced filling. Cardiac cycle 42
What are the pressure and volume changes during ventricular filling?
Pressure LV: ∼ 8 mm Hg; RV: ∼ 5 mm Hg (2-8 mm Hg); Volume: fills with ∼ 90 mL (60 mL → 150 mL). Cardiac cycle 43
What happens during rapid filling?
Blood flows passively from atria to ventricles. Largest volume of ventricular filling occurs. Follows isovolumetric relaxation & Occurs in early diastole, immediately after mitral valve opening. Cardiac cycle 44
What happens during reduced filling?
Follows rapid filling & Occurs in late diastole, immediately before atrioventricular valves close. Cardiac cycle 45
When are all heart valves closed?
During isovolumetric contraction and relaxation. Cardiac cycle 46
What happens during states of increased heart rate?
Duration of diastole decreases, less time for coronary arteries to fill, patients with narrow coronary arteries experience chest pain (angina pectoris). Cardiac cycle 47
What is the volume-pressure loop used to measure?
Measure cardiac performance. Cardiac cycle 48
Define each aspect of cardiac cycle loop: (1) End-diastolic state, (1 → 2) Isovolumetric contraction, (2) Opening of the semilunar valve, (2 → 3) Ejection phase, (3) Closure of the semilunar valve, (3 → 4) Isovolumetric relaxation, (4) Opening of the atrioventricular valve, and (4 → 1) Filling phase.
(1) AV valve closure, start of systole; (1 → 2) contraction increases pressure, volume constant; (2) Ventricular pressure exceeds artery pressure; (2 → 3) pumps out stroke volume; (3) ventricle pressure falls below artery pressure; (3 → 4) ventricle relaxes, all valves closed; (4) Ventricle pressure falls below atrium pressure; (4 → 1) ventricles receive blood & restarts. Cardiac cycle 49
What changes in the Pressure-Volume loop indicate Mitral regurgitation?
Rounder, flatter loop. ↑ LV end-diastolic volume/pressure. ↑ Stroke volume. No isovolumetric contraction/relaxation. ↓ LV end-systolic volume. Tall V-wave. Cardiac cycle 50
What changes in the Pressure-Volume loop indicate Mitral stenosis?
Narrower, flatter loop. ↑ LA pressure. ↓ LV end-diastolic volume/stroke volume/ LV end-systolic volume. LA pressure > LV pressure during diastole. Cardiac cycle 51
What changes in the Pressure-Volume loop indicate Aortic regurgitation?
Rounder, taller loop. ↑ LV end-diastolic volume/stroke volume. Normal/↑ LV diastolic pressure. No isovolumetric relaxation. ↑ Pulse pressure. Cardiac cycle 52
What changes in the Pressure-Volume loop indicate Aortic stenosis?
Narrower, taller loop. ↑ LV end-systolic pressure/end-diastolic pressure/ end-systolic volume; ↓ Stroke volume. LV blood pressure > aortic pressure during systole. Cardiac cycle 53
What does the width of the volume-pressure loop represent?
The SV (the difference between EDV and ESV). Cardiac cycle 54
What is the conduction system of the heart?
Collection of nodes and specialized conduction cells that initiate and coordinate contraction of heart muscle. Conduction system of the heart 55
Where is the Sinoatrial (SA) node located, what are its characteristics, and what is its frequency?
Upper wall of right atrium. Natural pacemaker center with specialized pacemaker cells that spontaneously generate electrical impulses influenced by the autonomic nervous system. 60-80/min Conduction system of the heart 56
Where is the Atrioventricular (AV) node located, what are its characteristics, and what is its frequency?
Within the AV septum in the Koch triangle, superior and medial to coronary sinus opening. Receives SA impulses and passes to Bundle of His. Delays conduction for 60-120 ms, supplied by AV nodal artery. 40-50/min Conduction system of the heart 57
Where is the Bundle of His located, what are its characteristics, and what is its frequency?
Below the cardiac skeleton, within membranous interventricular septum. Receives from AV node, splits into left and right bundle branches terminating into Purkinje fibers. Prevents retrograde conduction. 30-40/min Conduction system of the heart 58
Where are the Purkinje fibers located, what are their characteristics, and what is their frequency?
Terminal conducting fibers in the subendocardium; Ensure synchronized contraction of the ventricles and has a long refractory period. 30-40/min Conduction system of the heart 59
What is the normal electrical conduction pathway in the heart?
SA node → atria (contraction) → AV node (slowed) → bundle of His → Purkinje fibers → ventricles (contraction). Conduction system of the heart 60
What do cardiac pacemaker cells (e.g., sinus node) do?
Autonomously and spontaneously generate an action potential (AP). Heart excitation 61
What does the electrical excitation of the myocardium result in?
Its contraction (see electromechanical coupling and filament sliding theory in muscle tissue). Heart excitation 62
What is the purpose of a refractory period?
Prevents immediate re-excitation. Heart excitation 63
Name the different types of Calcium Channels, their location, direction of flow, and Activation phase (affected tissue).
L-type Calcium Channel: Responsible for electromechanical coupling and located on cell membrane of cardiomyocytes with influx of extracellular Ca2+ into the cytoplasm during Plateau phase (myocardium) Upstroke phase (SA node). T-type Calcium Channel: Located on cell membrane of cardiac pacemaker cells with influx of extracellular Ca2+ into the cytoplasm during middle of phase 4 in pacemaker cells. Ryanodine Receptor: Ca2+ channel that opens after Ca2+ binding and is located on membrane of SR and transports Ca2+ from SR to the cytoplasm during Plateau phase (myocardium). Heart excitation 64
Name the function for all the major Calcium Pumps.
SERCA (sarcoplasmic Ca2+-ATPase) to help facilitate Efflux of Ca2+ from the cytoplasm into the SR and Na+/Ca2+ Exchanger to also Efflux of Ca2+ from the cytoplasm into the extracellular space Heart excitation 65
What does the funny channels (HCN, If) cause in the heart and what are its characteristics?
Nonselective cation channels in pacemaker cells that open as the membrane potential becomes more negative (hyperpolarized). Extracellular → intracellular upstroke phase (sinus node). Heart excitation 66
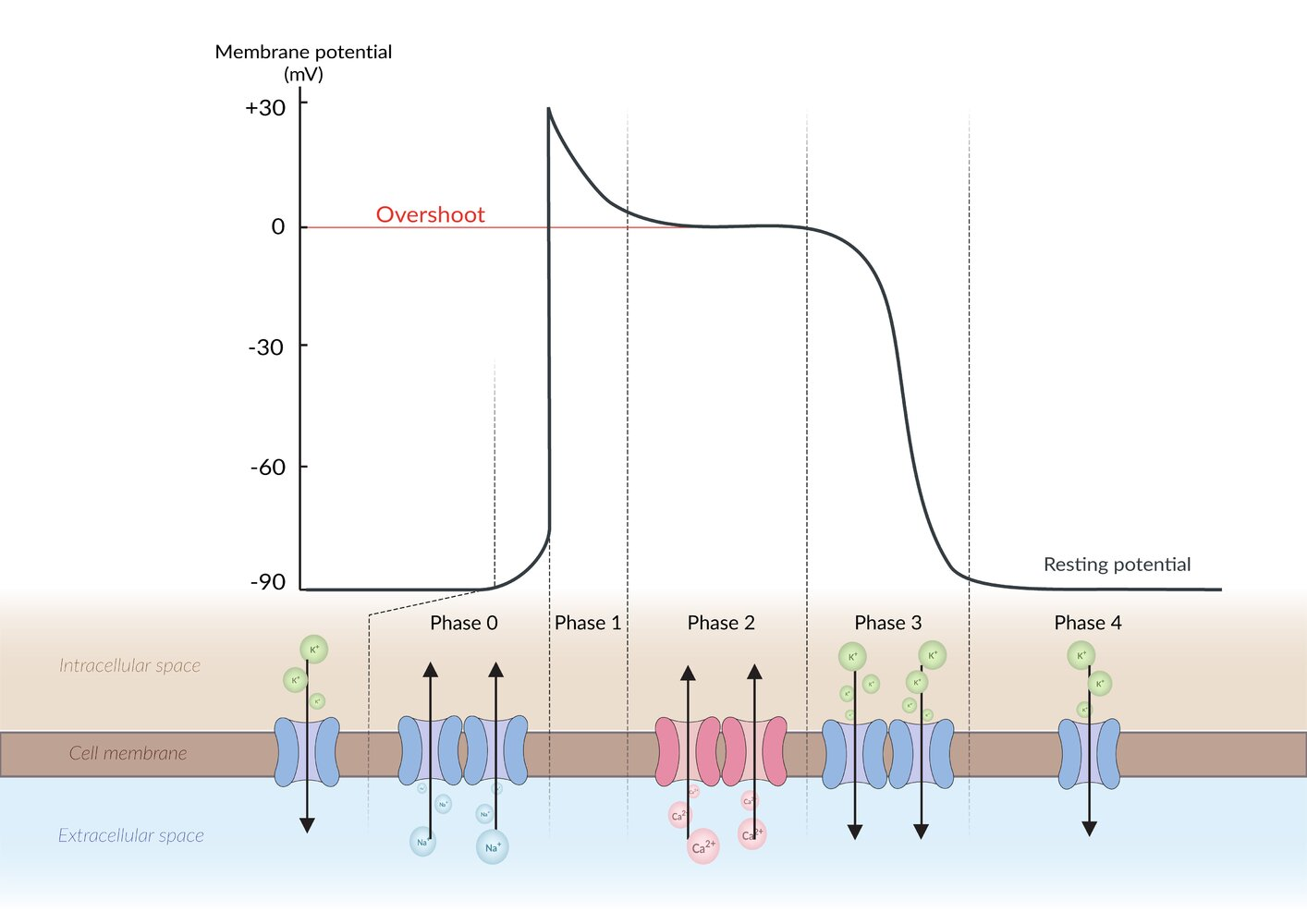
Name the phases of a Myocardial Action Potential and what occurs.
Phase 0: Upstroke occurs and action potential from pacemaker cell occurs. Depolarization: Fast Na+ channels open → rapid Na+ influx, Phase 1: Inactivation of voltage-gated Na+ channels and Transient K+ channels start to open, Phase 2: K+ efflux through delayed rectifier K+ channels and Ca2+ influx through voltage-gated L-type Ca2+channels occurs to trigger myocyte contraction, Phase 3: K+ efflux continues,Persistent outflow of K+ exceeds Ca2+ inflow and ions return to extracellular space, Phase 4: Stable Resting membrane potential at -90 mV due to outward K+ flow through channels. Heart excitation 67
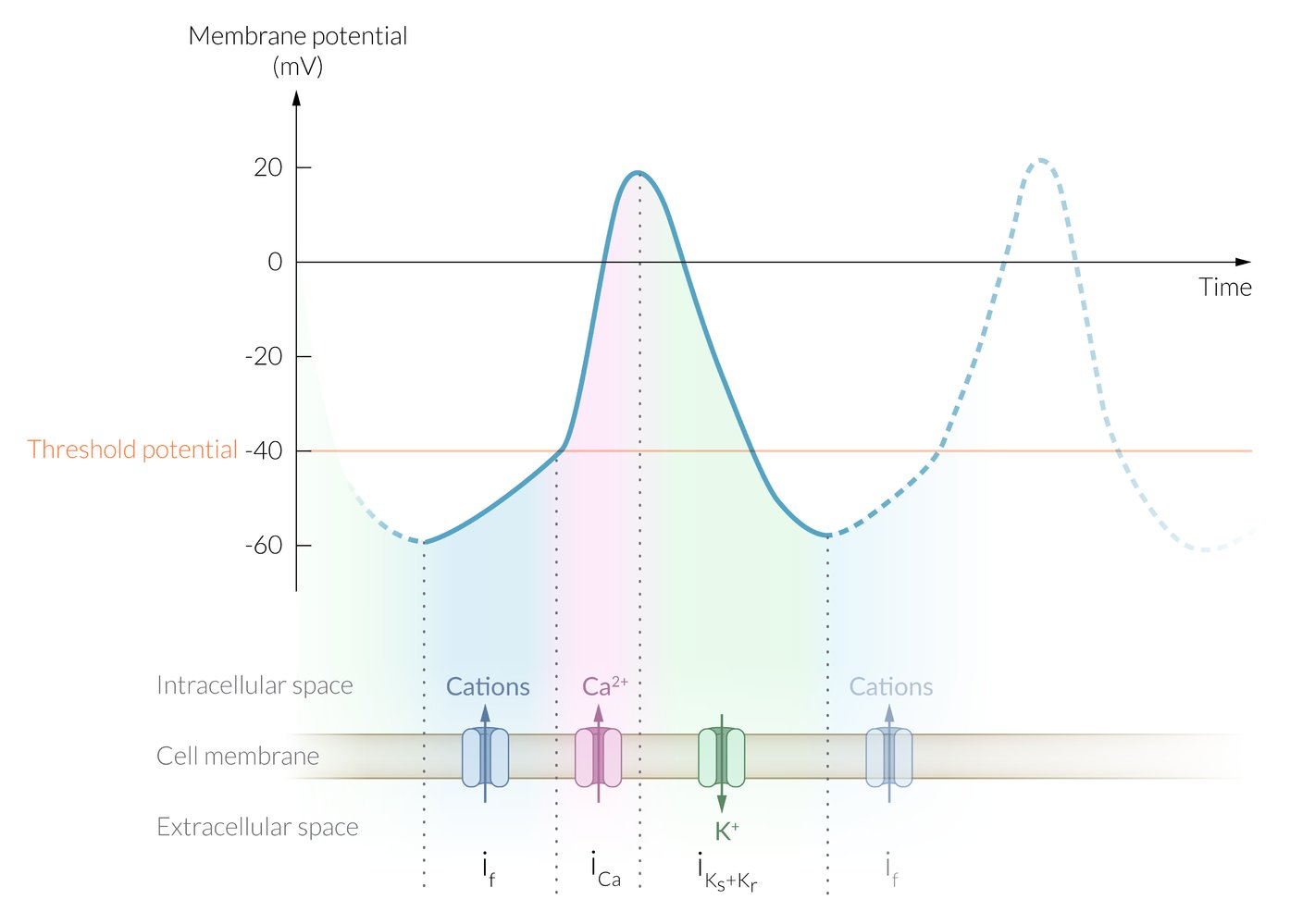
Name the phases of a Pacemaker Action Potential and what occurs.
Phase 0: Upstroke - At TMP -40 mV (threshold), L-type Ca2+ channels open → TMP increases. Phase 3: Repolarization. Closure of voltage-gated Ca2+ channels and Opening of delayed rectifier K+ channels. Phase 4: No resting phase. Gradual Na+/K+ entry via funny channels If (funny current or pacemaker current) → slow spontaneous depolarization. Heart excitation 68
What is the effective refractory period (ERP)?
Recovery period after stimulation where a second stimulus cannot generate a new AP in a depolarized cardiomyocyte. Heart excitation 69
What is the effect of the refractory period?
Ensures sufficient time for chamber emptying/refilling before next contraction, prevents re-excitation to avoid arrhythmia/tetany. Heart excitation 70
How does the firing frequency of the SA node affect other pacemaker sites?
SA node's firing is faster, so it activates these sites before they activate themselves (overdrive suppression). Heart excitation 71
How does the length of the plateau of the myocardial action potential help the heart function?
Allows heart muscle to relax after each contraction and prevents permanent contraction (tetany). Heart excitation 72
How can the heterogeneity of the refractory period lead to arrhythmias?
Different cells in the heart can have refractory heterogeneity allowing for the heart to be vulnerable from stimulus that cause arrhythmias. Heart excitation 73
Why should the shock from cardioversion be timed carefully?
Shock delivery must be synchronized with R wave (depolarization) and avoided during relative refractory period (T waves, repolarization). Heart excitation 74
What provides adaptation to short-term changes and long-term changes for cardiac activity?
Adaptation for short-term is provided by the Frank-Starling mechanism, and long-term regulation of the autonomic nervous system. Regulation of cardiac activity 75
What is the Frank-Starling mechanism?
Relationship between end-diastolic volume and cardiac stroke volume. Regulation of cardiac activity 76
How does increased end-diastolic volume affect contractility?
Increased end-diastolic volume (preload) will cause the myocardium to stretch and increase contractility which then increase stroke volume. Regulation of cardiac activity 77
What is the autonomic nervous system able to regulate in the heart?
Heart rate, excitability, conductivity, relaxation, and contractility. Regulation of cardiac activity 78
Which heart structures do Sympathetic fibers innervate? Which ones do Parasympathetic fibers innervate?
Sympathetic: innervate both atria and ventricles & Parasympathetic: innervate the atria only. Regulation of cardiac activity 79
What does each of the following terms mean: 1. Chronotropy, 2.Dromotropy, 3. Inotropy, 4. Lusitropy, and 5. Bathmotropy.
Any influence on: 1.heart rate, 2. conductivity of myocardium, 3. force of myocardial contraction, 4.rate of relaxation, and 5. excitability of the myocardium respectively. Regulation of cardiac activity 80
What is the effect and mechanism of action of Sympathetic stimulation?
Effect: Increases Heart rate, conduction, contractility, and relaxation. Mechanism of action: Activation of beta1 adrenergic receptors by epinephrine/norepinephrine →↑ adenylyl cyclase activity → ↑ cAMP → increased pacemaker & protein phosphorylation Regulation of cardiac activity 81
What is the effect and mechanism of action of Parasympathetic stimulation?
Effect: ↓ Heart rate and atrial contractility. Mechanism of action: on the heart through M2 receptor on SA/AV node - Reduces If channels conductance → ↓ pacemaker current - Increases slow K+ conductance - Vagal fibers innervate the AV node. Regulation of cardiac activity 82
What is preload, and what does it depend on?
Extent to which heart muscle fibers are stretched before the onset of systole. Depends on end-diastolic ventricular volume (EDV). Factors that affect cardiac output 83
What increases the Preload for the heart?
Increase: Venous constriction;Circulating blood volume: Factors that affect cardiac output 84
What decreases the Preload for the heart?
Decrease: Nitroglycerin, Inferior vena cava obstruction, Tricuspid and mitral valve stenosis, Aortic stenosis and Atrial tachycardia. Factors that affect cardiac output 85
What is afterload, and what determines it?
Force against which ventricle contracts to eject blood. Determined by mean arterial pressure (MAP) in aorta, which is influenced by total peripheral resistance (TPR). Factors that affect cardiac output 86
What occurs when there is increased afterload, and what equation describes it?
↑ Afterload → ↑ left ventricular pressure → ↑ left ventricular wall stress Described by the equation (LV wall stress = (LV pressure × radius)/ (2×LV wall thickness)) Factors that affect cardiac output 87
What are the 4 different factors that affect cardiac output and which direction do they increase or decrease?
Preload increases SV and decreases Venous return, Afterload decreases Systemic/Pulmonary vascular resistance, and Myocardial contractility increases or decreases in inotropy. Factors that affect cardiac output 88