biosex exam
1/207
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
208 Terms
New Brunswick LGBTQ rights
Children can ask to be called different name/pronoun at school without notifying parents
gender vs sex
Sex refers to the biological and physical characteristics that differentiate males from females, such as reproductive organs and chromosomes.
Gender refers to the social and cultural roles, behaviours, and expectations associated with being male or female.
It is important to recognize that gender identity may not always align with an individual's assigned sex at birth.
Influences on sex and the process as a whole
Social - cultural influences
External stimuli (things you see online making you less attracted to your reality)
Gender
Social Construct compromised of gender, expression, role, identity
Gender expression
Ones perception of gender including (but not limited to) physical, appearance, clothing choice, behavior. Expresses aspects of gender identity and role
Gender roles
A pattern of appearance, behavior that is associated with being a certain gender in a given culture. Gender role may not align with what is socially or stereotypically expected in ones sex assigned at birth.
Gender identity
Ones inherent sense/feeling of being a gender (women, man, non-binary, genderqueer, agender). Gender identity may not correspond with sex assigned at birth or to a persons physical characteristics
Gender dysphoria
Discomfort/distress related to experiencing a different gender than the sex assigned at birth. Also a diagnosis in the DSM-5 (gender euphoria is the opposite)
Gynophilic
Attraction to women
Amphiphilic
Attraction to men
Sex assigned at birth
Sex assigned at birth is the classification of an individual as male or female based on physical characteristics such as genitalia. It is typically determined by medical professionals shortly after birth. However, it is important to note that sex assigned at birth may not always align with an individual's gender identity or biological characteristics.
Gender identity
Gender identity refers to an individual's deeply held sense of their own gender, which may or may not align with the sex they were assigned at birth. It is a personal and subjective experience that can vary from person to person. Gender identity is an important aspect of a person's self-identity and can be different from their biological sex or the gender roles and expectations imposed by society. It is important to respect and affirm individuals' gender identities to promote inclusivity and support their well-being.
Gender dysphoria
Gender dysphoria is a condition where an individual experiences distress or discomfort due to a mismatch between their gender identity and the sex they were assigned at birth. It is recognized as a medical diagnosis and is often treated through various interventions, including therapy, hormone therapy, and gender-affirming surgeries. The goal of treatment is to alleviate the distress caused by gender dysphoria and help individuals live in alignment with their gender identity.
Sexual orientation
Sexual orientation refers to a person's enduring pattern of emotional, romantic, and/or sexual attractions to men, women, both genders, or neither gender. It is an intrinsic aspect of a person's identity and can be categorized as heterosexual, homosexual, bisexual, or asexual. Sexual orientation is not a choice and is believed to be influenced by a combination of genetic, hormonal, and environmental factors. It is important to respect and support individuals' sexual orientations as a fundamental aspect of human diversity.
Transgender
Transgender is a term for people whose gender identity is different from their assigned sex at birth. Gender identity is separate from biological sex. Some transgender individuals have medical interventions like hormone therapy or surgeries to align their appearance with their gender identity. It's important to respect and support transgender rights and identities.
Cisgender
Cisgender refers to individuals whose gender identity matches the sex they were assigned at birth. It is the opposite of transgender.
Gender non-binary
Gender non-binary refers to individuals who do not exclusively identify as male or female. They may identify as a combination of both genders, as neither gender, or as a different gender altogether. Non-binary individuals may use various terms to describe their gender identity, such as genderqueer, genderfluid, or agender. It is important to respect and acknowledge the gender identity of non-binary individuals and use their preferred pronouns.
Sexual Reproduction
Process of developing a genetically unique individual
Female gamete contributes ½ genetic content
Male gamete contributes ½ genetic content
homogametic
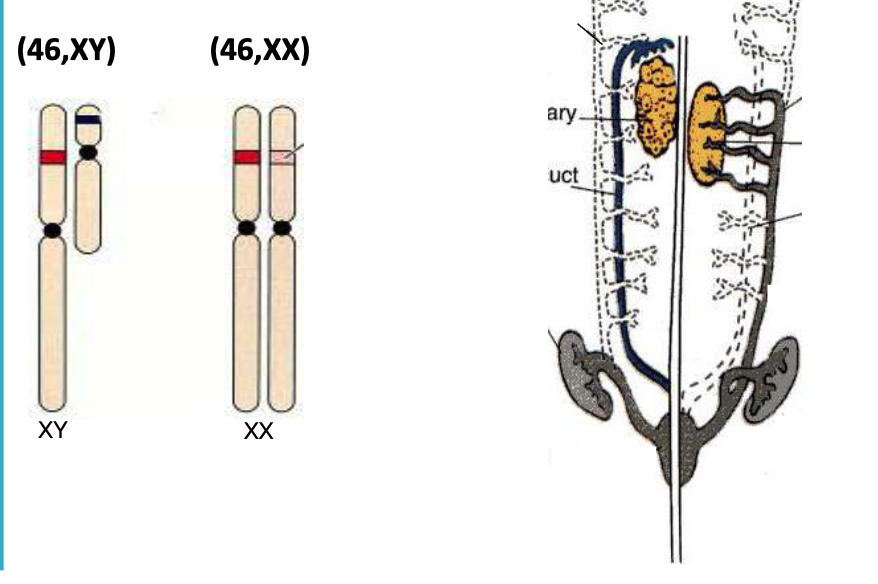
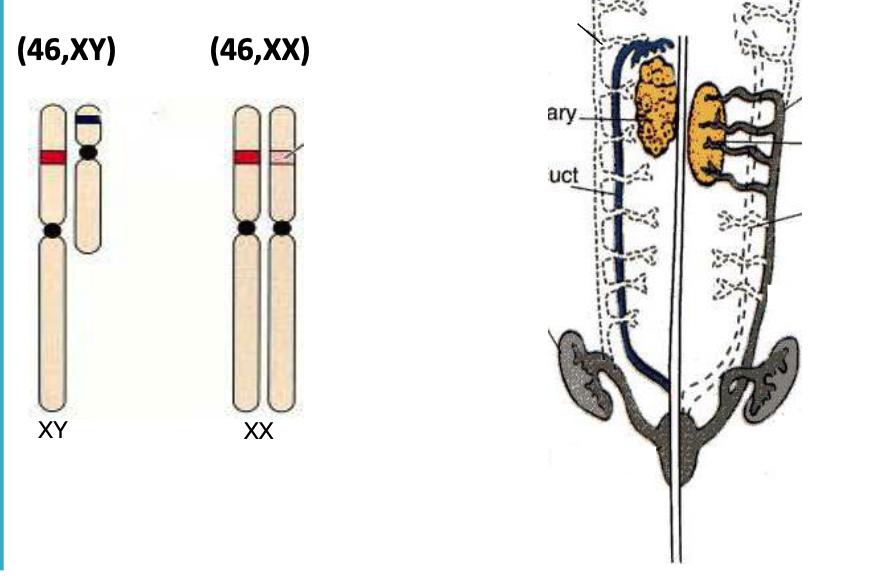
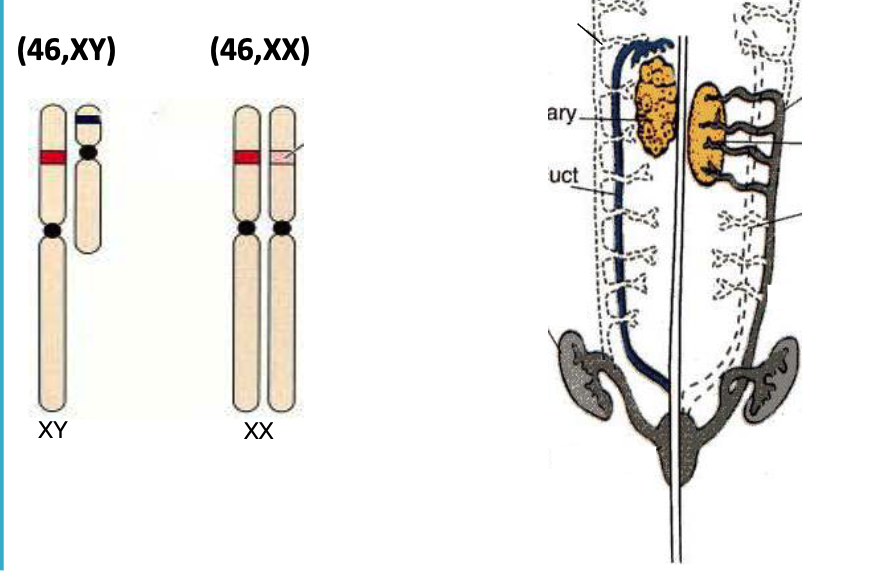
The term "homogametic" refers to an individual that has two of the same sex chromosomes. In humans, females are homogametic (XX), while males are heterogametic (XY).
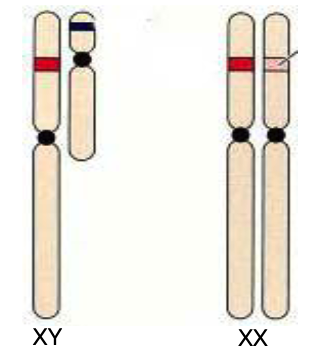
heterogametic
In biology, "heterogametic" means having two different sex chromosomes. In humans, males are heterogametic (XY) with one X and one Y chromosome, while females are homogametic (XX) with two X chromosomes.
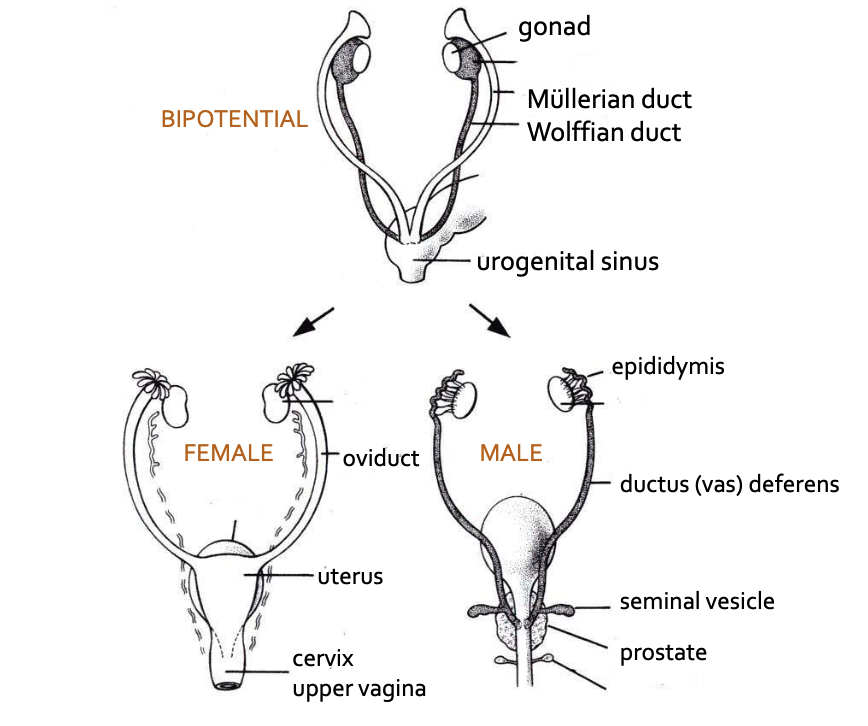
Bipotential Gonad
A bipotential gonad refers to an undifferentiated reproductive organ that has the potential to develop into either male or female gonads. During early embryonic development, the gonads are initially bipotential and can differentiate into testes or ovaries depending on the presence or absence of certain genetic factors. This process is regulated by the expression of specific genes and hormones. The bipotential gonad eventually undergoes sexual differentiation, leading to the development of either male or female reproductive structures.
Mullerian Duct
The Mullerian duct, also known as the paramesonephric duct, is a structure that develops in the early embryo and plays a crucial role in the formation of the female reproductive system. In females, the Mullerian duct gives rise to the fallopian tubes, uterus, cervix, and upper part of the vagina. It develops alongside the Wolffian duct, which gives rise to the male reproductive system. The presence of certain hormones determines whether the Mullerian duct develops into female reproductive organs or regresses in males.
Wolffian duct - dark tube in male figure
The Wolffian duct is a structure found in the development of the reproductive system in mammals, including humans. It is responsible for the formation of the male reproductive tract, including the epididymis, vas deferens, and seminal vesicles.
Developmental Events
Mini puberty
Adrenarche
Thelarche (F)
Gonadarche
Pubarche
Growth spurt
Spermarche
Menarche (F
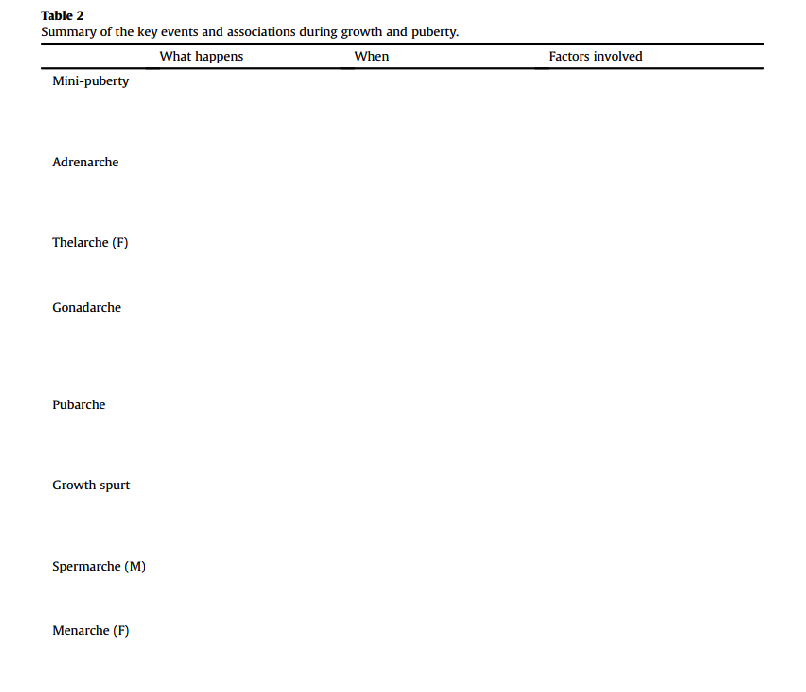
#1 Mini puberty
right after birth (2-3 months)
#2 Adrenarche
adrenal gland wakes up 6-9 y
Adrenarche is the term used to describe the maturation of the adrenal glands during childhood. It typically occurs between the ages of 6 and 8 years old and is characterized by an increase in the production of adrenal androgens, such as DHEA (dehydroepiandrosterone). Adrenarche is a normal part of development and is associated with the onset of pubic hair growth and the development of body odor. It is distinct from puberty, which involves the maturation of the reproductive system.
#3 Thelarche (F)
Thelarche is the onset of breast development in females, typically occurring during puberty. It is the first sign of secondary sexual characteristics in girls and is driven by hormonal changes, particularly the increase in estrogen levels. Thelarche usually begins between the ages of 8 and 13, but the exact timing can vary. It is a normal and expected part of female development.
#4 Gonadarche
Gonadarche refers to the onset of puberty and the development of the gonads (testies), which are the reproductive organs. It is characterized by the maturation of the testes in males and the ovaries in females, leading to the production of sex hormones and the ability to reproduce. Gonadarche typically occurs around the age of 9-14 in girls and 10-17 in boys.
#5 Pubarche
Pubarche refers to the onset of pubic hair growth during puberty. It is one of the physical changes that occur as a result of hormonal changes in both boys and girls. Pubarche typically occurs after the onset of adrenarche, which is the maturation of the adrenal glands. The timing and progression of pubarche can vary among individuals, but it generally occurs between the ages of 8 and 14.
#6 Growth spurt
Growth spurt refers to a period of rapid growth and development that occurs during puberty. It is characterized by a significant increase in height and weight, as well as changes in body proportions. Growth spurts typically occur between the ages of 10 and 16 for girls, and between the ages of 12 and 18 for boys. During this time, various hormones, such as growth hormone and sex hormones, play a crucial role in promoting growth and maturation of the body.
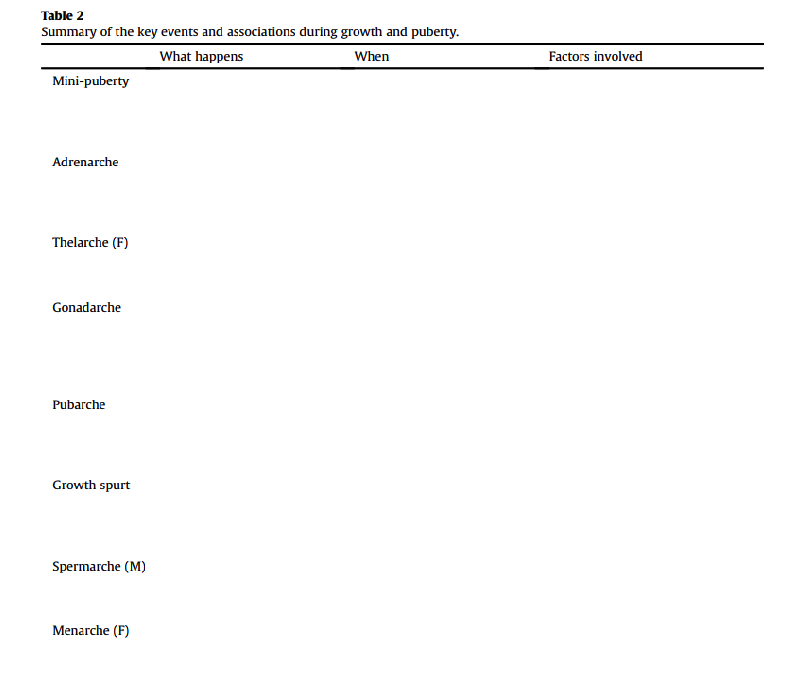
#7 Spermarche
Spermarche refers to the first occurrence of ejaculation in males, marking the onset of sperm production and sexual maturity. It typically occurs during puberty, around the age of 12 to 16 years old. Spermarche is a normal and natural part of male development.
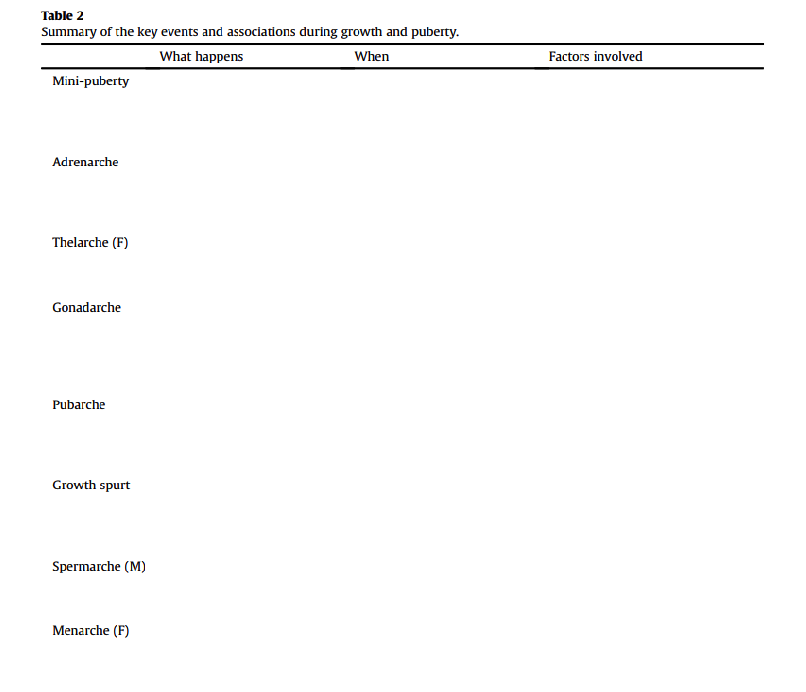
#8 Menarche (F)
Menarche is the term used to describe the first occurrence of menstruation in females. It marks the onset of puberty and the ability to become pregnant.
NO OVULATION
Pubertal Development
Pubertal development refers to the physical, cognitive, and emotional changes that occur during adolescence. It is a period of rapid growth and maturation, marked by the development of secondary sexual characteristics, such as breast development in girls and facial hair growth in boys. Hormonal changes, particularly the increase in sex hormones like estrogen and testosterone, play a crucial role in pubertal development. These changes also impact cognitive and emotional development, leading to increased independence, self-awareness, and the formation of personal identity.
Androgens
Androgens are a group of hormones that play a crucial role in pubertal development. They are primarily produced in the testes in males and in the ovaries and adrenal glands in females. The main androgen is testosterone, which is responsible for the development of male secondary sexual characteristics such as facial hair, deepening of the voice, and muscle growth. In females, androgens contribute to the development of pubic and underarm hair, as well as the sex drive. Androgens also play a role in bone growth and maintenance of overall health.
Testoterone
Testosterone is a hormone primarily found in males, although females also produce small amounts of it. It plays a crucial role in the development of male reproductive tissues and secondary sexual characteristics. Testosterone is responsible for promoting muscle and bone growth, regulating sex drive, and influencing mood and energy levels. It is produced in the testes in males and in the ovaries and adrenal glands in females. Testosterone levels can be influenced by various factors, including age, genetics, and overall health.
Estrogens
Estrogens are a group of hormones that play a crucial role in the development and functioning of the female reproductive system. They are primarily produced in the ovaries, although small amounts are also produced in the adrenal glands and fat tissues. Estrogens are responsible for the development of secondary sexual characteristics in females, such as breast development and the widening of the hips. They also regulate the menstrual cycle and are involved in the maintenance of bone density. Additionally, estrogens have an impact on mood, cognitive function, and cardiovascular health.
Androgens vs Estrogens
Androgens and estrogens are two types of sex hormones found in both males and females, but in different proportions. Androgens, such as testosterone, are primarily responsible for the development and maintenance of male characteristics, including the growth of facial and body hair, deepening of the voice, and muscle development. Estrogens, such as estradiol, are primarily responsible for the development and maintenance of female characteristics, including breast development, regulation of the menstrual cycle, and maintenance of bone health. While both hormones are present in both sexes, their levels and effects differ, contributing to the sexual dimorphism observed in humans.
Hormone
A hormone is a chemical signal/substance produced by the endocrine glands in the body. It acts as a messenger, regulating various physiological processes and maintaining homeostasis. Hormones are released into the bloodstream and travel to target cells or organs, where they bind to specific receptors and initiate a response. Examples of hormones include insulin, which regulates blood sugar levels, and estrogen, which controls female reproductive functions.
Endrocrine hormone - Produced in one spot used in a different spot
An endocrine hormone is a chemical substance secreted by an endocrine gland into the bloodstream. It acts as a messenger to regulate various physiological processes in the body. Examples of endocrine hormones include insulin, cortisol, estrogen, and testosterone.
Paracrine - Produced in one spot acts in same spot (global hormones)
Paracrine signaling is a form of cell communication in which a cell releases signaling molecules that act on nearby cells. These signaling molecules, called paracrine factors, are released into the extracellular fluid and diffuse to nearby target cells. This type of signaling is important for coordinating cellular activities within tissues and organs. Examples of paracrine signaling include the release of growth factors during tissue repair and the release of neurotransmitters in the nervous system.
Endogenous versus exogenous hormone
Internal made by you vs external made for you (inject or inject to receive this hormone) BC
Endogenous hormones are produced within the body, while exogenous hormones are introduced from outside the body.
cholesterol
Cholesterol is a waxy, fat-like substance that is found in all cells of the body. It is essential for the production of hormones, vitamin D, and bile acids. While cholesterol is necessary for normal body function, high levels of cholesterol in the blood can increase the risk of heart disease. It is important to maintain a healthy diet and lifestyle to keep cholesterol levels in check.
Cholesterol is the precursor for all steroid hormones
Cholesterol is the precursor for all steroid hormones
Cholesterol is a precursor for some steroid hormones, such as cortisol, aldosterone, and sex hormones like testosterone and estrogen.
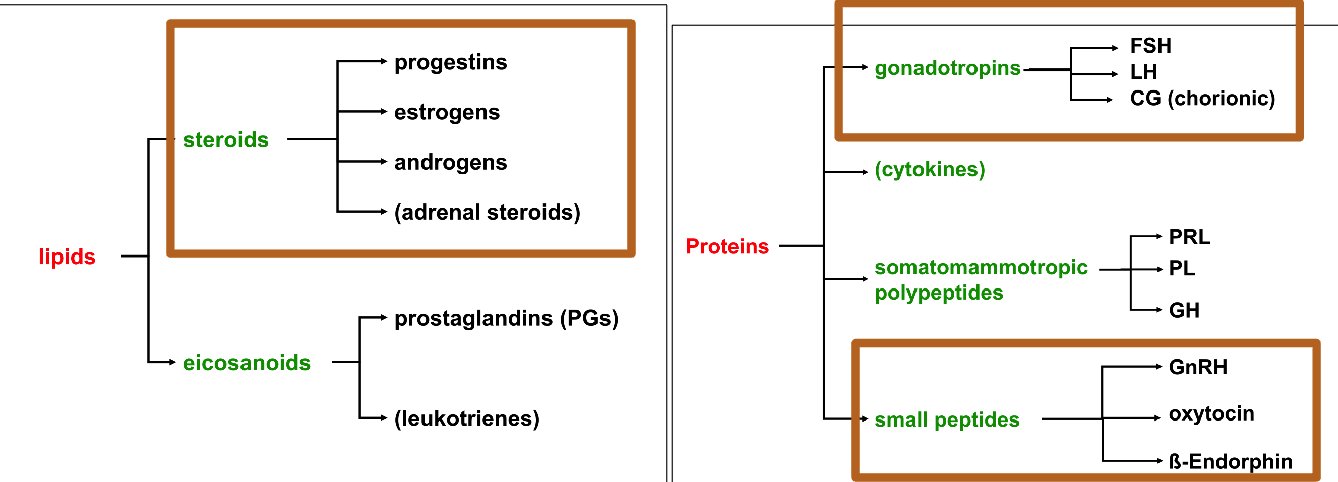
types of lipids
There are steroids and eicosanoids
Steroids = Progestins, Estrogens, Androgens, Adrenal Steroids
Eicosanoids = Prostaglandins (PGs) and Leukotrienes
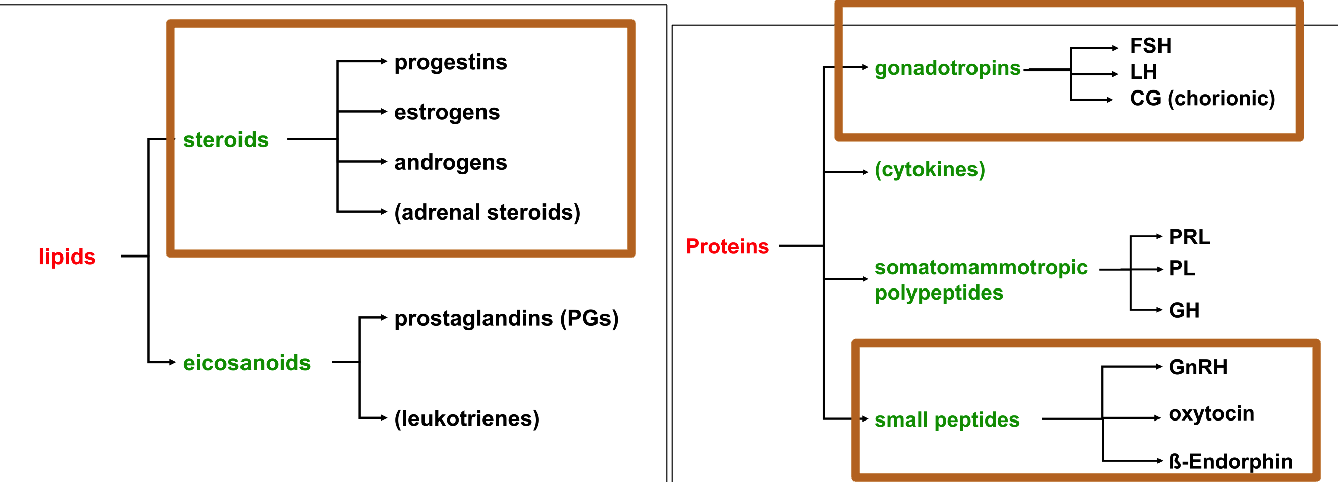
Types of Proteins
Gonadotropins = FSH, LH, CG(chorionic)
Cytokines
Somatomammotropic Polypeptides = PRL, PL, GH
Small peptides = GnRH, oxycotin, B-Endorphin
Steroids = Progestins, Estrogens, Androgens, Adrenal Steroids
Steroids refer to a class of organic compounds that include progestins, estrogens, androgens, and adrenal steroids.
Progestins are synthetic hormones used in birth control pills and hormone replacement therapy.
Estrogens are primarily female sex hormones responsible for the development and regulation of the female reproductive system.
Androgens are male sex hormones, such as testosterone, which are responsible for the development and maintenance of male characteristics.
Adrenal steroids are produced by the adrenal glands and play a role in various physiological processes.
Steroid (Progestins)
Progestins are synthetic hormones used in birth control pills and hormone replacement therapy.
Steroid (estrogen)
Estrogens are primarily female sex hormones responsible for the development and regulation of the female reproductive system.
Steroid (Androgen)
Androgens are male sex hormones, such as testosterone, which are responsible for the development and maintenance of male characteristics.
Steroid (Adernal)
Adrenal steroids are produced by the adrenal glands and play a role in various physiological processes.
Protein (Gonadotropins = FSH, LH, CG(chorionic))
Proteins are macromolecules composed of amino acids. Gonadotropins, including follicle-stimulating hormone (FSH), luteinizing hormone (LH), and chorionic gonadotropin (CG), are protein hormones involved in reproductive processes.
FSH stimulates the growth of ovarian follicles in females and spermatogenesis in males.
LH triggers ovulation and the production of testosterone in males.
CG supports pregnancy by maintaining the corpus luteum.
Protein (Cytokines)
Proteins are large biomolecules composed of amino acids.
Cytokines are a type of protein that act as signaling molecules in the immune system.
They regulate various immune responses, including inflammation and cell communication.
Cytokines play a crucial role in coordinating the body's defense against infections and diseases.
Protein - Somatomammotropic Polypeptides - (PRL, PL, GH)
Proteins, also known as somatomammotropic polypeptides (PRL, PL, GH), are large biomolecules composed of amino acids. They play a crucial role in various biological processes, including growth, repair, and maintenance of tissues. Proteins are involved in enzymatic reactions, transportation of molecules, immune response, and cell signaling. They are essential for the structure and function of cells, tissues, and organs in the human body. Examples of proteins include enzymes, antibodies, hormones, and structural proteins like collagen.
Protein - Small Peptides - (GnRH, oxycontin, β-endorphin)
Proteins are large molecules composed of amino acids, while small peptides are shorter chains of amino acids, typically consisting of fewer than 50 amino acids. Small peptides, such as GnRH, oxytocin, and β-endorphin, have specific functions in biological processes like cell signaling, enzyme activity, and immune response. They can be found in various sources, including food, plants, and animals, and are also utilized in research and pharmaceutical applications.
Oxytocin
Oxytocin is a hormone produced by the hypothalamus and released by the pituitary gland. It plays a crucial role in various physiological processes, including childbirth, breastfeeding, and social bonding. Oxytocin is often referred to as the "love hormone" due to its involvement in promoting feelings of trust, empathy, and attachment. It also has potential therapeutic applications in the treatment of certain psychiatric disorders.
Hormone Potencies
Different hormone forms have different potencies due to:
Interaction with different receptors
Conversion to alternative forms within tissues
Breakdown processes with the body
Alternate hormone forms can be precursors for other hormones
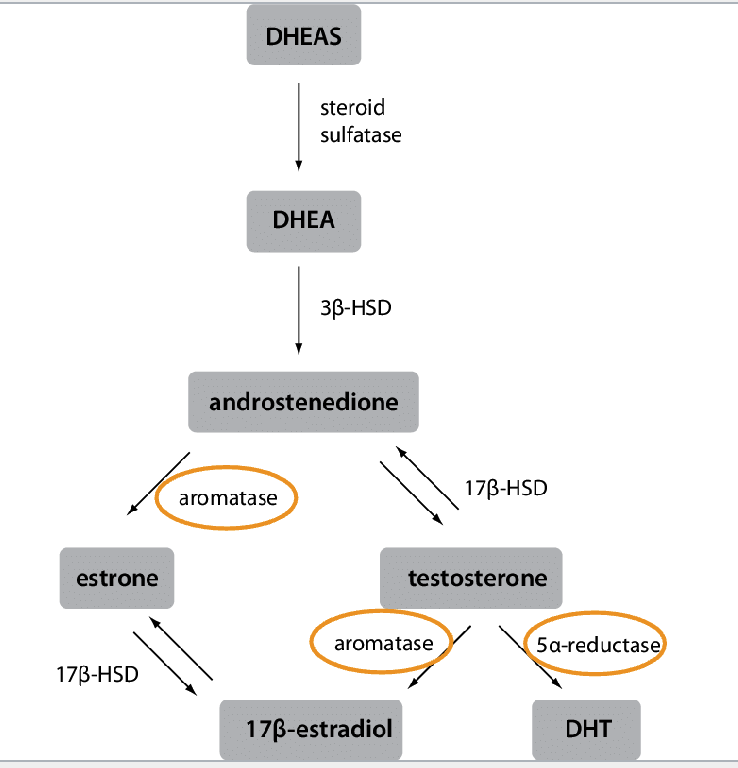
(e.g., cholesterol → steroids;androgens → estrogens)
Estrogen
Induces development of secondary sex characteristics
Cyclic changes in reproductive physiology (womens period/ovary realease
Androgen
Induces development of secondary sex characteristics
Stimulates activity of sex glands (e.g., prostate) sperm
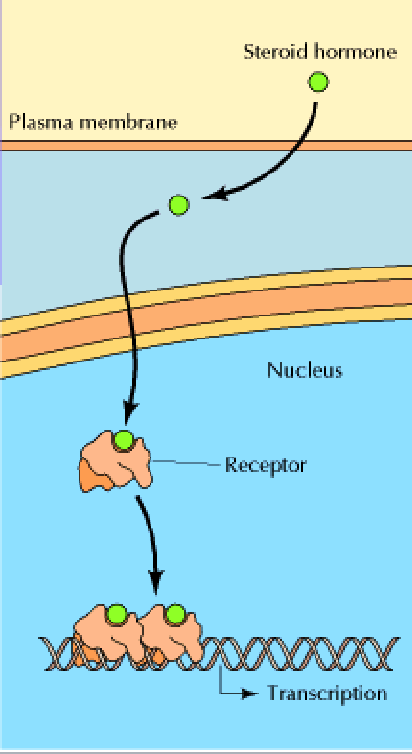
Lock and Key model – receptor and ligand
The lock and key model is a concept in biochemistry that describes the interaction between a receptor and a ligand. In this model, the receptor is like a lock and the ligand is like a key. The receptor has a specific shape that only allows a ligand with a complementary shape to bind to it. This binding is highly specific and plays a crucial role in various biological processes such as signal transduction and enzyme-substrate interactions.
Receptor specificity: distinguishing between specific hormones
Receptor specificity refers to the ability of a receptor to selectively bind to a specific hormone or ligand. Receptors are proteins located on the surface or inside cells that recognize and bind to specific molecules, such as hormones, neurotransmitters, or drugs. Each receptor has a unique structure that allows it to interact with specific ligands and initiate a cellular response.
The specificity of a receptor is determined by the shape and chemical properties of its binding site. Hormones have specific molecular structures that fit into complementary binding sites on their target receptors. This lock-and-key mechanism ensures that only the appropriate hormone can bind to its specific receptor, leading to a specific biological response.
Different hormones have different receptor specificities, allowing for precise regulation of physiological processes. For example, the hormone insulin binds to insulin receptors, while the hormone cortisol binds to cortisol receptors. This specificity ensures that each hormone can exert its effects on the appropriate target tissues and organs.
In summary, receptor specificity is crucial for distinguishing between specific hormones, as it allows for selective binding and activation of specific cellular responses.
- Receptor “promiscuity”: (specific to some hormones vs being able to bind easier) hormones binding to the same receptors
Receptor "promiscuity" refers to the ability of certain receptors to bind to multiple hormones. Some receptors are specific to certain hormones, while others have a broader binding capability, allowing them to bind to multiple hormones.
agonist
Mimics the action of the ligand. Binds and activates a receptor
An agonist is a substance that activates or stimulates a receptor in the body, producing a specific biological response. It can be a drug or a natural compound that mimics the action of a particular neurotransmitter or hormone. Agonists can have various effects depending on the receptor they target, such as promoting muscle contraction, increasing heart rate, or enhancing the release of certain chemicals in the brain.
Antagonist
Decreases or reverses the action of the ligand. Binds and deactivates a receptor.
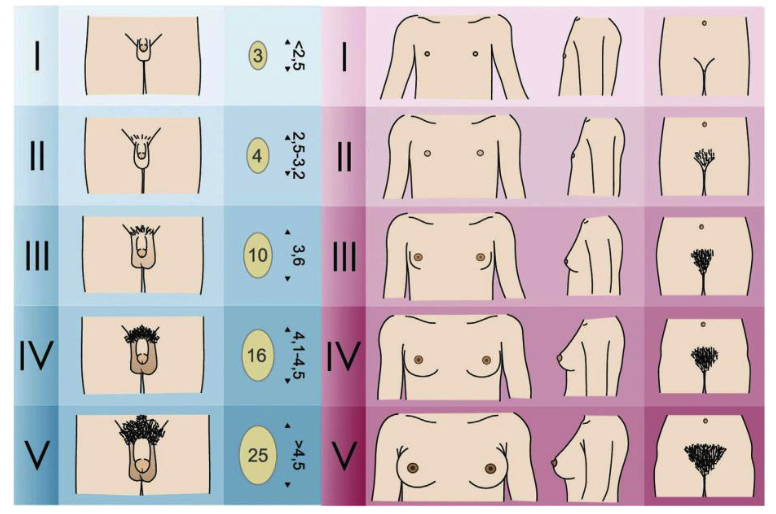
Tanner Staging
Tanner staging is a system used to assess the development of secondary sexual characteristics during puberty. It is commonly used to track the physical changes that occur in both boys and girls. The staging is based on the development of the breasts, genitals, and pubic hair in girls, and the genitals, pubic hair, and growth of the testes in boys. The Tanner staging system ranges from stage 1 (prepubertal) to stage 5 (adult-like development). It helps healthcare professionals monitor and evaluate the progression of puberty in individuals.
The timing of puberty
Influenced by genetic and environmental factors
Genetics, stress, in utero nutrition, infection, racial and ethnic group, weight-height ratio
Estimated that when puberty occurs in 58% genetically occurring
Hitting puberty closer to when family members have
Pubital Onset - Most girls hit puberty before boys
Pubital onset refers to the beginning of puberty, which is the period of sexual maturation and physical changes that occur during adolescence. It is characterized by the development of secondary sexual characteristics such as breast development in girls and testicular enlargement in boys. The timing of pubertal onset can vary among individuals, but it typically occurs between the ages of 8 and 14 in girls and between the ages of 9 and 14 in boys.
Average age of puberty
Age of puberty in girls has decreased over the last 150 years.
Increased obesity
decreased childhood stress (malnutrition, disease, in utero stress)
exposure to chemicals
Hormone action: DHEA/DHEAS
Female: Breast Development, Hair Growth
Male: Breast Development, Hair Growth
DHEA (Dehydroepiandrosterone) and DHEAS (Dehydroepiandrosterone sulfate) are hormones produced by the adrenal glands. DHEA is a precursor to other hormones, including testosterone and estrogen, and plays a role in various physiological processes. DHEAS is the sulfated form of DHEA and is the most abundant steroid hormone in the body. Both hormones have been studied for their potential effects on aging, cognition, mood, and overall health. However, the exact mechanisms of their action and their full range of effects are still not fully understood.
Hormone action: Testosterone
Female: Axillary & Pubic Hair
Male: Axillary & Pubic Hair
Testosterone is a hormone that plays a crucial role in the development and maintenance of male reproductive tissues and secondary sexual characteristics. It is produced primarily in the testes in males and in smaller amounts in the ovaries and adrenal glands in females. Testosterone acts by binding to androgen receptors in target cells, where it regulates gene expression and influences various physiological processes such as sperm production, muscle growth, bone density, and the development of male sexual characteristics.
Hormone action: Androstenedione
Female: Body Odours, Oils, Acne
Male: Facial Hair, Deep Voice, Body Odour, Oils, Acne
Androstenedione is a hormone that is produced in the adrenal glands and the ovaries. It is a precursor to both testosterone and estrogen. In the body, it can be converted into testosterone or estrogen depending on the needs of the individual. Androstenedione has been used as a supplement by athletes to enhance performance, but its use has been banned by many sports organizations due to its potential for abuse.
Hormone action: Estrone
Female: Breast Development
Male: Breast Development
Estrone is a hormone that belongs to the group of estrogens. It is primarily produced in the ovaries and adrenal glands. Estrone plays a role in various physiological processes, including the development and maintenance of female reproductive tissues, regulation of the menstrual cycle, and bone health. It acts by binding to estrogen receptors in target cells, thereby initiating specific cellular responses.
Hormone action: Estradiol
Female: Growth Spurt, Menarche, Breast Developement
Male: Growth Spurt
Estradiol is a hormone that belongs to the group of estrogen hormones. It plays a crucial role in the development and regulation of the female reproductive system. Estradiol is responsible for the development of secondary sexual characteristics in females, such as breast development and the growth of pubic and underarm hair. It also plays a role in the menstrual cycle and is involved in the maintenance of bone health. Additionally, estradiol has effects on various other tissues in the body, including the brain, cardiovascular system, and skin.
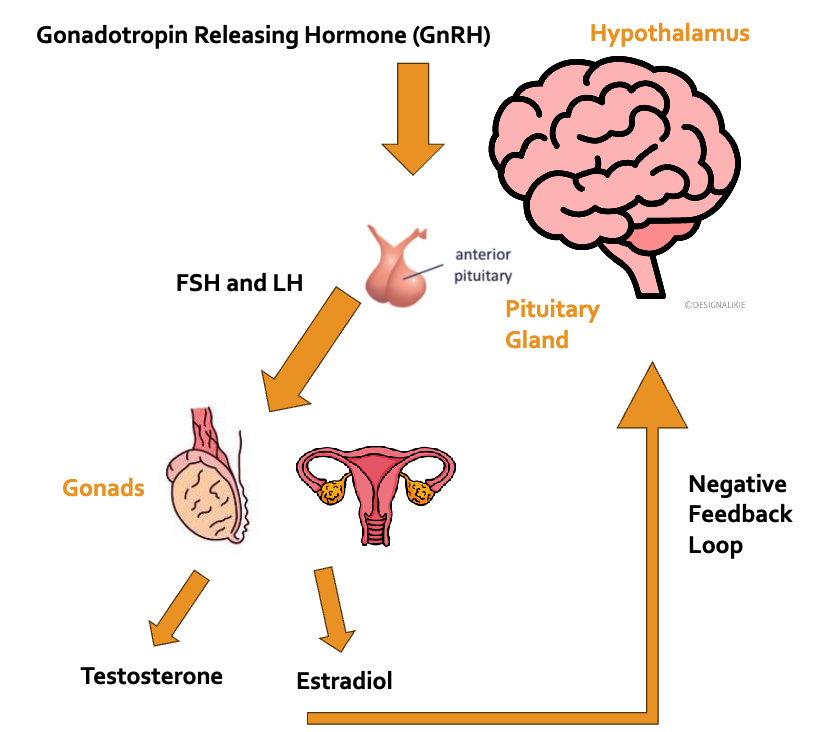
General Hormone Axis
Hormones bind to receptors - binding causes other things to happen
FSH = Follicle stimulating hormone
In women, FSH helps control the menstrual cycle and stimulates the growth of eggs in the ovaries.
FSH, or follicle-stimulating hormone, is a hormone produced by the pituitary gland. It plays a crucial role in the reproductive system, particularly in the regulation of the menstrual cycle and the development of eggs in females and sperm in males. FSH stimulates the growth and maturation of ovarian follicles in females, leading to the release of an egg during ovulation. In males, FSH stimulates the production of sperm in the testes.
LH - Luteinizing hormone (LH)
Glycoprotein hormone that is co-secreted along with follicle-stimulating hormone by the gonadotrophin cells in the adenohypophysis (anterior pituitary).
Luteinizing hormone (LH) is a hormone produced and released by the pituitary gland. It plays a crucial role in the reproductive system, particularly in the regulation of the menstrual cycle and ovulation in females, and the production of testosterone in males. LH stimulates the release of an egg from the ovary during ovulation and promotes the production of progesterone. In males, LH stimulates the production of testosterone by the testes. Abnormal levels of LH can indicate various reproductive disorders.
GNRH
Activated by absence of or low rates of testosterone and estrodiol
Gonadotropin-releasing hormone (GnRH) is a hormone that regulates the release of other hormones involved in reproductive functions. It is produced in the hypothalamus and stimulates the release of luteinizing hormone (LH) and follicle-stimulating hormone (FSH) from the pituitary gland. GnRH plays a crucial role in the menstrual cycle, fertility, and the production of sex hormones.
Ovarian steroid production
Pre-Puberty:
Production of estradiol by ovary very low
Able to get Adreogens from adrinal gland
Post-Puberty:
Gonadotropin levels rise (LH) (i.e., hormones that stimulate the gonads)
Greater amounts of steroid hormones produced from ovaries
Menstrual Phases
The menstrual cycle consists of four phases
the menstrual phase
the follicular phase
the ovulation phase
the luteal phase.
During the menstrual phase, the lining of the uterus is shed, resulting in menstrual bleeding. This phase typically lasts for 3-7 days.
the menstrual phase
The menstrual phase is the first phase of the menstrual cycle in females. It is characterized by the shedding of the uterine lining, resulting in vaginal bleeding. This phase typically lasts for about 3-7 days. The hormonal changes during this phase are marked by a decrease in estrogen and progesterone levels. The purpose of the menstrual phase is to prepare the uterus for a new cycle of ovulation and potential pregnancy.
the follicular phase
The follicular phase is the second phase of the menstrual cycle. It begins on the second day of menstruation and lasts until ovulation. During this phase, follicles in the ovaries start to develop and mature under the influence of follicle-stimulating hormone (FSH) released by the pituitary gland. These follicles produce estrogen, which stimulates the thickening of the uterine lining. As the follicles mature, one dominant follicle emerges and releases a mature egg during ovulation, marking the end of the follicular phase.
the ovulation phase
The ovulation phase is a stage in the menstrual cycle where a mature egg is released from the ovary. It typically occurs around day 14 of a 28-day cycle. During this phase, the hormone levels of estrogen and luteinizing hormone (LH) increase, triggering the release of the egg. Ovulation is a crucial step in fertility and conception.
the luteal phase
The luteal phase is the second half of the menstrual cycle in females. It occurs after ovulation and is characterized by the development of the corpus luteum, which produces progesterone. This phase prepares the uterus for potential implantation of a fertilized egg and lasts for about 10-16 days. If pregnancy does not occur, the corpus luteum degenerates, leading to the shedding of the uterine lining during menstruation.
High levels of progesterone
High levels of progesterone in the body are typically associated with pregnancy. Progesterone plays a crucial role in maintaining pregnancy by preparing the uterus for implantation and supporting the development of the placenta. It also helps regulate the menstrual cycle and prepares the breasts for milk production. However, high levels of progesterone outside of pregnancy may indicate certain medical conditions such as ovarian cysts or hormone imbalances. It is important to consult with a healthcare professional for a proper diagnosis and treatment.
Puberty
Puberty is the stage of development when a child's body undergoes physical changes, leading to sexual maturity. It is typically characterized by the development of secondary sexual characteristics, such as breast development in females and facial hair growth in males. Hormones, such as estrogen and testosterone, play a crucial role in initiating and regulating these changes. Puberty usually begins around the ages of 8 to 14 in girls and 9 to 16 in boys. It is a natural and important part of human growth and development.
Exogenous
Exogenous refers to something that originates from outside the body or system. It can refer to substances or factors that are introduced into the body from an external source. This is a hormone therapy you'd take
Exocrine
Exocrine glands are glands that secrete their products into ducts, which then carry the secretions to specific locations in the body. These glands are found in various organs such as the salivary glands, sweat glands, and pancreas. They play a crucial role in the body's digestive and excretory systems by producing substances like saliva, sweat, and digestive enzymes. This means the body produces hormone and leaves body for someone else (dogs)
100% potency
100% potency means little cause lot of effects
Precocious Puberty (CPP)
Precocious puberty (CPP) refers to the early onset of puberty, typically before the age of 8 in girls and 9 in boys (development of secondary sex characteristics before 8 or 9 years old). It is characterized by the development of secondary sexual characteristics, such as breast development in girls and testicular enlargement in boys, along with the onset of menstruation in girls. CPP is often caused by the premature activation of the hypothalamic-pituitary-gonadal axis, which leads to the production of sex hormones like estrogen and testosterone. Treatment options for CPP may include medication to delay puberty and address underlying causes.
Results in:
Short height – bone maturity too early
Social and emotional concerns
Metabolic disorders, insulin resistance
Treated with gonadotropin-releasing hormone agonist (GnRHa), a.k.a., puberty suppression
Gynecomastia
Overdevelopment of breast tissue in boys and men
Common in infancy, adolescence, and in middle-aged to older men.
Gynecomastia is a condition characterized by the enlargement of breast tissue in males. It is caused by an imbalance of hormones, specifically an increase in estrogen or a decrease in testosterone. Gynecomastia can occur at any age and may be temporary or persistent. Treatment options include medication, surgery, or addressing the underlying cause.
Disorder of sex development (DSD)
Disorder of sex development (DSD) refers to a group of medical conditions that affect the development of the reproductive or sexual anatomy. It occurs when there is a discrepancy between the chromosomal, gonadal, or anatomical sex of an individual. DSD can manifest in various ways, such as ambiguous genitalia, atypical chromosomal patterns, or differences in hormone production. The specific causes and variations of DSD are diverse, and diagnosis and treatment often involve a multidisciplinary approach involving medical professionals specializing in endocrinology, genetics, and urology.
DSD and intersex are often used interchangeably.
Intersex
Intersex is a term used to describe individuals who are born with reproductive or sexual anatomy that does not fit typical definitions of male or female. It is a natural variation of human biology and can manifest in various ways. Intersex individuals may have a combination of male and female characteristics, ambiguous genitalia, or chromosomal variations. The exact causes of intersex variations are not fully understood, but they are not considered to be abnormalities or disorders. It is important to respect and support the rights and identities of intersex individuals.
Considered potentially pejorative, stigmatizing, emphasizing binary biology.
DSD and intersex are often used interchangeably.
hermaphrodite
This is an unaccepted term; has been abandoned for decades.
D’Oro et al. (2020)
133 participants: clinic clients and their caregivers
Most liked terms were “variation of sex development” (37%) and “disorders of sex development (27%).
No term was liked by a majority of participants
“Disorders of sex development” (37%) and “intersex“ (53%) were most frequently viewed unfavourably
What is a DSD?
Umbrella term to describe groups of people that have genital conditions that
“A heterogenous group of congenital conditions that result in discordance between an individual’s sex chromosomes, gonads, and/or anatomic sex.”
Genetic and/or hormonal disorders that lead to differentiated development.
Gender dysphoria
Gender dysphoria is a condition where an individual experiences distress or discomfort due to a mismatch between their gender identity and their assigned sex at birth. It is recognized as a medical diagnosis and is often treated through various forms of gender-affirming care, such as hormone therapy or gender reassignment surgery. It is important to provide support and understanding to individuals experiencing gender dysphoria.
Sex Chromosome Aneuploidy (SCA)
Sex Chromosome Aneuploidy (SCA) refers to a condition where there is an abnormal number of sex chromosomes in an individual's cells. This can occur due to errors in chromosome segregation during meiosis or fertilization.
Examples of SCA include:
Turner syndrome (45,X)
Klinefelter syndrome (47,XXY)
Triple X syndrome (47,XXX)
These conditions can lead to various physical and developmental differences, including infertility, hormonal imbalances, and cognitive impairments. Treatment and management options for SCA depend on the specific condition and its associated symptoms.
Aneuploidy
Any Genetic disorder with more or less than 46 chromosomes
Isn't specific to sex development (SCA is specific to sex development)
Down syndrome
Aneuploidy refers to an abnormal number of chromosomes in a cell. It occurs when there is a gain or loss of one or more chromosomes, resulting in an imbalance of genetic material. A common example of aneuploidy is Down syndrome, which is caused by an extra copy of chromosome 21. Aneuploidy can lead to various genetic disorders and developmental abnormalities.
Trisomy
47 chromosomes (one pair has three chromosomes)
Trisomy 21 refers to an extra chromosome at the 21st location (i.e., down syndrome)
Trisomy is a genetic disorder where an individual has an extra copy of a chromosome in their cells. It can result in various health conditions, depending on which chromosome is affected. The most well-known trisomy is Trisomy 21, also known as Down syndrome, where there is an extra copy of chromosome 21. Trisomy can occur due to errors in cell division during the formation of eggs or sperm, or during early embryonic development. It is typically diagnosed through genetic testing.
Monosomy
45 chromosomes (one pair has a single chromosome)
One less chromosone
Monosomy is a genetic condition where an individual has only one copy of a particular chromosome instead of the usual two copies. It can result in various health issues depending on which chromosome is affected. Some examples include Turner syndrome (monosomy X) and Cri du Chat syndrome (monosomy 5p).