Health Promotion Through Education
1/39
Earn XP
Description and Tags
Ch. 11
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
40 Terms
Healthy People 2030 & Key Concepts r/t Health Promotion
SDOH
Socioeconomic gradient in health
“What is the social status of people based on how they are doing economically?”
Health disparities
Access to care
Quality of care
Healthy People 2030
Was developed by the office of disease prevention and health promotion.
The vision of this is for “a society in which all people can achieve their full potential for health and well-being.”
It’s framework consists of a vision and mission with foundational principles that guide the overarching goals and objectives for the plan of action.
Attaining the full potential for health and well-being, being through the creation of social, physical, and economic environment is one of the five overarching goals of this.
These objectives, when viewed in the broader context, can be used to identify client needs and align educational efforts that will advance this national initiative.
Social Determinants of Health (SDOH)
“The conditions in which people are born, grow, live, work and age and the wider set of forces and systems shaping the conditions of daily life.” World Health Organization
These are non-medical conditions—influences human beings across the lifespan and from their home to work and every place in between.
According to the CDC impacts on SDOH include:
Economic policy and systems
Societal norms and social policy
Developmental agenda
Politics
Racism
Climate control
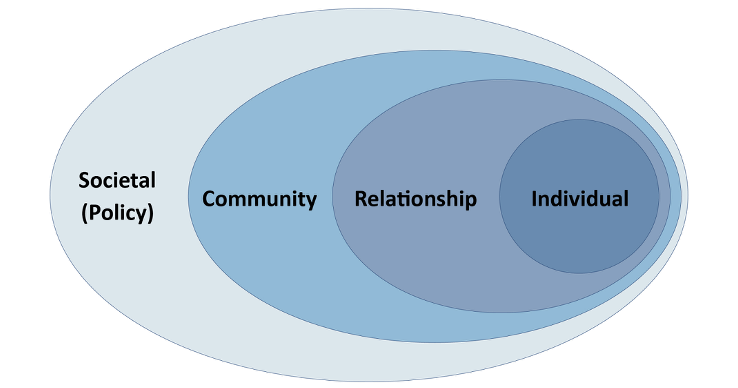
5 Domains Associated with SDOH
Economic stability
Access to quality education
Access to quality healthcare
Neighborhood and built environments
Social and community context
The unequal distribution of these factors among certain groups contributes to health disparities that are persistent and pervasive.
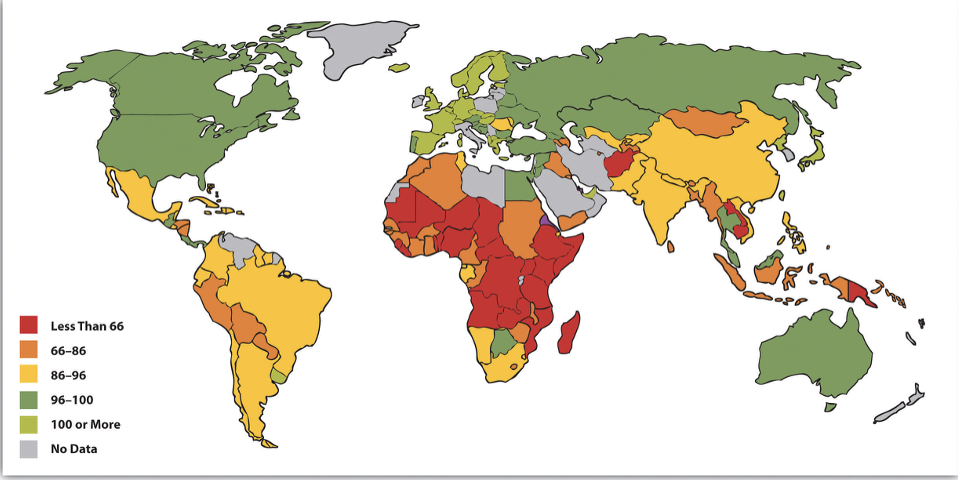
The United States experienced a severe reduction in US life expectancy between 2019 and 2021.
This was due to the medical conditions surrounding Covid, however, SDOH can also be attributed to the decline as seen with high uninsured rates in populations, such as American Indian, Alaska Natives, Hispanic, Native Hawaiian, Pacific Islanders, and the Black population.
Health Disparities
Preventable differences among population in the quantity and burden of disease, age and rate of morbidity.
*** occurs when a population does not receive education or counseling***
Populations of people who have experienced more systematic obstacles that are related to:
Race
Religion
Socioeconomic status
Gender
Age
Mental
Cognitive, sensory, physical disabilities
Sexual orientation
Geographic location
Health Disparities exist in…
Areas of quality of healthcare, access to care, levels of care and types of care, along with care settings.
Sub populations are also affected such as the aging, females, children, rural populations, and patients with disabilities.
Examples of disparities include poor access to quality care.
Discrimination, for example, the provider is biased against certain groups, holds stereotypical beliefs about a group or may not be confident in their treatment of racial or ethnic groups.
Language barriers exist leading to miscommunication.
Providers may be unfamiliar with cultures and norms of populations.
The patient does not trust the caregiver and therefore will not follow their information.
Health Disparities: Access to Healthcare
Inadequate or no health insurance
Problems getting healthcare
Quality of care
Fewer choices on where to go for care
Lack of regular providers
Fewer substance use disorder, treatment centers
Rural areas are especially affected when it comes to quality of care, fewer choices on where to go for care, and lack of regular providers.
People don’t want to live in rural areas as often therefore decreasing the likelihood of possible quality.
Doctors or the providers leaving the area, therefore causing a decrease in the consistency in care.
Quality of Healthcare
Quality of healthcare is essential for positive outcomes
Quality healthcare must be:
Safe
Timely
Effective
Equitable
People centered
Integrated throughout a lifespan
Accessible
Underrepresented groups have more barriers.
Not as many doctors of the same ethnicity.
Under or no insurance, not as many healthcare providers in rural areas, staffing, shortages, transportation issues, lead to people missing work, which causes a decrease in participation in care, leading to people postponing care.
Some solutions to these problems have been TeleMed, virtual visits, after hour services, and remote patient monitoring.

Health Literacy
Pertains to the information and services that people need to make informed decisions.
This includes:
The ability to read
The ability to calculate correct dosages and times to take prescribed medications
The ability to understand medical jargon
Personal health literacy—the ability to locate, understand and use healthcare information to make informed decisions.
Examples include healthcare forms, health promotion instructions, and the complex healthcare system overall.
Organization health literacy—providing people with equitable health information and services that are easy to find, understand, and use for making healthcare decisions for themselves or others.
Examples include easy to use appointment systems, ensuring patient health, education comprehension through the use of teach back method and providing communication using appropriate format, language, and reading level.
Digital health literacy—patient access to their EHR, apps for wellness, communication for scheduling and Bill Pay.
Health Promotion
Health behaviors that improve well-being and lead to a desire to meet one’s human potential.
Example:
When the community public health nurse plans an educational program for community dwelling older adults to learn about the need for a balance diet, rich in fruits and vegetables.
There is no clear disease or condition at issue, thus it remains at the primary level of prevention.
As the nurse continues to work with these people, the nurse learns that several clients have had recent falls.
The nurse begins to discuss foods that will help reduce bone loss and promote healthy bone growth, adequate vitamin D, a safe home environment, and weight-bearing exercises.
This effort would still be primary prevention, but with the purpose of disease prevention or health protection.
Disease Prevention
Focused on specific efforts aimed at reducing the development and severity of chronic diseases and other morbidities.
Example:
As the nurse continues to work with these people (community dwelling older adults), the nurse learns that several clients have had recent falls.
The nurse begins to discuss foods that will help reduce bone loss and promote healthy bone growth, adequate vitamin D, a safe home environment, and weight-bearing exercises.
This effort would still be primary prevention, but with the purpose of disease prevention or health protection.
health promotion; disease prevention
Both ______ _________ and _______ __________ operate at the primary level.
The Nature of Change
To be a C/PHN is to be a health educator with the goal of affecting in people’s behaviors.
Imperative for C/PHN’s to understand the nature of change, how people respond to it, and how to affect change for improved community health.
Change can be planned or unplanned.
Change can be by design or by default.
Change means things are out of balance.
Evolutionary Change is…
Gradual, overtime, incremental, modified and does not replace.
Example: Becoming parents, cutting back on smoking, losing weight by cutting back on desserts.
Revolutionary Change is…
Rapid, drastic, threatening, produces radical new behavior.
Example: Sudden unemployment, stoping smoking overnight, removing children from an abusive home.
There is no time to prepare high level of emotion, its demands are too great, it may lead to defense mechanisms, developing such as denial, resistance, or incapacitation.
What are the 3 stages of change?
Unfreezing
Changing
Refreezing
Stages of Change: Unfreezing
Desire for change develops, either intrinsically, or extrinsically. (initiating the change!)
A developing need for change causes disequilibrium in the system. The system is now more vulnerable.
People are now motivated to change.
Stages of Change: Changing
New ideas are accepted and tried out.
Occurs when people examine and try the innovation.
Example:
Participants in a prenatal class are learning exercises or when older clients in a center for older adults are discussing in trying ways to make their apartment safe from accidents.
During this stage people experience a series of attitude transformations, that range from early questioning of the innovations worth to full acceptance and commitment and then to accomplishing the change.
The change agents role during this moving stage is to help the client see the value of the change, encourage them to try it out, and assist them in adopting it.
Stages of Change: Refreezing
Change is integrated and stabilized in practice—Integrating or internalizing the change into the system and then maintaining it.
It occurs when changes are established as an accepted and permanent part of the system.
The rest of the system has adapted to it.
People no longer feel resistant to it because it is no longer viewed as disruptive, threatening, or new.
As the change is integrated, the system becomes refrozen and stabilized.
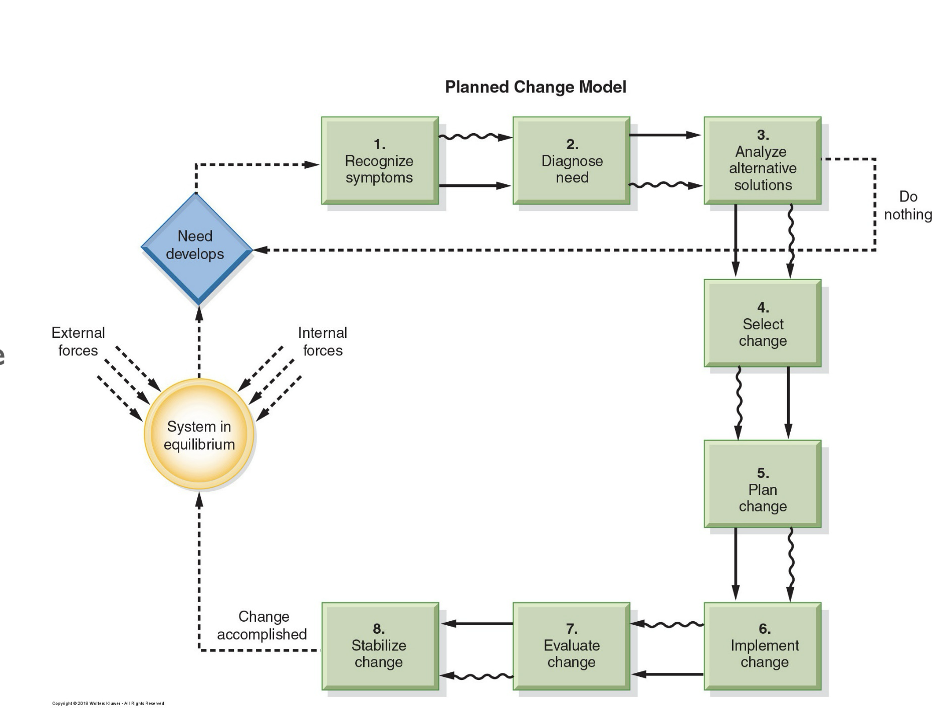
Planned Change
Plan is the purposeful, designed effort to affect improvement and involves a change agent.
The following characteristics of this type of change are the key to its success:
The change is purposeful and intentional.
There are specific reasons or goals prompting the change.
These goals give the change effort a unified focus, and a specific target unplanned changed, occurs, haphazardly, and its outcomes are unpredictable.
The change is by design, not by default.
Thorough systematic planning provide structure for the change process and a map to follow.
Planned change in community health aims to improve.
Seeks to better the current situation, to promote a higher level of efficiency, safety, or health enhancement.
Planned change is accomplished through an influencing agent.
Is a catalyst in developing and carrying out the design, often in a leadership role as an educator.
The Planned Change Process
Involves the systematic sequence of activities that follows the nursing process.
The eight basic steps lead to the successful management of change.
The community public health nurse uses the change process when managing change at an organization, population group, community, and larger aggregate levels.
For example, as a result of information gleaned from parents and other caregivers, the community public health nurse may suspect that there’s a widespread lack of confidence among young parents.
This hypothesis could be tested through a social media survey to determine parenting needs and the entire communities population of young parents.
If the symptoms are present, which is step one, the nurse will then collaborate with the health department personnel and analyze the symptoms to reach a diagnosis step two.
Approaches to meeting this need will be put into place such as a parenting center in the community, organizing churches or clubs to sponsor parents or working through the community college system to hold workshops on parenting classes.
This demonstrates step three.
The most feasible and useful alternatives could be selected step four and the parenting program for the community would be planned.
Step five implementation would begin step six the nurse with the parents and other professionals would then evaluate the outcome step seven and make the necessary adjustment step eight.
Evaluation of the Educational Process
Systematic and logical method for making decisions to improve the program.
Educator Evaluation:
Feedback to the educator provides an opportunity for the educator to modify the teaching process and enables the educator to better meet the learner’s needs.
Can we modify the process to better meet the learner’s outcome/objective?
Process Evaluation:
This examines the dynamic components of the educational program. It follows and assesses the movements and management of information transfer, and attempts to make sure that the objectives are being met.
Are goals and objectives being met?
How much time is required for each achievement?
Is the desired health behavior change really necessary? (enables rethinking the practicality and merit of each objective)
The Nature of Learning: What are the 3 Domains of Learning
Cognitive (thinking)
Affective (feeling)
Psychomotor (acting)
Each domain has behavioral components that form a hierarchy of steps, or levels.
Each level builds on the previous one
Motivating adult learners
Adults are Motivated to Learn When….
They think they need to know something.
The new information is compatible with their prior life experiences.
They value the person(s) providing the information.
They believe they can make any necessary changes that are implied by the new information.
Cognitive Domain
Includes memory, recognition, reasoning, understanding, application, and problem-solving.
Hierarchical classification of behaviors.
First step: assess cognitive abilities
Literacy and health literacy
(notes section…)
The cognitive domain consists of these components (Bloom et al, 1956):
Knowledge: this requires recall of information
Comprehension: which combines recall with understanding
Application: new information is taken in and used in a different way
Analysis: breaks down communication into parts to understand both the parts and their relationships to one another
Synthesis: builds on the first four levels by assembling them into a new whole
Evaluation: learners judge the value of what has been learned
Domains of Learning: Cognitive
Knowledge: recall basic facts.
Example: would be when a school nurse asks adolescents in a weight loss group to list food time fat…?
Comprehension: understanding.
Example: would be when the school nurse asks adolescents and a weight loss group to identify ways to lose weight.
Application: Transfer understanding into practice.
Example: when the school nurse ask the adolescents in the weight loss group to keep a food and physical activity record for a week, draw up a diet, and share this plan with the group at the next meeting.
Analysis: Break down concepts.
Example: would be when the school nurse ask the adolescents in the weight loss group to distinguish the fat content in a variety of package foods.
Synthesis: Summarize
Example: when the school nurse asked the adolescents in the weight loss group to select a menu that is low in fat.
Evaluation: Validate information.
Example: when the school nurse asks the adolescents in the weight loss group to develop a menu that is low in fat.
Affective Domain
Attitude changes and development of values.
Nurse’s attitudes and values may differ.
Difficult to change deeply rooted attitudes, beliefs, and values.
(note section…)
Affective learning, like cognitive learning, consists of a series of steps that the learner takes.
These steps are as follows:
Knowledge: receives the information
Comprehension: responds to the information received
Application: values the information
Analysis: makes sense of the information
Synthesis: organizes the information
Evaluation: adopts behaviors consistent with new values
Domain of Learning: Affective
The affective domain involves emotion, feeling, or affect.
The nurse tries to influence what a person values or feels.
Four Levels:
Learners are receptive and willing to listen.
They are simply receptive; they’re willing to listen, to show awareness, and to be attentive.
Learners become active participants.
They become active participants by responding to the information in some way.
Examples are a willingness to read educational material, to participate in discussions, to complete assignments, or to voluntarily seek out more information.
Learners attach value to the information.
They have attached value to the information.
Valuing ranges from simple acceptance through appreciation to commitment.
Learners internalize or value an idea.
They internalize an idea or value.
The value system now controls learner behavior.
Consistent practice is a crucial test at this level.
Psychomotor Domain
Neuromuscular coordination and motor skills.
First, demonstrate; then practice:
In a classroom environment, learner may benefit from observing one another.
3 Conditions:
Necessary ability
Sensory image
Opportunities to practice
(notes section…)
Psychomotor learning depends on learners meeting the following three conditions:
The learner must have the necessary ability. This will include both cognitive and psychomotor ability.
For example, you may find that a person with Alzheimer’s disease can follow only one-step instructions. Thus, you need to tailor your education plan to that person.
The learner must have a sensory image of how to carry out the skill.
For example, when teaching a group of women how to cook in a more heart-healthy manner, ask the women to describe their kitchen and how they would actually go about the cooking process.
The learner must have opportunities to practice the new skills. Provide practice sessions during the program to help the patient adapt the skill to his or her home or work environment where the skill will be performed.
Domain of Learning: Psychomotor
This domain includes visible, demonstrable performance skills that require some kind of neuromuscular condition.
For psychomotor learning, 3 conditions must be met:
Learner must be capable of the skill.
Learner must have a sensory image of how to perform the skill.
Learner must practice the skill.
(notes section…)
The client must be physically, intellectually and emotionally capable of performing the skill.
For example, an older or adult with diabetes, who has trembling hands and fading vision, may find it very difficult to give their own insulin injections. It could frustrate or harm them.
Clients intellectual and emotional capabilities also influence their capacity to learn motor skills. It may be inappropriate to expect people with a significant developmental delay to learn complex skills.
Developmental stage is another point to consider, and determining whether it is appropriate to teach a particular skill.
For example, most children can put on some article of clothing at two years of age, but are not ready to learn to fasten buttons until they are past their third birthday.
An adequate sensory image must be included in order to demonstrate and explain the task. And then this task must be practiced before the client can acquire a sensory image.
One good example is teaching CPR. With demonstration teach back and practice.
Learning Theories
Clients have different learning style preferences. These include visual, auditory, Reid/right, and kinesthetic.
A learning theory is a systematic and integrated look into the nature of the process, whereby people relate to their surroundings in such ways as to enhance their ability to use both themselves and their surroundings more effectively.
Each Nurse has and uses particular theory of learning, whether consciously or unconsciously, and that theory, intern, dictates the way, the C/PHN teaches clients.
Behavioral: focuses on behaviors that can be observed, measured and changed. (Pavlov, Skinner)
Health Belief Model/Pender’s Health Promotion Model
Cognitive: development that is orderly, sequential, and interactive. (Piaget)
Social: used to explain behaviors and facilitate learning. (Bandura)
Humanistic: a natural tendency to learn and the learning is flourished in an encouraging environment. (Maslow)
Adult Learning: is self-directed and includes a lifetime of experiences. It is a readiness to learn and the need to be able to apply knowledge.
Tertiary Prevention
Rehabilitation:
Restore functions; a nurse teaches a stroke survivor about home safety.
Health Promotion and Education:
Health teaching; a nurse teaches the stroke survivor about the importance of medication, diet, rest, and exercise.
Health Protection:
Maintenance; a nurse observes the stroke survivor’s medication regimen to ensure the client is taking medications properly.
Secondary Prevention
Early Diagnosis:
Screening and case finding: a nurse takes blood pressure measurements from all family members at each home visit and teaches them the importance of maintaining a healthy BP reading.
Prompt Treatment:
Treatment: a nurse teaches clients how to navigate through the complexities of the healthcare delivery system to receive prompt treatment,
Primary Prevention
Health Promotion:
Health education; a nurse teaches a class on sensible eight control for teenagers.
Health Protection:
Immunizations; a nurse teaches about the importance of pneumonia and flu vaccinations for older adults followed by an immunization clinic.
When planning educational interventions or public health programs, aligning activities with the appropriate level of prevention ensures resources are targeted effectively.
For example:
School-based health education → Primary prevention.
Cancer awareness and screening campaigns → Secondary prevention.
Chronic disease self-management workshops → Tertiary prevention.
If the C/PHN focuses on teaching at the primary level, it would help diminish years of morbidity and limit subsequent incapacity.
Education, Learning, and Change
Remember 3 things:
Easiest thing to change is knowledge.
Changing attitudes is the next step.
The Most difficult thing to change is behavior.
Difference between education and learning:
Education emphasizes the provider of knowledge and skills.
Learning emphasizes the recipient of knowledge and skills and the person(s) in which a change is expected to occur. Learning involves change.
(notes section…)
Education is an activity “undertaken or initiated by one or more agents that is designed to effect changes in the knowledge, skill, and attitudes of individuals, groups, or communities” (Knowles et al 2005, p 10). Education emphasizes the provider of knowledge and skills.
In contrast, learning emphasizes the recipient of knowledge and skills and the person(s) in whom a change is expected to occur. Learning involves change.
To change means to move away from one way of thinking, believing, and acting and move toward a new way.
Thomson’s (2010) steps to understanding and managing organizational change:
Identify the need for change, and this means the client or clients being served need to believe that they need to make a change.
Plan how to implement the change, and this step includes explaining the basis for the change, the benefits of the change and seeking ideas from those being served about the best way to make an identified change.
Implement the change.
Evaluate whether the change made a difference in health.
Fielding (2013) offers a similar approach toward health education consisting of the following five steps: (1) understanding the problem; (2) understanding what works; (3) agreeing on approach or action; (4) implementing plan; and (5) evaluating effect.
Teaching Process
The process of teaching in community health nursing follow steps similar to those of the nursing process:
Interaction, assessment and diagnosis, setting goals, objectives, planning, teaching, and evaluation.
Nursing Short-Term Goal:
Goal: Manage patient's acute pain effectively within 48 hours.
Objectives:
Assess patient's pain level using a standardized pain scale every 4 hours.
Administer prescribed pain medication as needed, monitoring for effectiveness and side effects.
Implement non-pharmacological pain relief methods such as relaxation techniques and positioning.
Educate the patient on pain management strategies and encourage reporting of pain promptly.
Reassess pain levels after interventions to ensure target pain level is maintained at 3/10 or lower.
Nursing Long-Term Goal:
Goal: Improve patient's ability to perform activities of daily living (ADLs) independently within 6 months.
Objectives:
Conduct a comprehensive assessment of the patient's current functional status.
Develop a personalized rehabilitation plan in collaboration with physical and occupational therapists.
Encourage participation in daily physical therapy sessions to enhance strength and mobility.
Educate the patient and family on adaptive equipment and techniques to support independence.
Evaluate progress monthly, adjusting the care plan as needed to achieve improved ADL performance.
These goals and objectives provide a clear roadmap for patient care, supporting measurable outcomes and continuous improvement.
Teaching Methods and Materials
Formal or informal, planned or unplanned
Methods
Lecture
Discussion
Demonstration
Role-playing
Materials (visual images, anatomic models, equipment, printed support materials)
Content, complexity, reading level, culturally appropriate
Teaching: Learning Prinicples
Client readiness
Client perceptions
Educational environment
Client participation
Subject relevance
Client satisfaction
Client application
(notes section…)
The goal of all teaching is learning.
Learning is a process of simulating new information that promotes a permanent change in behavior.
Learning is gaining knowledge, comprehension, or mastery.
Effective teaching takes place when the client is ready to learn.
Clients may not be ready to learn due to perceived fears of education, readiness, maturational levels.
Clients need to participate in the learning for teaching to be effective.
Learning is facilitated when the student is engaged and the student chooses their own direction.
Clients perceptions also affect their learning, serving as a screening device or filter through which all new information must pass.
Individual perceptions, help people interpret and attach meaning to things.
For example, in coronary disease; the person screens out the need to quit smoking and lose weight, paying attention only two factors that would not require a drastic change in lifestyle.
The educational environment is also important for effective teaching.
The setting in which teaching takes place can affect learning, for example, sitting in a cold room and trying to concentrate access noise ventilation lighting.
Subject, relevance, and client satisfaction also play an important role.
As well as client application learning; It is reinforced through application learners need as many opportunities as possible to apply the knowledge to their daily life.
SMART GOALS—Example:
Example of a Nursing SMART Goal:
Goal: Improve patient education on diabetes management to enhance patient outcomes.
Specific: Provide comprehensive diabetes management education to all newly diagnosed diabetic patients admitted to the unit.
Measurable: Achieve a 90% completion rate of diabetes education sessions for all newly diagnosed diabetic patients within three months.
Achievable: Utilize existing educational materials and collaborate with the diabetes education team to deliver consistent, high-quality sessions.
Relevant: Enhancing patient education aligns with the unit’s objective to improve patient self-care and reduce readmission rates related to diabetes complications.
Time-bound: Complete the goal within three months, with monthly evaluations to track progress and make necessary adjustments.
Refinements:"Reformat the SMART goal as a bullet-point list for clarity."
"Condense the goal into a brief paragraph highlighting key points."
"Emphasize the impact of the goal on patient care and outcomes.”
