Infection Control in Dental Hygiene: OSHA, PPE, Waterline Management, and Sterilization
1/70
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
71 Terms
OSHA
Occupational Safety and Health Administration
OSHA Standards
Protect the employee's right to a safe workplace through enforcement of standards that: 1. Reduce exposure to bloodborne pathogens. 2. Provide and maintain personal protection. 3. Guide the handling of items containing body fluids. 4. Guide the use and storage of drugs and chemicals (MSDS sheets).
Hazardous Waste Manual
MSDS data sheets - information on all chemical products used in the office or clinic.
MSDS Hazard Levels
0 = minimal hazard, 1 = slight hazard, 2 = moderate hazard, 3 = serious hazard, 4 = severe hazard.
Hazard Color Codes
Blue = Health hazard, Red = Fire hazard, Yellow = Reactivity hazard, White = Special hazard.
Standard Precautions
You must treat all patients as if they are infected with a contagious disease.
Five Steps to Reduce Infection Exposure Risks
1. Host Immunity and Immunization 2. Restriction of duties during illness 3. Patient health history 4. Extraoral / intraoral examination 5. Personal Hygiene and appearance.
Natural Immunity
An individual is exposed to a pathogen which stimulates the immune system to produce specific antibodies to the pathogen.
Artificial Active Immunity
Vaccinations or immunizations stimulate the immune system to produce specific antibodies without the individual having the disease.
Passive Immunity
Immunity develops in infants from antibodies from the mother. This type of immunity is temporary.
Restricting Duties During Illness
Healthcare workers should withdraw from direct patient contact and indirect-contact activities when exhibiting symptoms of infectious diseases.
Patient Health History
Tool to provide information that may point-out if modification to dental care procedures is necessary.
Extraoral / Intraoral Examination
A comprehensive patient examination often identifies lesions associated with systemic diseases.
Personal Hygiene and Appearance
Hair should be tied up and pulled back; personal jewelry may harbor high levels of bacteria.
Hand Care
Includes nails, broken skin, hand lotions, soap, and hand washing.
Personal Protection Equipment (PPE)
Purpose: Protect skin, eyes, nose, mucous membranes, and clothing from exposure to biohazardous materials in the workplace.
PPE Protection
Protect the clinician, not the patient, from biohazardous materials in the dental office.
Purpose of PPE's
Reduce direct contact - barrier for direct contact of infectious agents, saliva or blood. Minimizes indirect transmission - barriers for direct contact with contaminated object such as instruments, surface and equipment.
PPE Change Conditions
Must be changed if compromised: visibly soiled, wicked (moisture produced by operator), torn or visible holes.
PPE Examples
1. Gloves 2. Protective Eyewear 3. Face masks and Shields 4. Protective Garments.

Types of Gloves
Examination or procedure gloves, Surgical gloves, Utility gloves - used when handling sharp instruments. Always worn. New pair for each patient. Gloves should be removed before leaving the operatory. Change gloves often.
Glove Integrity Factors
Length of time worn, Complexity of procedure, Packaging of the gloves, Pressure of time, Storage of gloves, Agents used, Hazard from hands (long nails, rings, etc.).
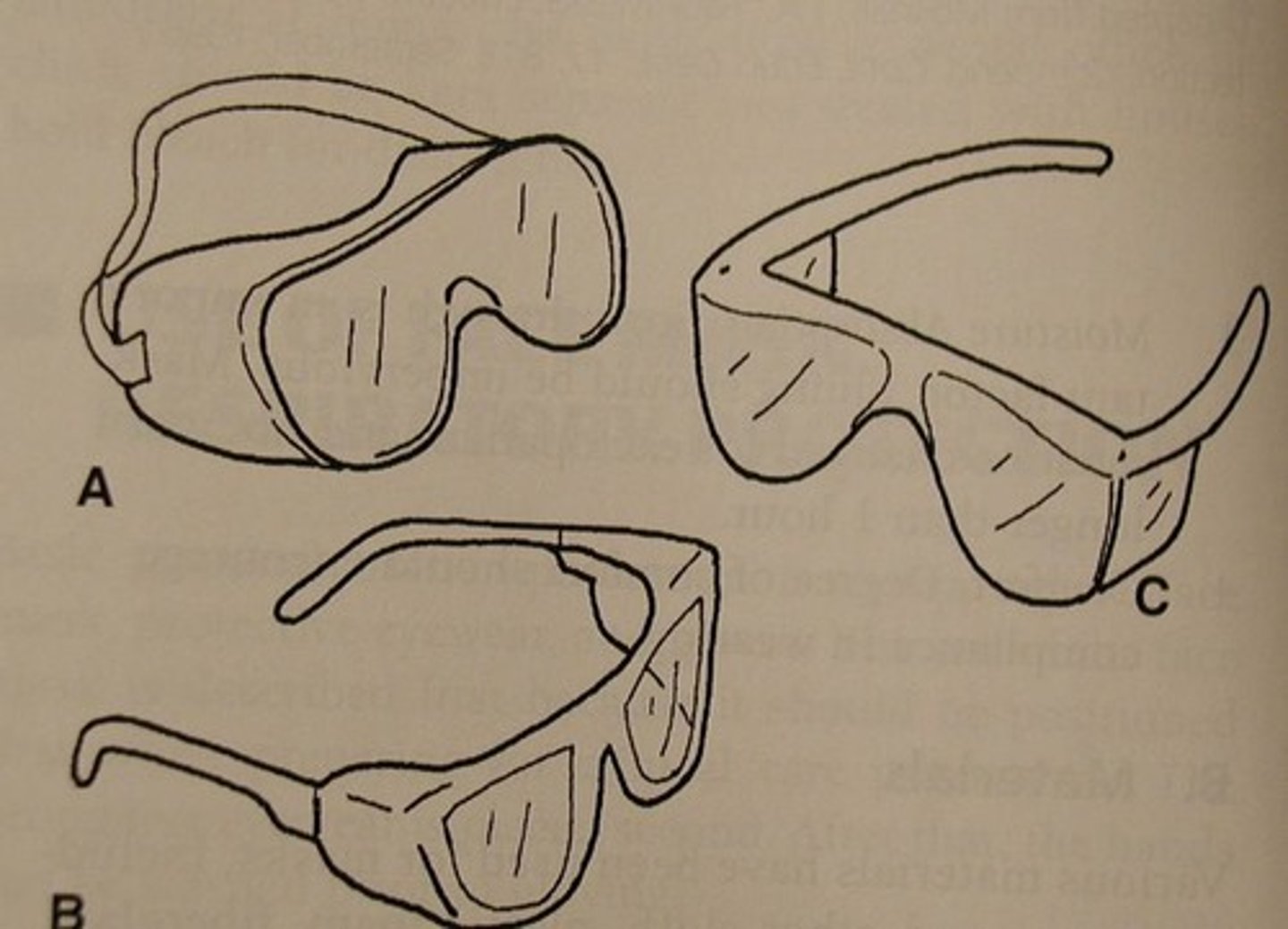
Protective Eyewear
ALWAYS wear protective eyewear (treatment and clean-up of the dental unit and instruments). Types: Safety glasses, face shields, loupes, patient protective eyewear.
Face Masks Usage
Worn for all procedures and clean-up of the dental unit and instruments. Mask must cover the nose, mouth and facial hair. The mask should fit snuggly with no gaps.

Face Mask Change Conditions
The mask MUST be changed for each patient OR if it becomes contaminated by touch, or visibly soiled or wet (wicked). Surgical masks should be changed every hour or more often if used in a moist/wet environment such as when using the ultrasonic scaler.
Face Mask Filtration Standards
The mask should have a 95% BFE with a 1 to 3 micron particle filtration level.
Protective Garments
Clinic attire protects the clinician's clothes and skin from contamination. Garments should cover lap area when sitting, cover arms, cuff on sleeves to seal the arms, pants cover ankles, and velcro or secured collar on coat.
PPE Placement (Donning)
Hand hygiene, Gown, Mask, Protective eyewear (safety glasses or loupes and face shield), Hand hygiene, Don gloves.
PPE Removal (Doffing)
Remove gloves, Remove Gown - turn inside out, Leave operatory and perform hand hygiene, Place new gloves and remove eyewear and disinfect. Remove mask, Remove gloves, Perform hand hygiene.
Implementation of Work Practice
Barrier protection, High-velocity evacuation, Reduction of microbial load, Disposable items, Chairside safety.
Dental Waterline Management
Biofilm: Colonies of cell growth that attach to the wet inner surfaces of small tubing. These microbes develop into a matrix which can get as thick as 400 micrometers (mu). Biofilm is 'slime' which enables microbes to grow and may serve as a reservoir for transmission of pathogens.
ADA Standard for Water
Water used during patient treatment should contain no more than 500 CFU/ml (colony-forming units) as what is found in normal, safe drinking water. Flush waterlines for 1-2 minutes prior to patient treatment. 20-30 seconds between patients.
Infection Control Procedures
General Environmental and Equipment Procedures including handwashing, Sterilization vs disinfection, College of Lake County Dental Hygiene Program Infection Control Procedures.
Principles of Handwashing
Reduce overall bacterial flora of the skin to a minimum. Handwashing will accomplish: 1. Surface dirt and bacteria removal. 2. Dissolve the normal greasy film found on the skin. 3. Rinse and remove loosened debris and microorganisms.
Handwashing Equipment/Supplies
Sink: foot pedal or electronic start for water-flow. If sink has hand controls: Turn on; leave on during procedure; turn off with a paper towel. Soap: Liquid surgical soap containing an antimicrobial agent (Povidone-iodine, iodophore, Chlorhexidine, etc). Paper towels.
Scrub brushes
Scrub brushes are to be used with caution as to not irritate the skin or cause abrasions.
Disposable sponges
Disposable sponges can also be used: Less irritating to the skin.
Towels
Towels: Disposable paper towels.
Handwashing Procedures
Handwashing is considered the most important single procedure for the prevention of cross-contamination.
Indications for Handwashing
Before placement and after glove removal. When hands appear visibly soiled or after contaminated surfaces were touched with a barehand.
Four Types of Handwashing Procedures
1. Antiseptic handwash 2. Routine handwash 3. Antiseptic hand rub 4. Surgical antisepsis (Surgical scrub)
Antiseptic Handwash - Preliminary Steps
Remove watch and jewelry. Fasten hair back. Don protective eyewear and mask. Use cool water. One lathering in three minutes is less effective than 3 short latherings in 30 seconds.
Antiseptic Handwash - Procedure
Lather hands, wrists, and forearms with liquid antimicrobial soap. Use pressure, interlace fingers, rub back and forth vigorously. Rinse thoroughly running the water down the hand to finger tips. Repeat two more times. Dry with disposable towel.
Routine Handwash
Wet hands, apply soap; avoid hot water. Rub hand together for at least 15 seconds; cover all surfaces of fingers, hands and wrists. Interlace fingers. Rinse under running water; dry thoroughly with disposable towel. Turn off faucet with towel. If bar soap was used; keep soap on soap rack where drainage and drying is possible.
Antiseptic Hand Rub
Decontaminate hands with a hand rub. Apply the product following manufacturer's recommendations. Cover all surfaces of the hands and rub together until dry. If dry in less than 10-15 seconds another application is needed.
Surgical Antisepsis - Preliminary Steps
Remove watch & Jewelry. Pull hair back. Don protective eyewear and mask. Open surgical brush or sponge.
Surgical Antisepsis - Procedure
Wash hands and arms with strong brushing motion (10 on each side). Rinse thoroughly from fingertips across hands and wrists. Hold hands higher than elbows throughout the procedure. Use orangewood stick to clean nails. Rinse.
General Environmental and Equipment Procedures
1. Work Zones 2. Daily Preparation 3. Surface Protection 4. Operatory Prep 5. Operatory Clean-up 6. End of Day Procedures
Work Zones
Define work areas. Floor plan should flow as to minimize cross contamination.
delete
(No definition provided in the notes)
Aseptic
A method to prevent contamination by pathogens.
Environmental Surface Protection
Measures taken to prevent contamination of surfaces in a treatment area.
Sanitization
Process by which a number of microorganisms is reduced to a relatively safe level.
Disinfection
Kills most microorganisms; hospital level disinfection agents must destroy specific pathogens.
Sterilization
Designed to kill ALL microorganisms including spores.
High Level Disinfection
Used in surgical areas; example includes 3% glutaraldehyde.
Intermediate Level Disinfection
Common in dental offices; kills Mycobacterium tuberculosis.
Low Level Disinfection
Unacceptable in the dental office; example includes simple phenol.
Steam Autoclave
Heats water in the chamber creating steam under pressure for sterilization.
Chemical Vapor Sterilization
Uses chemical vapor to destroy microbes with heat, pressure, and chemistry.
Dry Heat Sterilization
Relies on heat alone to oxidize cellular material or microbes.
Temperature for Steam Sterilization
250 degrees F for 20-30 minutes.
Temperature for Chemical Vapor Sterilization
270 degrees F for 20 minutes.
Temperature for Dry Heat Sterilization
320 degrees F for 60-120 minutes.
Geobacillus stearothermophilus
Spore test used for monitoring steam and chemical vapor sterilization.
Bacillus subtilis
Spore test used for monitoring dry heat sterilization.
Contaminated Barriers
Items that must be removed and disposed of at the end of the day.
Regulated Waste/Biohazard Waste
Waste saturated with blood and/or saliva or hard or soft tissue removed from the patient.
Sharps Containers
Containers designated for the disposal of sharp objects.
Non-regulated Waste
Items not saturated with blood; includes patient bibs, barriers, PPEs, and disposable items.
Quality of an Ideal Disinfection
Broad spectrum, fast acting, non-toxic, compatible with surfaces, easy to use, residual effect, odorless.