11 UT- Bladder and Urethra
1/44
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
45 Terms
• Cystotomy
incision into the bladder
• Cystectomy
excision of a portion of the bladder
eg neoplasia
• Cystostomy
hole into bladder allows for drainage while bypassing the urethra
Urethrotomy
creating a hole into the urethra
Urethrostomy
creating a new, permanent stoma into the urethra
above the point of obstruction
bladder surgery: clean or contaminated
Clean-contaminated surgery
Principles of bladder surgery 5
Empty bladder prior to surgery— catheterisaiton
Keep tissues moist, halsted
Bladder wall heals quickly
regains strength 14-21 days
Absorbable monofilament suture material with swaged-on needle
PDS polydioxanone
patterns: water tight seal, don’t go into lumen!!
suture-induced calculi mineral deposit
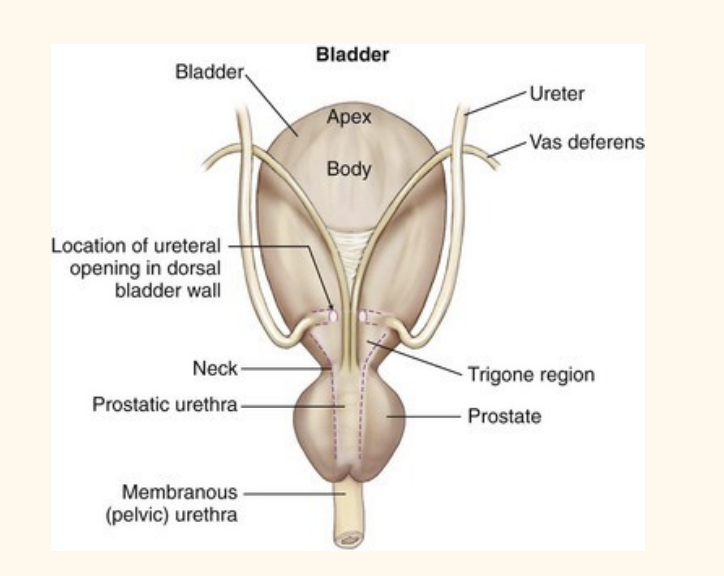
Surgical anatomy: bladder
ureter: 1 on each side
note hook on caudal ureter
enter trigone region of urinary bladder
M—> vas deference pass through bladder; prostate withinirethre wall
Cystotomy INdication 5
Remove bladder / urethral stones
Biopsy / resection masses
Repair of ectopic ureters (referral/ senior)
Biopsy / culture bladder wall severe cystitis
Repair bladder trauma
Cystotomy : day 1 competecy
prep 5
Ventral midline clip: exploratory coeliotomy
Include genitalia in field
allow catheterise intraop
Caudal approach or full ex-lap
more caudal: may want to flush urethra check patent
Bladder easily traumatised
Minimise handling
Atraumatic forceps— debakey
Stay sutures
Suction
Cystotomy site: ventral cystotomy
Used most common
Readily accessible
Visualise the trigone well on doral (opposite)
No increased risk of leakage
Cystotomy site: dorsal cystotomy
Potential damage to neurovascular bundle + ureter
Less easy to visualise
Ureters enter dorsally
—> don’t do it :(
Cystotomy steps ** organise diagram 13
Isolate bladder from abdomen
Place stay suture in apex —> atraumatic handling
pack around bladder to minimise spillage
Select cystotomy site— ventral
± cystocentesis (unless preop catheter)
Stab incision —avascular area
Extend with Metzenbaums —> longitudinal apex towards trigone
ectopic urether—> more causally
sphincter damage will heal with incontinence within. a few day
stay suture on either side of incision
perform necessary procedure
Remove clots before closure
Single-layer, appositional pattern – simple interupted/ continuous
watertight, do not go into lumen
Thickened wall – occasional two-layer closure
Leak test and omental wrap
leak test: inject sterile saline/ via catheter
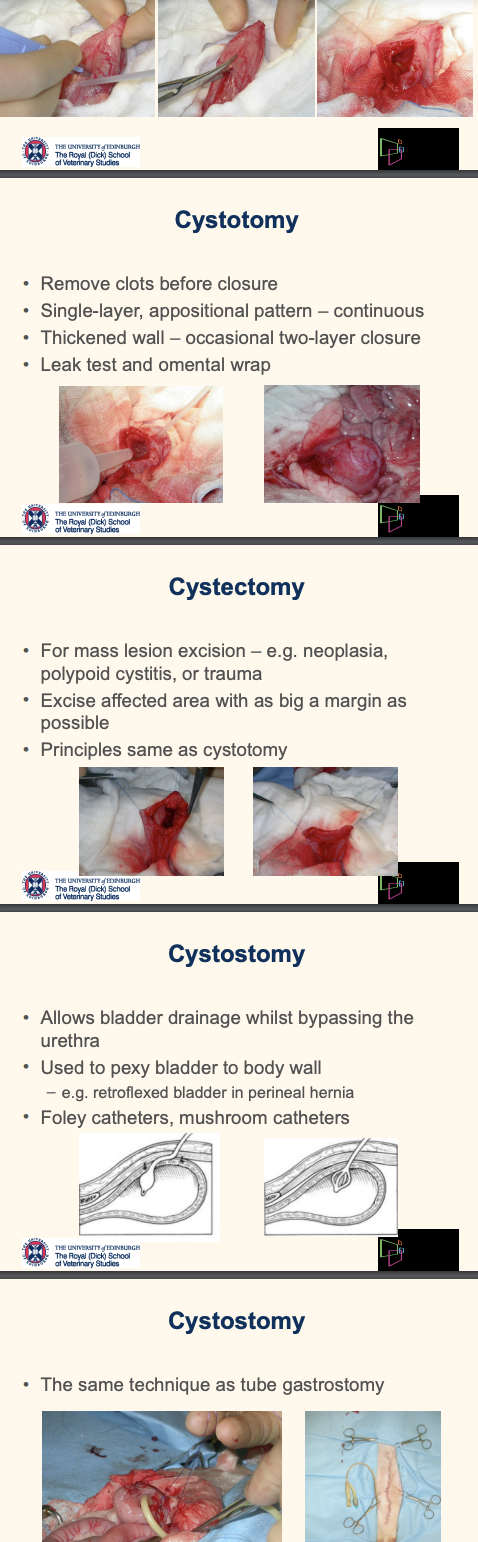
Cystectomy • For mass lesion excision
considerationa nd principle 2
Excise affected area with as big a margin as possible
Principles same as cystotomy
Cystostomy
indication 2
uncommon, Allows bladder drainage whilst bypassing the urethra
neoplasm: divert prior to chemo; uroliths: transport from referral temporary diversion
Used to pexy bladder to body wall – e.g. retroflexed bladder in perineal hernia
Foley catheters, mushroom catheters
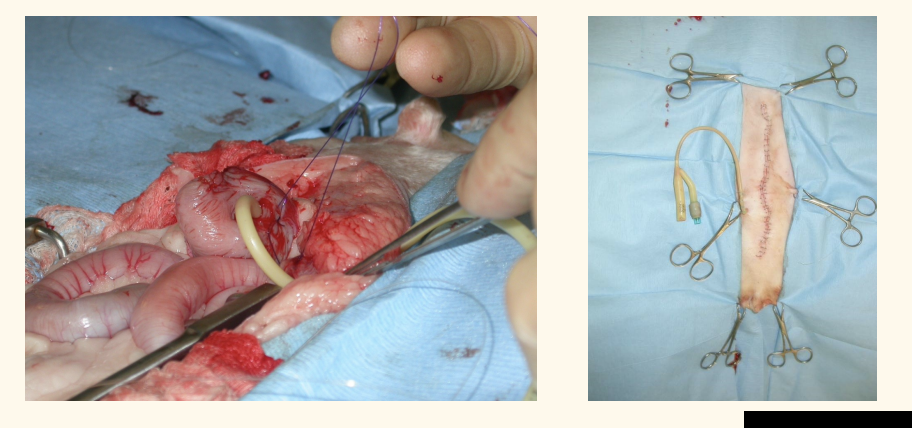
Cystostomy • The same technique as tube gastrostomy
A cranial midline coeliotomy is performed to access the stomach5 .
For gastropexy in GDV, a pyloric antrum gastrotomy is performed6 .
A de Pezzer catheter (mushroom tipped) is commonly used as the gastrostomy tube5 ....
The tube is pulled through a tunnel in the left body wall (or right body wall for GDV according to one source6 )5 .
A purse-string suture is placed on the stomach wall, and a stab incision is made in the centre5 ....
The feeding tube is inserted into the gastric lumen, and the purse-string suture is tightened around the tube5 ....
Pexy sutures are placed to secure the stomach to the abdominal wall5 ....
The tube is further secured to the body wall, often using a Chinese finger trap suture5 .... This helps prevent the patient from removing the tube5 .
FIX THIS
care: M dog: cauda; epigastric + retractor penis m.
foley catheter
purse-string in urinary baldder→ stab purse string
tighten purse string
tacking suture: bladder and body wall
Urethral surgery • Indications 3
Urethral obstruction: urolithiasis or FLUTD
Penile / urethral trauma or disease
Urethral prolapse
Urethral obstruction usually
urolithiasis
FLUTD (medx management ok)
Urethral obstruction Consequences: 4
emergency
Postrenal azotaemia
Hyperkalaemia
Hydronephrosis
Bladder damage
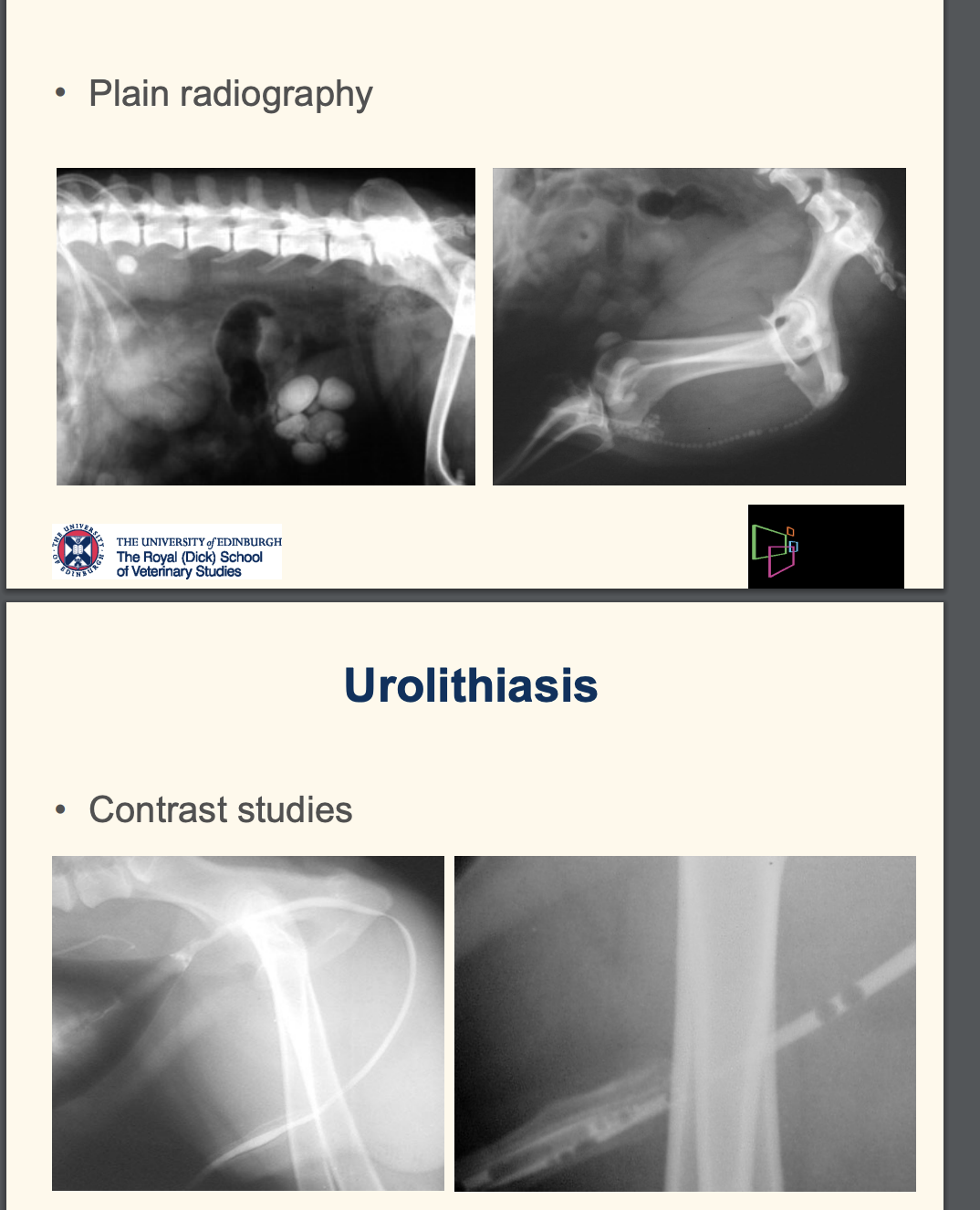
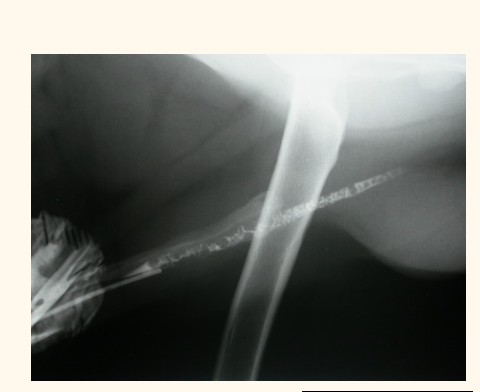
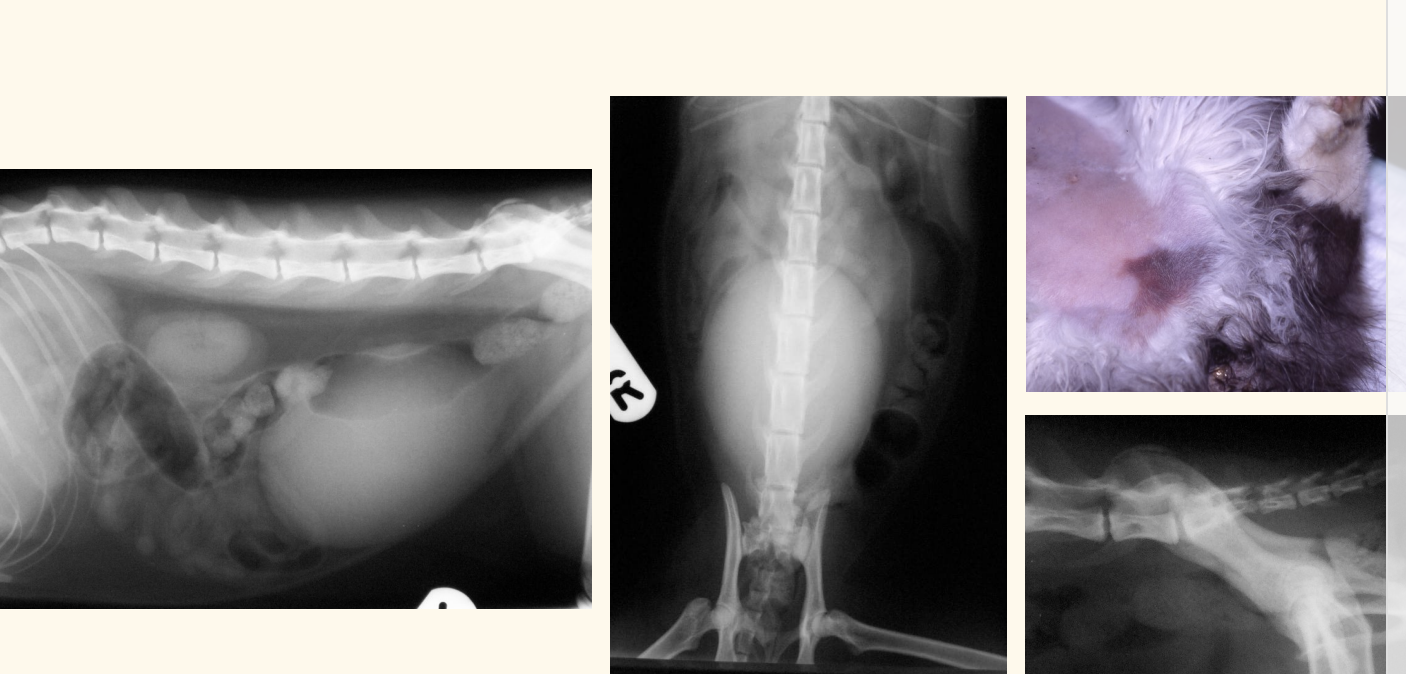
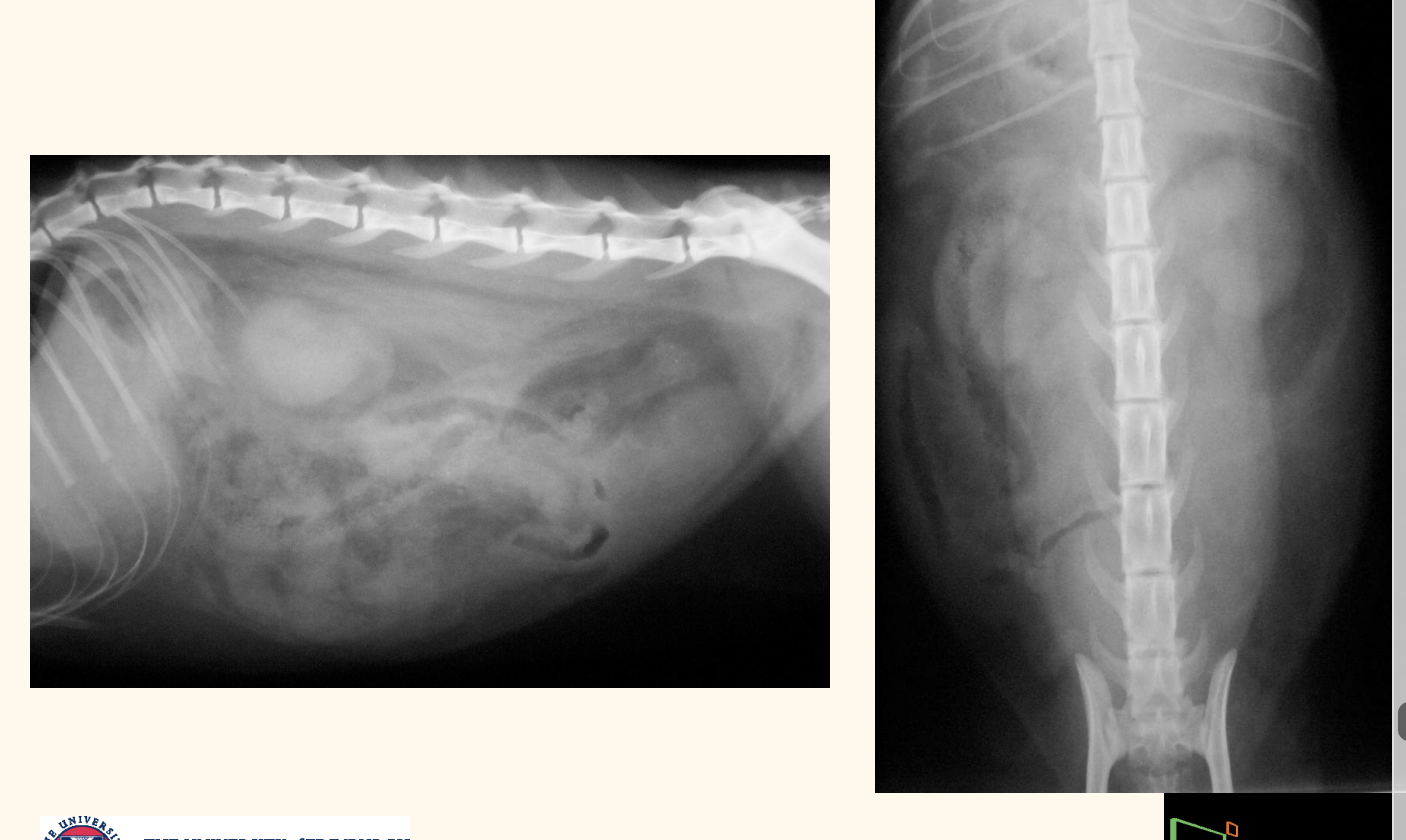
Urolithiasis dx imaging
plain radiograph
contrast (if radiolucent stone): retrograde urethograms
—> important to include the ENTIRE UT
Urethral obstruction urolithiasis
Options for management 3
which one most common and first choice?
Push stones into the bladder
Remove stones from urethra (uncommon)
damage/stricure—> Create a new stoma into urethra above the obstruction (uncomon)
Push urolithiasis into bladder— how? 8
Preferred option: retrograde urohydropropulsion
Remove stones by medical dissolution or cystotomy
feel pelvic brim through rectal
squish finger between recum and pelvic brim
tube like structure—> urethra
squish distal to stone
introduce foley catheter until tip of penile urethra
inject saline through catheter
dilates everything distal to stone
urothelium fills and lift up until pressure build up
once pressure if high, lift finger
release occlusion, urolithiasis fly into bladder
± lidocaine, ± KY jelly
repeat a few time. cystocentesis may be needed .
confirm with radiography
urolithiasis— Remove from urethra
how?
uncommon in
Urethrotomy — hole into
Create temporary hole into urethra
Remove stones
Allow urethra to heal by second intention
Uncommon in female dogs or cats — Shorter and wider urethra
Urethrotomy in male dog
common location
usually prescrotal region

– Urethrotomy in male dog
how?
do we like this sx?
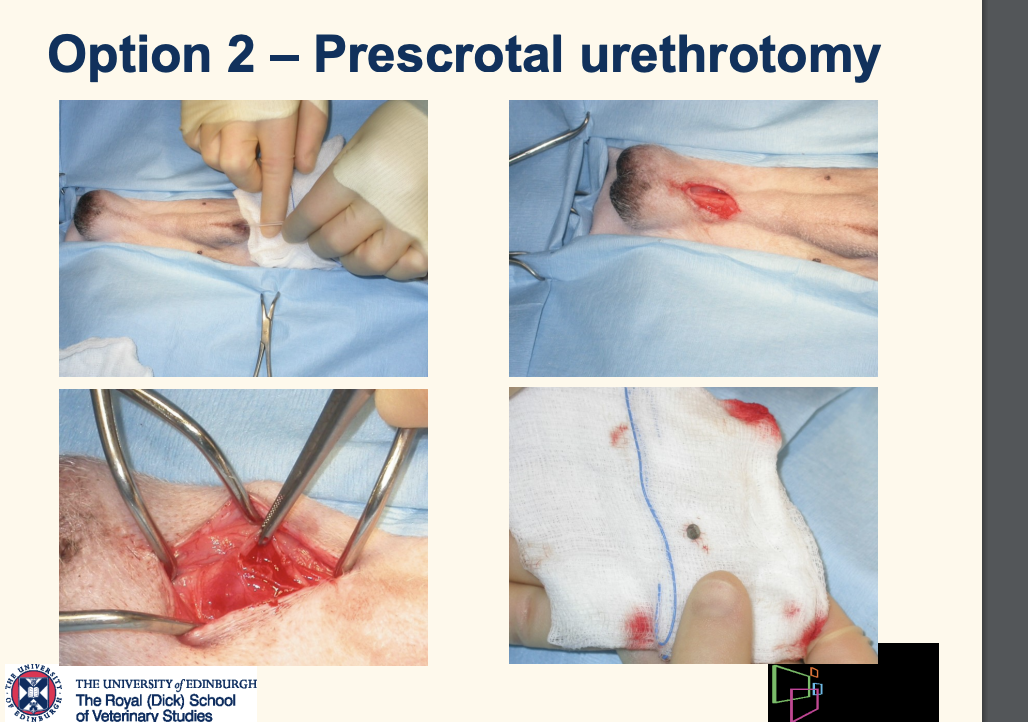
Prescrotal urethrotomy
Place urinary catheter
Incise skin behind os penis
Reflect retractor penis muscle
Incise urethra
Remove stones
Flush to ensure all stones removed
Suture or leave open to heal by second intention
NO IT IS BLOODY FIDDLY AVOID IF YOU CAN
– Permanent urethral stoma: Urethrostomy
performed whem
– Can’t dislodge stones – Stricture has formed – Repeated obstructions
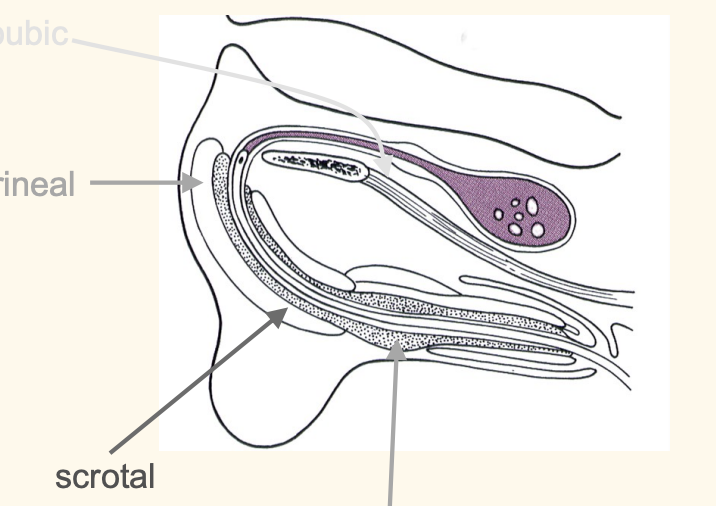
**MCQ SAQ EXAM Urethrostomy male dog: ideal location
prepubic x
perineal (uncommon)
prescrotal (too much vasculature, thin urethra)
SCROTAL REGION is the most common
Scrotal urethrostomy
consideration 2
• Castrate • Make stoma large: 2.5 – 4 cm
perineal urethrostomy
indication
Scrotal urethrostomy and prescrotal urethrotomy cannot be performed in the male cat
severely obstructed FLUTD cases: cats
Perineal urethrostomy— how?
ventral recumbancy, tail reflected to dorsum
teardrop shape incision around penis
pull penus towards me, blunt dissection going forward
spiral shape debridement
when cannot move forward—> ischial cavenosus muscle— between ischium and penis
transect
urethrostomy site: bulbourethral gland (when narrow urethra becomes wide)
suture urothelium to skin: aim for primary closure
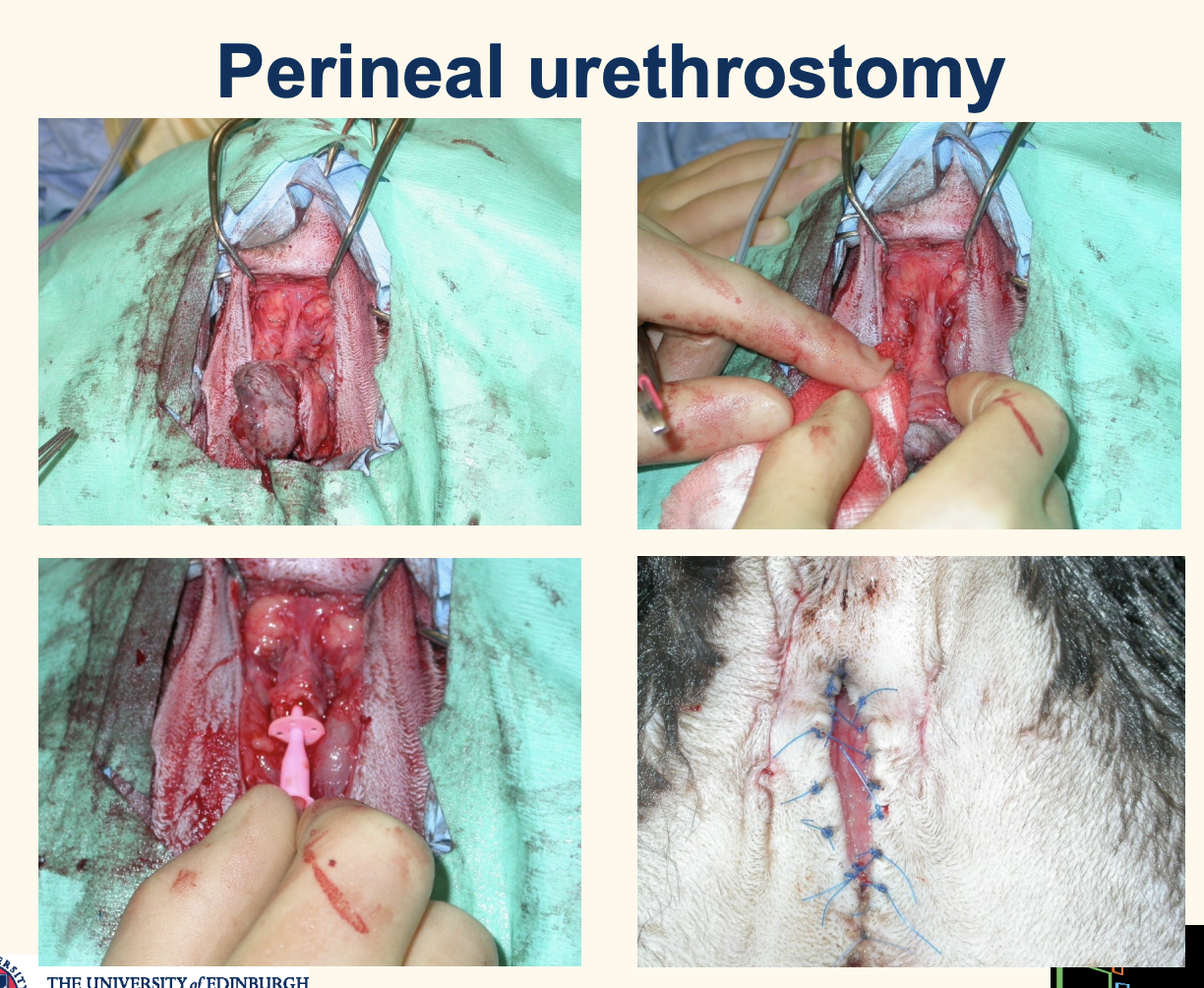
Complications of urethrostomy 4
Haematuria : UT trauma/cyctitis/ ooze around surgical site
Stenosis: stoma can reduce 50% of size
ensure meticulous appositional urothelium and skin closure
big enough stoma as possible
no one pokes the site! do not clean!
Incontinence
Urinary tract infection

Urethral prolapse is commonly seen in 4
Young male dogs that likes to hump
Sexually intact
Brachycephalic breeds
Self-inflicted trauma (or 2dry)
Urethral prolapse: surgery
Resect prolapse — same as rectal prolapse
double-check and add
Castrate
Alternatively: urethropexy
advise to owner pre bladder surgery
even if leak tested, still uroabdomen risk
can place temp foley to help with healing
Uroabdomen - causes
Trauma
Ureter avulsion
Bladder rupture
Urethral rupture
Pelvic fracture—> laceration
Secondary to bladder disease
Iatrogenic
Urinary surgery
Traumatic catheterisation
Cystocentesis
Uroabdomen - presentation
similar to blocked bladder
uraemia + hyperkalaemia
cardiac arrythmis: sinus brady, peak t wave
Ascites, abdominal discomfort
Initially bladder often palpable
Animal is often able to urinate
bladder rupture rx
how long?
rupture bladder: Radiography at 1 hour
bladder rupture rx
how long?
Radiography at 8 hours
cannot see bladder
idelaly want to dx before 8hr
what to do for early diagnosis imaging of uroabdomen?
US
Uroabdomen - diagnosis
Serum biochemistry + urinalysis
what else will you do?
where do u find abdo fluid
increased Urea, Creatinine, Potassium (postrenal azotemia +hyperkalemia)
+/- Haematuria
Urine SG 1.008 to >1.050
Look for free abdominal fluid: usually collects in apex of urinary bladder and liver
Abdominal fluid analysis : crea: high, abdo>blood; urea: high, abdo=blood
Urinary tract imaging
Abdominal fluid collection mehtods: 3
test of choice
Abdominocentesis
POCUS scan
Diagnostic peritoneal lavage (like 4 sepsis)
uroabdomen: Abdominal fluid analysis
which one is more indicative
confirmed if
Urea: small molecule equilibrates quickly
Creatinine: large molecule does not equilibrate, stay high in abdo
confirmation:
[Creatinine (ascites)] > [Creatinine (serum) - mean 2:1
[Potassium (ascites)] > [Potassium (serum)]- dog 1.9/ cat 1.4:1

what deos this contrast radiography shoe
leakage of contrast into abdomen
urethrea lost…
Uroabdoman: management once diagnosed
5
Medical stabilisation
IV fluid therapy (shock dose for hyper K)
Analgaesia (full mu opioid)
+/- Urinary diversion
Treat hyperkalaemia
Surgery once stabilised—> Exploratory coeliotomy
** MCQ SAQ EXAM treatment for arrythmia in hyperK 3
IV fluid
Calcium Gluconate intravenously over 20 minutes (unless hypophosphatemia)
Glucose and Insulin