Workshop- Anaesthesia of Small Mammals and Exotics
1/29
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
30 Terms
how long do you starve rabbits before GA?
you don't want to starve them as they can't vomit, make sure they have eaten a few hours before
just remove food and rinse mouth abt 30 mins before intubating
Why may you remove food from the enclosure before inducing ?
removing food 30 minutes ish before induction means there will be less food in their mouth when you intubate
why is reducing stress so important in rabbits pre-anaesthesia ?
stress releases catecholamines and this can cause arrythmias, and resistance to drugs - higher doses needed have more side effects.
they are prey animals
can cause gut stasis too
how do you ventilate rabbits, devices, form and considerations?
- ET tubes (more difficult as they have an elongated soft palate),
- masks - for shorter procedures (they are obligate nose breathers)
- supraglottic device (v-gel - easier to place, but can move if animal moves), IPPV (manual ventilation)
use a non-rebreathing system (mini lack or T-piece) because of their size and ratio of lung to body.
attach to capnograph
why do you have to be careful if moving patients when theyre ventilated
Tracheal tube wont move
Vgel only on top of glottis so could move if animal moves and system doesn’t-> not ventilated anymore
Can you intubate ferrets and other small furries ?
complicated due to size and anatomy of the trachea
can use an endoscope to visualise
intubation is not usually done
how do you position rabbits and why is this different from dogs and cats?
elevated thorax and head because guts puts pressure on the diaphragm, and straighten neck for optimal ventilation
don’t want neck falling down onto chest when doing this as tube could be bent so try make head and neck straight
what equipment do you use to monitor you rabbit under GA?
- capnograph (esp for v-gel),
- pulse oximetry on auricular vein (difficult, made for dogs, and rabbits very furry),
- blood pressure monitor - not very accurate.
Doppler hard to catch pulse
Oscillometric machine nice but only usually works when bp is normal -> low pressure wont give number
So if give reading its ok, but if not then is probs low
Invasive in a -> usually lot of bleeding and clotting/ necrosis of eat, can be expensive too -> only really if you really want to know
- temperature - anal probe more effective
Oes temp probe not best bc tend to bite
- doppler - rate and rhythm, other equipment may not be reliable for small furries
- ECG - pads don't work, clips do but be carful on small ones
how will you prevent hypothermia in your rabbit?
- heated pads (not weight triggered)
- bair huggers (can be too big)
- fluid warmer
- small amount of clipping
- cover ears - sock or bubblewrap
how can you increase a rabbits blood pressure
IVFT - bolus,
reduce isoflurane,
give drugs to counteract
glycopyrrolate -
instead of atropine bc have the enzyme
wake animal up if possible, adrenaline for crash
what drugs would you administer to your rabbit during GA to ensure a quick recovery
pain relief,
reverse any drugs,
keep them warm,
gut stimulants if needed
how long do you starve your bird before GA
you want their crop to be empty
Crop doesn’t have sphincter on proximal end to is open -> content will come out
budgies around 1 hour, parrots, chickens around 3 hours
variablility in size, water foul ?
raptors - dont typically need starve as they don't eat frequently, but if procedure in morning don't feed in morning.
palpate crop
Palp crop if empty is okay -> wait if not
But in crop stasis it will be full and cant do owt
Need to find balance between emptying of crop and glucose of gut (don’t want hypoglycaemic)
hypoglycaemia is more common is passerines
how will you ventilate your bird
ET tubes,
Can use iv catheter -> may get secretions stuck in them tho
masks.
DO NOT use cuffed tubes.
Closed rigns in trachea so esp important no cuff -> necrosis of mucosa of tracha if cuff-> stenosis
caudal air sac ventilation (O2 and iso) cannot use if cutting into coelomic cavity, but bypasses neck and secretions
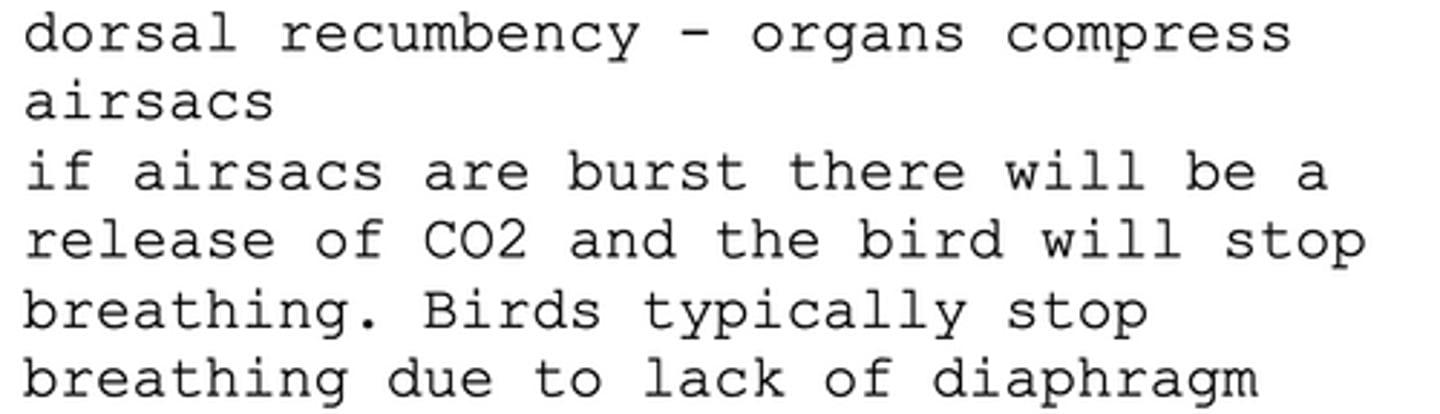
Why is it important that you ventilate a bird (manually or mechanically)
CO2 release makes birds stop breathing
lack of diaphragm makes them stop breathing
dorsal recumbancy - organs compress airsacs
if they burst CO2 is released
How do you intubate a parrot ?
trachea gets narrow in the distal section - so don't use tube size that fits glottis. stop when there is any friction (complete rings)
or use a specific parrot tube
why might a fracture of the birds humerus effect the respiratory tract
pneumatised bones - air leaves bones. different birds have different pneumatic bones, but humerus is in most
What are some considerations for open fractures in birds?
infection coming in
air going out of pneumatic bones- reduced respiration capacity
blood in resp system
how will you clean ? - fluid will go into airsacs
so don’t OR flush with small amounts at a time and use aspiration devise at the same time so doesn’t go to resp system
considerations for closed fractures in birds
Less of an issue bc no exposure to external environment
but in Surgery -> once cut skin -> is now open fracture so same as before
what equipment do you use to monitor your bird under GA?
capnography, stethoscope, blood pressure, doppler, thermometer
SPO2 - reading will not be reliable, but can give you pulse waves
Thin skin so works quite well
ECG - be careful with clips - use less trauma
temp- cloaca, oesophagus (not parrots bc their beak will break probe)
doppler
On wing (ulnar a on inside of wing)
Clamp it on with the tongue depressors
Listen to rhythm of pulse
how will you prevent hypothermia in birds?
bair huggers, no surgical spirit, heat pads, hot hands, minimal plucking, keep them as dry as possible
Feathers acta as an isolating device if you keep them dry -> easier to maintain temp
Wet makes the transfer of temp easier -> colder quickly
how could you administer fluids to this bird whilst under GA?
IV - into the wing ulnar vein or jugular vein,
SC - inguinal flap,
IO
easier to place but remember pneumatic (tibiotarsal bone (bigger and easier, goes through knee), ulnar bone (distal to proxmial, harder but eaier when woke up))
how do you ventilate a tortoise?
ET tube - never cuffed, IPPV or electric ventilator is needed to keep them breathings - tortoises use their legs to induce breathing, when unconscious, they can't do this. once or twice a minute.
never gas them down - they will hold their breath and have low resp rate so too long
How quickly will reptiles take to start breathing post anaesthesia
slow recovery they will take a long time
why is it important to keep tortoises temperature as close to 30 degrees as possible?
They need external sources of heat to regulate their temperature, their metabolism is low so we have to keep it steady. Drugs will take longer to take effect if they are cold
Low temp -> low metabolic rate -> dcrs hr -> drugs take longer to move round the body -> longer to take effect
and they will take a long time to warm up if they're cold
what equipment do we use to monitor a tortoise (reptiles) under GA?
doppler
Peripheral bp of reptiles is normally low
on heart is best
Tortoise on shell where heart would be if small enough
If big on between neck and shoulder
BP - not reliable measure in reptiles - it is low even on invasive read.
capnograph (levels not reliable),
oesophageal or cloacal stethoscope
pulse oximeter (not accurate because of scales, and tongues not long enough to exteriorise.
ECG - chelonians have 3 ventricles so wave is different but is accurate to HR, use needles and clamp clip to needle (scales)
Stick needles into skin then clip to needles
How will you use a temperature probe in reptiles
mouth or cloaca
How do you use a doppler for a reptile or chelonian?
peripheral blood pressure is very low - will need to be placed directly on top of their heart - know the anatomy. You may find a pulse close to the entrance of the neck/ shoulder
what stimulates a reptile to breath?
their oxygen levels, when they are low they are stimulated to take a breath. higher blood pH and can do a lot of anaerobic resp, so high CO2 doesn't effect them
why can reptiles sometimes not breath when waking up?
the oxygenation you provided is still lasting and they won't be stimulated to breathe. ventilate with an ambo bag - to deliver lower oxygen
So on recovery stop the oxygen disconect tube and ventilate with abu bag or room air (use o2 in air) -> help stimulate the breathing
why might you not be able to keep the tube connected to reptiles when theyre waking up
They will wake up/ move before they start breathing
So may not be able to keep the tube connected -> take tube out (and move legs in tortoise)