Ella Kulman Rheumatology/MSK
1/139
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
140 Terms
Give 3 causes of inflammatory joint pain
1. Autoimmune diseases (eg. RA, vasculitis, connective tissue disease)
2. Crystal arthritis
3. Infection
Give 2 causes of non-inflammatory joint pain
1. Degenerative (e.g. osteoarthritis)
2. Non-degenerative (e.g. fibromyalgia)
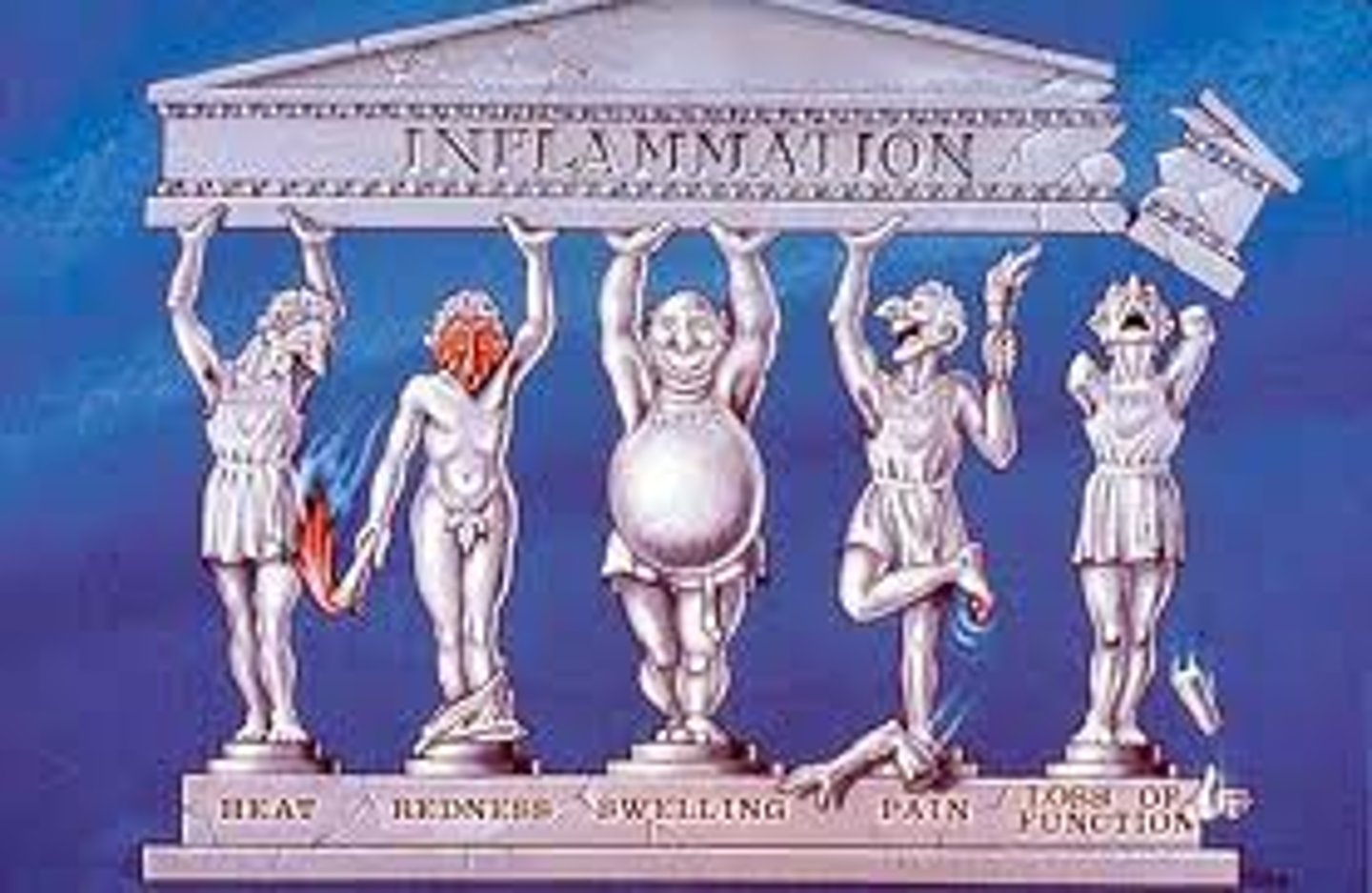
5 cardinal signs of inflammation
1. Rubor (redness)
2. Calor (heat)
3. Dolor (pain)
4. Tumor (swelling)
5. Loss of function
How does inflammatory pain differ from degenerative non-inflammatory pain?
Inflammatory pain tends to ease with use, whereas degenerative pain increases with use
Are you more likely to see swelling in inflammatory or degenerative pain?
In inflammatory pain you are likely to see synovial swelling. There is often no swelling in degenerative pain
Name 2 inflammatory markers that can be detected in blood tests
1. ESR (erythrocyte sedimentation rate)
2. CRP
Explain why ESR levels are raised in someone with inflammatory joint pain
Inflammation leads to increased fibrinogen which means the RBC's clump together. The RBC's therefore fall faster and so you have an increased ESR
Explain why CRP levels are raised in someone with inflammatory joint pain
Inflammation leads to increased levels of IL-6. CRP is produced by the liver in response to IL-6 and therefore is raised
Describe the ESR and CRP levels in someone with lupus
ESR is raised and CRP is low
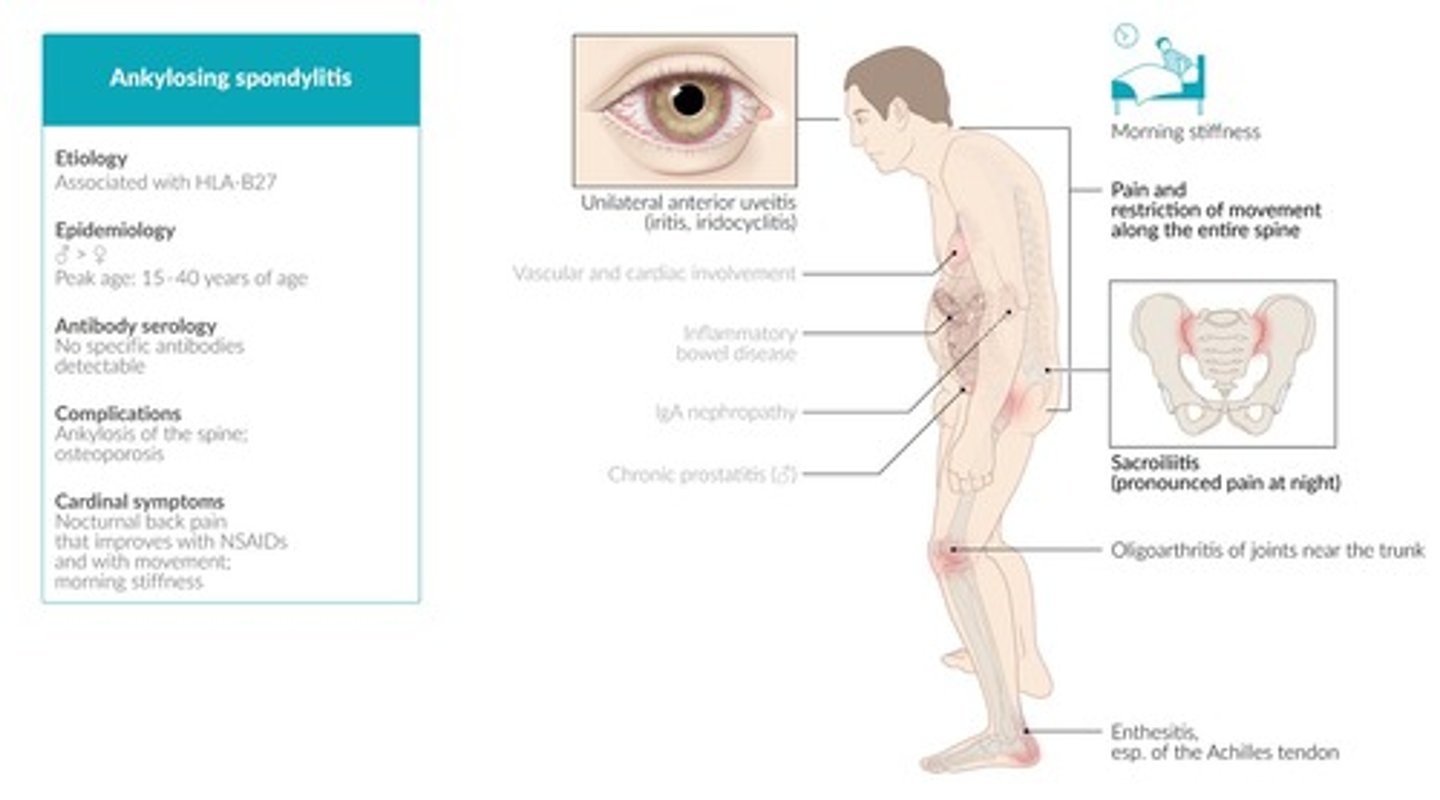
5 conditions that fall under the umbrella term spondyloarthritis:
1. Ankylosing spondylitis
2. Reactive arthritis
3. Psoriatic arthritis
4. Enteropathic arthritis
5. Juvenile idiopathic arthritis
Signs of spondyloarthritis:
1. Psoriasis
2. Inflammatory spine and buttock pain
3. Good response to NSAIDs
4. Enthesitis
5. Arthritis
6. Crohn's/colitis associated
7. Uveitis
General treatment for all spondyloarthritis:
Initially DMARDs and then biological agents if DMARDs fail, e.g. TNF blockers
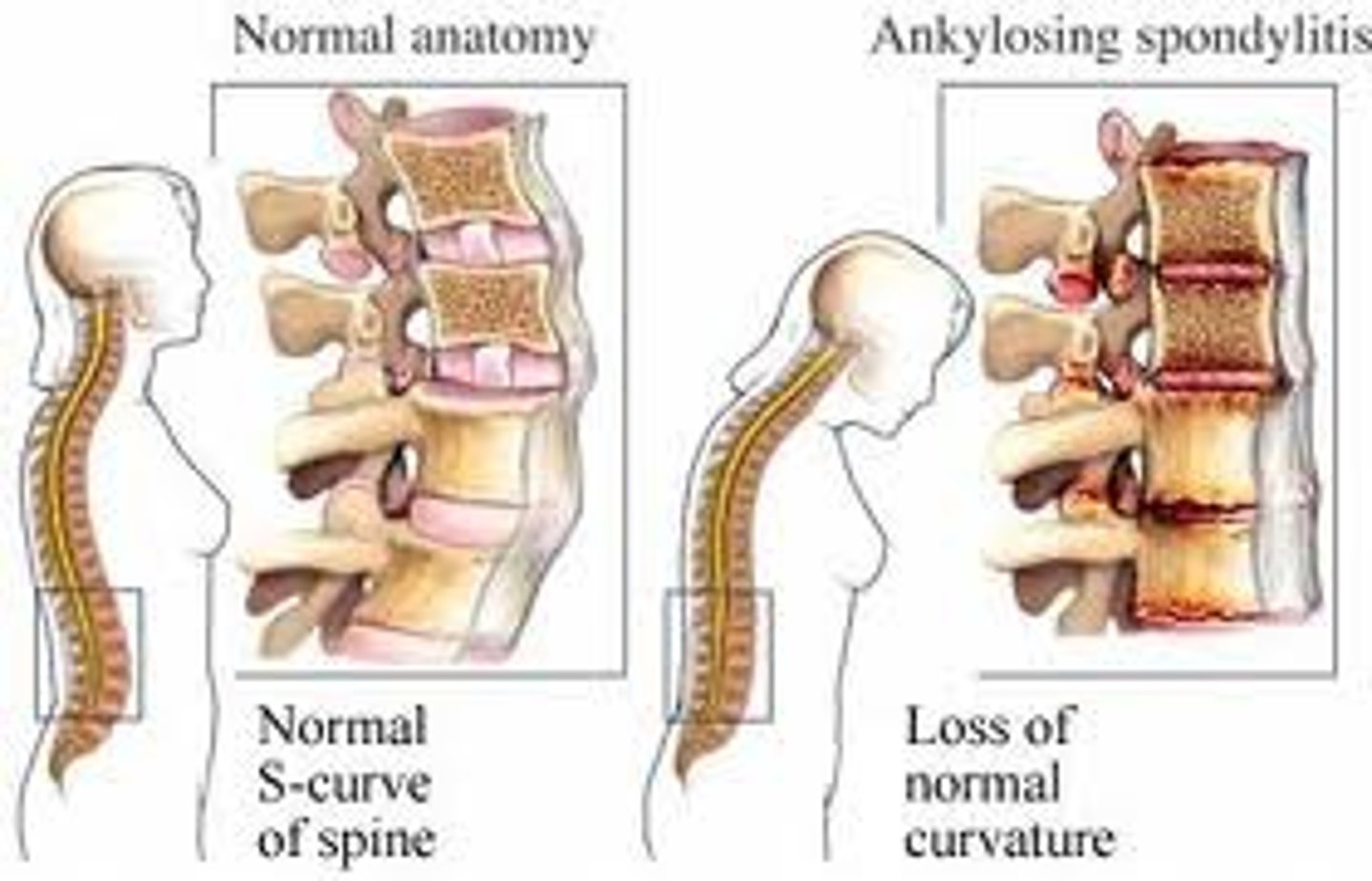
Describe the pathophysiology of ankylosing spondylitis
Inflammation of spine → erosive damage → repair/new bone formation → irreversible fusion of spine
Symptoms of ankylosing spondylitis:
1. BACK PAIN!!
2. Morning stiffness
3. Waking in the second half of the night
4. Buttock pain
5. Insidious onset
6. Usually <40 y/o at onset
3 locations that psoriasis commonly occurs at:
1. Elbows
2. Knees
3. Fingers

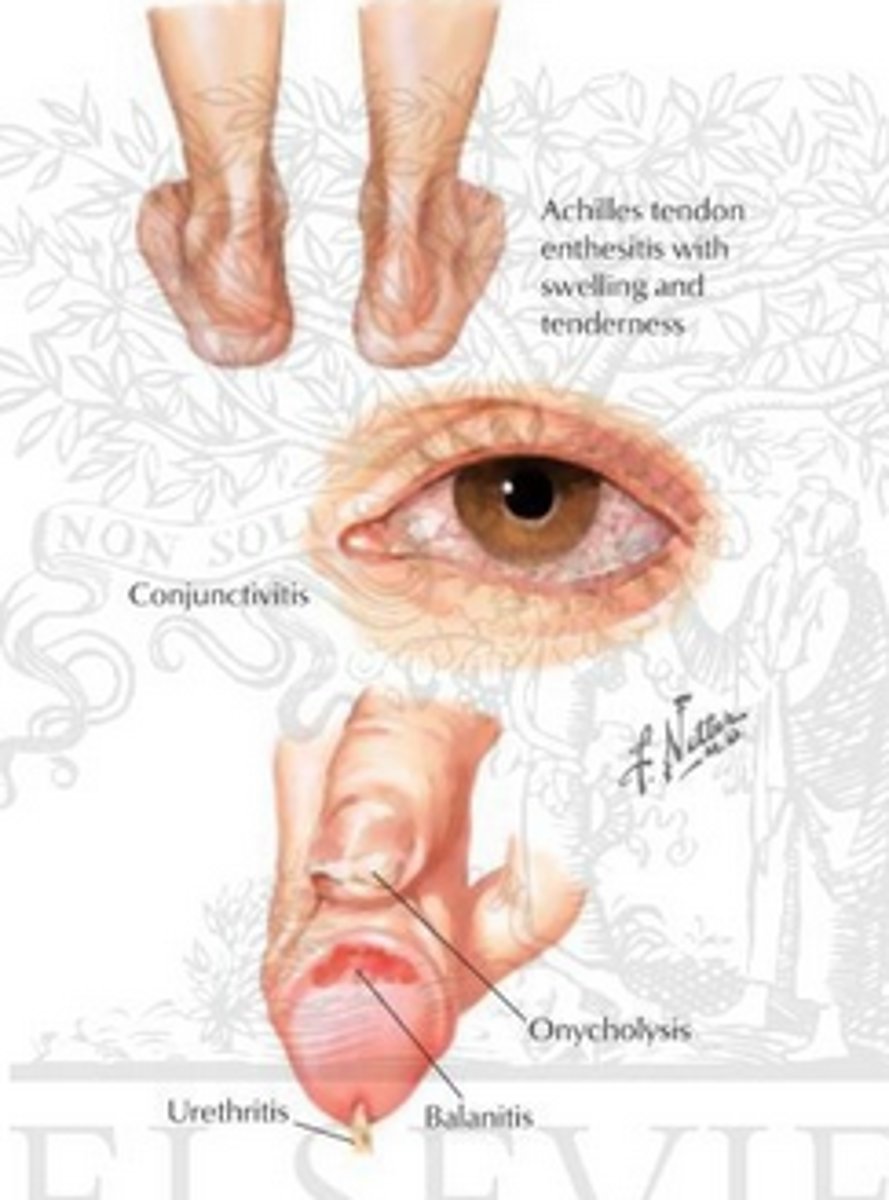
What is reactive arthritis?
Sterile inflammation of the synovial membrane, tendons, and fascia triggered by an infection at a distant site (usually GI or genital)
What gut infections are usually associated with reactive arthritis?
Salmonella, shigella
What STI's are associated with reactive arthritis?
Chlamydia
What is the triad of symptoms for reactive arthritis?
1. Arthritis
2. Conjunctivitis
3. Urethritis
What type of spondyloarthritis occurs in 20% of pts with IBD?
Enteropathic arthritis
Why is it important to check eyes in JIA (juvenile idiopathic arthritis)?
The lining of the eyes and the joints is very similar. Children with JIA are at a high risk of developing uveitis
Describe the medical treatment for JIA
1. Steroid joint injections
2. NSAID's
3. Methotrexate
4. Systemic steroids
4 diseases that fibromyalgia is commonly associated with:
1. Depression
2. Chronic fatigue
3. Chronic headache
4. IBS
What 2 things are essential in the management of fibromyalgia?
1. Explaining that sleep disturbance is central to what they're feeling
2. Emphasising the importance of exercise + fitness
What is vasculitis?
Inflammation and necrosis of blood vessel walls with subsequent impaired blood flow
What cells might you see on a histological slide taken from someone with vasculitis?
neutrophils and giant cells
What is rheumatoid arthritis?
An auto-immune inflammatory synovial joint disease
Is RA more common in men or women?
women (2-3x more)
Symptoms of RA:
1. Early morning stiffness (>60 mins)
2. Pain eases with use
3. Swelling
4. General fatigue/malaise
5. Extra-articular involvement
Signs of RA:
1. Symmetrical
2. Deforming
3. Polyarthropathy
4. Erosion on x-ray
5. 80% are RF +ve
RA extra-articular involvement: describe the effect on soft tissues
- nodules
- bursitis
- muscle wasting
RA extra-articular involvement: describe the effect on the eyes
- dry eyes
- scleritis
- episcleritis
RA extra-articular involvement: describe the haematological effects
- palpable lymph nodes
- splenomegaly
- anaemia
RA extra-articular involvements: describe the pulmonary effects
pleural effusion
what investigations might you do in someone who you suspect has RA?
Bloods - ESR and CRP
Test for anaemia
Test for RF and anti-CCP
Describe treatment for RA
- NSAIDs
- corticosteroids
- DMARDs
- biological agents
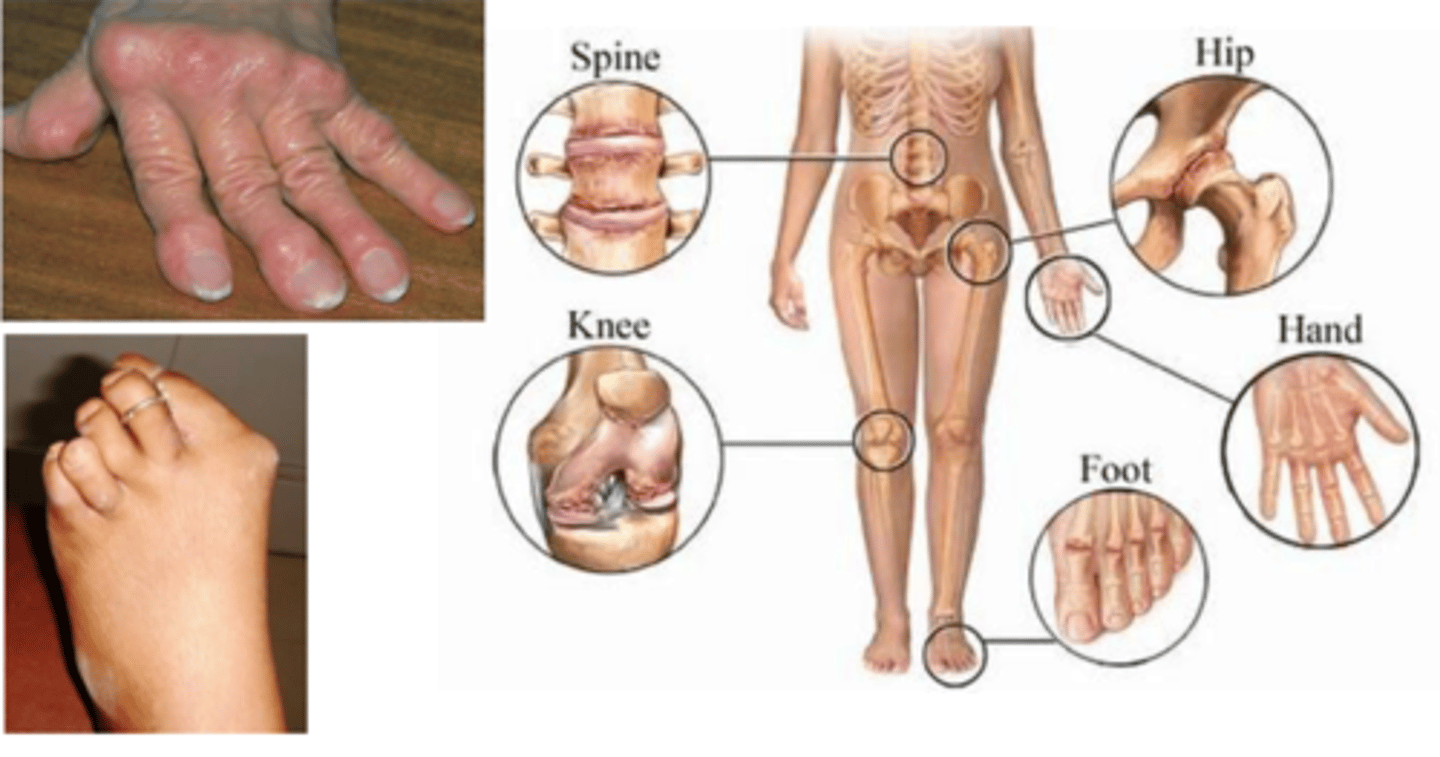
Define osteoarthritis
A non-inflammatory degenerative disorder of moveable joints characterised by the deterioration of articular cartilage and the formation of new bone

5 risk factors for OA
1. Genetic predisposition
2. Trauma
3. Abnormal biomechanics e.g. hypermobility
4. Occupation e.g. manual labour
5. Obesity; pro inflammatory state
What are the most important cells for OA?
chondrocytes
Symptoms of OA:
- morning stiffness (<30 mins)
- pain → aggravated by activity
- tenderness
- walking and ADLs affected
- joint swelling and bony enlargement
- deformities
- crepitus
Radiological features associated with OA:
1. Joint space narrowing
2. Osteophyte formation
3. Sub-chondral sclerosis
4. Sub-chondral cysts
5. Abnormalities of bone contour

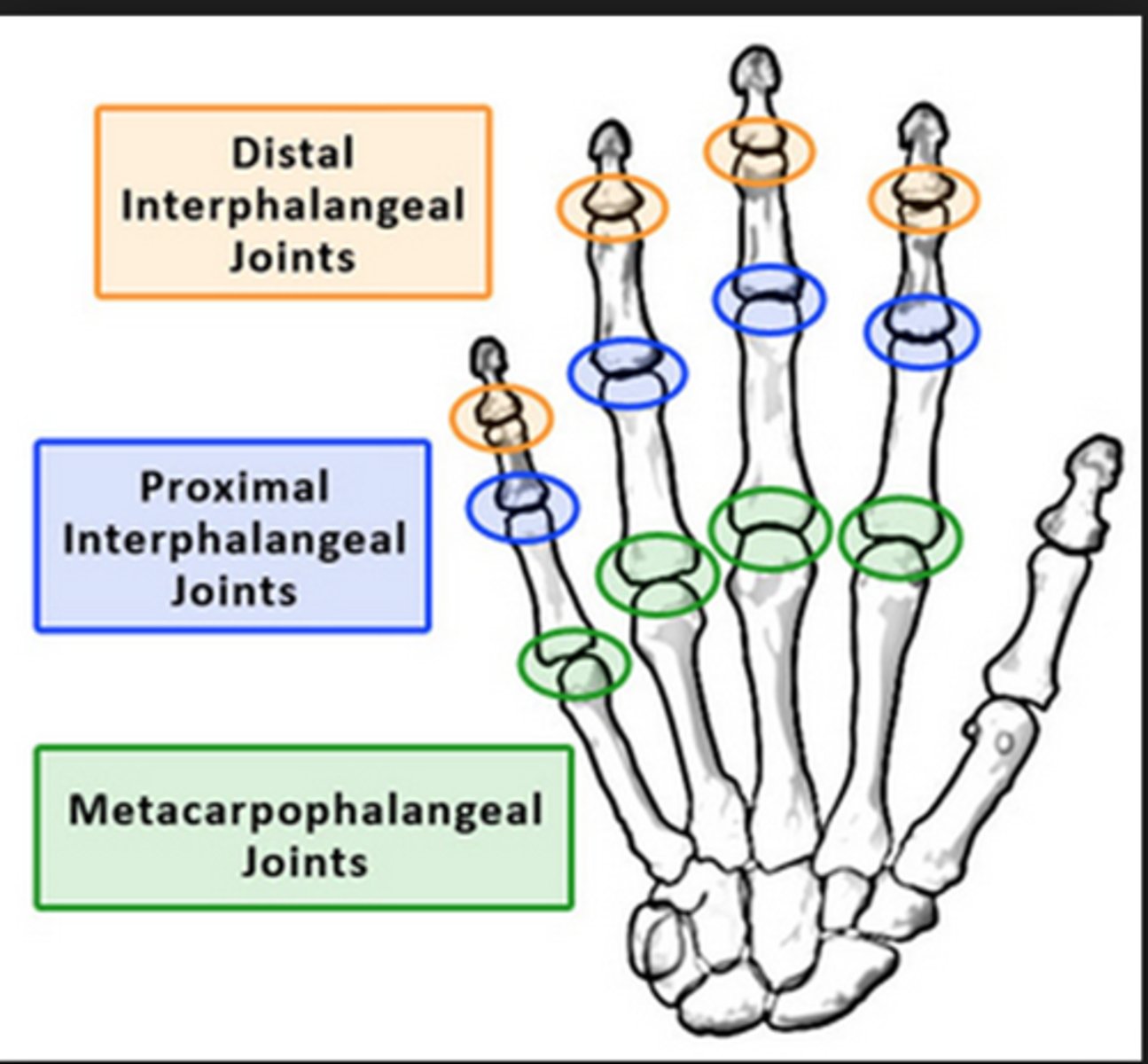
Name 3 joints of the hand that are commonly affected in Osteoarthritis
1. Distal interphalangeal joint
2. Proximal interphalangeal joint
3. Carpometacarpal joint
Which surface of the knee is most commonly affected by OA?
medial
What is the primary investigation used to make a diagnosis of OA?
X-ray (look for asymmetric loss of joint space; sclerosis; cysts and osteophytes)
Describe the pharmacological management for OA
- NSAIDs (topical better than PO)
- paracetamol
- intra-articular steroid injections
- DMARDs if there is an inflammatory component
Give 3 indications for surgery
1. Significant limitation of function
2. Uncontrolled pain
3. Waking at night from pain
Pt complains of 'locking', what is the most likely cause of this?
probably due to a loose body (e.g. a bone or cartilage fragment)

what is the treatment for loose bodies?
Arthroscopy
What is SLE?
systemic lupus erythematosus → an inflammatory multi-system disease characterised by the presence of serum anti-nuclear antibodies (ANA)
Who is most likely to have SLE?
- 90% of cases are young women
- more common in afro-caribbeans
- genetic association
Symptoms of SLE:
1. Butterfly rash
2. Mouth ulcers
3. Raynaud's phenomenon/'cold pale fingers'
4. Fatigue
5. Depression
6. Weight loss
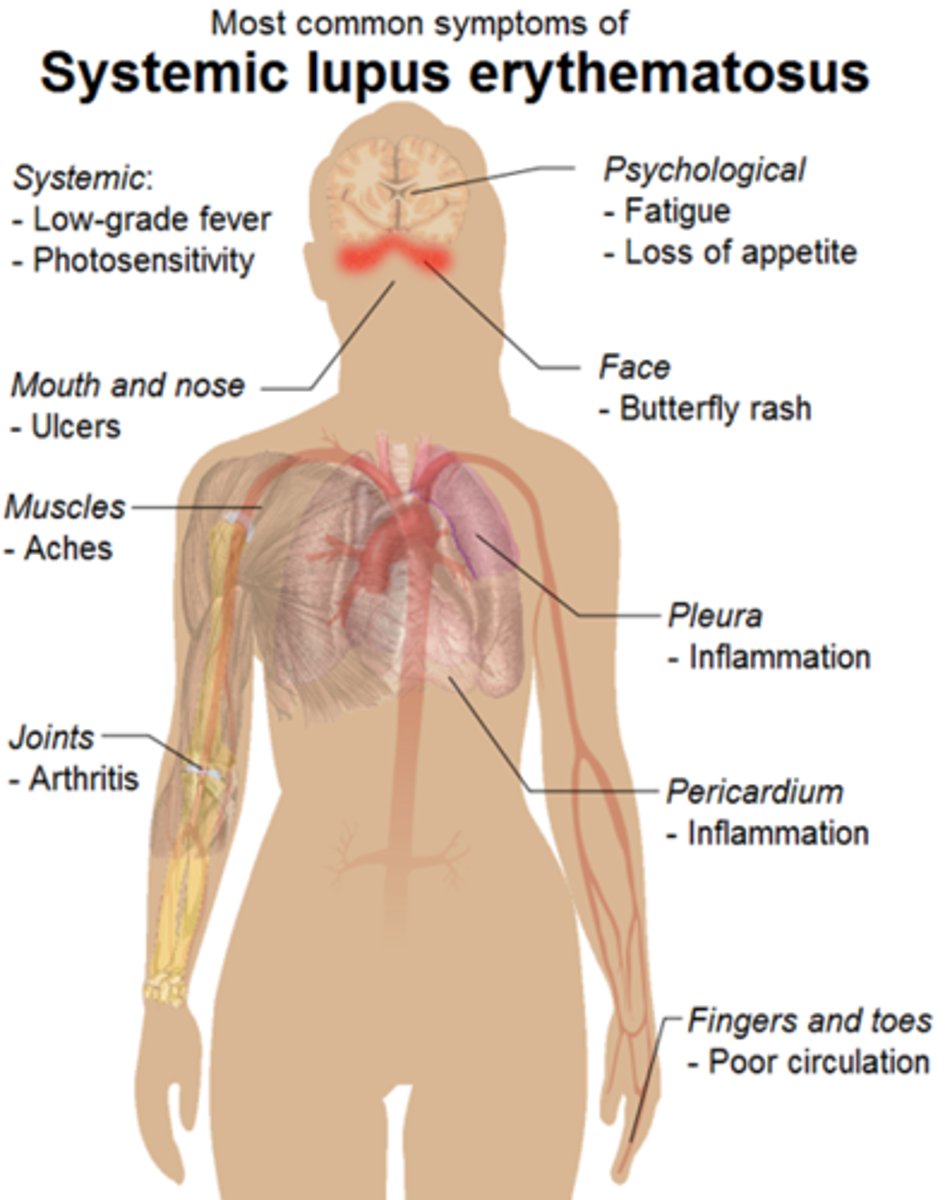
What investigations might you do in someone with suspected SLE?
1. Blood count might show normocytic anaemia; neutropenia; thrombocytopenia. Raised ESR, normal CRP
2. Serum antibodies: ANA, anti-dsDNA
Describe the non-medical treatment for SLE
- education and support
- UV protection
- Screening for organ involvement
- reduce CV RF e.g. smoking cessation
Descibe the pharmacological treatment for SLE
- corticosteroids
- NSAIDs
- antimalarials (DMARDs)
- anticoagulants (for those with antiphospholipid antibodies)
- biological therapy targeting B cells (eg. rituximab)
What is the name given to the inflammation of an entire digit?
dactylitis

Who is most likely to get gout?
men >75 y/o
Symptom of gout
Hot and swollen joints (toes are commonly affected)

What are tophi?
White chalky aggregates of uric acid crystals with inflammatory calls. Proteolytic enzymes are released → erosion

Conditions someone with gout is at risk of developing
1. Hypertension
2. CV disease (e.g. stroke)
3. Renal disease
4. T2DM
What is the aim of treatment for gout?
To get urate levels <300umol/L
Treatment options for gout:
1. Lifestyle modification (e.g diet, weight loss, reduced alcohol)
2. Allopurinol (blocks xanthine oxidase)
3. Colchicine or NSAIDs
4. Switch from bendroflumethiazide to cosartan
5. Rasburicase → rapid urate reduction
Describe the pathophysiology of pyrophosphate arthropathy (pseudogout)
Calcium pyrophosphate crystals are deposited on joint surfaces → the crystals elicit an inflammatory response
What conditions can cause pseudogout?
1. Hypo/hyperthyroidism
2. Diabetes
3. Haemochromatosis
4. Magnesium levels
Give a symptom of pyrophosphate arthropathy (pseudogout)
Acute, hot and swollen joints. Typically the wrists and feet
What investigations might you do in someone who you suspect might have pyro phosphate arthropathy (pseudogout)?
Usually diagnosed clinically. If doubt:
- aspiration (fluid for crystals and blood cultures)
- x-rays (can show chondrocalcinosis)
Describe the treatment for pyrophosphate arthropathy (pseudogout)
Treat the underlying cause and use methotrexate for inflammation
Define osteoporosis
A systemic skeletal disease characterised by low bone mass and mico-architectural deterioration. Pt is at increased risk of fracture
Name a hormone that can control osteoclast action and so bone turnover
Oestrogen
Why are so many women over 50 affected by osteoporosis?
likely to be post-menopausal → they therefore have less oestrogen, and so osteoclast action isn't inhibited. There is a high rate of bone turnover → bone loss and deterioration → fracture risk
What happens to bone micro-architecture as we get older that leads to a reduction in bone strength?
Trabecular thickness decreases; especially in the horizontal plane. There are fewer connections between trabecular and so an overall decrease in trabecular strength → increased risk of fracture
Why can RA cause osteoporosis?
It's an inflammatory disease → there are high levels of IL-6 and TNF; these are responsible for increased bone resorption
What is the effect of high cortisol levels on bone turnover?
Cortisol increases bone turnover. It leads to increased bone resorption and it also induces osteoblast apoptosis
RF for osteoporosis:
1. Previous fracture
2. FHx
3. Excessive alcohol
4. Smoking
5. Medications (e.g. steroids, depo provera)
6. Immobility
what investigations might you do in someone who you suspect to have osteoporosis?
DEXA scan (T score will be generated)
Name 2 areas of the skeleton commonly affected by osteoporosis that the DEXA scan focuses on
1. Lumbar spine
2. Hip
What T score signifies osteoporosis?
T < -2.5
What T score signifies pt has osteopenia?
-2.5 < T < -1
Give 2 examples of anti-resorptive treatments used in the management of osteoporosis
1. Bisphosphonates
2. HRT
*anti-resorptive treatments decrease osteoclast activity
Give an example of an anabolic treatment used in the management of osteoporosis
Teriparatide
*anabolic treatments increase osteoblast activity
Advantages of HRT:
1. reduces fracture risk
2. stops bone loss
3. prevents menopausal symptoms
disadvantages of HRT:
1. increased risk of breast cancer
2. increased risk of stroke and CV disease
3. increased risk of thrombo-embolism
3 initial steps in the management of fractures:
1. reduce the fracture (e.g. restore the length, alignment, rotation)
2. immobilise
3. rehabilitate
What is often the first line management option for paediatric fractures and why?
non-operative management e.g. traction, casts, splints. This is because paediatric bone heals quickly due to the thick periosteum
What can cause a supracondylar fracture in children?
falling on outstretched hand

what nerve might be affected in a supracondylar fracture?
median nerve
potential complications of fractures:
1. open fractures
2. neurovascular compromise
3. mal union - bone heals with deformity
4. non union - bone fails to heal
5. compartment syndrome
6. cast problems e.g. tightness, compartment syndrome, plaster burns/blisters
define osteomyelitis
bone inflammation secondary to infection
name 2 predisposing conditions for osteomyelitis
1. diabetes
2. PVD
Describe 3 ways a pathogen can get into bone
1. easy: inoculation of infection into the bone e.g. trauma/open wound
2. quite easy: contiguous spread of infection to bone from adjacent tissues
3. difficult: haematogenous seeding e.g. due to cannula infection
signs of osteomyelitis:
1. fever
2. rigors
3. sweats
4. malaise
5. tenderness
6. warmth
7. swelling
8. erythema
what investigations might you do on someone who you suspect has osteomyelitis?
1. bloods: raised inflammatory markers and WCC
2. plain radiographs and MRI
3. bone biopsy
4. blood cultures
what is the most common cause of septic arthritis?
Staphylococcus aureus
RF for septic arthritis
1. any cause of bacteraemia (e.g. cannula, UTI)
2. local skin breaks/ulcers
3. damaged/prosthetic joints
4. RA
5. elderly
symptoms of septic arthritis:
1. painful
2. red
3. swollen
4. hot
5. fever

treatment for septic arthritis:
- antibiotics guided by aspirate cultures
- joint wash out/repeated aspiration
- rest/splint/physio
- analgesia
what is bacteraemia?
bacteria in the blood
what is debridement?
removal of damaged tissue
what is the most serious complication of arthroplasty surgery?
prosthetic joint infection
what investigations might you do on someone who you suspect might have a prosthetic joint infection?
1. aspirate → microbiology
2. bloods for inflammatory markers and FBC
3. x-rays
what must you never do before aspirating a joint?
never give antibiotics before aspiration!