RCM 03 Respiratory Tract Infections: Bacterial Infections
1/34
Earn XP
Description and Tags
Learning outcomes - List important bacterial causes of upper respiratory tract infections and briefly describe clinical features and diagnostic investigations - Outline the classification of pneumonia and distinguish between community acquired, hospital acquired disease and infection in the immunocompromised, listing common organisms and main effects. - List predisposing factors to recurrent infection of the lung (chronic bronchitis, cystic fibrosis, COPD) and outline the profile of organisms involved. - Outline diagnostic investigation of LRTI
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
35 Terms
Pneumonia Classification
What are types of pneumonia?
Lecture Slide 4
Pneumonia is classified as community-acquired or nosocomial (hospital-acquired).
Community-acquired pneumonia is further subdivided into typical and atypical.
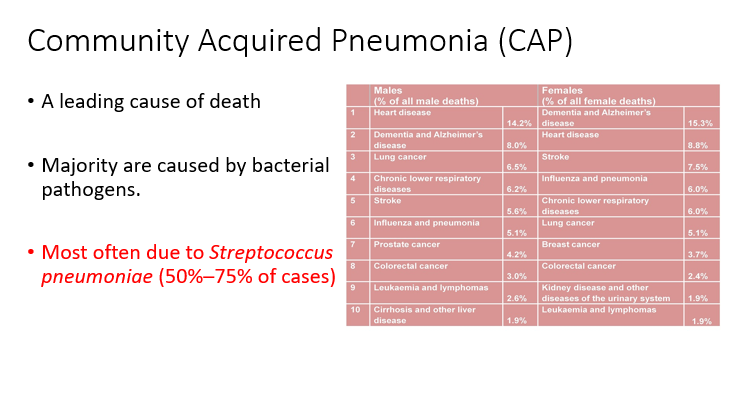
Community Acquired Pneumonia (CAP)
Which type of pneumonia is a leading cause of death and what are the majority often cause by?
Lecture Slide 5
Community acquired pneumonia (CAP) is a leading cause of death
Majority are caused
Diagnosis
How is pneumonia diagnosed? (2)
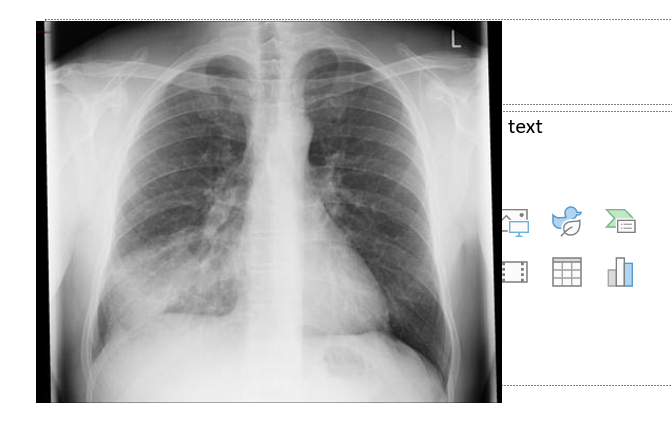
Lecture Slide 6
The presence of new symptoms or signs of lower respiratory tract infection
and
New pulmonary shadowing on CXR (Sensitivity 50% to 85%)

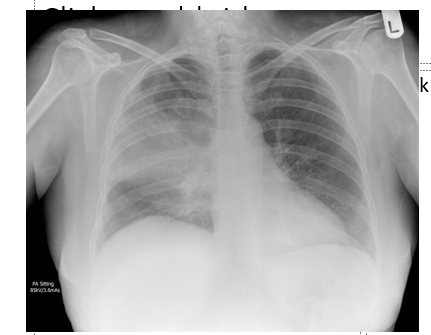
Can you provide labels, descriptions, and an explanation of the elements within this diagram, detailing what it represents or illustrates?
Lecture Slide 7
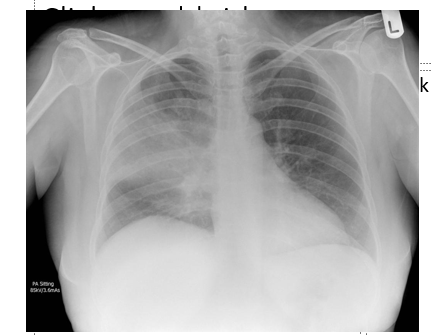
Can you provide labels, descriptions, and an explanation of the elements within this diagram, detailing what it represents or illustrates?
Lecture Slide 8
Pathogenesis Pneumonia
What are the primary pathways of pathogenesis for pneumonia, including the most common and least common causes? (3)
Lecture Slide 9
Microaspiration of oropharyngeal contents during sleep (most common cause)
Inhalation of aerosol drops ranging in size from 0.5 to 1 µm (second most common cause)
Bloodstream infection (least common cause)
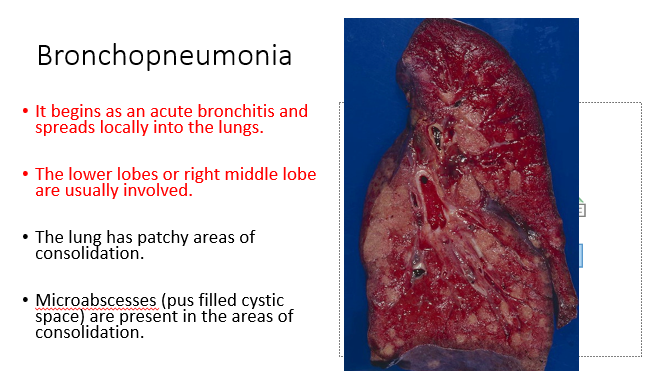
Bronchopneumonia
What characterizes bronchopneumonia in terms of its initiation, typical lung involvement, and the pathological features observed?
Lecture Slide 10
It begins as an acute bronchitis and spreads locally into the lungs.
The lower lobes or right middle lobe are usually involved.
The lung has patchy areas of consolidation.
Microabscesses (pus filled cystic space) are present in the areas of consolidation.
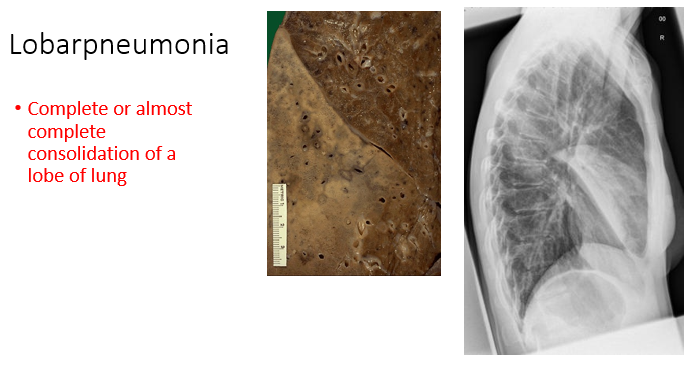
Lobar pneumonia
What is lobar pneumonia?
Lecture Slide 11
Complete or almost complete consolidation of a lobe of lung
Complications of pneumonia
What are some complications associated with pneumonia?
Lecture Slide 12
Complications of pneumonia may include lung abscesses, empyema (accumulation of pus in the pleural cavity), and the development of sepsis.
Causative Organisms
What are the proportions of causative organisms in cases of Community-Acquired Pneumonia (CAP), and how do they distribute among conventional bacteria, 'atypical' bacteria, and viruses?
Lecture Slide 13
In cases of Community-Acquired Pneumonia (CAP), conventional bacteria account for 60-80% of all cases, 'atypical' bacteria are responsible for 10-20%, and viruses cause 10-20% of CAP cases.
URTI - basically strep throat from a abacterial point of view
What is URTI, and what is its most common cause?
Lecture Slide 15
URTI, or Upper Respiratory Tract Infection, encompasses conditions from the top of the respiratory system to the vocal folds. The most common non-bacterial cause of URTI is rhinovirus, responsible for the common cold. Other viral culprits include influenza virus, adenovirus, enterovirus, and respiratory syncytial virus. Bacteria, particularly Group A streptococcus (S. pyogenes), cause around 15% of sudden onset pharyngitis presentations.
URTI - basically strep throat from a abacterial point of view
How is the common cold diagnosed, and what factors are considered in making this diagnosis?
Lecture Slide 15
The presence of classical features for rhinovirus infection, coupled with the absence of signs of bacterial infection or serious respiratory illness, is sufficient to make the diagnosis of the common cold. The common cold is a clinical diagnosis, and diagnostic testing is not necessary.
URTI - basically strep throat from a abacterial point of view
What recommendations are provided for testing for influenza, and what specimens are considered optimal for different age groups?
Lecture Slide 15
When testing for influenza, obtain specimens as close to symptom onset as possible. Nasal aspirates and swabs are the best specimens to obtain when testing infants and young children. For older children and adults, swabs and aspirates from the nasopharynx are preferred.
URTI - basically strep throat from a abacterial point of view
What can be used to rule out bacterial pharyngitis?
Lecture Slide 15
Rapid strep swabs can be used to rule out bacterial pharyngitis, which could help decrease number of antibiotics being prescribed for these infections.

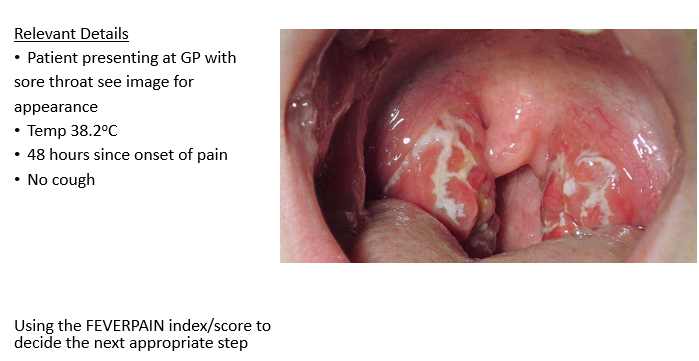
A patient is presenting at the GP with a sore throat, temperature of 38.2°C, 48 hours since onset of pain, and no cough. What could be the possible diagnosis or considerations?
Lecture Slide 16
The patient's symptoms suggest a possible upper respiratory infection. Further evaluation, including examination and possibly a rapid strep test, may be considered to determine if the sore throat is due to a bacterial infection, such as streptococcal pharyngitis. If bacterial, antibiotics may be prescribed. However, viral causes, such as the common cold or influenza, should also be considered, and symptomatic treatment may be recommended.
Most likely tonsilitis - bacterial infection - deviated uvula
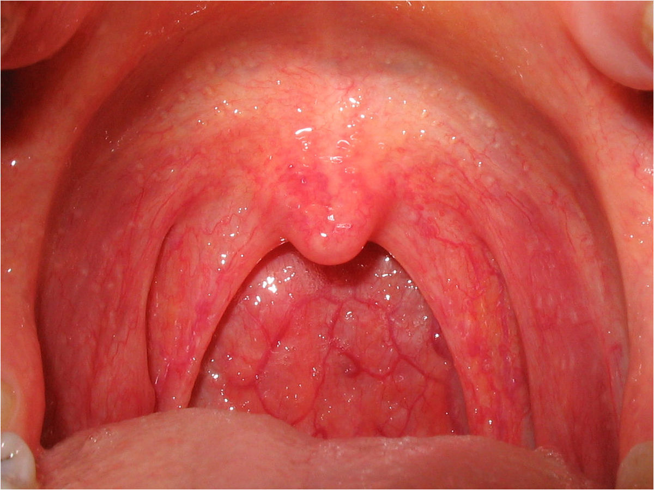
What could be the potential causes of a patient's symptoms, including a temperature of 37.8°C, 5 days since onset of pain, and a dry cough?
Lecture Slide 17
The symptoms, particularly the duration of pain, temperature elevation, and dry cough, may suggest a viral respiratory infection, such as the common cold or influenza.
Most likely viral - strep throat due to erythema (redness), uvula not deviated, no enlarged tonsils
What is the FEVERPAIN index/score
Lecture Slide 17
FEVERPAIN Index/Score:
Components: Fever, Purulence, Attend rapidly (within three days), Severe symptoms, Centor score (age-based).
Purpose: Assess severity of sore throat and guide antibiotic prescription decisions.
Categorization: Helps classify patients into low, intermediate, or high likelihood of Group A streptococcal infection.
Decision-Making: Influences the choice of prescribing antibiotics, with higher scores indicating a higher likelihood of bacterial infection.
Consideration: Clinical judgment should be exercised, and local guidelines may vary.
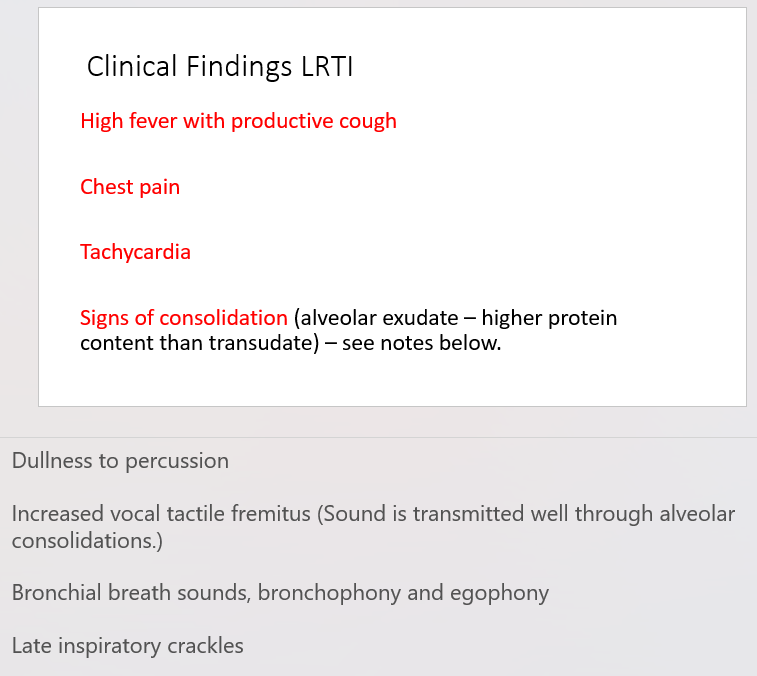
Clinical findings LRTI
State 4 clinical findings of lower respiratory tract infections.
Lecture Slide 18
High fever with productive cough
Chest pain
Tachycardia
Signs of consolidation (alveolar exudate – higher protein content than transudate) – see notes below.
Streptococcus pneumoniae (Gram-positive diplococcus)
What is the most common cause of Community-Acquired Pneumonia (CAP), and what is its major virulence factor?
Lecture Slide 19
Streptococcus pneumoniae is the most common cause of CAP. Its major virulence factor is the capsular polysaccharide, which provides protection against phagocytosis and drying.
Streptococcus pneumoniae (Gram-positive diplococcus)
Why is S. pneumoniae becoming relatively resistant to penicillin, and what is the recommended screening method for detecting this pathogen in CAP?
Lecture Slide 19
S. pneumoniae is becoming relatively resistant to penicillin, with a minimum inhibitory concentration (MIC) greater than 0.1 and less than 2.0 mgs/l becoming common. The recommended screening method for detecting S. pneumoniae in CAP is the urine antigen test, which serves as an excellent screening tool.
Streptococcus pneumoniae (Gram-positive diplococcus)
What clinical features are associated with S. pneumoniae-induced CAP, and what are some characteristic signs of this infection?
Lecture Slide 19
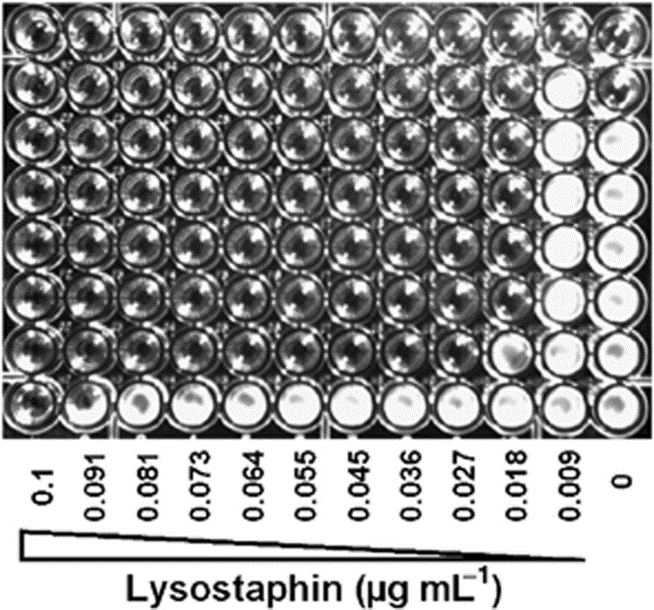
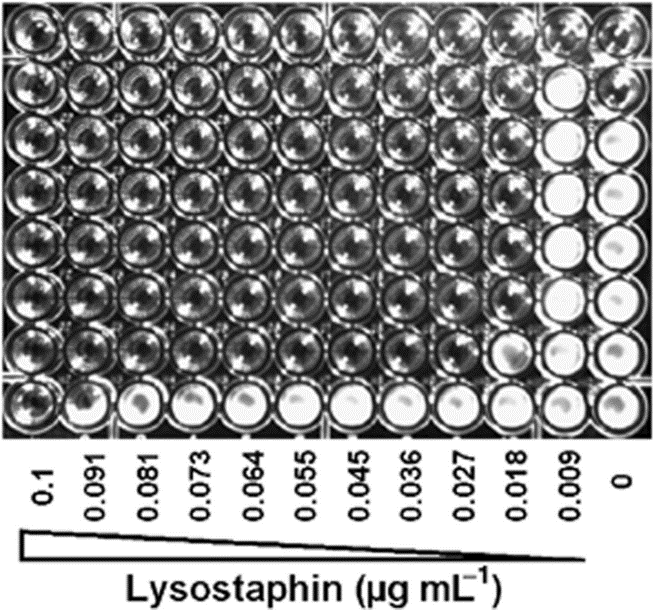
Antibiotic Susceptibility Testing
Describe antibiotic susceptibility testing.
Lecture Slide 20
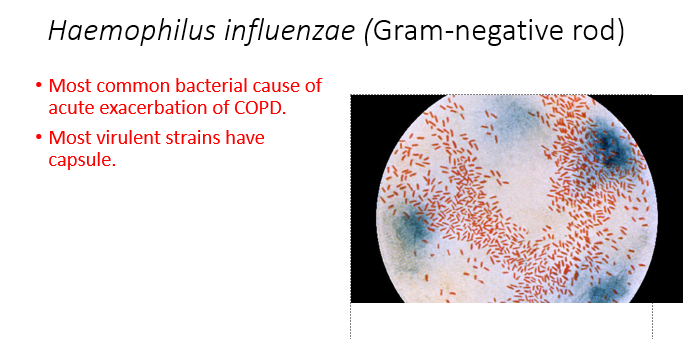
Haemophilus influenzae (Gram-negative rod)
What is the most common bacterial cause of acute exacerbation of Chronic Obstructive Pulmonary Disease (COPD), and what is a notable virulence factor associated with this bacterium?
Lecture Slide 21
Haemophilus influenzae, a Gram-negative rod, is the most common bacterial cause of acute exacerbation of COPD.
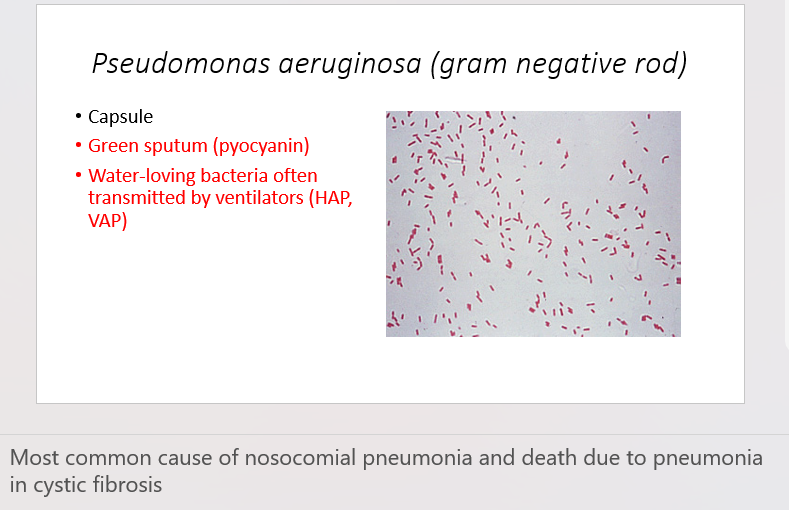
Pseudomonas aeruginosa (gram negative rod)
What are some characteristics of Pseudomonas aeruginosa, a Gram-negative rod, and what clinical features are associated with its infections?
Lecture Slide 22
Characteristics: Pseudomonas aeruginosa possesses a capsule.
Clinical Features: Infections with P. aeruginosa are often associated with the production of green sputum due to the presence of pyocyanin.
Transmission: This water-loving bacterium is frequently transmitted through ventilators, contributing to Hospital-Acquired Pneumonia (HAP) and Ventilator-Associated Pneumonia (VAP).
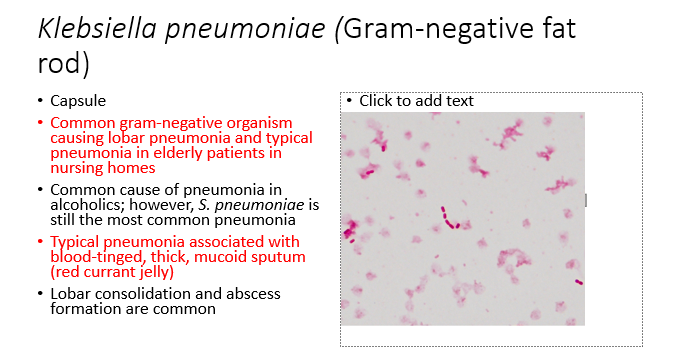
Klebsiella pneumoniae (Gram-negative fat rod)
What are the characteristics and clinical features associated with Klebsiella pneumoniae, a Gram-negative fat rod? (5)
Lecture Slide 23
Capsule
Common gram-negative organism causing lobar pneumonia and typical pneumonia in elderly patients in nursing homes
Common cause of pneumonia in alcoholics; however, S. pneumoniae is still the most common pneumonia
Typical pneumonia associated with blood-tinged, thick, mucoid sputum (red currant jelly)
Lobar consolidation and abscess formation are common
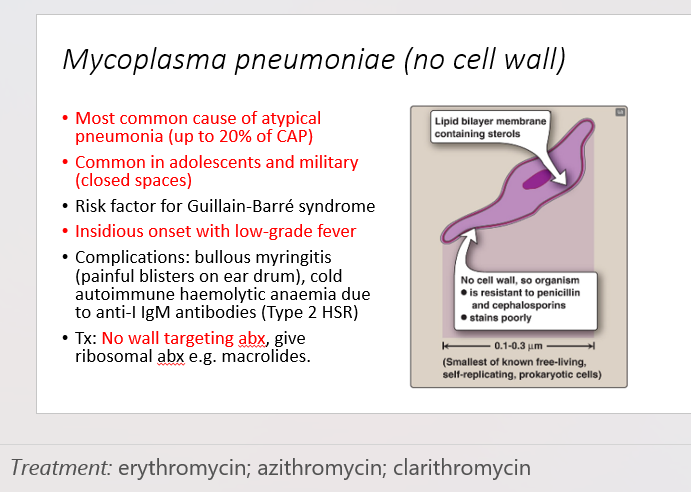
Mycoplasma pneumoniae (no cell wall)
What are the characteristics and clinical features associated with Mycoplasma pneumoniae, a bacterium lacking a cell wall? (6)
Lecture Slide 25
Most common cause of atypical pneumonia, accounting for up to 20% of Community-Acquired Pneumonia (CAP).
Common in adolescents and military populations, especially in closed spaces.
Associated with an increased risk of Guillain-Barré syndrome.
Presents with an insidious onset and low-grade fever.
Complications may include bullous myringitis (painful blisters on the ear drum) and cold autoimmune hemolytic anemia due to anti-I IgM antibodies (Type 2 Hypersensitivity Reaction).
Treatment: Antibiotics targeting the ribosome, such as macrolides, are preferred since Mycoplasma pneumoniae lacks a cell wall. Wall-targeting antibiotics are not effective.
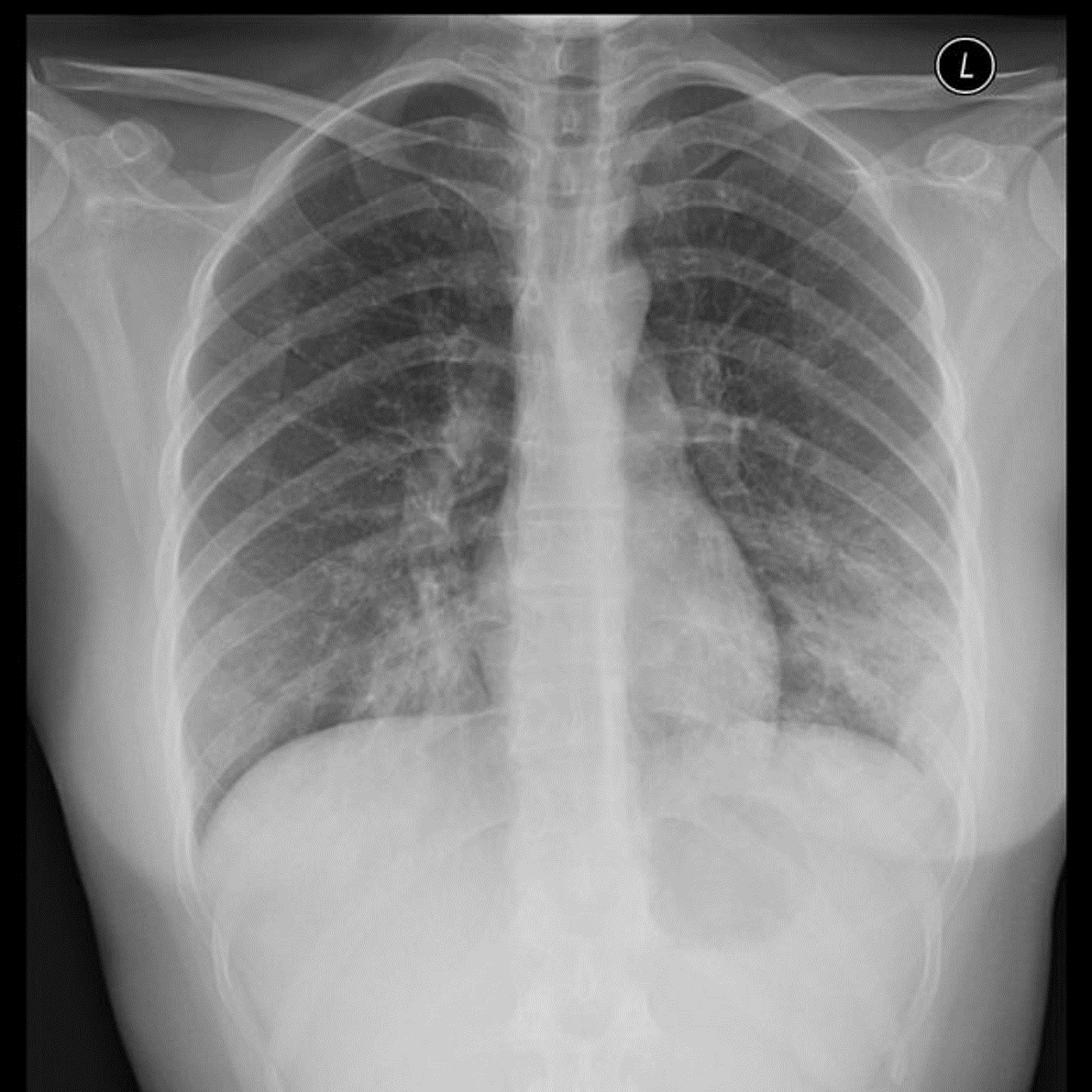
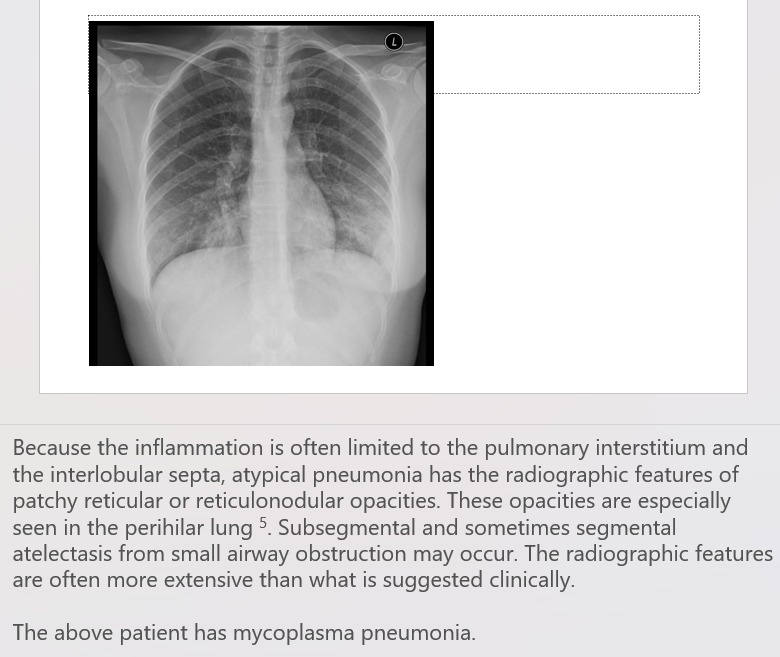
Can you provide labels, descriptions, and an explanation of the elements within this diagram, detailing what it represents or illustrates?
Lecture Slide 26
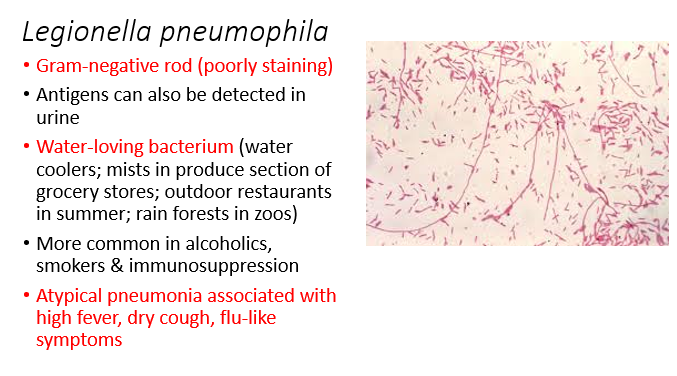
Legionella pneumophila
What are the characteristics and clinical features associated with Legionella pneumophila, a poorly staining Gram-negative rod? (6)
Lecture Slide 27
Legionella pneumophila is a Gram-negative rod that stains poorly.
Antigens can be detected in urine.
It is a water-loving bacterium found in various environments, including water coolers, mists in produce sections of grocery stores, outdoor restaurants in summer, and rainforests in zoos.
More common in alcoholics, smokers, and individuals with immunosuppression.
Atypical pneumonia is associated with high fever, dry cough, and flu-like symptoms.
Legionella pneumonia can cause severe respiratory illness and is a notable cause of community-acquired pneumonia, especially in certain environmental settings.
Nosocomial pneumonia (HAP) (after 48 hours post admission)
What are the key characteristics and factors associated with Nosocomial Pneumonia (Hospital-Acquired Pneumonia - HAP), including Ventilator-Associated Pneumonia (VAP)? (4)
Lecture Slide 28
Nosocomial pneumonia occurs after 48 hours post-admission, with VAP commonly associated with ventilators and intubation.
Opportunistic infections are prevalent in patients with severe underlying diseases.
Antibiotic therapy and immunosuppression are common risk factors.
Pathogens commonly implicated in nosocomial pneumonia include Pseudomonas, E. coli, and Gram-positive bacteria such as Staphylococcus aureus.
Management pneumonia (CAP)
What are the key steps in the management of Community-Acquired Pneumonia (CAP) in general practice, and when should a referral be considered? (6)
Lecture Slide 30
Most managed in general practice, refer if
Symptoms and signs suggest a more serious illness or condition (for example cardiorespiratory failure or sepsis), or
Symptoms are not improving as expected with antibiotics.
Other things to consider, there is bacterial resistance to oral antibiotics, or the person is unable to take oral medication.
Consider referring young people with community-acquired pneumonia to hospital, or seek specialist paediatric advice on further investigation and management.
Confirm diagnosis & aetiological agent (aim is to give specific therapy)
CXR, Culture and stain (moderate, and severe)
Assess severity of disease, (Correction of respiratory failure, Correction of haemodynamic compromise.)
Identify complications
Severity of CAP - Criteria CURB-65
What is the CURB-65 criteria used for assessing the severity of Community-Acquired Pneumonia (CAP), and what are the individual criteria, each contributing to a score of 1 if positive? (6)
Lecture Slide 31
Each one if positive gives you score of 1.
Confusion (mini-mental test score of 8 or less) – or confused to time, place etc.
Urea > 7 mmol/l
Respiratory rate > 30 per minute
Blood pressure: systolic BP < 90 mmHg or diastolic BP < 60 mm Hg
65 or more years old
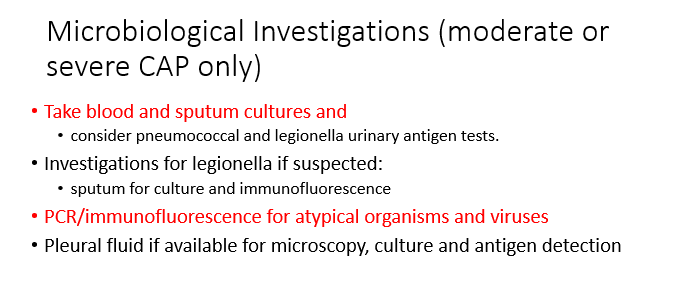
Microbiological investigations (moderate or severe CAP only)
What are the recommended microbiological investigations for moderate or severe Community-Acquired Pneumonia (CAP), and what specific tests should be considered for Legionella if suspected? (4)
Lecture Slide 32
Take blood and sputum cultures and
consider pneumococcal and legionella urinary antigen tests.
Investigations for legionella if suspected:
sputum for culture and immunofluorescence
PCR/immunofluorescence for atypical organisms and viruses
Pleural fluid if available for microscopy, culture and antigen detection
List predisposing factors to recurrent infection of the lung (chronic bronchitis, cystic fibrosis, COPD) and outline the profile of organisms involved.
What is the most common cause of a COPD acute exacerbation?
Lecture Slide 33
Haemophilus influenzae
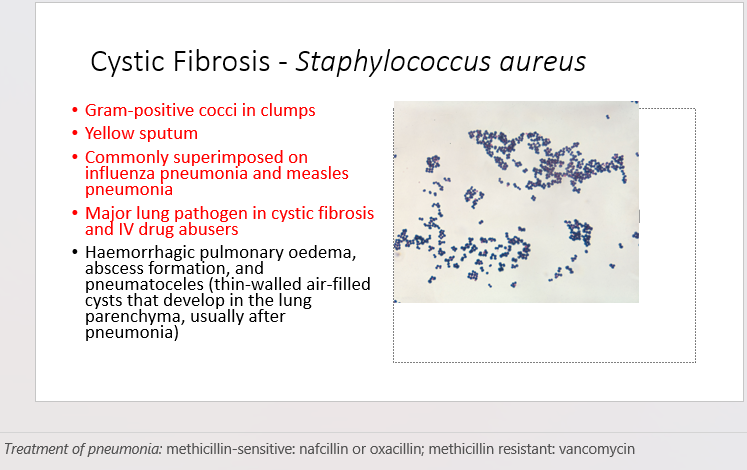
Cystic Fibrosis - Staphylococcus aureus
What are the characteristics and clinical features associated with Staphylococcus aureus in the context of Cystic Fibrosis? (5)
Lecture Slide 34
Gram-positive cocci in clumps
Yellow sputum
Commonly superimposed on influenza pneumonia and measles pneumonia
Major lung pathogen in cystic fibrosis and IV drug abusers
may lead to complications such as haemorrhagic pulmonary oedema, abscess formation, and pneumatoceles (thin-walled air-filled cysts that develop in the lung parenchyma, usually after pneumonia)
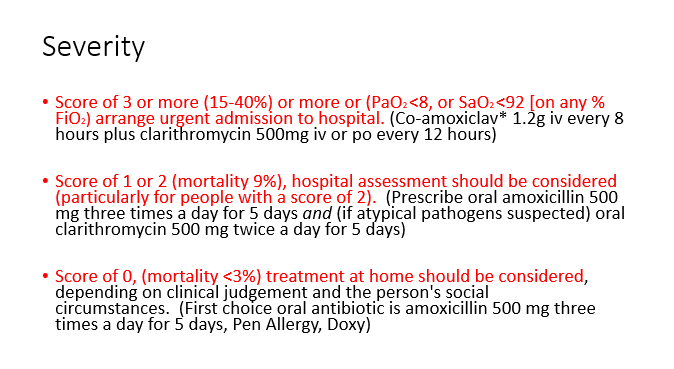
Severity
How is the severity of Community-Acquired Pneumonia (CAP) assessed, and what are the recommended management approaches based on severity scores?
Lecture Slide 36
Score of 3 or more (15-40%) or more or (PaO2 <8, or SaO2 <92 [on any % FiO2) arrange urgent admission to hospital. (Co-amoxiclav* 1.2g iv every 8 hours plus clarithromycin 500mg iv or po every 12 hours)
Score of 1 or 2 (mortality 9%), hospital assessment should be considered (particularly for people with a score of 2). (Prescribe oral amoxicillin 500 mg three times a day for 5 days and (if atypical pathogens suspected) oral clarithromycin 500 mg twice a day for 5 days)
Score of 0, (mortality <3%) treatment at home should be considered, depending on clinical judgement and the person's social circumstances. (First choice oral antibiotic is amoxicillin 500 mg three times a day for 5 days, Pen Allergy, Doxy)