UKMLA: Rheumatology
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
33 Terms
AS: What is the epidemiology?
There is a peak in onset between the ages of 20 to 30 years
It is twice as common in men than women (with higher rates of HLA-B27 positivity in men)
It is strongly heritable
AS: What are the symptoms?
Lower back and buttock pain
Pain elsewhere in the spine may also occur
Stiffness that is worse in the morning and with rest, and improves with activity
Patients may wake in the second half of the night with pain
Pain and stiffness respond to NSAIDs
AS: What is schober’s test?
Mark two points on the back (one at the level of the L5 spinous process and one 10 cm above this)
On forward flexion, the distance between the two points should increase by 5cm or more
If the increase in distance is <5 cm, this indicates restricted forward flexion
AS: What is the typical x-ray finding?
Pelvic x-ray→ sacroiliitis
‘Bamboo’ spine appearance
AS: What is the management?
NSAIDS with PPI to prevent peptic ulcers
Paracetamol ± codeine
-mab biologics
Surgery
Gout: What is it?
Gout is a form of arthritis that occurs when monosodium urate crystals deposit in joints
Gout: What are the different types?
Acute→ within 24 hours and very painful
Tophaceous→ chronic but painless
Gout: What is the gold standard investigation?
Joint aspiration→ needle shaped monosodium urate crystals with negative birefringence
Gout: What are some additional investigations?
Urate levels→ over 360
Repeat urate levels within 2-4 weeks of flare
HLA-B5801 screening for East Asians before starting allopurinol
Gout: What is the management?
NSAIDS at maximum dose
Colchicine
Prednisolone
Gout: Which drugs are used for prevention via urate-lowering therapy?
ULT:
Allopurinol (check HLA-B5801 in East Asians first before starting!!)
Uricosuric drugs
OA: What is the epidemiology?
More women than men are affected
Average age of onset is 55
The commonest joint affected is the knee, followed by the hip then the hand
OA: What are the symptoms?
Pain in the affected joint exacerbated by use
Crepitus→ friction between bone and cartilage
Limping/antalgic giant
Herberdens nodes on DIP
Bouchards nodes on PIP

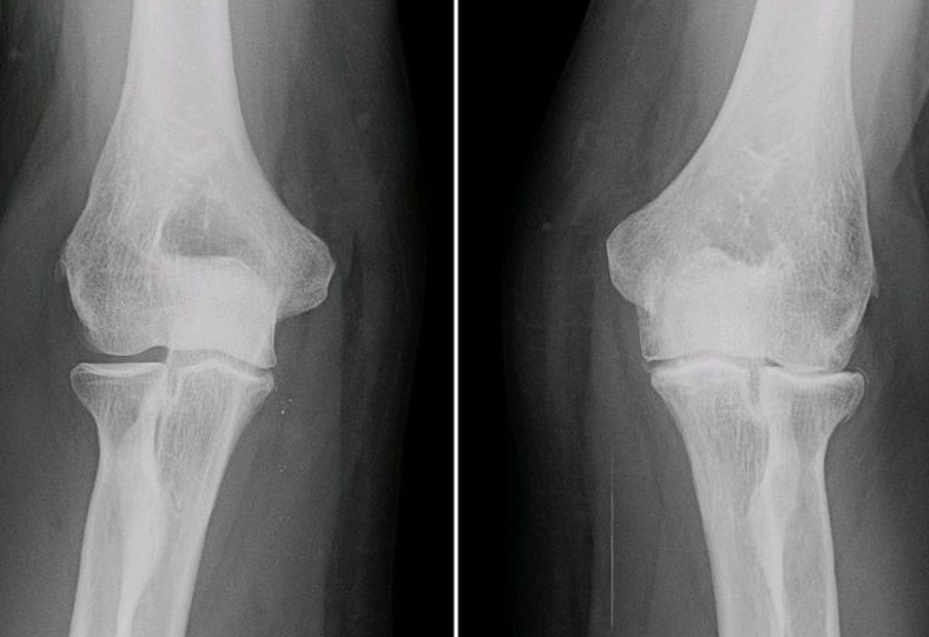
OA: What are the typical findings on x-ray?
Typical findings can be remembered with the mnemonic "LOSS":
Loss or narrowing of joint space due to thinning of cartilage
Osteophytes i.e. formation of new bony spurs at the joint margins
Subchondral sclerosis i.e. increased bone density beneath the cartilage
Subchondral cysts which are fluid-filled sacs in the subchondral bone
OA: What is the management?
Conservative
Topical NSAIDS and analgesia
Topical capsaicin for knee OA
Steroid injections
Arthroplasty surgery (joint replacement)
RA: What is the epidemiology?
The majority of patients are female (3:1 ratio)
Onset peaks between 30-50 years old
Smoking is a risk factor and worsens the symptoms
RA: What are the symptoms and signs?
Ulnar deviation
Swan neck deformity
Pain which improves with movement
Prolonged early morning stiffness (over an hour)
RA: What are the investigations?
Rheumatoid factor positive
Anti-CCP antibodies positive
Joint aspiration with synovial fluid analysis to rule out septic arthritis
RA: What is the management?
Conservative:
Urgent referral to rheumatology
Education and self-management
Regular monitoring using DAS28 score
Medical:
Analgesia: paracetamol, NSAIDs
cDMARDs (e.g. methotrexate) as first-line treatment
Escalate dose or add another DMARD if needed
Disease-modifying antirheumatic drugs (DMARDs) are first-line → METHOTREXATE
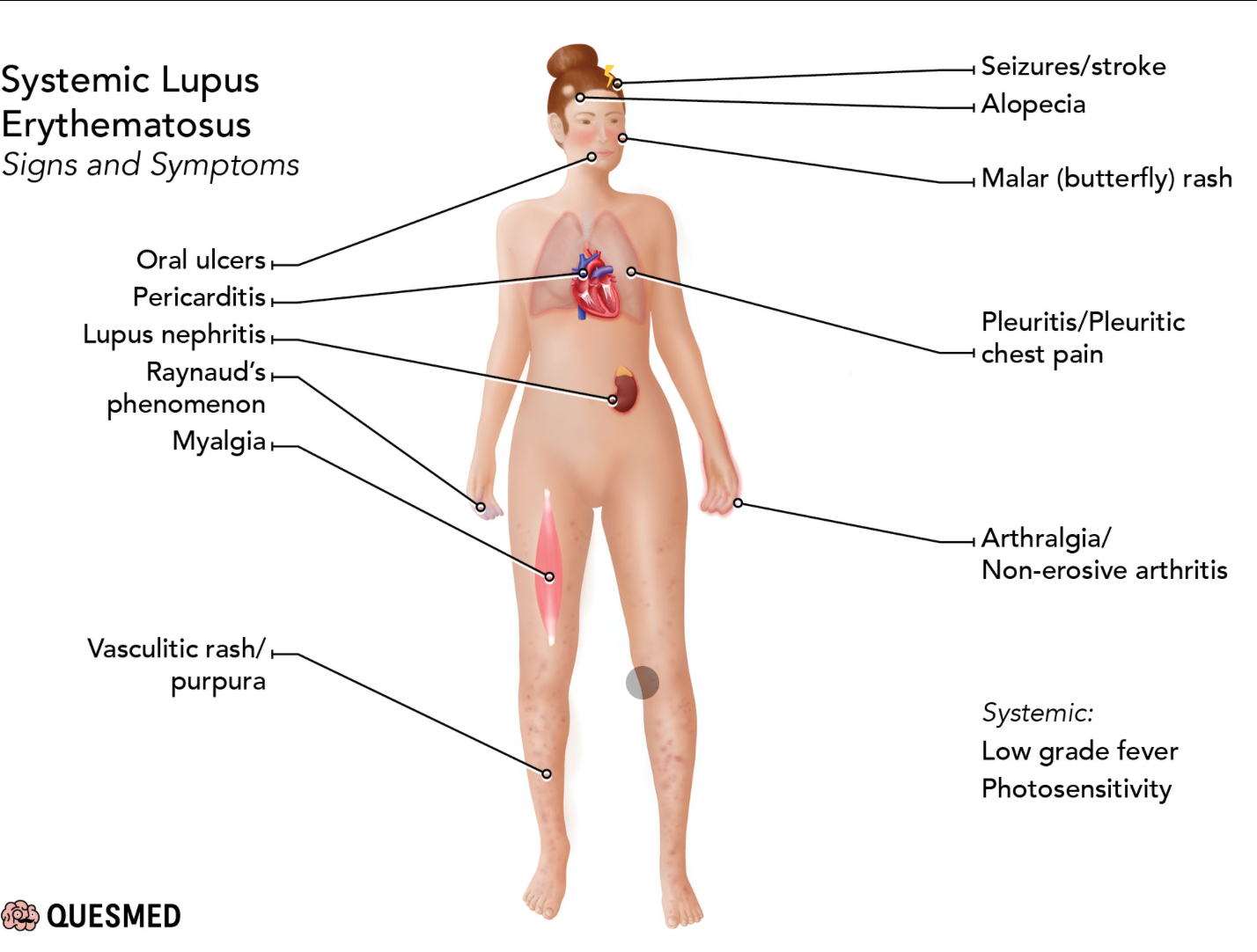
SLE: What is it?
A complex autoimmune disease that may affect a wide variety of organs
SLE: What is the epidemiology?
SLE is nine times more common in women than men
It is most common in people of Afro-Caribbean and South Asian descent
Mean age at diagnosis is 49 years
SLE: What are the risk factors?
Smoking
Ultraviolet light
Silica exposure
Epstein-Barr virus
COCP
Infection
Stress
SLE: What are the general symptoms?
Systemic - fevers, fatigue, weight loss, myalgia, malaise, mouth ulcers
Dermatological - photosensitivity, malar rash, discoid rash, livedo reticularis, alopecia, Raynaud's phenomenon, cutaneous vasculitis
Rash is usually photosensitive aka gets worse in sunlight

SLE: What are the systemic symptoms?
SLE: Which antibodies are specific markers for SLE diagnosis?
Anti-double stranded DNA (anti-dsDNA)
SLE: Why is urinanalysis so important?
To look for proteinuria→ evidence of lupus induced glomerulonephritis
SLE: What is the management?
Hydroxychloroquine for all patients
Steroids (oral prednisolone, IV methylprednisolone for acute cases)
Steroid-sparing agents → cyclophosphamide (methotrexate, azathioprine)
Biologics (belimumab, rituximab) for severe/refractory cases
SLE: What is the management of neuropsychiatric symptoms e.g. headaches and psychosis due to SLE?
High-dose steroids and cyclophosphamide
SLE: How can you differentiate between SLE and drug-induced lupus?
Drug-induced lupus:
Black people
Butterfly rash is not so common
Positive anti-histone antibodies
Typically induced by use of hydralazine or isoniazid (first line TB treatment which taken for 6 months)
SLE:
Black people
Butterfly rash is more common
Positive anti-dsDNA and anti-smith antibodies
SLE: Use of which drug can cause neutrophilia?
Steroids!!
SLE: What is the complication of SLE in pregnant women?
May cause congenital heart block leading to foetal bradycardia during second trimester
SLE: What are the expected blood findings?
Low C3 + C4
High ESR
Anti-dsDNA antibody positive
High creatinine
SLE: How do you differentiate between Sjrogen syndrome, dermatomyositis and SLE?
Sjrogen syndrome→ Anti-ro antibodies
Dermatomyositis→ anti-jo antibodies + non-photosensitive facial rash