microbiology final exam week 2
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
upper respiratory system (head and neck)
common but usually not life-threatening
viral or bacterial
immune system clears in about a week
lower respiratory system (chest)(lungs)
often serious and may be fatal
viral, bacterial, fungal
sinusitis
inflammation with the sinuses (upper resp)
pharyngitis
inflammation of the throat (upper resp)
rhinitis
inflammation of the mucous membranes of nose (upper resp)
tonsilitis
inflammation of the tonsils (upper resp)
ottis media
inflammation of the middle ear
what does the upper respiratory tract do? (function?)
warms and moisturizes inhaled air
protective mechanisms of the upper respiratory tract?
nasal hairs (catch particles)
lysozyme
igA
saliva flushing
coughing, sneezing, swallowing
continuous sloughing of epithelium
normal microbiota
mucous and cilia (MUCOCILIARY ESCALATOR!)
normal microbiota of the upper resp tract or pathogen?
strains can be protective OR pathogenic or commensal depending on strain
moraxella
gram negative diplococci and diplobacilli
ottis media
haemophilus
small gram negative rods
meningitis
streptococcus
gram positive cocci in chains
10% strep pyogenes
corynebacterium
pleomorphic, gram positive rods; non-motile non spore forming
diptheria
staphylococcus
gram positive cocci in clusters
25% staph aureus
what causes fever, throat pain, and difficulty swallowing?
pharyngitis (inflammation of the throat)
caused by streptococcus pyogenes (treatment is penicillin or amoxicillin)
streptococcus pyogenes
gram positive
cocci that grow in chains
encapsulated
NON MOTILE
group A carbohydrate
B hemolytic
“pyo" (pus)
causes strep throat (makes us sick)

what are the steps in the pathogenesis of infectious disease?
entry
attachment (M protein, F protein)
multiplication
invasion or spread (tissue degrading enzymes)
evasion of host defenses
damage to host tissues
what are the evasion of host defenses in pathogenesis of infectious disease?
M protein
streptolycin (leukocytes lyses or breaks open your immune cells)
protein G (binds to antibodies)
capsule (evade phagocytosis)
C5a peptidase (avoiding of complement)
lysogenic phages encode what?
toxins in some strains
what are toxins?
superantigens
lead to… massive activation of T cells (MASSIVE INFLAMMATORY RESPONSE)
scarlet fever
toxic shock
necrotizing fasciitis (“flesh eating disease”)
why can you get strep throat (pharyngitis) more than once?
we do not have a vaccine yet
>80 types (antigenic variants) of M protein
too many types to make a vaccine
epidemiology of streptococcus pyogenes
naturally only infects humans
spread by respiratory droplets or contaminated food
treatment and prevention of streptococcus pyogenes
confirmation via diagnostic tests (rapid strep elisa) and throat culture
treatment with penicillin and erythromycin about 90% effective
prevents post streptococcal sequelae
why is it important to treat strep throat?
can lead to post-streptococcal sequelae (complications that happen after strep is gone)
post streptococcal sequelae
acute rheumatic fever (3%) → can lead to chronic rheumatic heart disease because antibodies to M protein cross react w/proteins on the HEART
acute post-streptococcal glomerulonephritis
antibody-antibody complexes activate complement → damages kidneys (rare)
(both sequelae are strain dependent!)
what is another bacterial pharyngitis?
diptheria
caused by corynebacterium diphtheriae (do not leave throat BUT toxins circulate)
strains carrying lysogenic phage produce toxin that can circulate in blood → shuts down protein synthesis in heart, kidneys, and nerves (damage!)
how do you prevent diptheria?
effective toxoid vaccine (DTaP)
humans are the only reservoir
common cold causes
mainly rhinoviruses (>100 types)
infect respiratory epithelial cells → stop ciliary motion (more susceptible to 2ndary infection!)
average adult gets 2-4 colds each year, kids get 2x that number!
characteristics of the common cold
short incubation period (1-2 days)
non-enveloped (common, persist, resist dessication, stable)
usually no fever
first 2-3 days: nasal secretions contains high numbers virus
portals of entry: eyes and nose
prevention: wash hands, keep away from face, avoid crowds
treatment: symptoms only: aspirin and ibuprofen may prolong duration
viral pharyngitis
adenoviruses most common (>50 types)
LONGER INCUBATION PERIOD (5-10 days)
can also infect other tissues (eg. conjunctivitis)
NON ENVELOPED, can remain infectious for long periods of time
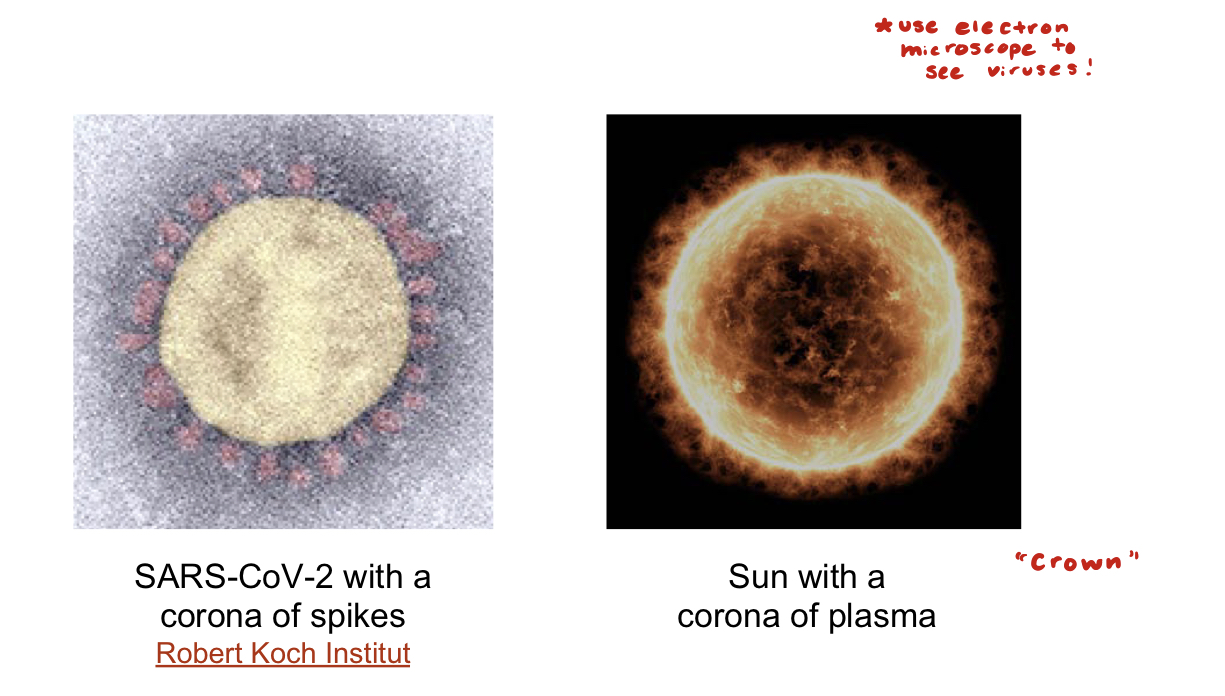
corona virus
upper respiratory viral infection
many types
cause 10-30% common colds
can spread to lower resp tract
fairly high mortality rate
ANIMAL RESERVOIR (bats!)
what are the deadly coronaviruses?
SARS (sudden acute respiratory syndrome)
bats, cirets, high mortality rate
MERS (middle east respiratory syndrome)
bats, camels, high mortality rate
upper respiratory infections can spread to?
sinuses, middle ear, and lower resp system (bronchitis, pneumonia)
causative agents of lower respiratory infections?
bacteria
viruses
fungi
infections of the lower respiratory tract?
bronchitis (infections of bronchi, larger airways)
bronchiolitis (infection of smallest airways)
pneumonia (alveoli filled w/fluid and pus)
pneumonia can spread to?
CNS (meningitis)
heart (endocarditis)
blood (sepsis)
pneumonia can result from?
inhalation of pathogen
spread from upper respiratory infection)
aspiration of foreign material
periodontal disease
blood infection
how can a lung infection spread?
short distance for bacteria to travel from blood into lungs or vice versa
protective mechanisms of the lower respiratory tract?
mucociliary escalator present in trachea, bronchi, and bronchioles
few normal microbiota
macrophages waiting in alveoli are able to phagocytize and get rid of foreign material
streptococcus pneumoniae
most common cause of community acquired pneumonia
~60% hospitalizations
30% indiv carry encapsulated s.pneumoniae (dont develop disease)
symptoms of s.pneumoniae infection
fever
cough
chest pain
productive cough
shallow and rapid breathing
fatigue
(because of small air sacs filled w/fluid from inflammatory response)
treatment for s.pneumoniae infection
antibiotics but resistance is rising
who should get vaccinated for s.pneumoniae?
children (under 5)
anybody 65+
>90 different capsular serotypes; vaccines contain COMBINATIONS (w/capsular fragments from many serotypes)
klebsiella pneumoniae
soil organism
often a HAI
damages lung tissue
high mortality rate
antibiotic resistance (eg. carpenum resistant entobacteriaceae) to almost all antibiotics
cough up red currant jelly

mycoplasma pneumoniae
“walking pneumonia”
generally mild
small infectious dose (droplets)
patient infectious for many weeks
treatable, NO CELL WALL (so you could NOT treat with beta lactam…)

bordetella pertussis
very rare in US
characterized by violent coughing (whooping cough)
bronchioles blocked
PREVENTED BY DPT OR DTaP VACCINATION
legionella pneumophila
causes legionnaire’s disease in compromised hosts
vulnerable are those really young and over 65+ (DEPEND ON HERD IMMUNITY!)
ubiquitious, found in nature and ponds
what is one of the world’s deadliest diseases?
tuberculosis
1/3 of the world’s population is infected
4,000 people die each day
active TB has a high mortality rate
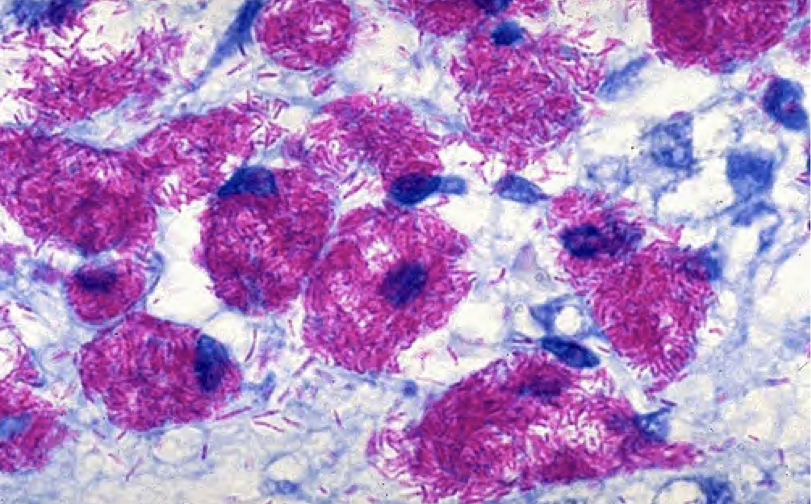
cause of tuberculosis
mycobacterium tuberculosis
aerobic
rod shaped
acid fast streptobacillus (doesn’t stain well in gram stain, very THICK mycolic acid well wall
transmission of tuberculosis
humans are reservoir
airborne
droplet spread
quite resistant to drying, antibiotics, and disinfectants
pathogenesis of tuberculosis
entry: inhalation of airborne particles or droplets carrying bacteria
attachment: binds to alveolar macrophages
avoiding host defenses: phagocytosed by alveolar macrophages but PREVENTS FUSION OF LYSOSOMES WITH PHAGOSOME
damage: infected macrophages lyse inducing inflammation; tubercles (granulomas) can block alveoli and bronchioles. the bacteria can sometimes spread to other organs like kidney, brain, spinal cord, bone, or skin…
facultative intracellular pathogen
mycobacterium tuberculosis has acid fast cell wall
resist digestion
bacteria can multiply within human macrophage cells (use it as host)
thick waxy wall prevents many antibiotics and disinfectants from entering bacterium; resist desiccation
droplet transmission
5 minutes of talking generates 3000 droplet nuclei
latent infection tuberculosis
90-95% infected individuals
no symptoms
non infectious
usually positive skin test
chest x ray and sputum normal
active infection tuberculosis
5-10% infected individuals
symptoms
infectious to others
positive skin test
chest x ray may be abnormal
positive sputum sample
can spread BEYOND LUNGS
result of active TB disease?
lungs damaged
slight fever
decreasing weight loss
persistent cough (bloody sputum)
night sweats
can spread → military TB (problem for children!)
patients with latent tuberculosis do not have symptoms but are treated with antibiotics, why?
reactivation of tuberculosis
infects CD4 pos cells (T helper cells)
levels get low
not able to keep TB infection in check
diagnosis for tuberculosis
tuberculin skin test (mantoux)
x ray
sputum culture
blood tests for interferon
treatment for tuberculosis?
3-4 drugs given in combination for many months
wanna know if person with TB has significant number of resistance organisms (for someone with active TB!)
DOTS (directly observed therapy short course)
for those not able to regularly get medication
multiple drug resistant TB
resistance to rifampin and isoniazid
russia and soviet union
extensively drug resistant (mycobacteria XDR: resistant to all 1st line drugs and many 2nd line drugs)
why doesn’t everybody receive the TB attenuated vaccine (BCG)?
prevents childhood TB but not latent tuberculosis later in life
vaccinated individuals test positive on skin test (disadvantage for false positive tests in future)
the majority of upper respiratory infections are caused by?
viruses
what is the key reason there is no effective vaccine against streptococcus pyogenes?
the number of antigenic variants (more than 80 types of M proteins!)
true or false, most people infected with M.tuberculosis develop active TB?
false (only 5-10%)
some people with latent infections will go on to develop active TB if they become immunocompromised (ex: co infected with HIV)
mycobacterium can evade the host immune system by:
producing a large capsule
moving with flagella
reproducing inside macrophages
expressing different M proteins
reproducing inside macrophages
SARS-CoV2
a corona virus
several types of coronavirus infect humans: (4) cause a common cold, or severe symptoms (2, SARS and MERS)
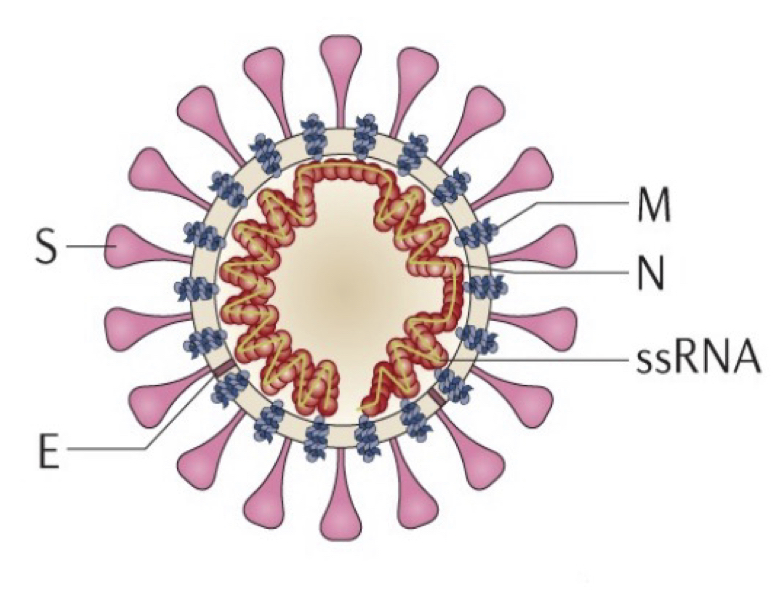
structure of SARS-CoV-2?
RNA virus
4 structural proteins
1 single stranded viral RNA (ssRNA)
membrane ENVELOPED (lipid bilayer comes from host cell membrane)
the spikes (S) bind to HOST RECEPTORS (attachment!)
why are enveloped viruses easier to inactivate?
more delicate than non enveloped
don’t survive as long outside of host
more likely to be inactivated by hand sanitizer!
what does SARS-CoV-2 attach to?
ACE2 (angiotensin converting enzyme 2)
host receptor that is found on the surface of many cell types
(COVID-19 (illness) is caused by SARS-CoV-2!
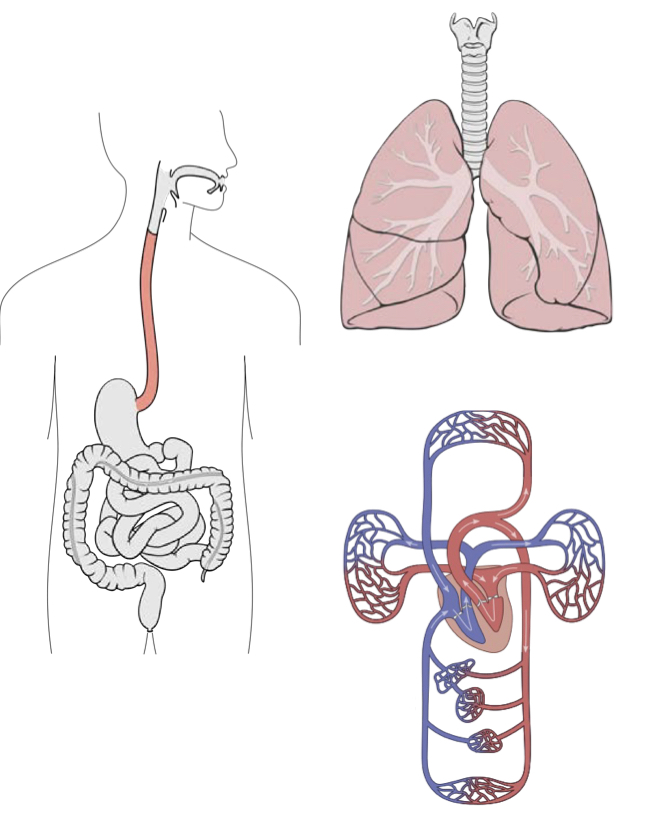
why does COVID-19 affect multiple areas of the body
because Ace2 receptors are found in so many areas of the body
throughout respiratory tract (sore throat)
GI tract
epithelial cells of veins and arteries (cardio and neurological symptoms)
and more…
what is the updated COVID-19 vaccine?
bivalent, it targets the ORIGINAL SARS-CoV2 strain (Wuhan) AND OMICRON VARIANTS BA.4/BA.5
made by pfizer and moderna
BOTH ARE mRNA VACCINES
contan SPIKE mRNA ENCLOSED IN A LIPID SHELL
all persons 6 months and older should get at least one dose of the UPDATED BIVALENT vaccine (targets spike protein from 2 strains)
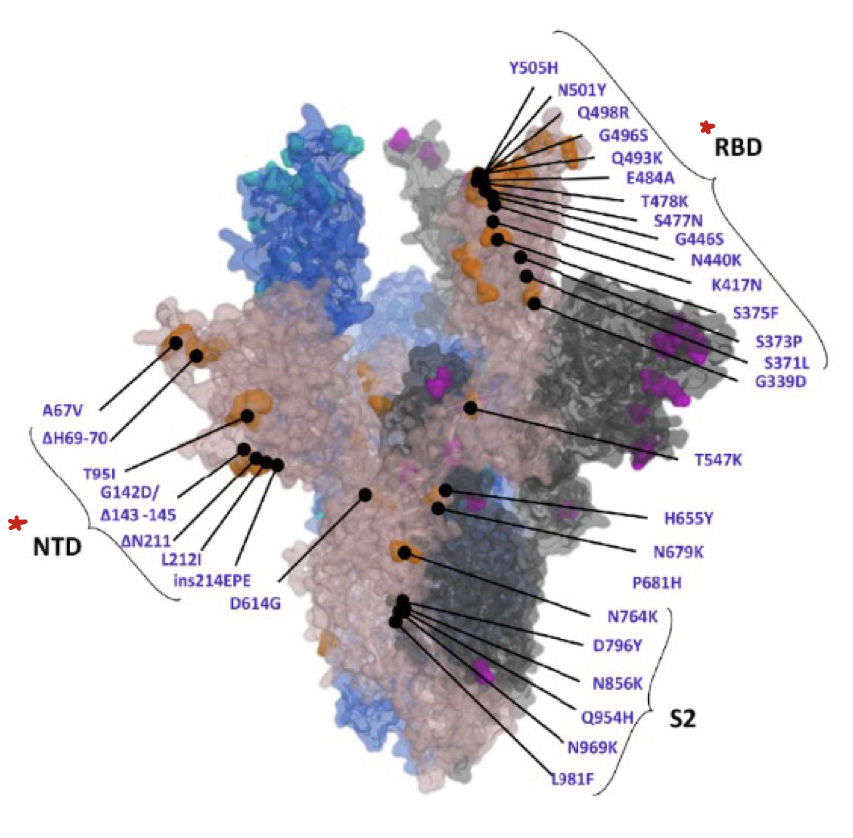
why do we need updated vaccines?
spike protein of the omicron variant:
32 mutations shown
protective antibodies bind to the N-terminal domain (NTD) (prevent virus from successfully infecting the cells!)
receptor binding domain (RBD) binds to the host ACE2 receptor
some mutations affect how well the spike protein binds to the ace-2 receptor…
what species does SARS-CoV2 infect?
it is ZOONOTIC (animal reservoir, animals → humans)
more species likely to infect:
binturoung
cat
coatmundi
deer
dog
ferret
fishing cat
gorilla
etc…
in the US, what animal is a reservoir for SARS-CoV2?
white tailed deer
new variants and mutants spread within deers that could spill over to humans
how could covid 19 be treated? (which drugs interfere with viral replication?)
remdesivir
paxlovid
block viral replication without harming host cells because remdesivir is selectively toxic for viral RNA polymerase humans dont have and paxlovid viral protease…
remdesivir
blocks RNA dependent RNA polymerase
needs this bc RNA virus (RNA dependent)
human cells dont have this
paxlovid
blocks viral protease → necessary for viral replication
effective if given at beginning of covid infection
influenza virus
A, B, C, and D types
A causes the MOST SEVERE DISEASE IN HUMANS
A INFECTS MULTIPLE SPECIES
flu vaccines contain which strains of influenza?
A and B
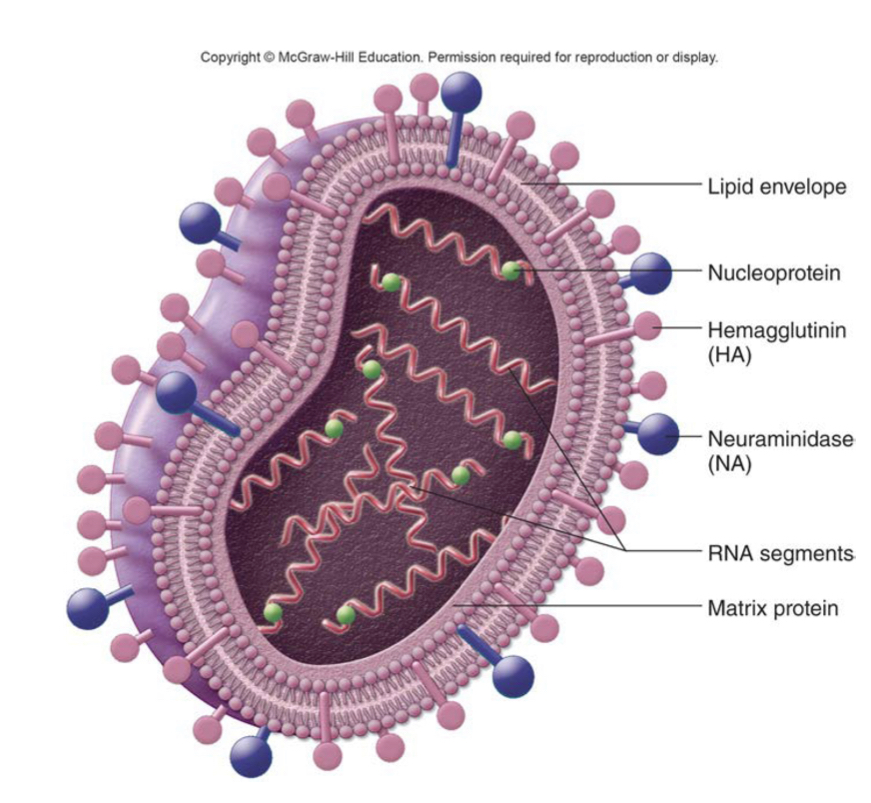
what type of virus is influenza?
RNA virus
enveloped
4 structural proteins
8 single stranded RNA (ssRNA)(allows to mutate more dramatically)
membrane envelope
the spikes (hemagglutinin) BIND TO HOST RECEPTORS
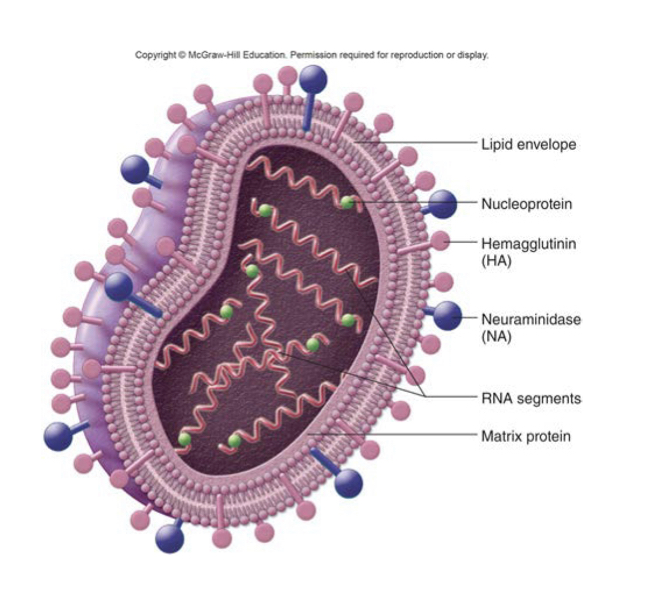
how are flu strains named?
by the types of HA and NA proteins that are present
18 types HA
11 types NA (neuraminidase: protein required for viral exit from the cell)
humans are infected by which strains of HA and NA?
HA (hemogluttenin) 1,2 and 3
NA 1 and 2
ex: 2009 swine flu (infected humans) was H1N1
2015 avian flu (mainly infected birds) was H5N2
what are flu symptoms and treatment?
“FACTS”
F: fever
A: aches
C: chills
T: tiredness
S: sudden onset
drug tamiflu (neuraminidase inhibitor) can be used but only EARLY IN THE INFECTION
what is in the flu vaccine?
quadrivalent contains
influenza A (H1N1, N3N2) and 2 strains of influenza B
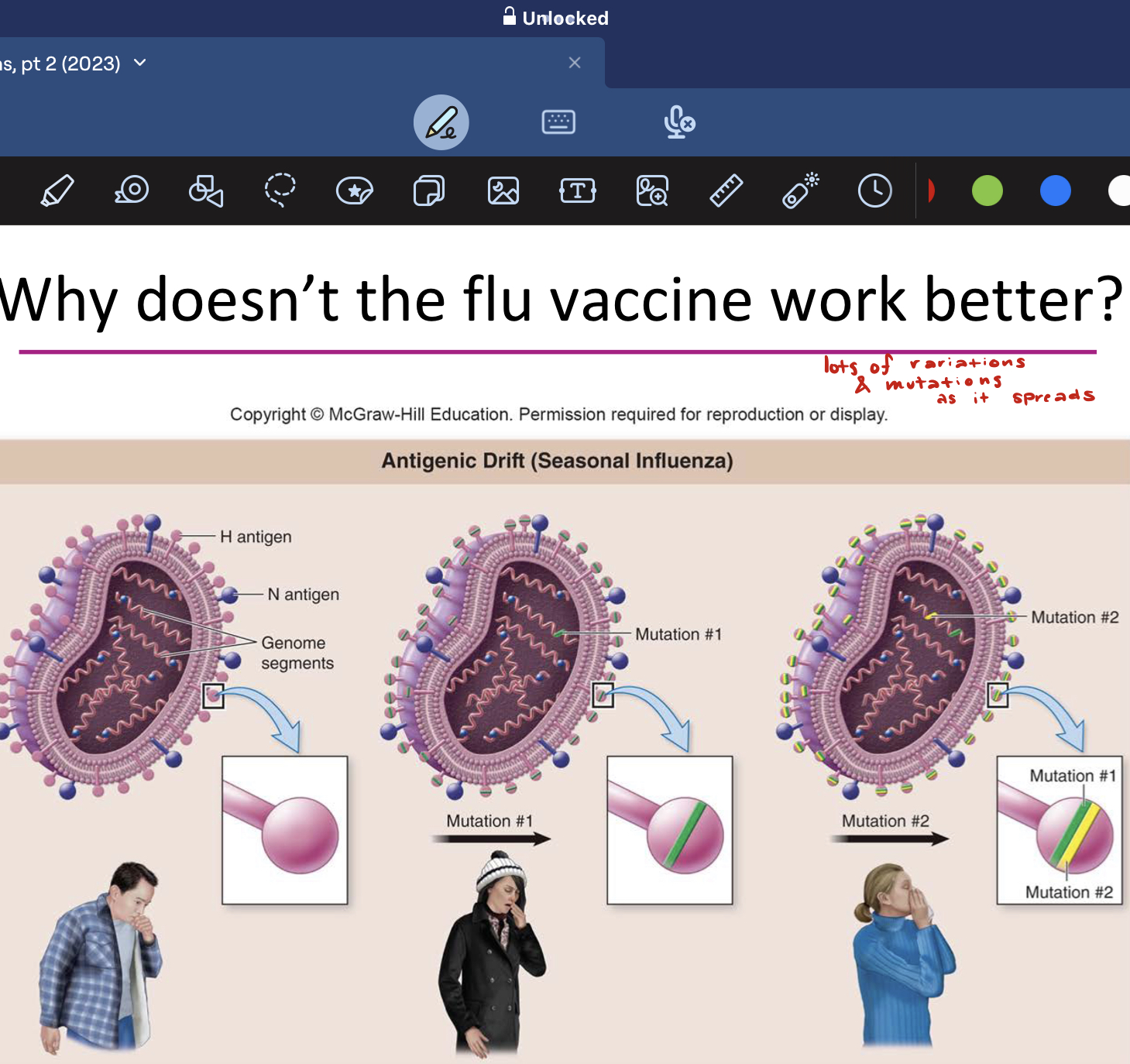
why doesn’t the flu vaccine work better?
lots of variations and mutations as it spreads
egg adapted strains contain mutations (virus grown in egg embryos)
who gets vaccinated for flu vaccine?
80-90% should be vaccinated to achieve herd immunity
unless immunocompromised or very young and eldery
depend on herd immunity!
how does flu vaccination affect antibiotic resistance
reduces spread of antibiotic resistance
less clinic visits, less antibiotics prescribed inappropriately
prevented 3.7 million office visits!
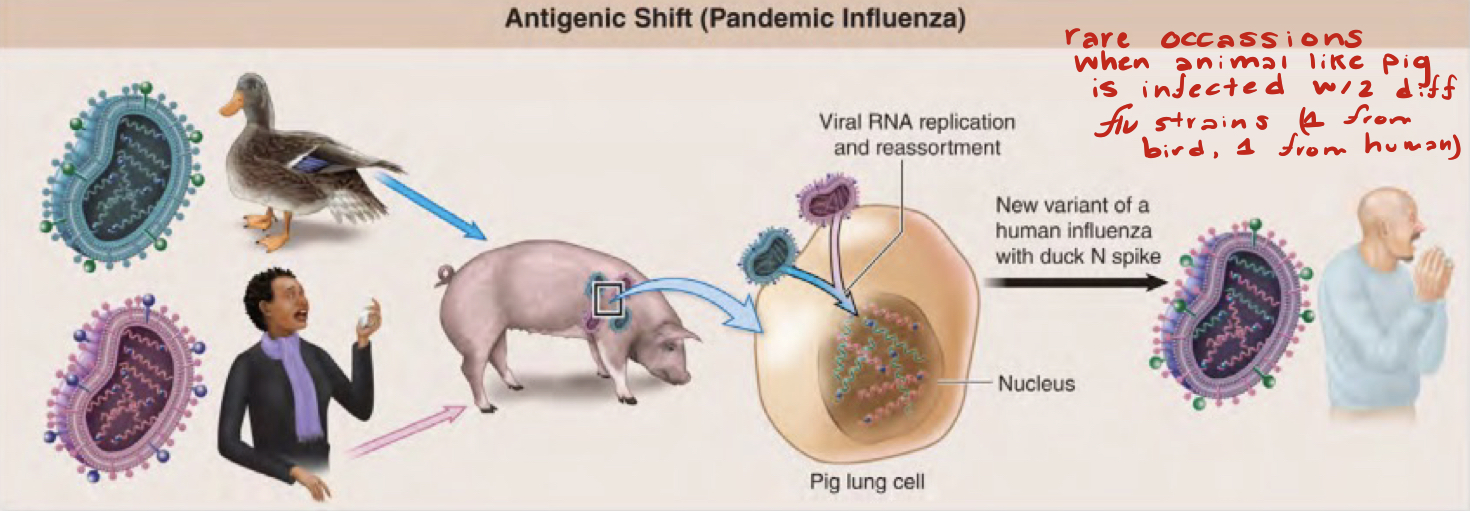
how do pandemic strains arise?
new strain could have N and HA spikes that recognize human receptors (zoonotic!)
rare occassions when animal like pig is infected w/2 different flu strains (1 from bird 1 from human)
antigenic drift
individual mutations (ex: change from A to C) occur frequently
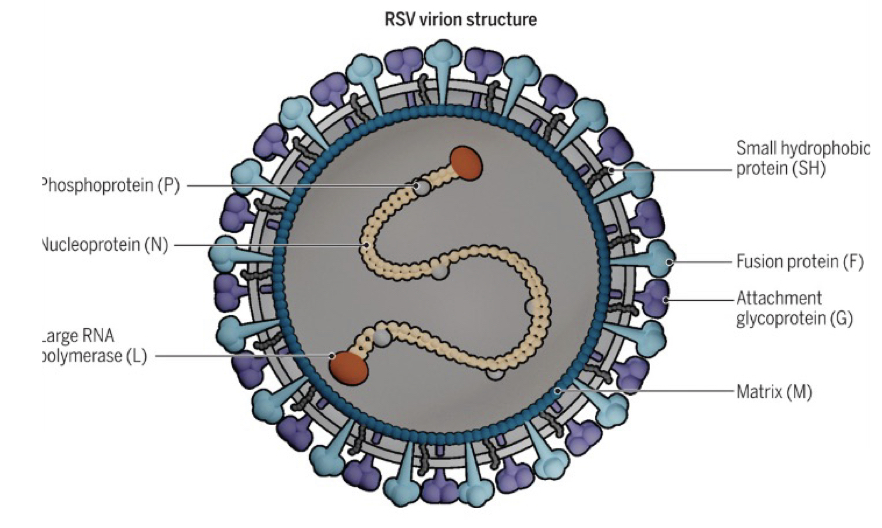
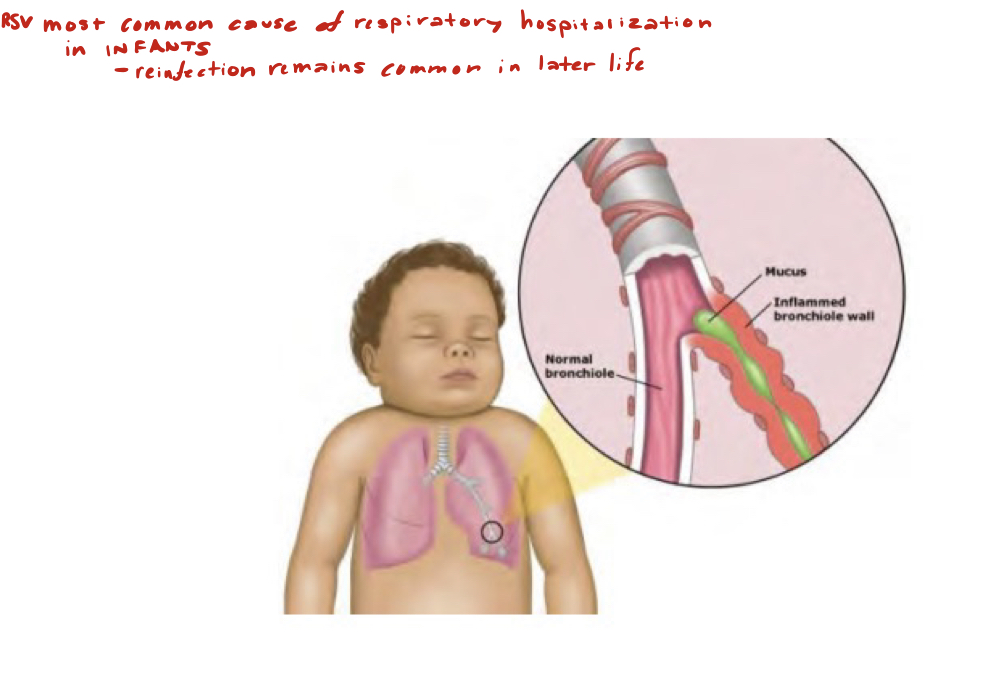
respiratory syncytial virus (RSV)
enveloped virus with RNA genome
not zoonotic, humans only reservoir
7 structural proteins
1 single stranded RNA (ssRNA)
membrane enveloped
the attachment glycoproteins (G) bind to host receptors
what type of illness does RSV cause?
spread by respiratory droplets and fomites
leading cause of serous infections in infants, young children, and elderly
infection in infants can lead to bronchiolitis caused by sloughed cells and inflammatory response; pneumonia in elderly and immunocompromised individuals!
can cause common cold like symptoms in healthy adults
what is the new vaccine approved for adults?
RSV vaccine (adults only, not approved for infants)
subunit vaccine consist of attachment and glycoprotein adjuvant
how can we prevent severe RSV illness?
most people are infected multiple times
avoid close contact with sick people
hand washing and good hygiene
avoid touching face with unwashed hands
vaccination for adults 60 and older, those with underlying conditions
antibodies for high risk infants and some children
fungal pneumonia
more rare
3 types
coccidiomycosis
histoplasmosis
pneumocystis pneumonia
coccidiomycosis
“valley fever”
US: arid regions of southwest
usually self limiting
fungal pneumonia
histoplasmosis
mild illness in most
fungal pneumonia
found in soil contaminated with bat or bird droppings
usually benign
pneumocystis pneumonia
organism present in many people but does not cause disease
only causes disease in immunocompromised individuals (AIDS)
rare enough to be considered “AIDs defining”
fungal pneumonia
flu infection directly damages these cells, which can lead to secondary bacterial infections
ciliated epithelial cells
true or false, the host specificity of a flu virus is dependent on its hemagglutinin (HA) type
true
virus strains with H1 can infect humans, while strains with H5 infect birds