PATHO EXAM 1
1/72
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
73 Terms
Homeostatsis
a dynamic steady state at which the bodymaintains itself at a relatively constant composition.
What 4 things does a cell do when faced with challenges, stress, or injury?
1. adapt to compensatory changes
2. develop maladaptive changes
3. reverse the damage
4. cell death
What are the types of cellular adaption?
atrophy, hypertrophy, hyperplasia, metaplasia, dysplasia, neoplasia
Atrophy
- decrease in cell size
-Cell reverts to a smaller size in response to changes in metabolic requirements or their environment.
-Results from:• Disuse or diminished workload• Lack of nerve stimulation (paralysis)• Loss of hormonal stimulation• Inadequate nutrition• Decreased blood flow (ischemia)• Aging
- positive adaption
-benefit: cell need less resources when not enough resources.
Hypertrophy
- increase in cell size
-Increase in individual cell size that results in an enlargement of functioning tissue mass
- can lead to greater metabolic demand and energy needs
- is a +/- adaption
Hyperplasia (overgrowth)
-increase in the number of cells
- +/- adaptation
-increased mitotic activity
- results in increased tissue/ organ mass
-can happen through hormones or repairment (wound healing)
- EX: Pregnancy increases demand of milk production (lactation),which causes hyperplasia of breastmilk glands and tissue mass
Metaplasia
- cella replaced by another type of cells
- results of Cells genetic reprogramming in response to a change in environmental conditions. chronic inflammation
- EX: GERD- Normal squamous epithelial cells transform in columnar like cells.
- + adaption
Dysplasia
-deranged/ altered cellular growth
- cell changes in morphology
- caused by precancerous condition and chronic inflammation.
- watch carefully because very often will develop into neoplasia (cancerous)
- can happen in development or acquired
Neoplasia
- uncontrolled cell growth
- new cells every 3 days
- cells lack normal cell function and are disorganized
- usually cancerous continue to grown and grow
- can break away and travel
- neoplasm = tumor
- can be benign or malignant
- can be due to genetics, hormones, uv light, or radiation
What are the causes of cellular injury/ damage
- hypoxic cell
- free radicals
- physical agents
- chemical
- infectious agents
-injurious immunological reactions
- genetic defects
- nutritional imbalances
Apoptosis
-Known as programmed cell death
-Can be triggered by cellular injury or it can be genetically programmed
-Example of cellular injury: A cell that has become cancerous and needs to be destroyed
-Example of genetically programmed:• Ovaries undergo apoptosis in females aged 55
-Cells that fail to undergo apoptosis can give rise to certain cancers, tumors, and detrimental hyperplastic cell changes.
-Example: Prostate cancer is theorized to arise from cells that lose their apoptotic function.
Necrosis
- when a cell that is flagged for death and doesn't undergo it, it explodes and causes other cells to stress.
What is inflammation?
-a protective, coordinated response of the body to an injurious agent
- can be acute or chronic
- commonly termed "itis"
What are the major aims of inflammation?
- wall of the area of injury
- prevent spread of the injurious agent
- bring the body's defense to the region under attack
What system powers immflamuation?
all powered by the immune system
What are the cardinal signs of inflammation?
- rubor (redness); due to increased BF
- tumor( swelling): due to increased BF
-calor(heat): due to increased BF
-dolor (pain): due to histamine and prostaglandin's
-loss of function
- ALL CAN BE ASSED DURING assessment
What are the 3 stages of acute inflammatory response?
1. vascular permeability
2. cellular chemotaxis
3. systemic response (cardinal signs)
Vascular permeability
- blood vessels dilate at the site of injury
-the dilation allows for permeability
- increased permeability allows WBC, fluids, and platelets to travel to site of injury
How does the body know to open blood vessels?
Inflammatory mediators such as histamine, nitric oxide, and bradykin
What causes swelling?
the fluid that flows out of the blood vessels to the injured tissue
cellular chemotaxis
Chemical signals are sent to both help amplifyand stop the inflammation process.
What are cytokines?
-inflammatory mediators released by WBCs
- EX: Tumor necrosis factor (TNF- alpha) and interleukins (ILs)
- Cytokines amplify or deactivate inflammation
Acute Phase Proteins
-released by the liver under direction of cytokines
- Examples include C-reactive protein(CRP), fibrinogen, and serum amyloid A
-Influence the inflammatory process by stimulating, modulating, and deactivating the reaction.
- USED AS INFLAMMATORY MARKERS IN BLOOD WORK
Systemic response
-This systemic response is caused by inflammatory mediators released from WBCs: cytokines
- Ex of cytokines: Prostaglandins, Leukotrienes, Tumor necrosis factor (TNF-alpha), Interleukins (Ils), Histamine,Bradykinin
-results of acute inflammation: fever, pain, general malaise, lymphadenopathy, anorexia, sleepiness, lethargy, anemia, weight loss.
What is fever?
fever is a protective mechanism the body uses to fight off infectious agents or due to acute inflammation where the body rises its temperature.
What is pyrogens?
-substance that causes fever
- microbial organisms, bacterial products, and cytokines all act as pyrogens
How do pyrogens cause fever?
Pyrogens activate prostaglandins to reset the hypothalamic temperature-regulating center in the brain to a higher level
What is a normal fever?
-100.4 F
-Fever can reach levels high enough to cause seizures and brain damage.
-Recommended to keep fever below 102°F through the use of antipyretic medications such as aspirin, ibuprofen, or acetaminophen.
How does aspirin, ibuprofen, and acetaminophen work to reduce fever?
These medications inhibit prostaglandin formation and, thus reduce fever
How does fever vary inthe geriatric populationcompared to adults orchildren?
older adults are typically a degree lower because they have less subcutaneous fat and lower metabolic rate.
Reye's Syndrome
-Typically occurs after a viral illness (particularly an upper respiratory tract infection, influenza, varicella, or gastroenteritis) and is associated with the use of aspirin during the illness in CHILDREN
-In ages 18 years or younger (mainly 4 or younger)
-Affects liver and the neurological system
-Symptoms: Nausea and vomiting, Change in mental status, Weakness, Vision and hearing changes, Agitation/ Seizures
-Treatment: supportive measures; Particular attention paid to control of increased intracranialpressure (ICP)
- usually fatal
How can be assess the immune response during inflammation or infectious agent?
-Determined by a CBC (complete blood count) via venipuncture
-Examines amounts of leukocytes and other white blood cells
-During inflammation, increased number of WBCs from bone marrow into bloodstream
What is the normal range of WBC?
4,000-10,000 cells/ mL
What is the range for leukopenia?
less than 4,000 cells/ mL
- happens with autoimmune diseases, HIV, AIDS, chemo
What is the leukocytosis range?
greater than 10,000 cells/ ml
What is the range for acute inflammation?
15,000 - 20,000 cells/ml
What is the range for leukemoid reaction?
greater than 50,000 cells/ml
-seen with leukemia patients
What are the types of WBC?
granulocytes and agranulocytes
What are granulocytes?
-neutrophils, eosinophils, basophils
- have granule enzymes on them
- mature in the bone marrow
-provides immediate immunity
What are agranulocytes?
-lymphocytes and monocytes
- long term immunity
-uses memory
- helps with vaccines
Neutrophils
- most abundant (80%)
- considered the EMTs of WBC (with in 24-28 hrs)
- destroys pathogens quickly
- die quickly and become puss
- when infection is severe, immature neutrophils will be released from bone marrow to help.
Eosinophils
- present in allergy or parasitic infections
- 1-5% of WBC
Basophils
-filled with histamine
-present with infections and chronic allergies
- less than 2%
Monocytes/Macrophages
-phagocytic leukocytes that follow the neutrophils to clear the debris
- travels through tissue to pathogen
- doesn't show up till later (after 24-28 hrs)
-long life span (weeks to months)
Lymphocytes
- creates antibodies
- two types: B & T cells
What are bands?
Immature neutrophils; increased levels suggest acute infection; pushed out before maturity due to need for more.
What are the phases of wound healing?
1. Hemostasis
2. Inflammation- WBC rush to area, chemotaxis, breakdown of debris
3. Proliferation, granulation tissue formation, and epithelialization- rebuild what was broken down
4. Wound contraction and remodeling- scar tissue is starting to be reshaped and blood vessel regrowth
What factors affects wound healing?
• Nutrition- need protein and calories
• Oxygenation- need good BF
• Circulation
• Immune strength
• Diabetes; weakens healing
• Use of corticosteroids; diminishes healing
• Use of immunosuppressant agents
• Contamination
• Surgically inserted devices
• Obesity
• Age
How can a nurse promote good wound healing?
• Dressing Changes - keeping area clean
• Lab values- albumin, pre-albumin
• Tight glycemic control (avoid high blood glucose levels)
• Nutrition- encourage high protein diet
• Nutrition- encourage supplementation (zinc, vitamin C)
• Ambulation - to increase circulation and perfusion
• Turning bed bound patients every 2 hours
• Off loading weight
What are so complications of wound healing?
keloid, contractures, dehiscene, evisceration, stricture, fistula, adhesions
Keloid
hyperplasia of scar tissue

Contractures
inflexible shrinkage of wound tissue that pulls the edges toward the center of the wound

Dehiscene
opening of a wound's suture line

Evisceration
opening of wound with extrusion of tissue and organs

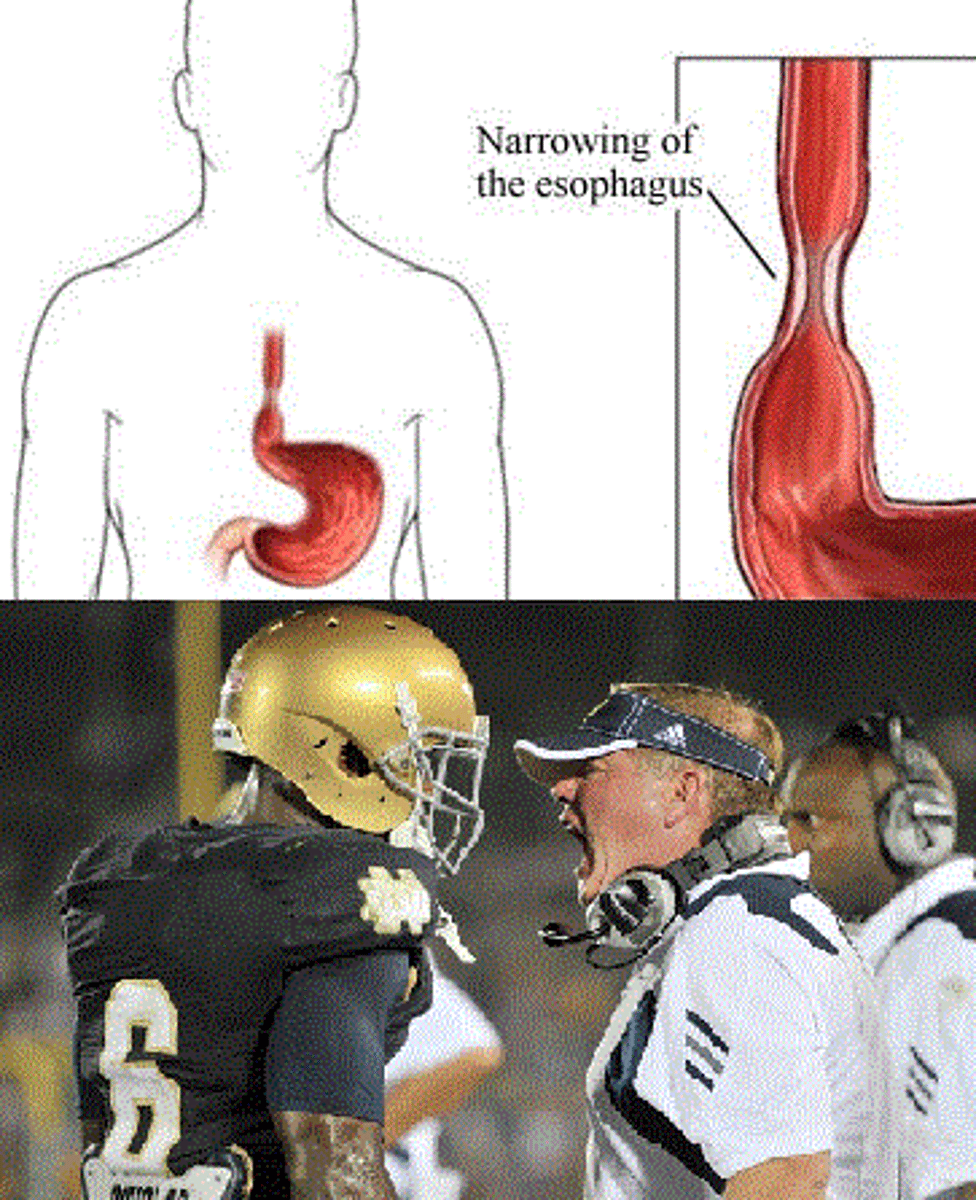
Stricture
an abnormal narrowing of a tubular body passage from the formation of scar tissue
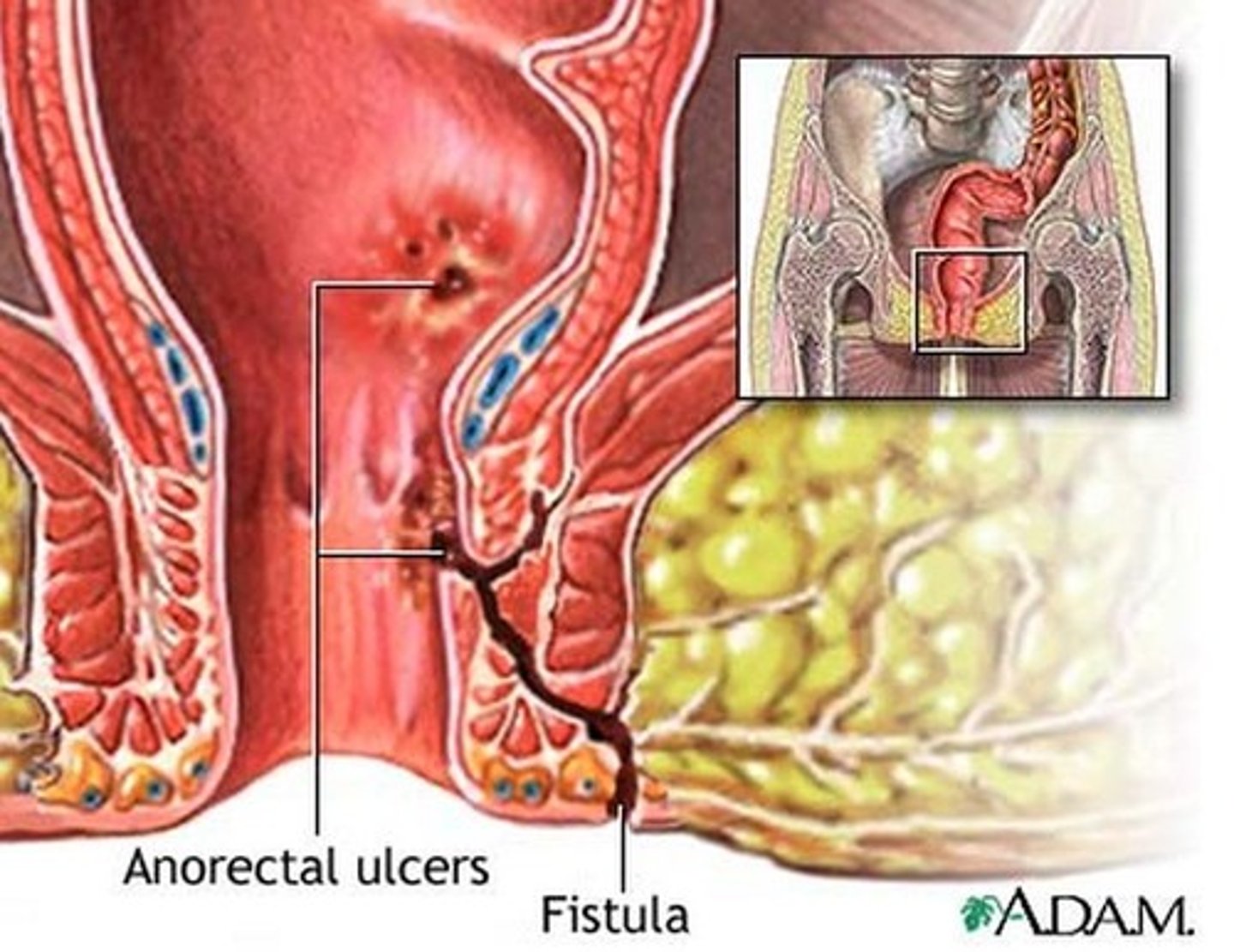
Fistula
an abnormal connection btw two epithelium-lined organs or vessels
usually most common in bowls or vaginal areas
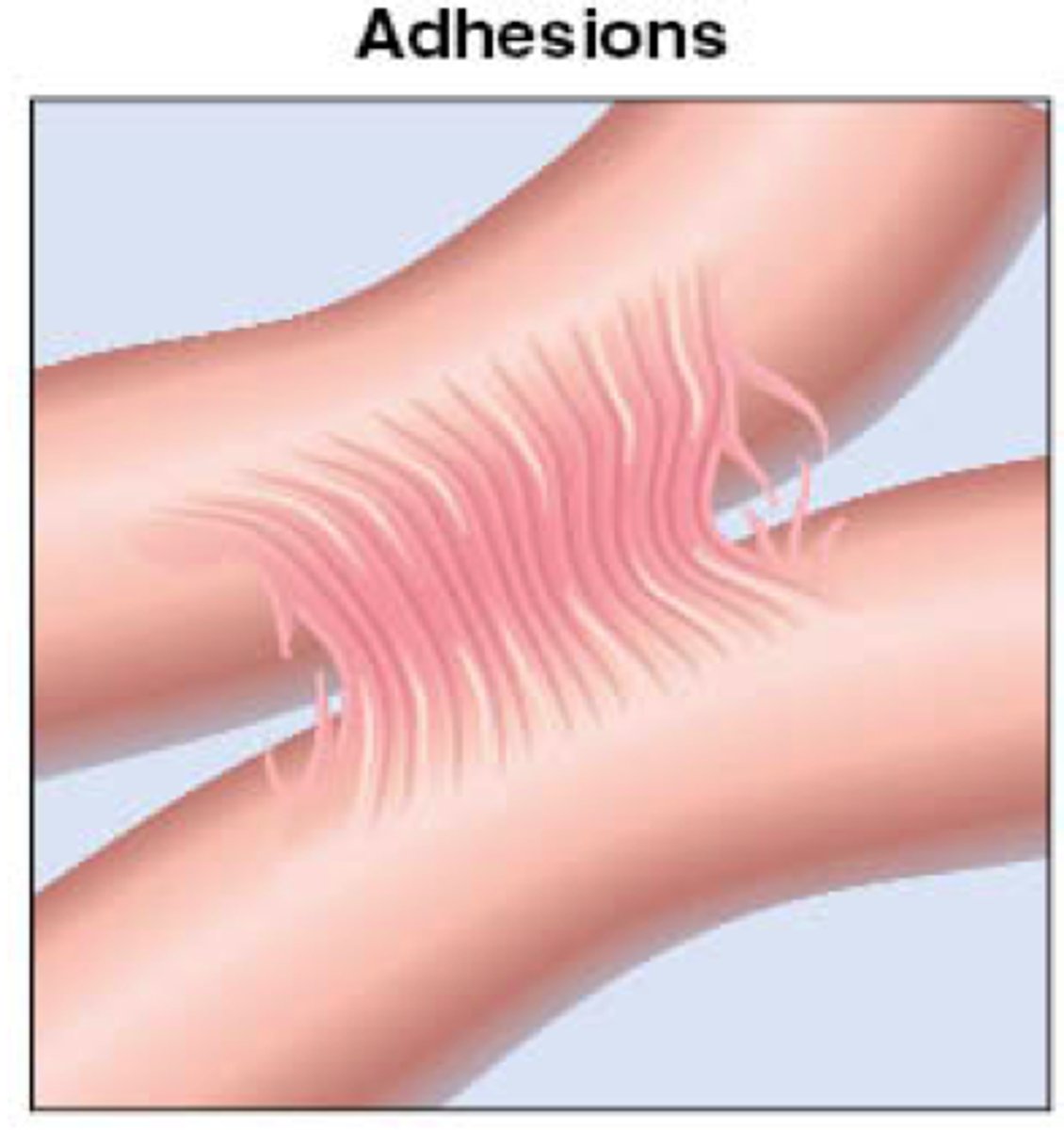
Adhesions
internal scar tissue btw tissues and organs
Can normal flora cause infection?
Normal flora do not cause infection when they remain within the strict boundaries of their anatomic niche in the body.However, if normal flora bacteria invade non colonized areas of the body, they can cause infection
Opportunistic Infection
caused by a microorganism that flourishes because of a host's deficient immune system
Nosocomial infection
caused by microorganisms inherentto the health-care facility environment; hospital-acquiredinfection.
Why are nosocomial infections difficult to treat?
because they are often caused by antibiotic-resistant bacteria
-commonly caused by staphylococcus aureus
Innate Immunity
Nonspecific mechanism that defends the body against all types of pathogens immediately; 1st line of defense
- born with
-no memory
Adaptive Immunity
Specific mechanism that develops with exposure to antigens and targets precise pathogens; 2nd line of defense
-get when vaccinated
- stronger than innate
-has memory
- B & T cells
What are the portals of entry?
- skin
-respiratory tract
-GI tract
- Genitourinary tract (GU) tract
-blood to blood transmission
- maternal-fetal transmission
Incubation
-Organism begins active replication without symptoms in the host
-Host is highly contagious, not aware of illness
- could be hours or days
Prodromal stage
-Initial appearance of symptoms (starting to feel sick)
• Vague symptoms: malaise, headache, fatigue
• Host is highly contagious
- immune response starting
Acute stage
-Host experiences full infectious disease with rapid proliferation of pathogen
• Defenses are in full force, inflammation reaction is fully engaged
• Symptoms are heightened; still contagious
Convalescent stage
- body attempt to eliminate the pathogen
- fell less sick
-pathogen decreased
- resolution of symptoms begin
Resolution stage
total elimination of pathogen' no signs or symptoms
-can have permeant damage to host (ex: scar in lung tissue)
What lab test should be done with their is a infection or pathogen?
-CBC with differential
• Gram stain (bacteria)
• Culture (urine, stool, sputum,wound)
• Biopsy
• Antibody titer
• Polymerase chain reaction (PCR) detects genetic material (especially used with viruses)
What is the most effective method of controlling contagious diseases?
vaccines
What does vaccines do to the immune system?
stimulate the immune system to make antibodies against pathogens
involves b and t cells
How long does it take the body to make antibodies?
30 days