L3: the determinants of cardiac output
1/89
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
90 Terms
Why is it important to regulate cardiac output CO
needs to be sufficient to ensure adequate perfusion of all the tissues
this means it must increase as metabolic demands rise in exercise
Critical in determining arterial blood pressure (ABP)
Heart’s control of CO, experiement
Replaced right atria of dogs with high-output pumps
reducing pumping capacity below normal→ reduced cardiac output
however:
increasing the pumping capacity→ NOT INCREASE in CO
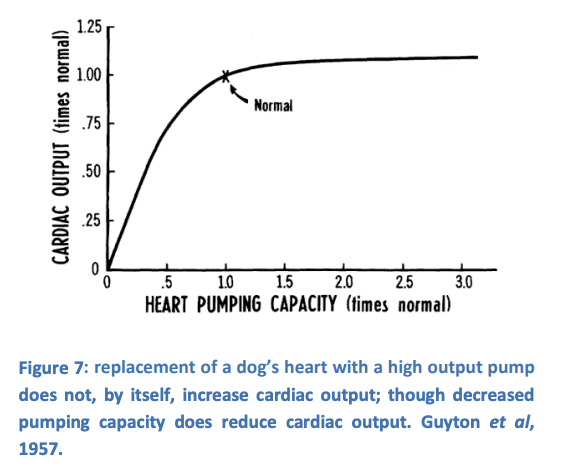
This experiment illustrated two circulatory concepts
The heart is necessary to maintain CO
but
The heart does not normally limit CO
Why can’t the increase in heart pumping, increase its own CO?
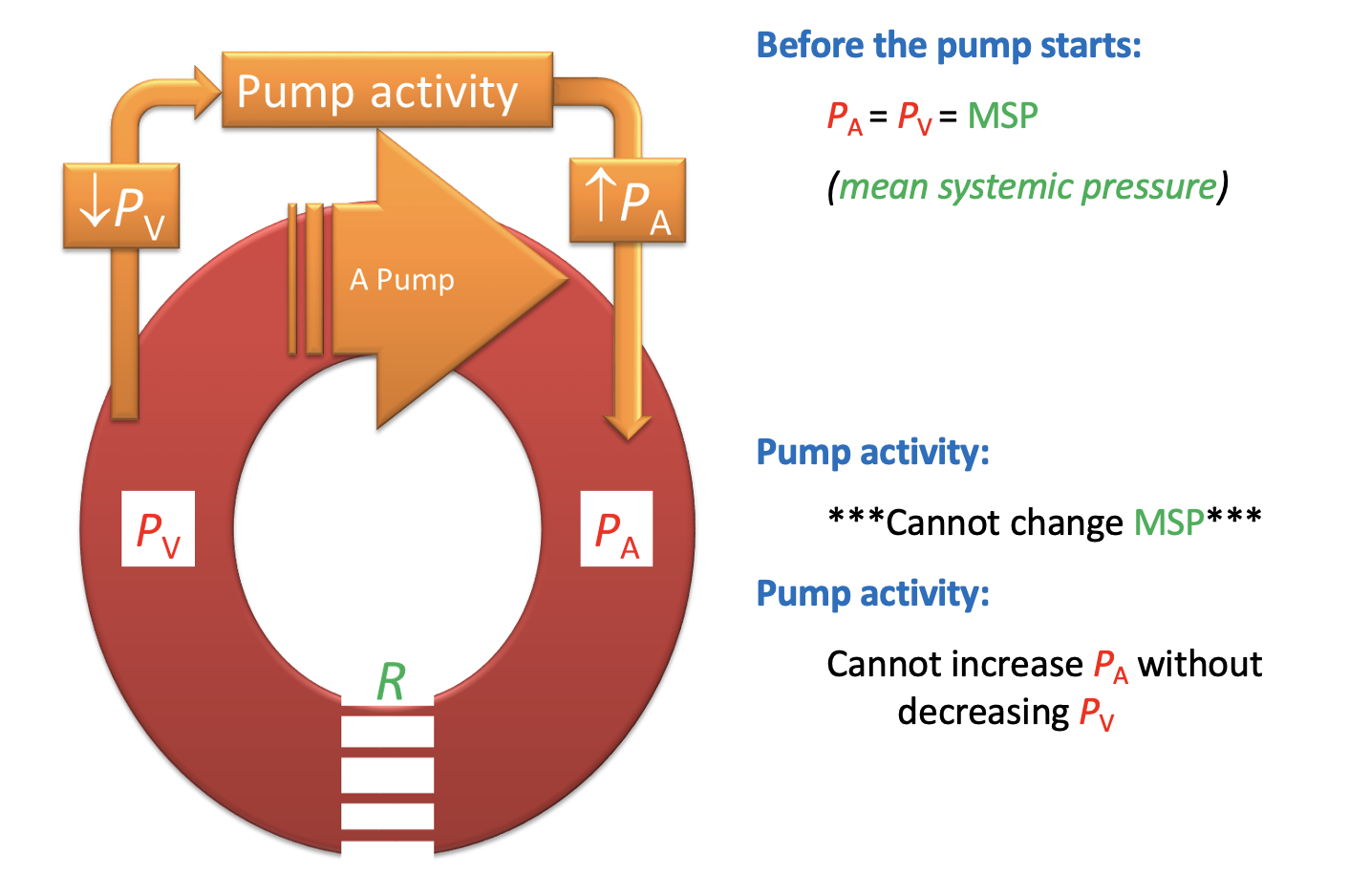
Circulation is a closed system
like a balloon with fluid
can’t change the average pressure in the balloon
certainly can’t inflate or deflate it
A pump or fan inside the balloon CANNOT change the MEAN pressure in the balloon
It can onlyuse pressure gradients

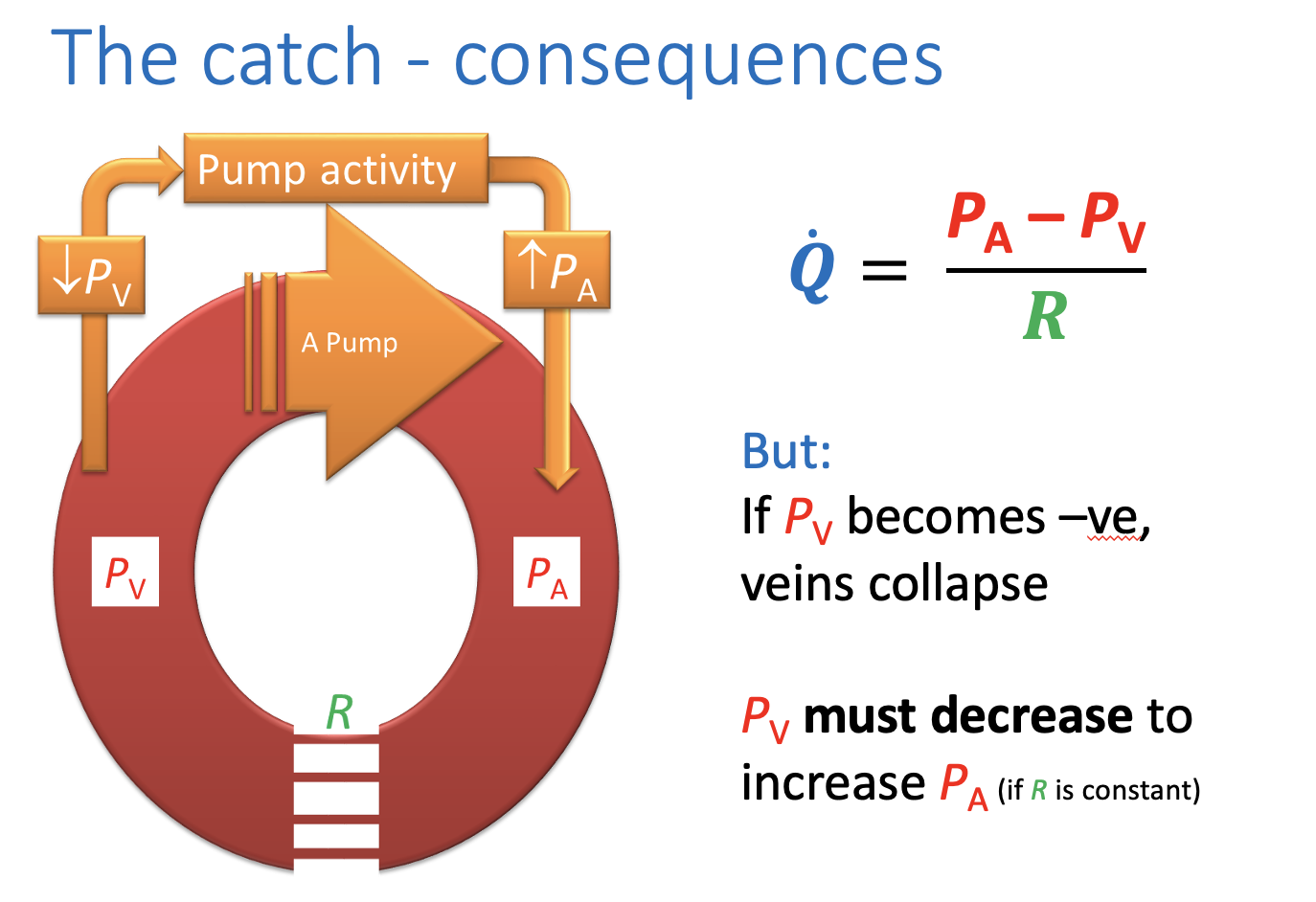
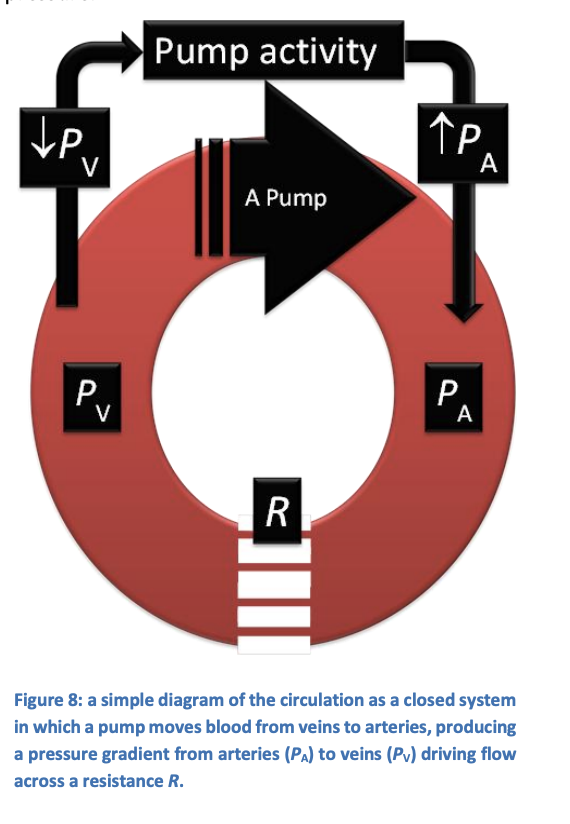
Explanation
Heart takes blood from the veins→ reducing venous pressure Pv
puts it in the arteries→ increases arterial pressure PA
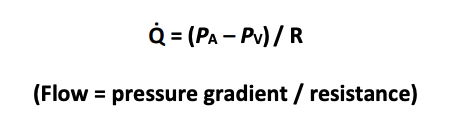
This pressure difference then drives flow through our model system according to:
Q=(PA-Pv)/R
If the closed system was made of rigid tubing…
greater pump activity could produce ever-increasing pressure gradients
and hence flows
However, if the tubing is not rigid:
Important constraint appears:
if Pv becomes negative (with respect to atmosphere pressure)
then tubing will collapse
similarly:this provides exaplnanation for figure 7
real veins collapse when pressure within them drops
more than 1 or 2 mmHg below atmospheric pressure
Pascal’s principle→ pressure the same everywhere
LaPlace→ all tension largest where vessel diameter greatest
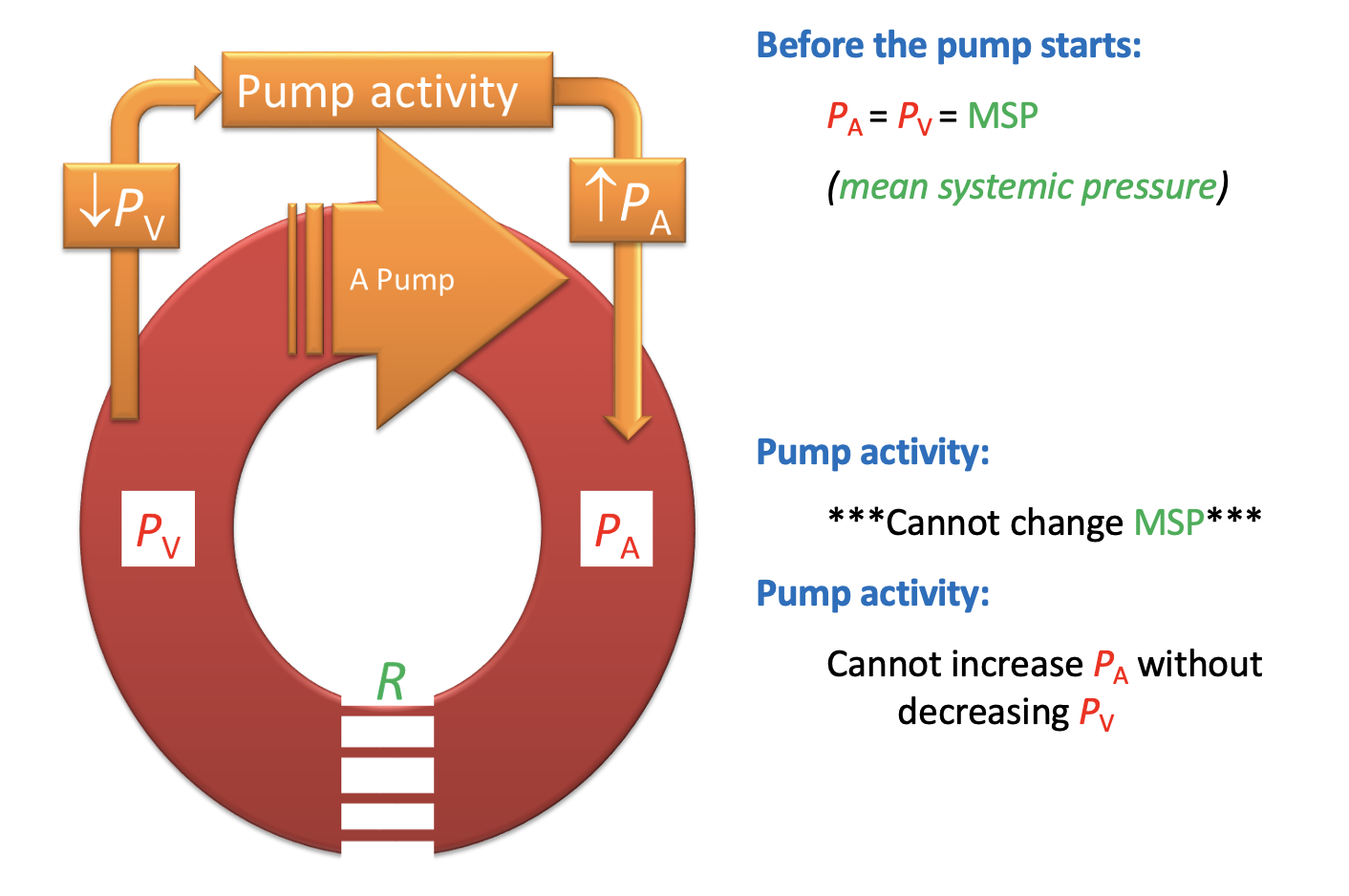
Why can’t the heart increase the ateriovenous pressure difference (PA-PV) beyond the point at which Pv becomes signficantly negative
because if Pv becomes, negative
venous collapse limits venous return
→ cardiac output
veins are floppy walled like a balloon
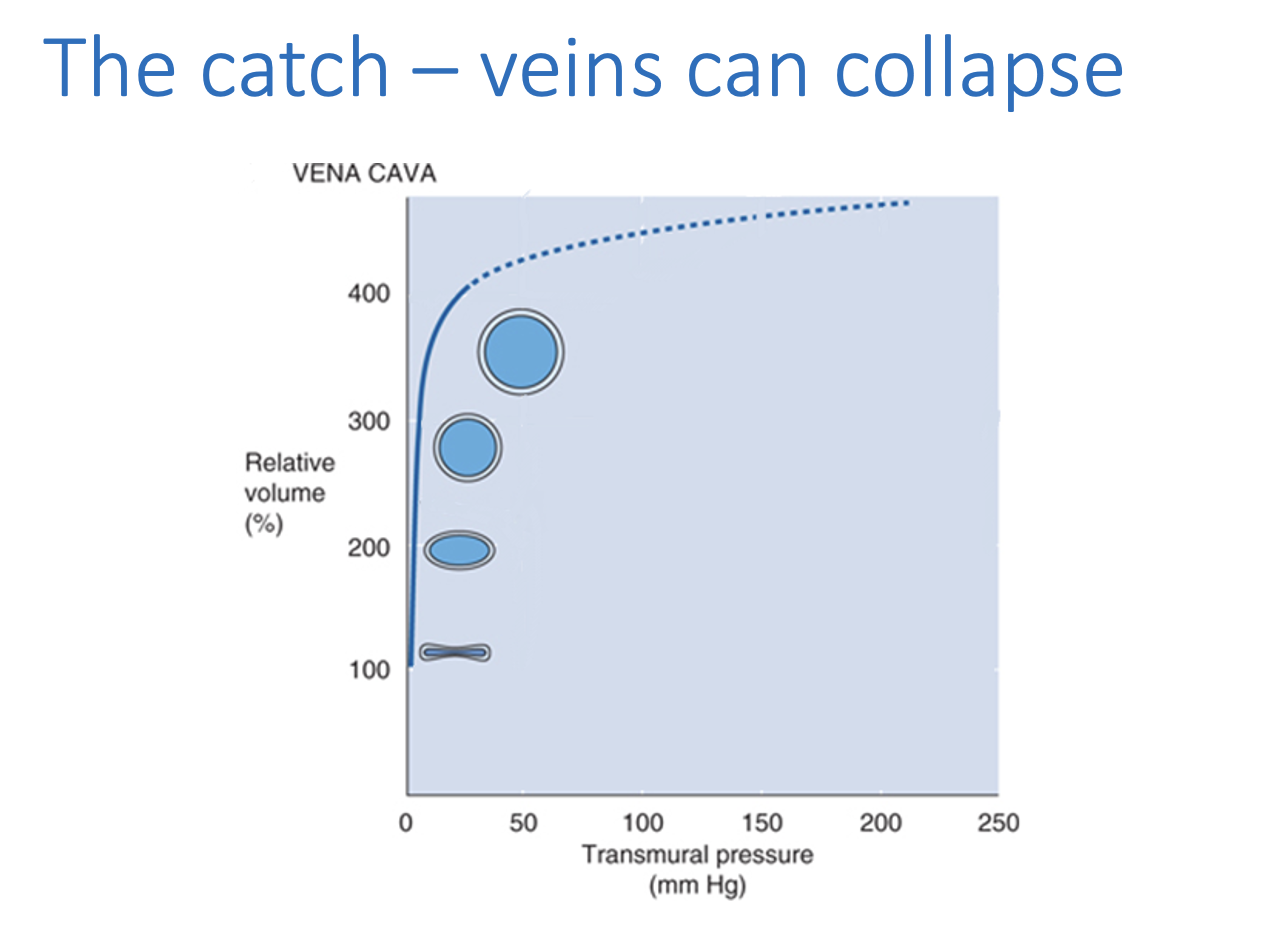
Due to veins being collapsable
Although Q=PA-Pv/R
If Pv becomes negative, veins collapse
THEREFORE: PV must decrease to increase PA
if R is constant
What do direct measurements show
of the right atrial pressure
by inserting a catheter via the jugular vein
Confirms:
a healthy heart reduces central venous pressure to almost zero
even at rest
What does this mean
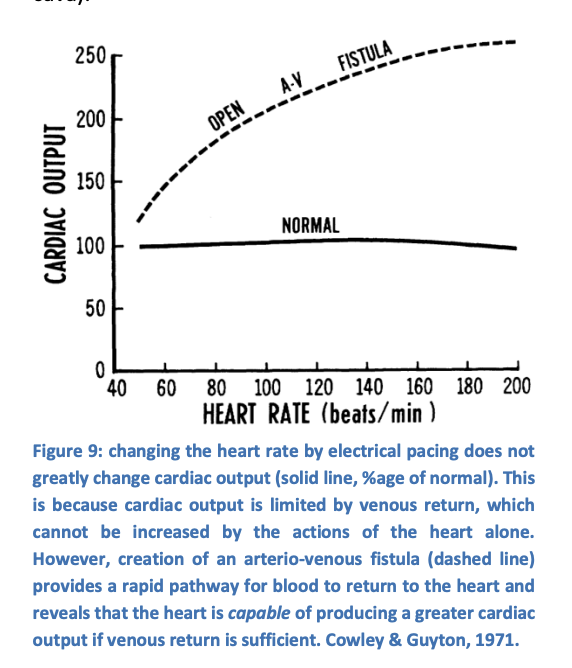
Increasing heart rate or myocardial contractility in isolation
e.g by stimulating the cardiac sympathetic nerves or electrically pacing the heart
cannot significantly increase cardiac ouput
unless venous return is also increased
in this experiment, accomplished by connecting the aorta to the vena cava
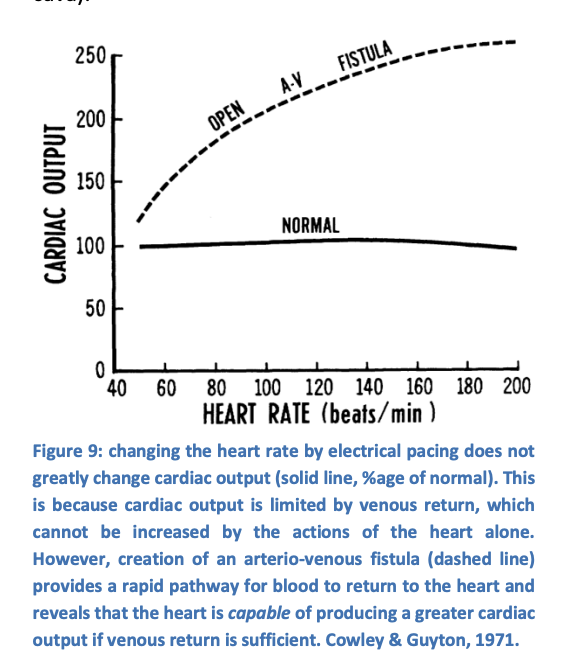
Evidence 1: What this shows
Heart rate does not change cardiac output
stroke volume changes reciprocally
however:
Give the heart more blood
i.e surgically
the heart can now pump more
How can Mean Styemeic filling pressure be changed?
Add volume
Constrict circulation→ decrease capacitance
This leads to the question of…
if increasing cardiac pumping capacity is not sufficient to increase cardiac output
what else is necessary?
What is the main determinant of cardiac output
Mean systemic filling pressure
In order to increase PA
the pump must reduce Pv
However
Pv is normally close to zero and so cannot be reduced
The solution?
raise the mean pressure in the whole system
Model to exmplain this
Imagine the mean pressure was0
Implies that Pv would become negative as soon as the pump started and prevent any flow of blood
next
IMagine the mean pressure was 10mmHg
now it is possile for pumping to produce a significant arterio-veous pressure gradient without collpasing the veins
Therefore, the mean pressure determines…
The maximum flow rate for a given distance
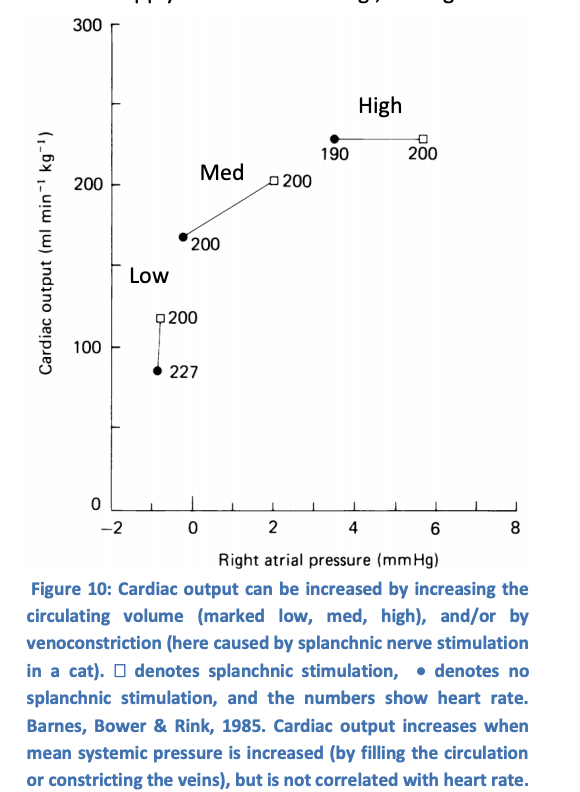
Check that this model applies to real life
circulating volume: Low Med high→ shows:
Med→ Right atrial pressure at 0
Low→ less blood= lower MSP, lower CO
High→ pumps all blood it can, CO increases
Splanchnic vs non-splanchnic stimulation (venoconstriction)
venoconstriction→ increased CO
MSP increase→ heart can respond to MSP to cahnge CO
not correlated with heat rate
What is mean systemic filling pressure (MSFP)
mean pressure in the system
equvalently, the pressure that would eventually exist everywhere in the system if the heart stopped
Like a balloon, MSFP can be increased by…
Extra filling
blood transfusion, drinking isotonic water
Constricting the filled volume
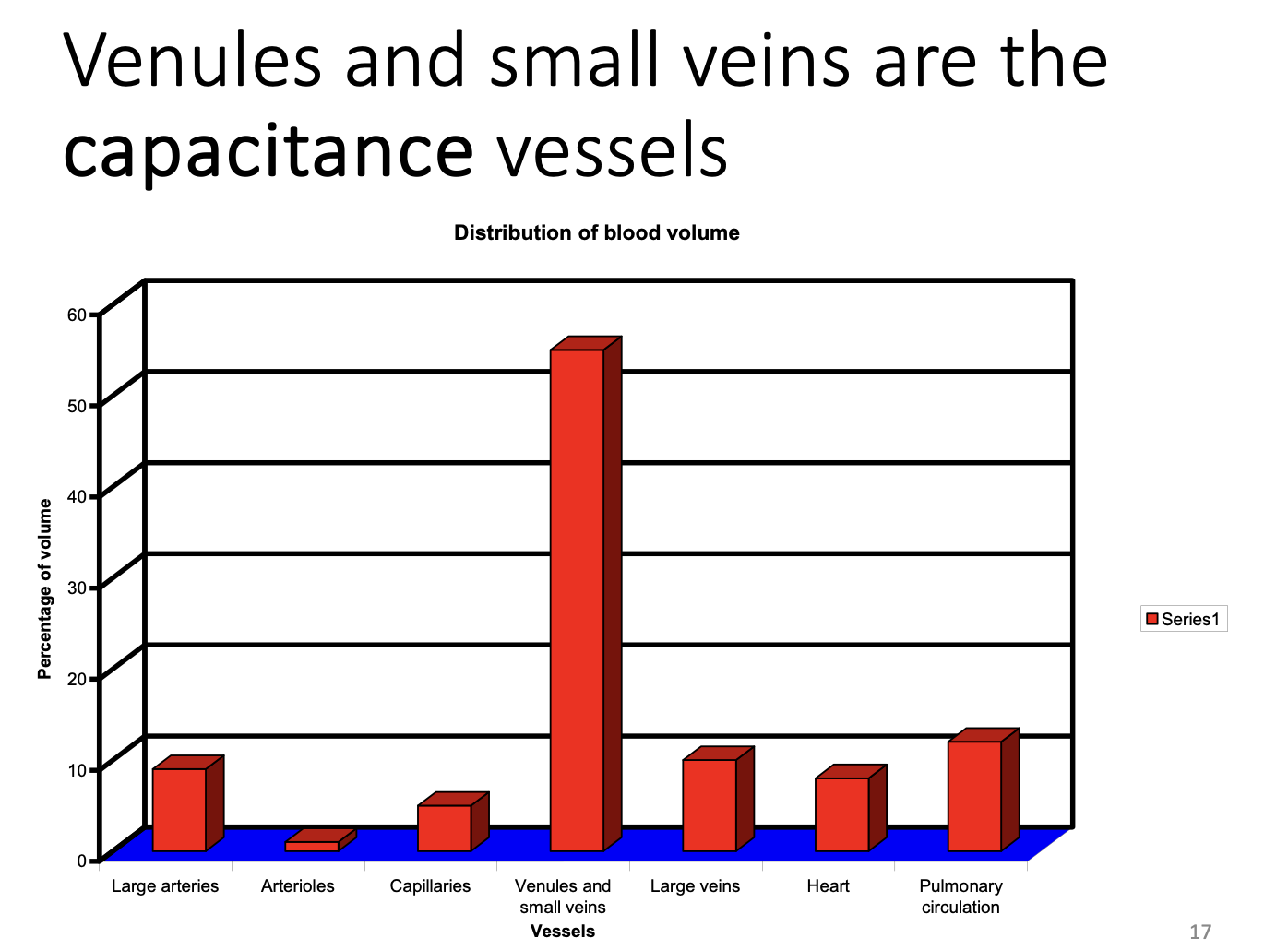
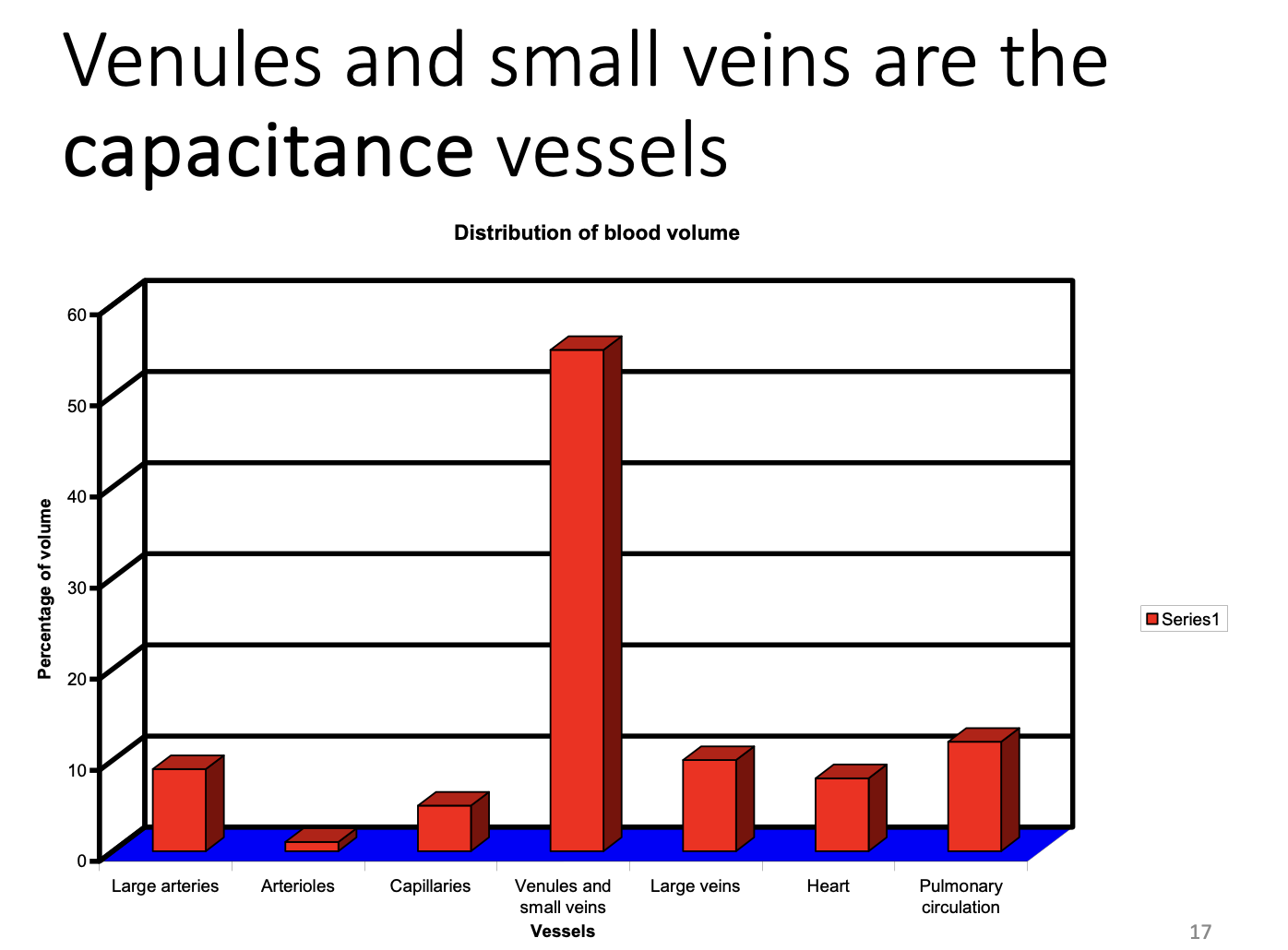
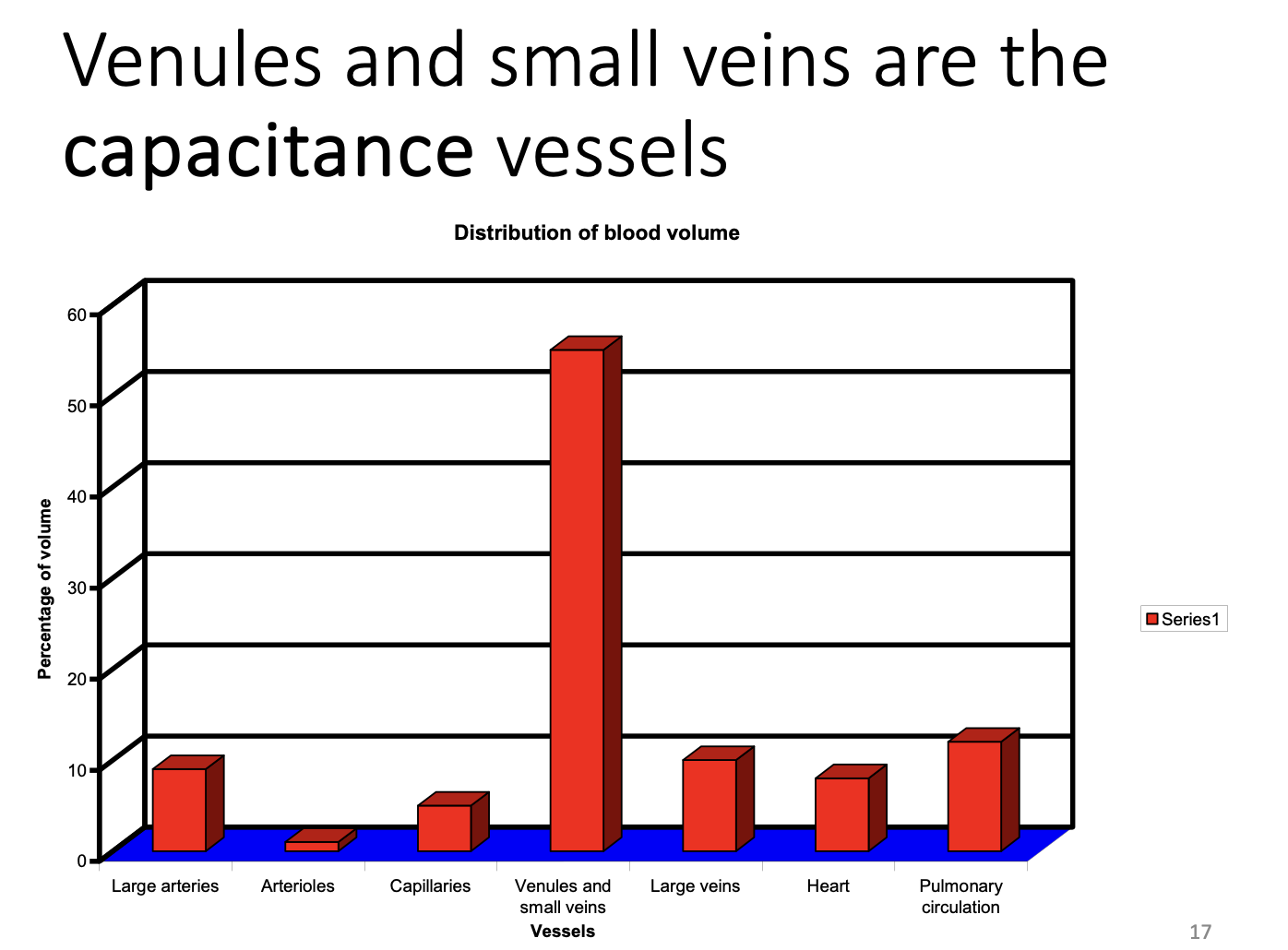
venoconstriction→ because 65-70% of the blood is in the veins
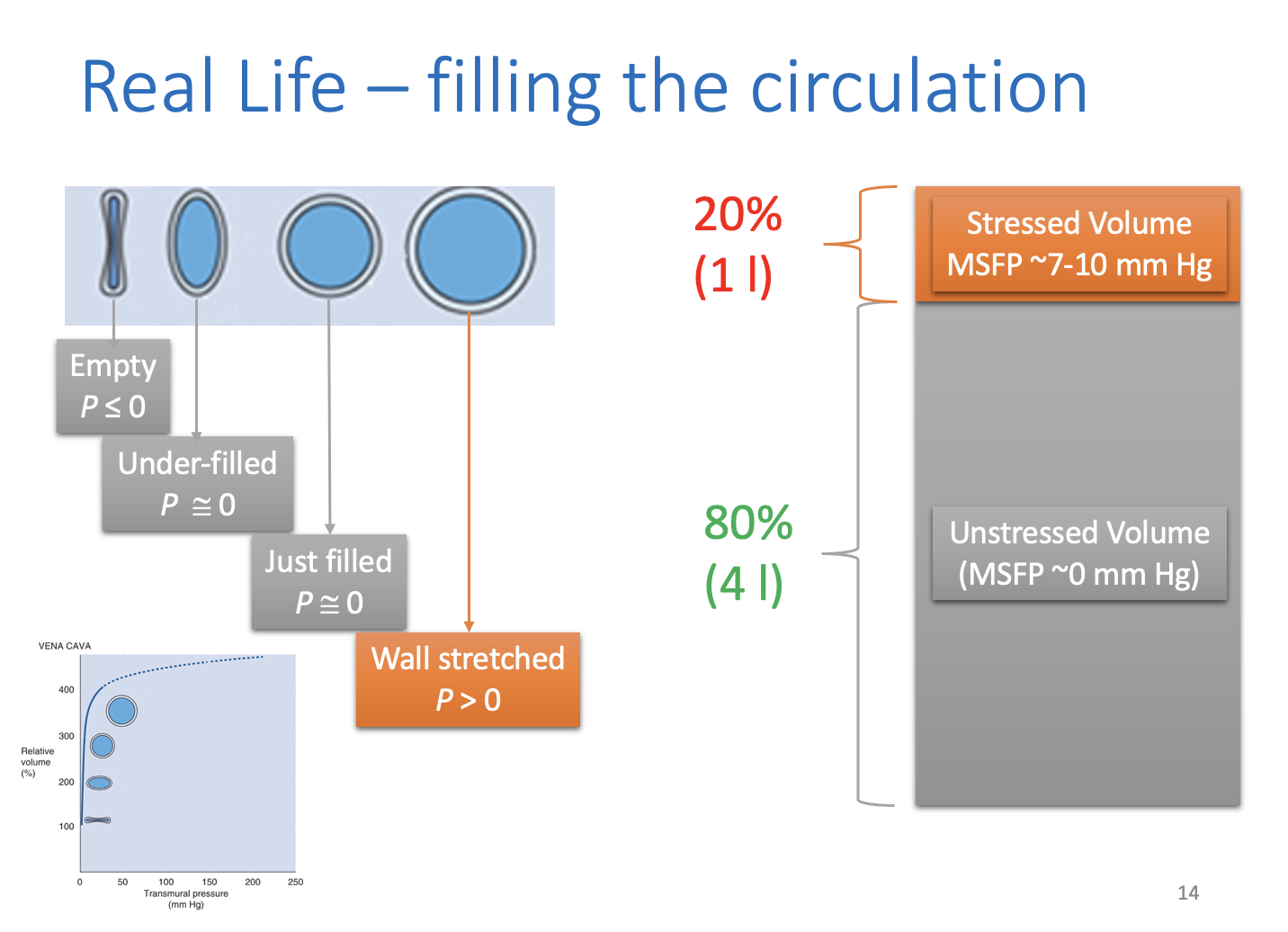
Understanding the real circulation, beyond the model 1
Start with empty circulation: 70-80ml/kg of body mass→ 5l for 70kg
if this is added to empty circulation→ first 0% does not cause a rise in pressure
pressure stays at 0 until the vessel walls begin to stretch
Unstressed volume
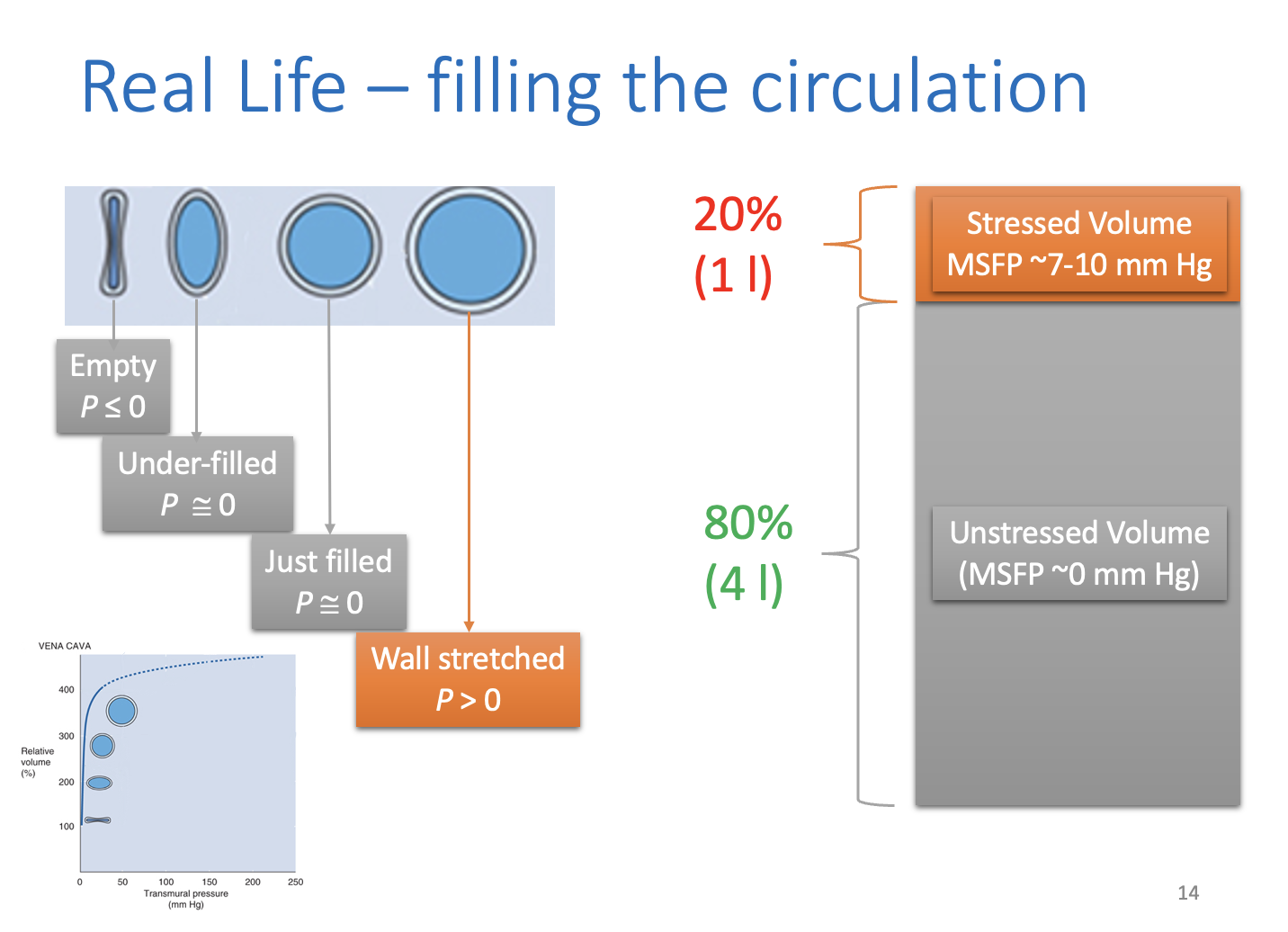
The unstressed volume
volume of blood that just fills the circulation without stretching the vessel walls
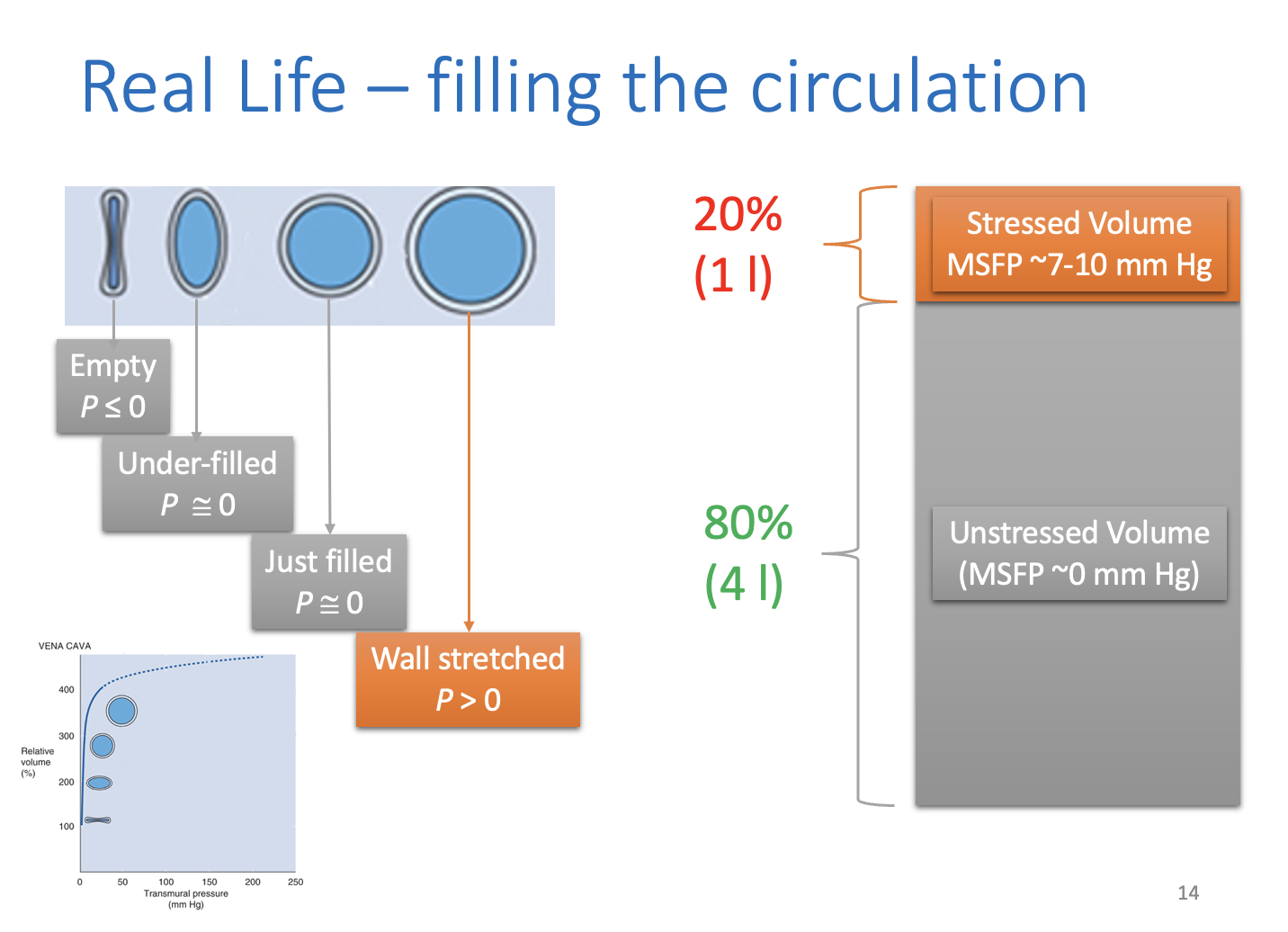
Understanding the real circulation, beyond the model 2
Add last 20% of normal blood volume
mean pressure in he system will rise
Extra volume: stressed volume
normally gives rise to mean presure of 7-10 mmHg in the circulation
Understanding the real circulation, beyond the model 3: heart starts to pump
blood transferred from the veins to the arteries
changes the venous and arterial presures according to their compliance
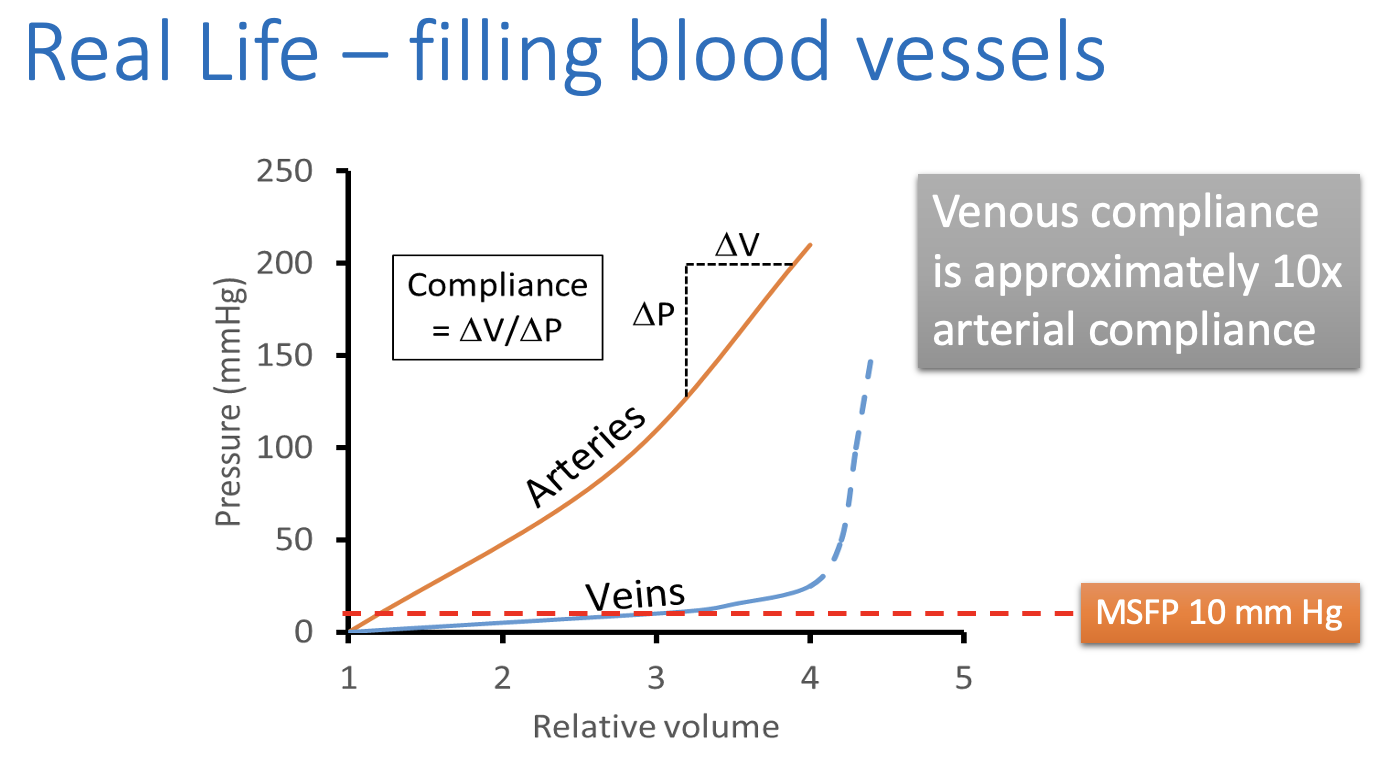
Compliance
change in volume/change in pressure
high compliance: Large change in volume for a low change in pressure
Compliance: Veins
Very compliant in the psyhiological range
In non physiological (very overstretched)→ VERY stiff
greatt for using saphenous vein graft to replace blocked coronary artery
What does high venous compliance ensure?
if pressure without cardiac activity was 7mmHg everywhere
the reduction in venous pressure with cardiac actitivty would be relatively small
Compliance: arteries
Much less compliant
causes a steep ris in presure due to movement of blood
Understanding the real circulation, beyond the model 4: venous and arterial pressures change until…
venous pressure is close to zero
Mean arterial pressure is about 90-95 mmHg
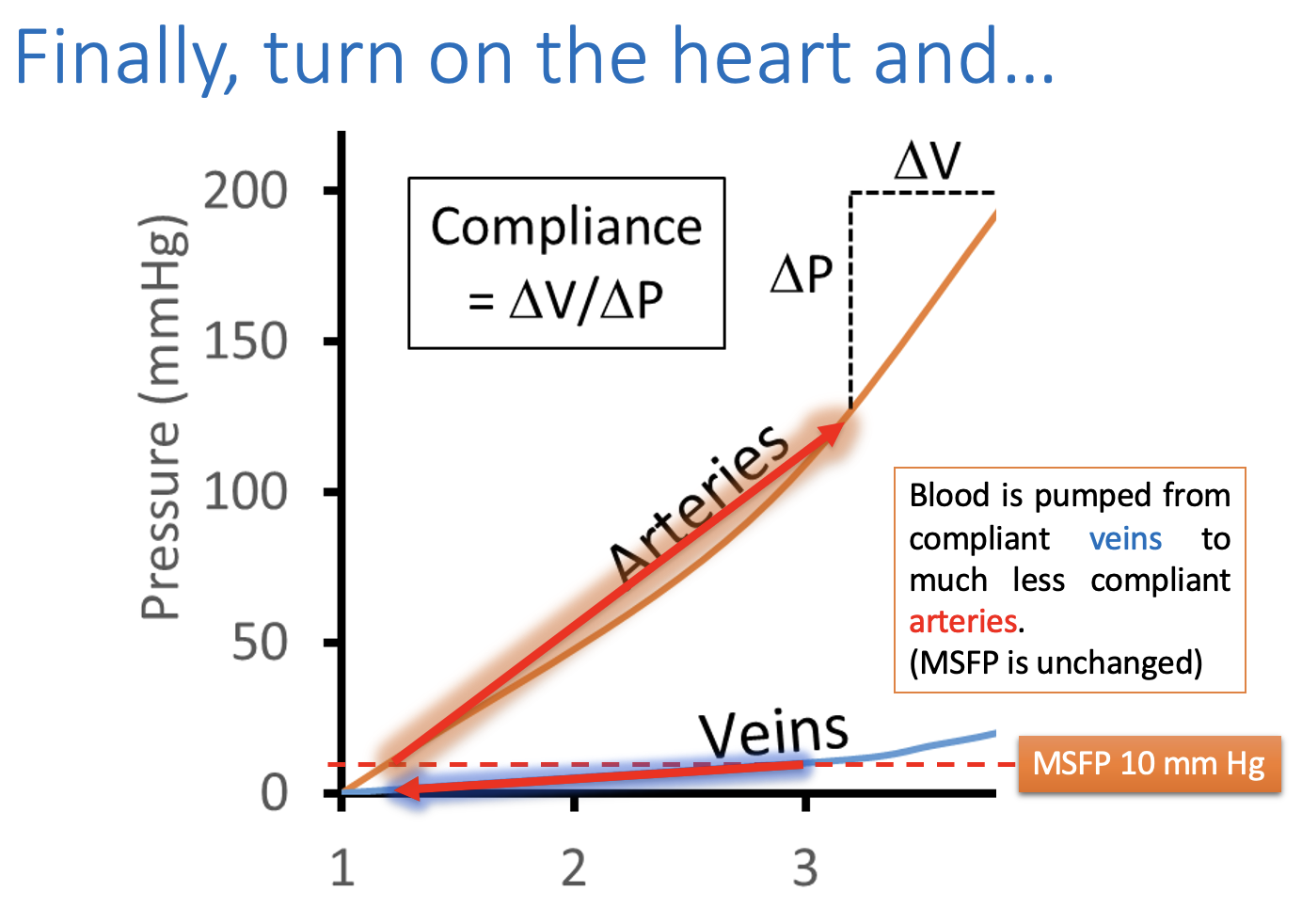
What does this mean
the heart is working normally:
Arteries are more filled
veins are less filled
Than they would be if the heart stopped
Understanding the real circulation, beyond the model 5
The ateriovenous pressure difference then drives blood flow
from the arteries via the capillaries
to the veins
→ Circulation
Because veins can collapse if the veous pressure falls below atmospheric pressure…
the maximum arteriovenous pressure difference is set by the mean filling pressure
This implies:
The heart cannot change the mean pressure
the mean pressure determines the maximum cardiac output
Recap of the abbreviations
Mean systemic filling pressure is therefore…
a critical determinant of cardiac output
How is MSFP determined
by the volume of blood
mean tension in blood vessel walls
MSFP can be doubled by
increasing the blood volume by 20%
Why is this?
this doubles the stressed volume
What does this also double?
The cardiac output
loss of 20% of cirulating volume…
reduces the MSFP ( and hence CO) to zero
because only the last 20% of blood actually stresses vessel walls
Fortuantely, mean tension in the blood vessel walla can be regulated
60% of blood is in thhe venules and small veins
→ venoconstriction can reduced the capactiy of the circulation
such that MSFP can be maintained above zero until about 40% of the circulating volume is lost
How is this accomplished?
sympathetic venoconstriction
→ can up to treble MSFP
Note: venoconstriction and Total peripheral pressure
Venoconstriction does not significantly influence TPR
What is TPR determined by
Resistance of the arterioles
But why does arteriolar constriction increase TPR but not influence MSFP
because (as seen in the graph) less than 1% of blood is contained within the arterioles
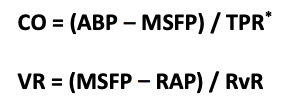
Quantifying cardiac output
Darcy’s law: Flow=pressure difference/resistance
therefore arteriovenous pressure difference produces blood flow:
CO= (ABP-RAP)/TPR
arterial blood pressure-right atrial pressure/total preipheral resistance
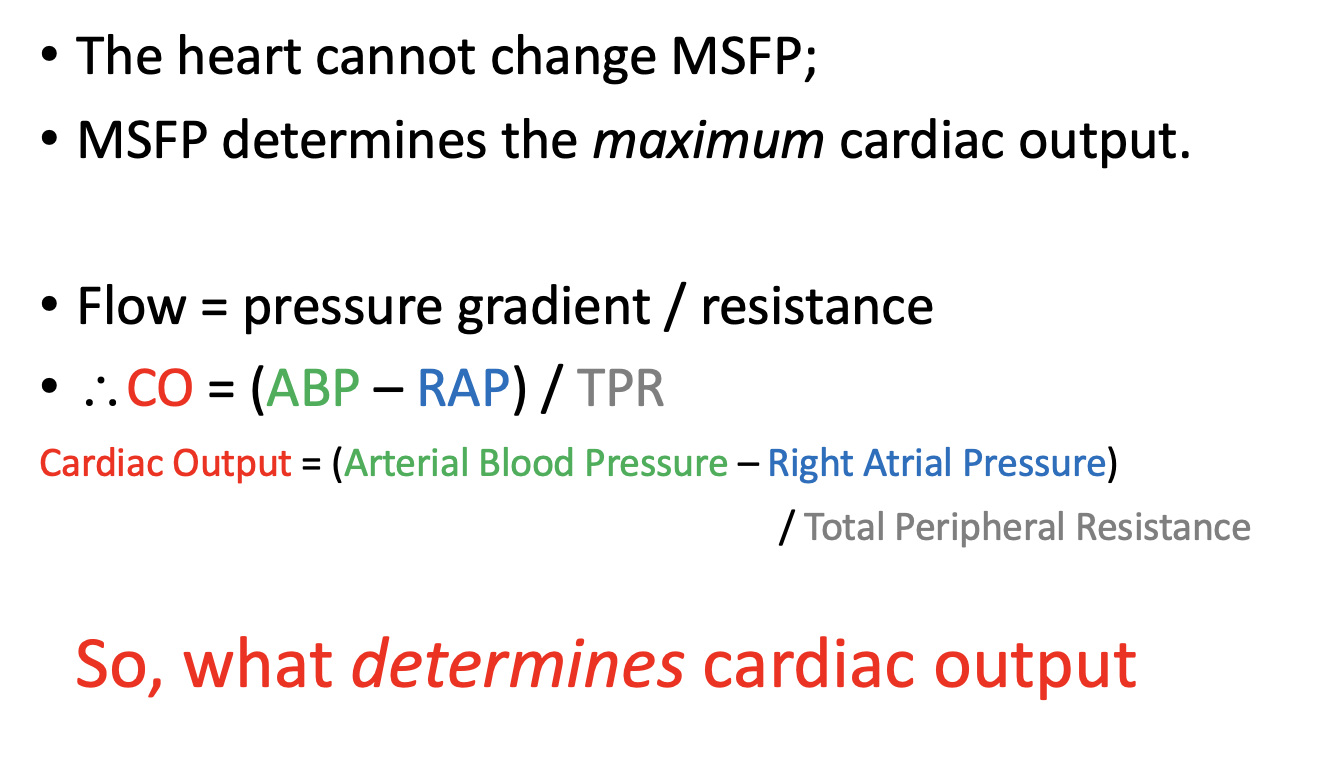
Arteriovenous pressure difference (ABP-RAP)
created by the action of the heart
limited by MSFP
TPR
‘lumped parameter’
treats all resistances as the varous vascular pathways as a single resistance
but
primarily determined by arteriolar resistances
RAP
usually so small compared to ABP
can often be omitted from the equation
How can CO be measured?
cannot be directl measured anywhere in the body
it is regulated to maintain ABP
The heart is able to respond to changing physiological need through…
intrinsic
and
extrinsic mechanisms
Intrinsix regulation of cardiac output: Starling’s ‘law of the heart’: Frank-Starling mechanism
Responsible for increasing CO when MSFP increases
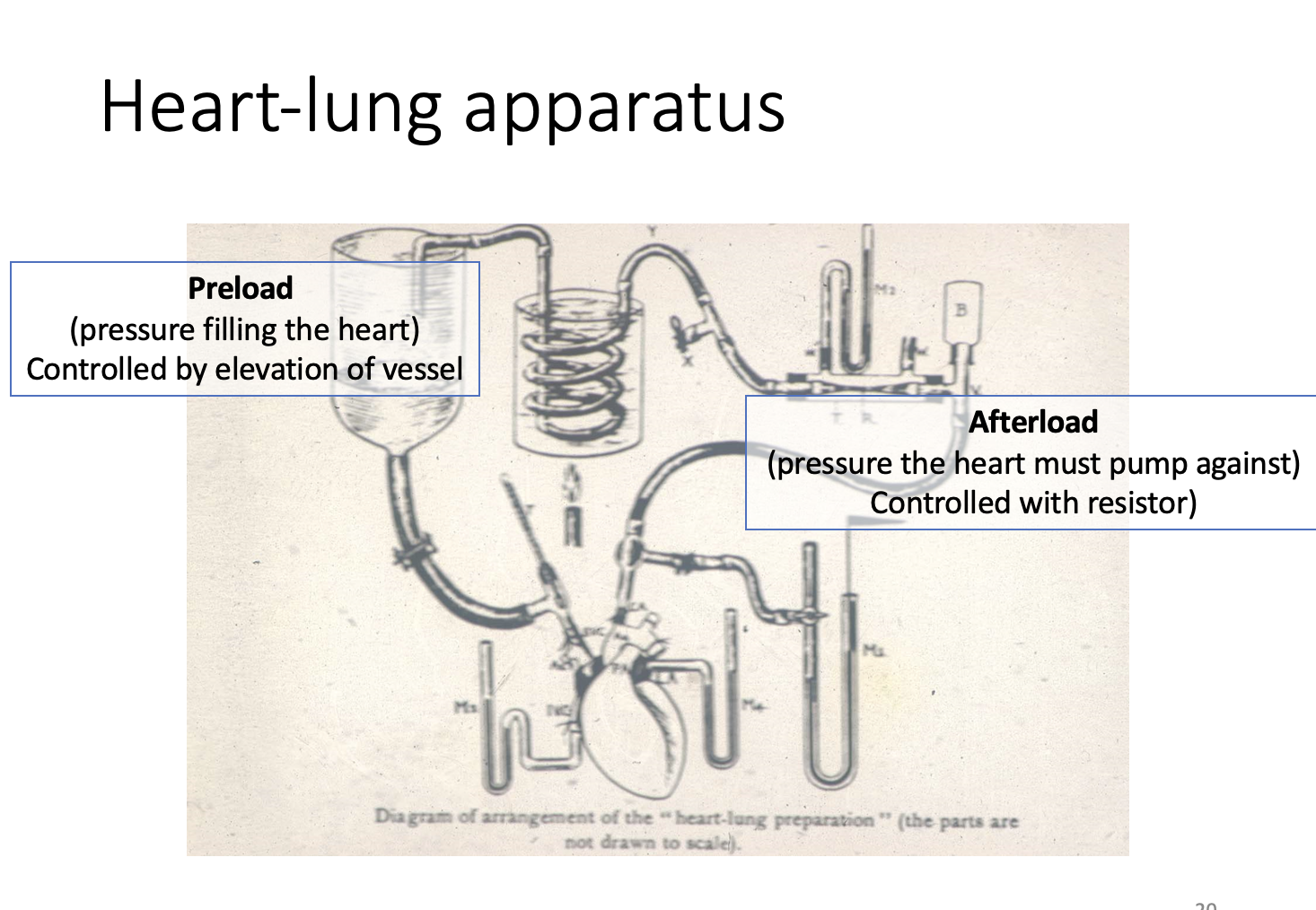
Preload and afterload
Preload→ right atrial pressure
Afterload→ arterial blood pressure
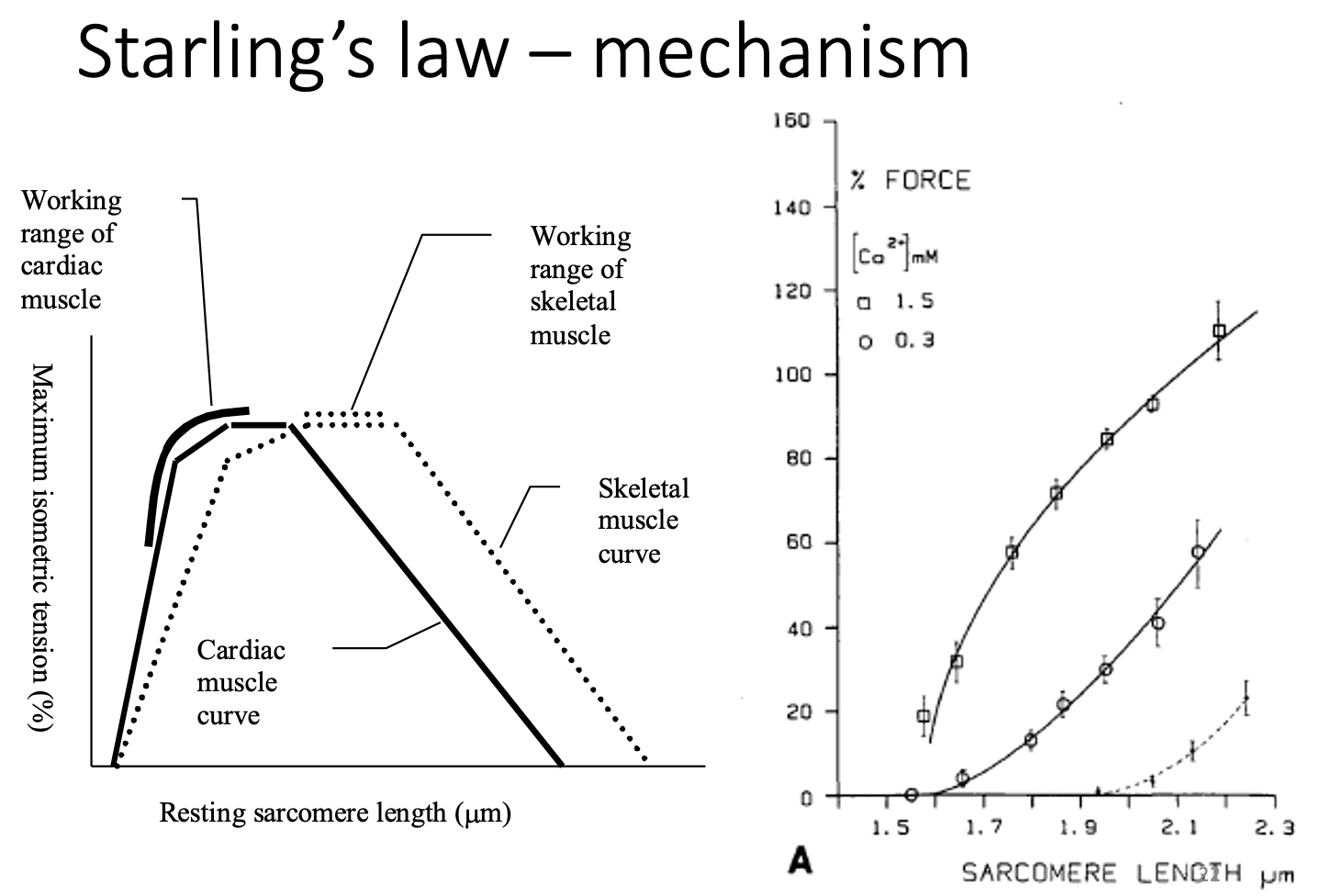
Increase in preload and afterload does what
stretches the cardiac muscle
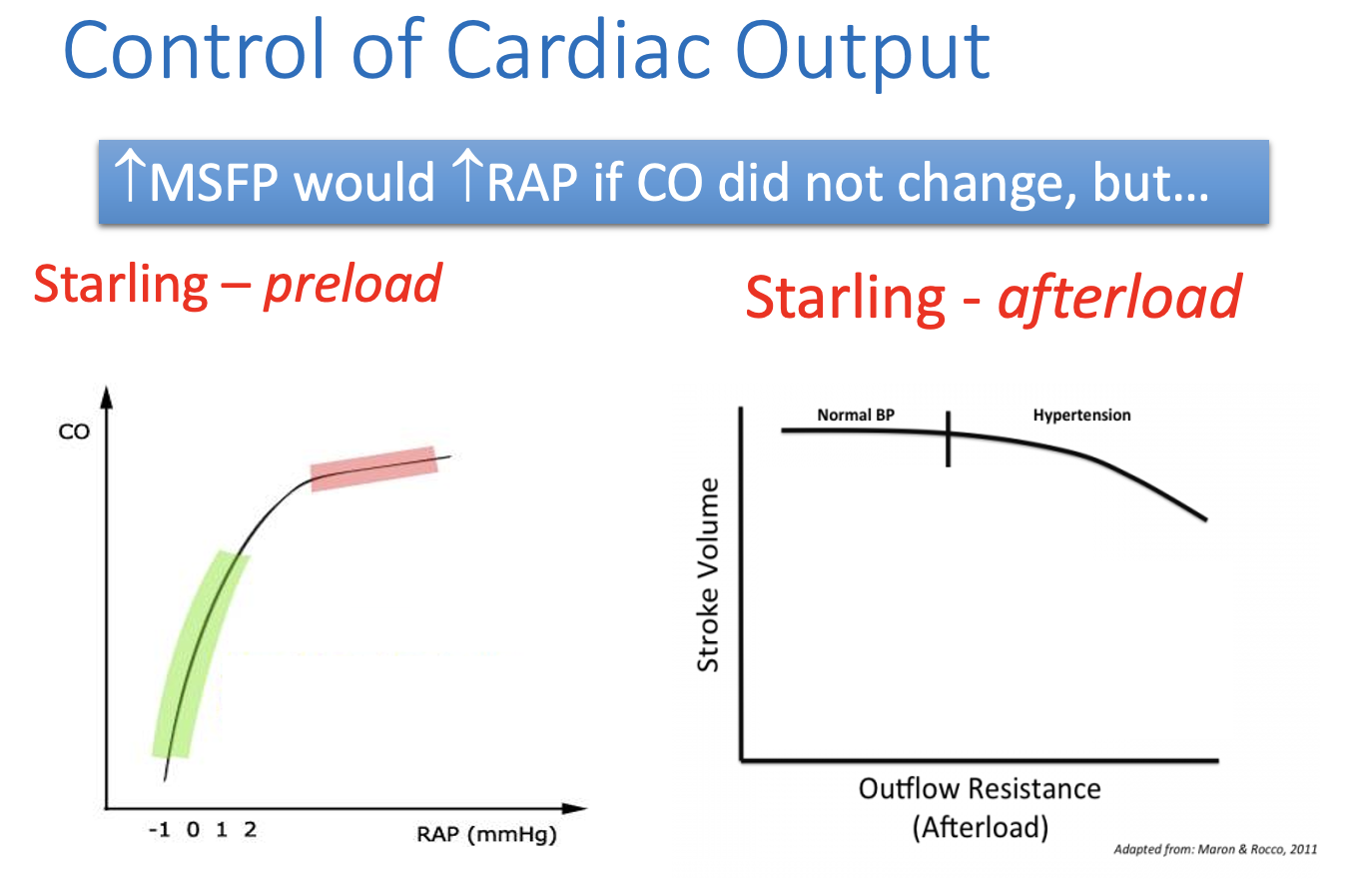
This increases the mycocardial contractile force by at least two mechanisms
stretching ardiac muslce incrases the overlap between myosin and actin filaments
→ allowing greater crossbridge formation
Stretch of cardiac muscle increases its sensitvity to Ca2+ such that greater force is produced at any given Ca2+ concentration
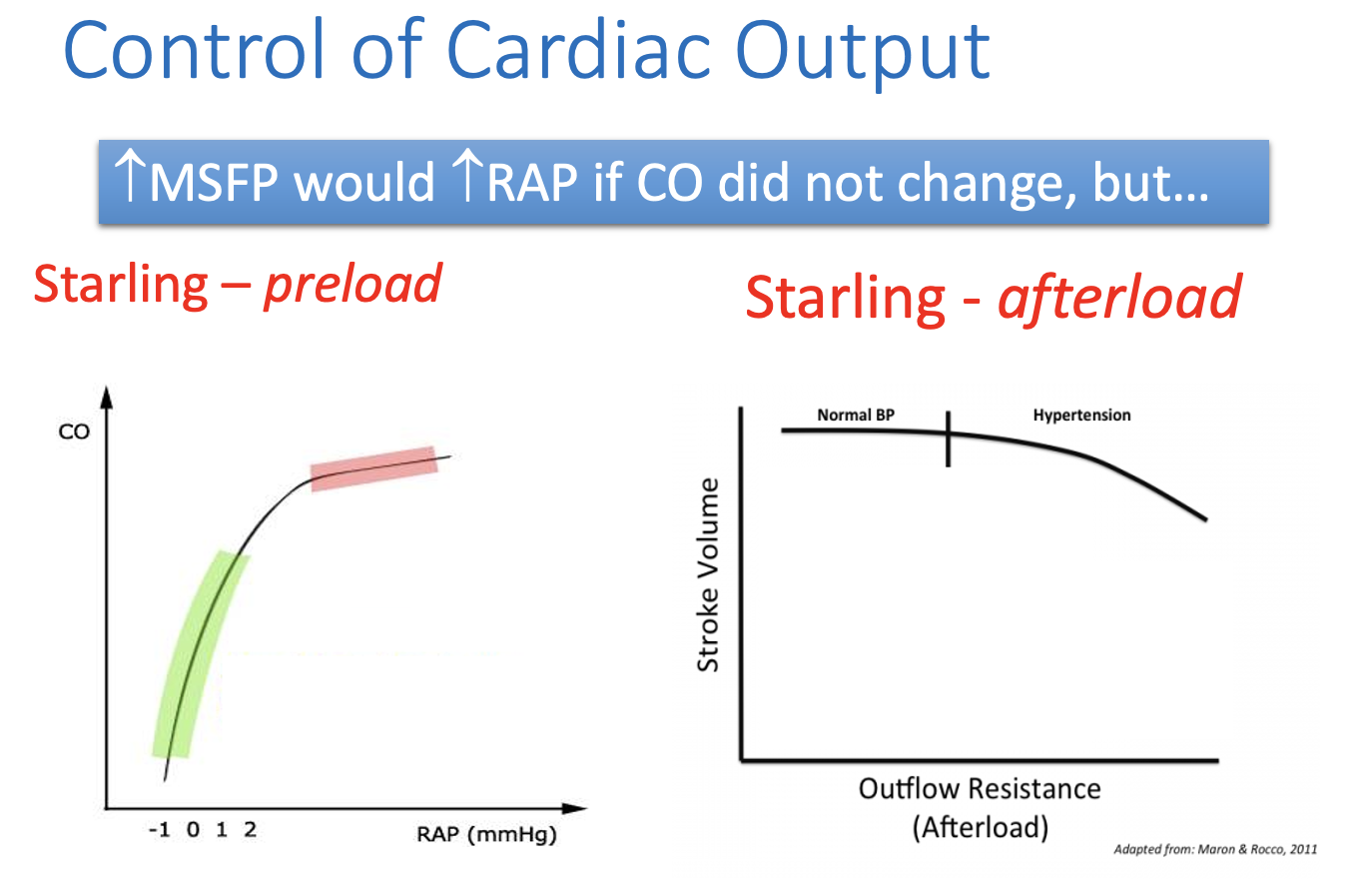
The steep response of the heart to increased RAP ensures that…
increased MSFP produces increased CO
The increase in myocardial contractility with increased afterload ensures that…
an increase in TPR
by generalised arteriolar vasoconstriction
does not reduce CO
instead: causes an increase in ABP because (ABP= COxTPR)
This is supported by evidence from miscrosphere experiments
microspheres injected into dogs bloack manny arterioles
more than doubling TPR
Result…
This did not reduce CO
THEREFORE: ABP more than doubled
RAP is therefore a key point of control in circulation…
If CO stayed constant
then an increase in MSFP would incrase RAP
Why does this happen?
the pressure would increase throughout the circulation
the greatest percentage increase would be at the right atrium
where pressure was initially lowest
However, in real life CO would…
not stay constant
from starling’s experiments we know
that the increased RAP
i.e increased pre-load)
will increase stroke volume and hence
CO (and ABP by ABP =CO x TPR)
Form figure 8, by considering Starling mechanism…
Increased MSFP causes increased CO under normal physiological conditions
Decrased MSFP decreases the maximum CO
This is why blood loss…
decreases blood pressure
And one reason why exericise is impaired by severe dehydration
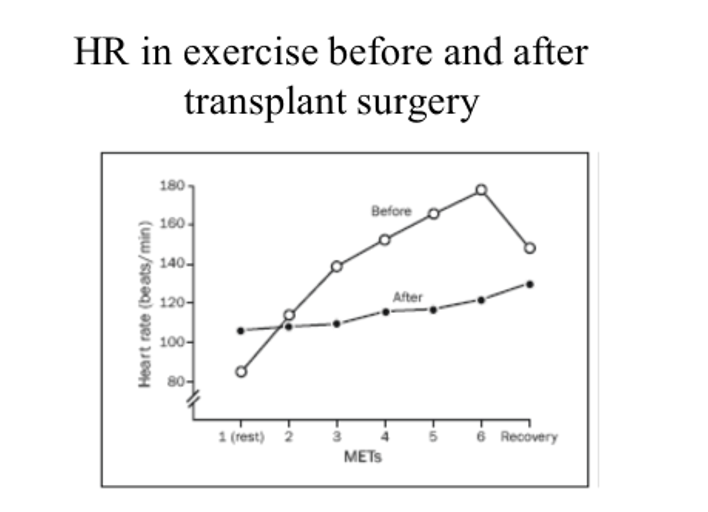
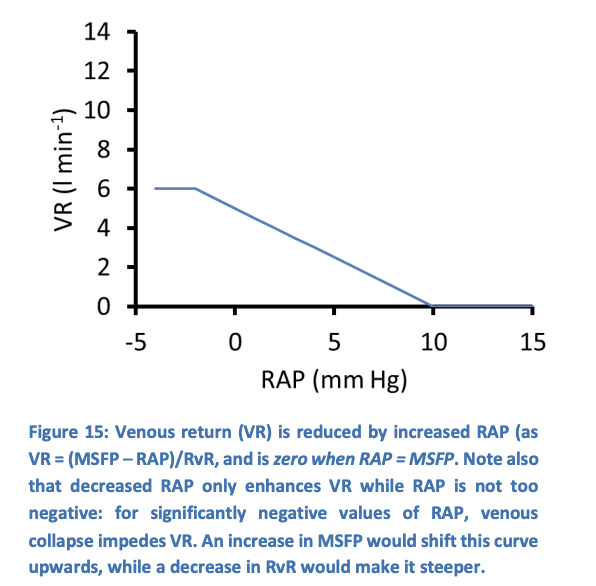
Extrinsic control of cardiac output: if heart rate changes in isolation…
stroke volume drops and cardiac outpute barely changes
→ the heart cannot ‘pull’ more blood from the veous system
However, increased heart rate in exercise…
facilitates increased cardiac output by shifting the curve CO vs RAP
In addition…
sympathetic stimulation
e.g during exercise
enhances Ca2+ entry
in diagram: transplant= sympatheic fibres are severed→ so it is the heart that is responding to exercise and not the symathetic but this shows that both are happening
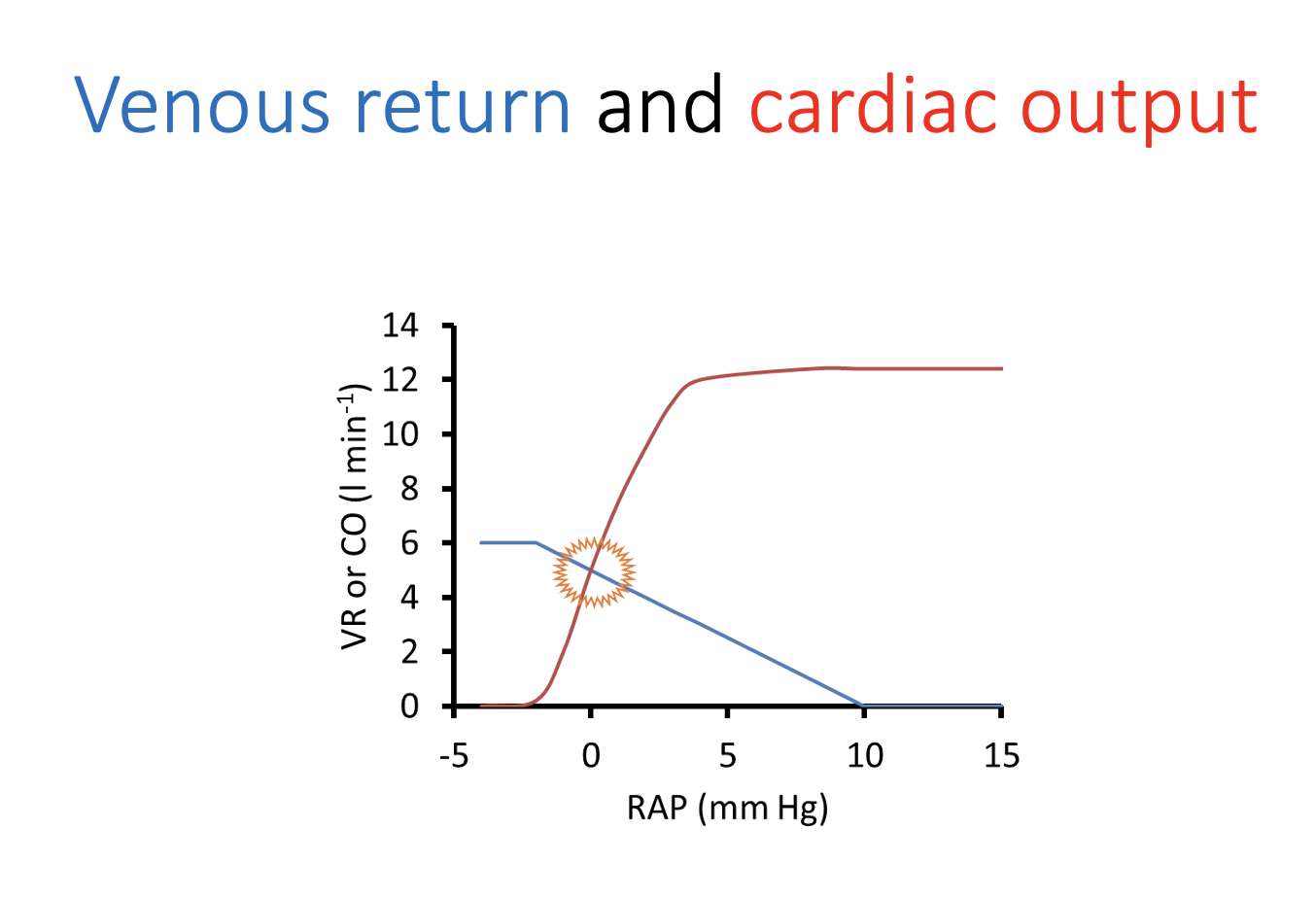
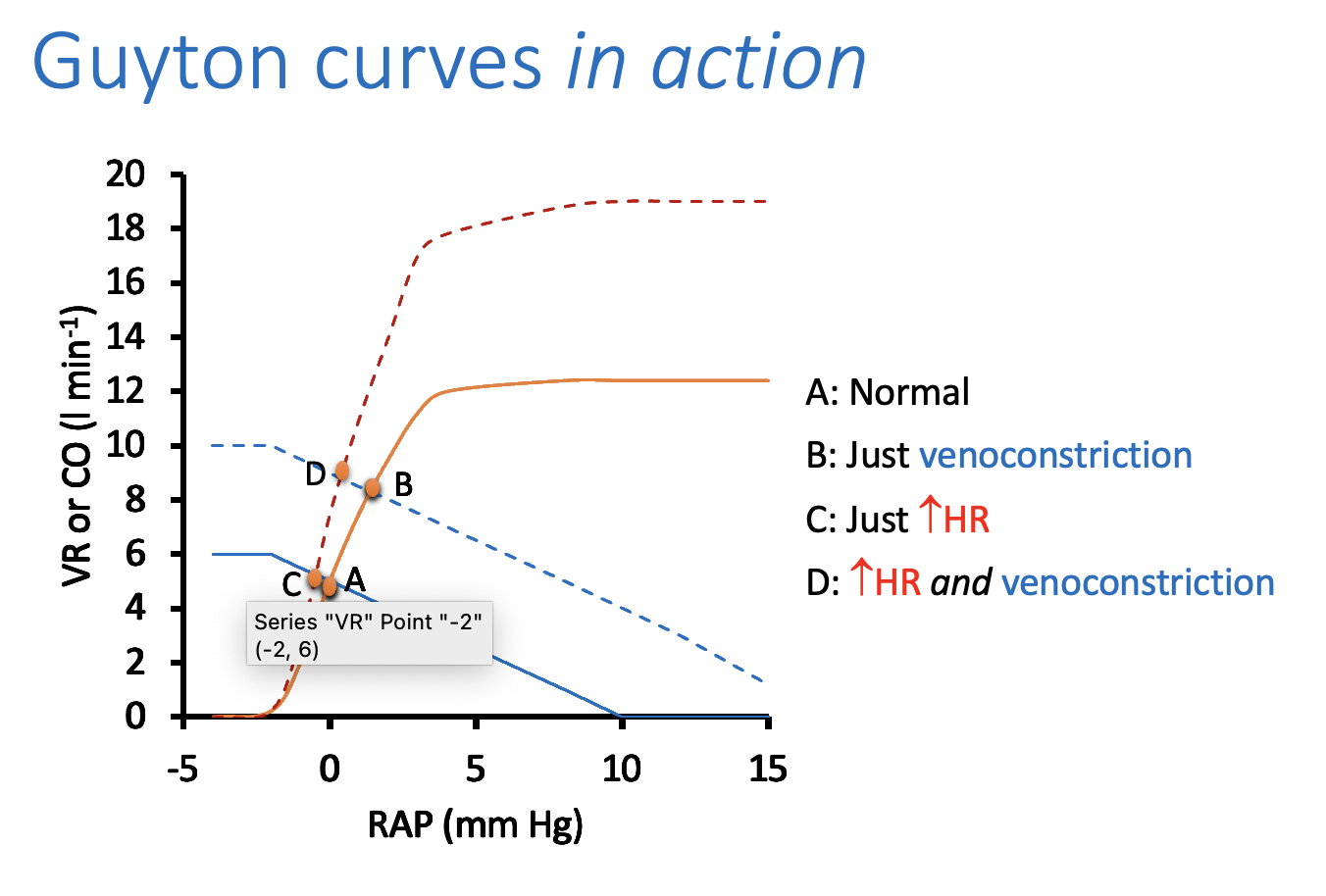
May be easier to look at the corculation in two parts: Guyton’s curves
part which pressure if above MSFP
part which pressure is below MSFP
Then we consider cardiac output and venous return separately (even though they must be equal)
Where TPR is the resistance prior to the ‘pivotal point’
where pressure = MSFP
RvR → resistance to venous return→ the reamining resistance
RvR is a bit of an oddity…
best to think of it as a term that reflects the difficulties blood has in returning to the heart
the fact that capillary pressure in the feet is insufficient to drive blood more than a meter upwards to the heart
so that venous return from the lower legs must wait for voluntary muscle movements to pump blood back
Therefore…
RvR can change→ expeically in exercise
but this is specifically regulated
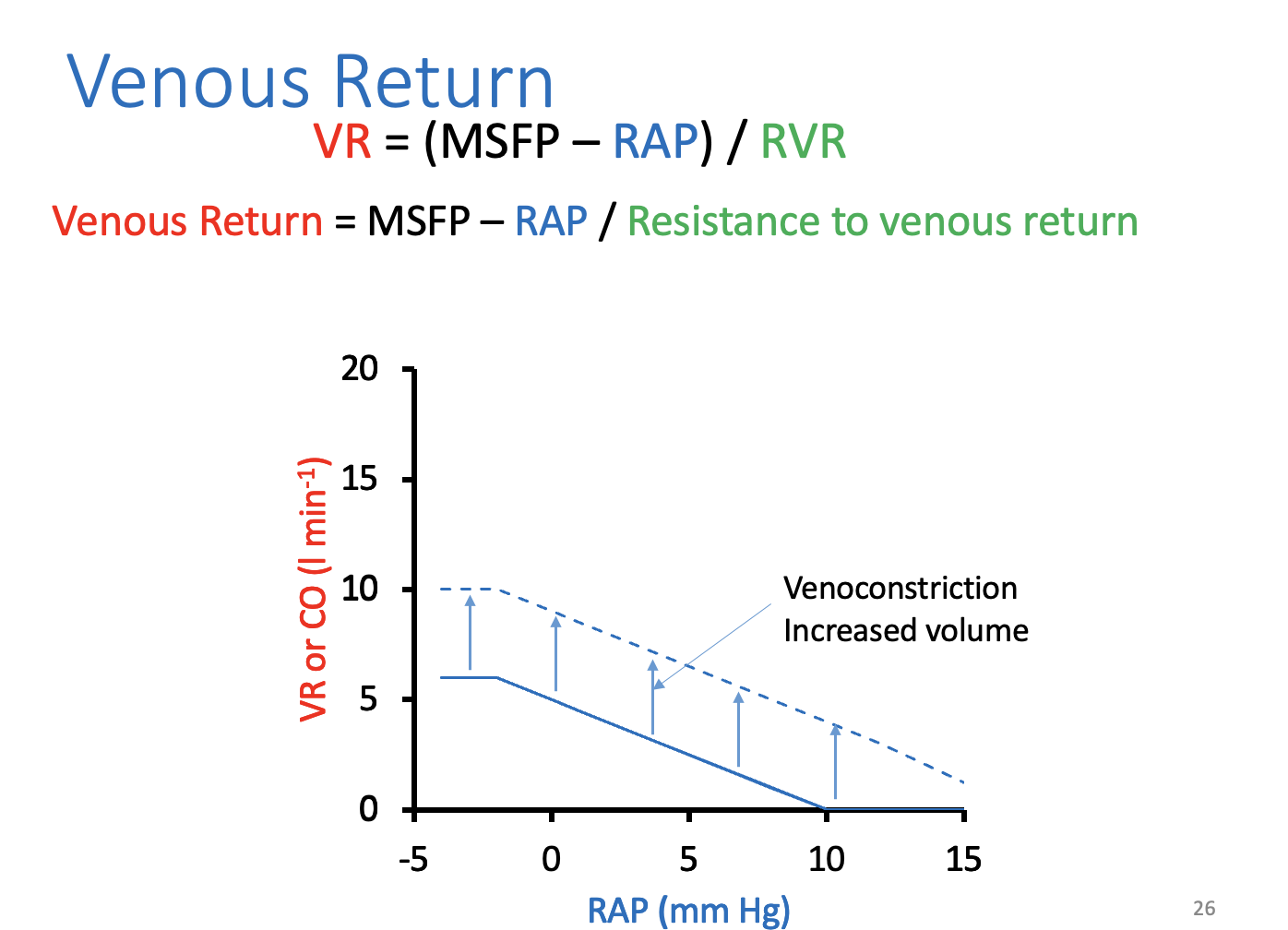
The venous return equation allows us to…
consider venous blood flow at different values of RAP
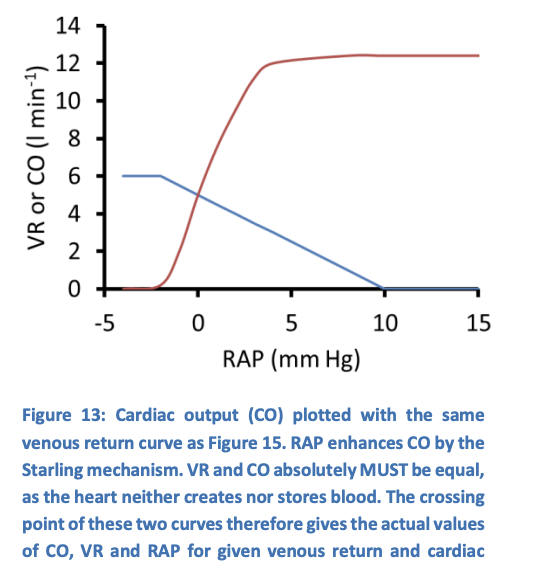
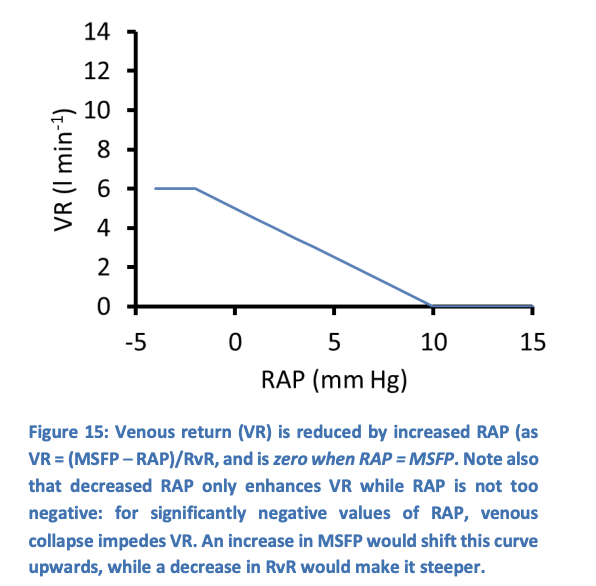
Figure 15 suggests that…
venous return drops as RAP increases:
The differencebetween MSFP nad RAP gets smaller
RAP at a venous return of 0→ which is the mean systemic filling pressure
Rasing MSFP by increasing circulating volume or venoconstriction would…
increase the slope without changing MSFP
i.e→ it would not change the intersection of the line with the X-axis
But RAP does not just influence venous return…
Starling mechanism→ incrased RAP increases cardiac output
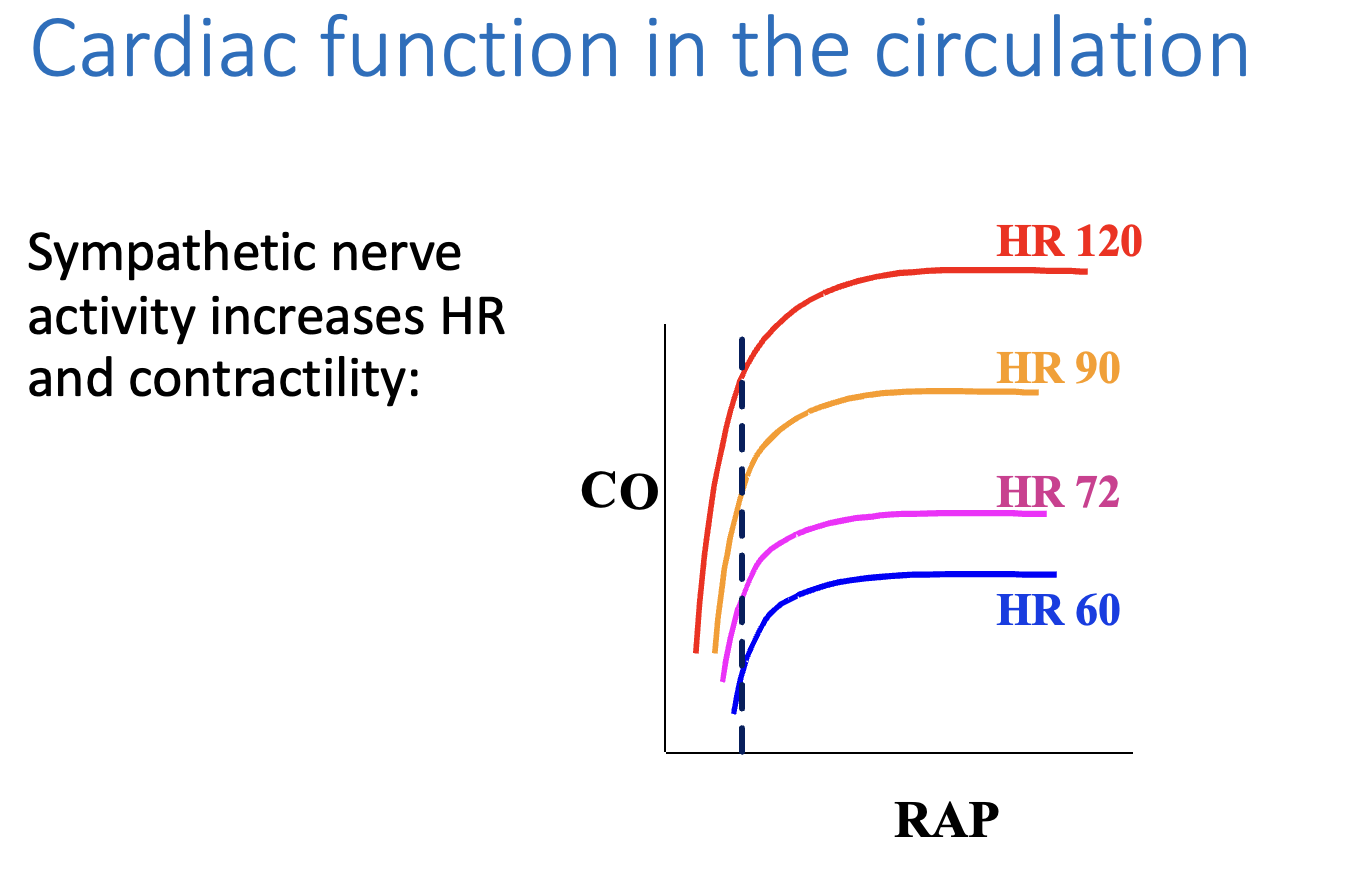
Cardiac output and venous return must be
The same
This is where the curves cross
for this system, at an RAP of 0mmHg and CO of 5 lmin'-1
If RAP was 5 mmHg…
CO would transiently exceed venous return
which would cause RAP to drop until VR and CO became equal again
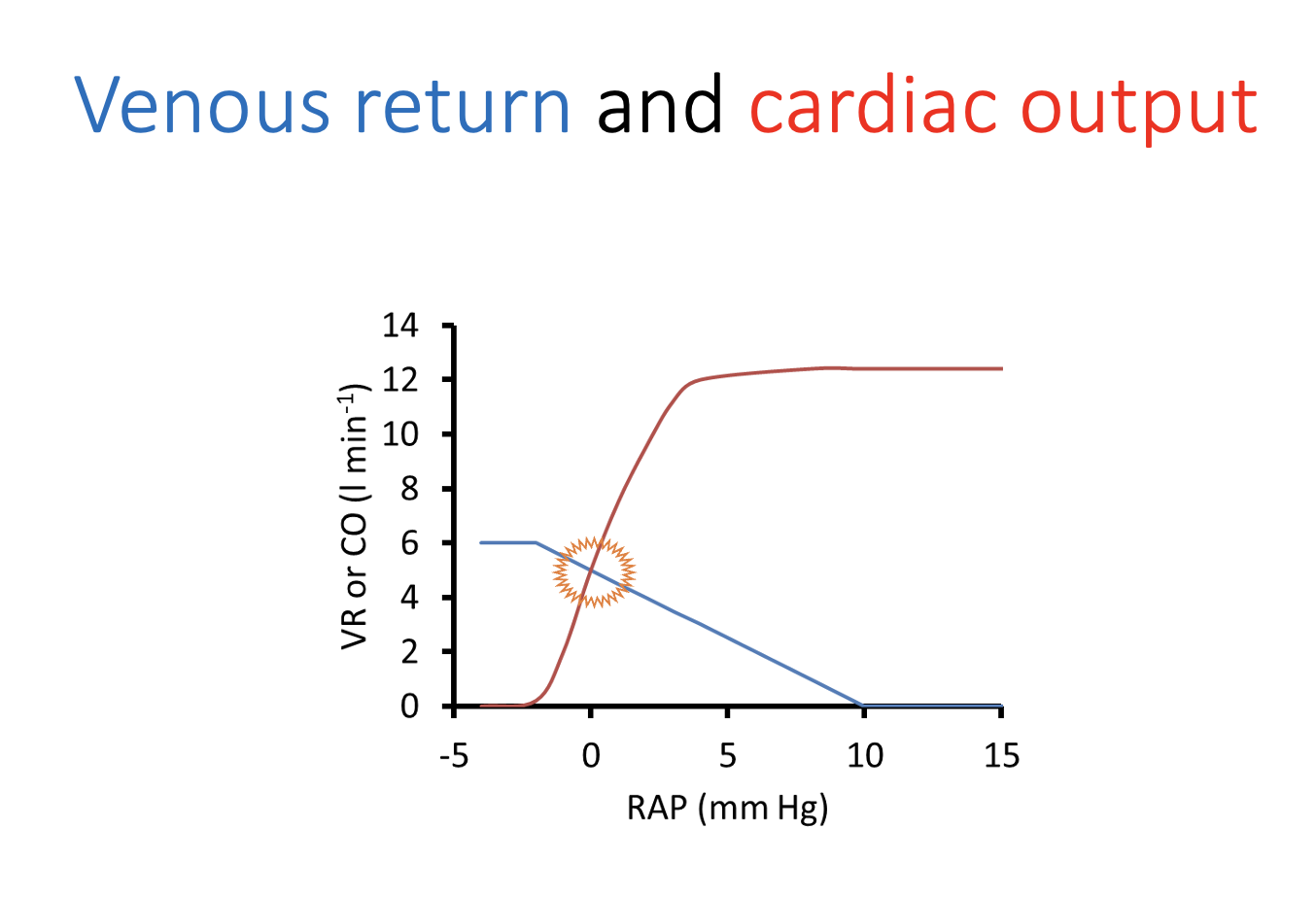
These curves are helpful because… guyton curves
MSFP only shifts
→ VR curve and TPR
or
changes in myocardial contracility only shift→ CO curve
What does figure 14 show: without stimulation
Considers two effects of sympathetic stimulation sparately
Without stimulation→ the system rests at a point A
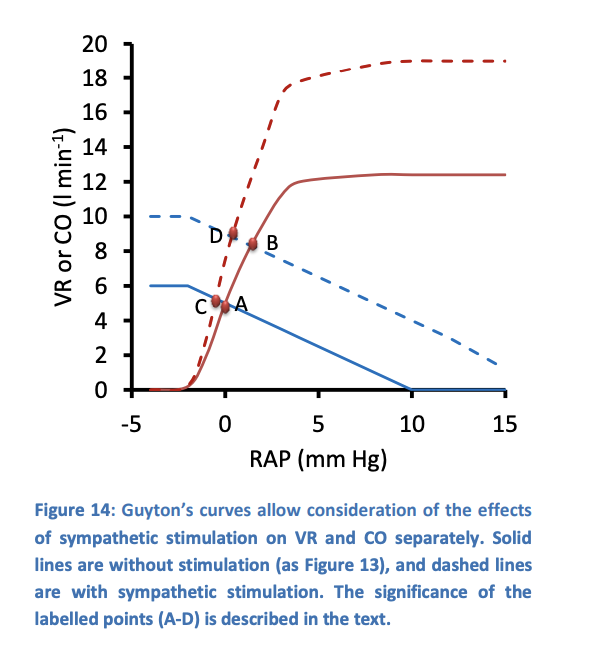
What does figure 14 show: with sympathetic venoconstriction
Symathetic venoconstriction→ increases MSFP
hence shifts the venous return curve higher at any RAP (as VR=MSFP-RAP)
this upward shift means:
for a moment
VR Exceeds CO
but this increases RAP
CO increases
system settles at point B→ raised RAP and raised CO
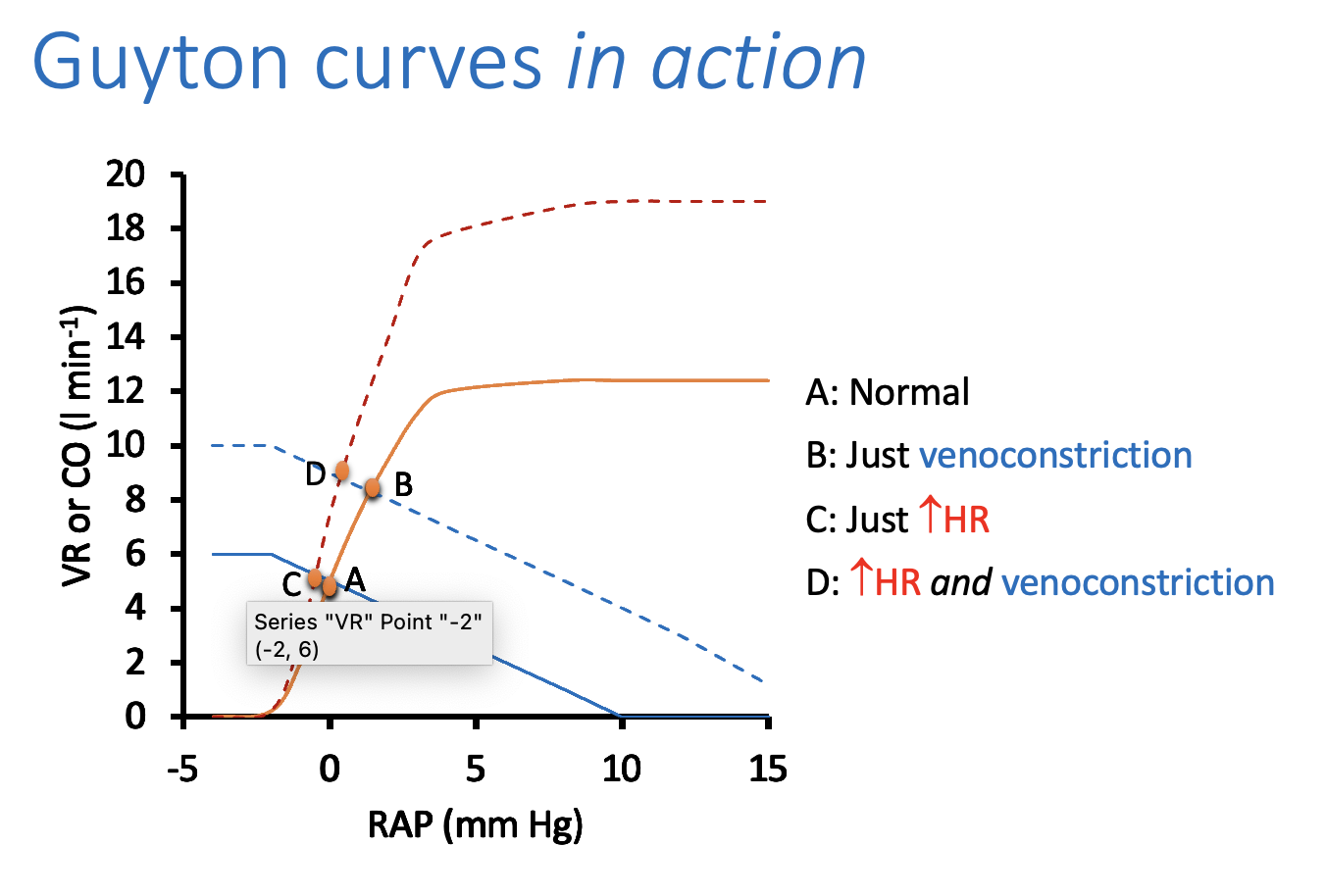
What does figure 14 show: with sympathetic sstimulation of heart only
cardiac output curve shift to igher outputs at any RAP
however:
as this drives RAP negative→ so the CO cannot incrase any further
the increase in CO is minimal to point C
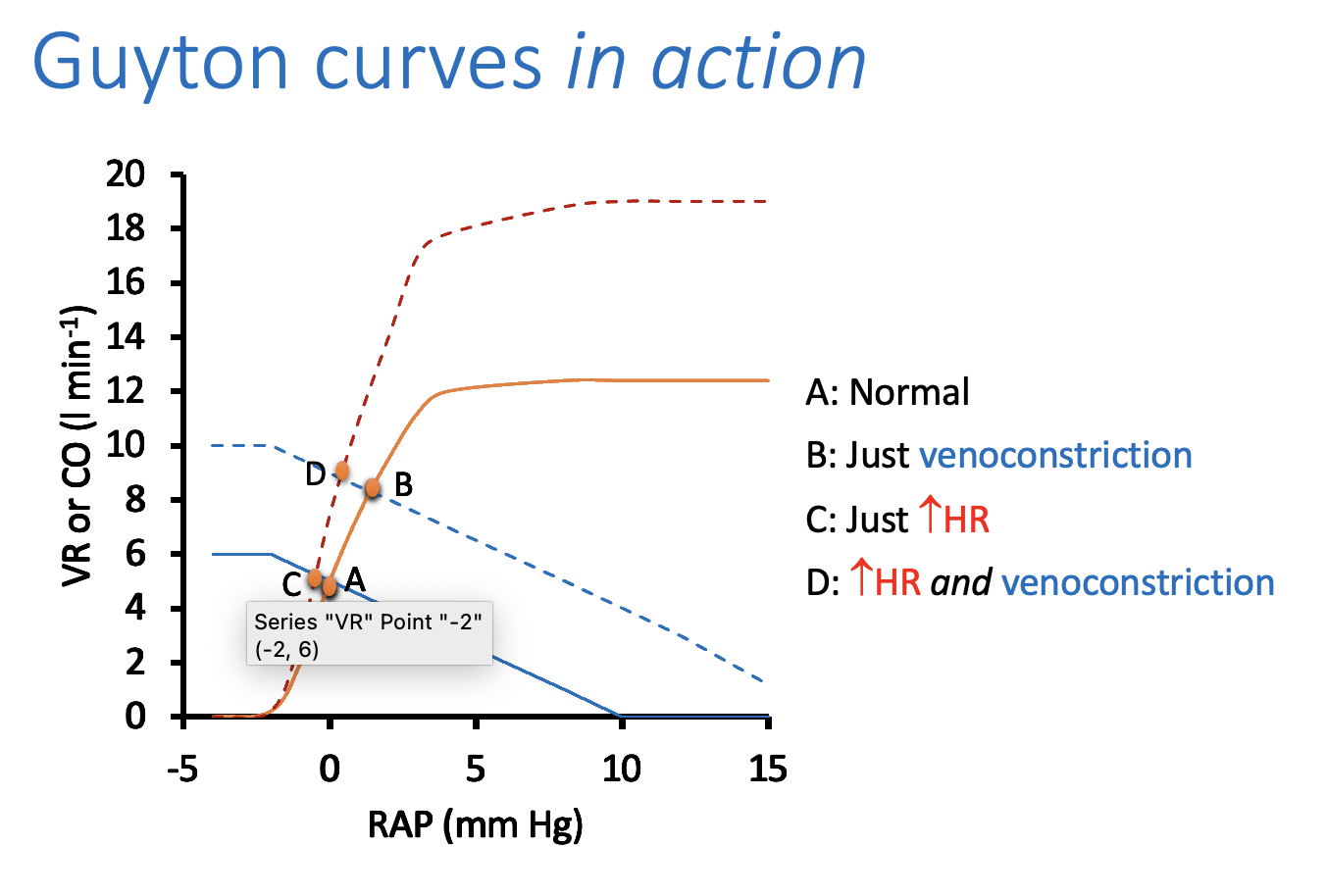
What does figure 14 show: with sympathetic sstimulation of heart AND venoconstriction (BOTH EFFECTS COMBINED)
the curve both overal at point D
a higher cardiac output with RAP remaining at zero
Why are guyton’s curves helpful
help in considering the effect of various changes to the circulation
e.g to imagine what would happen in heart was failing
Curves to imagine waht would happen in heart was failing:
→ CO reduced at every RAP:
result:
crossing point would slide down the VR curve
such that CO would reduce somewhat
RAP would increase significantly
However,
it should be clear that these curves are a simple model
it is also possible to think about th circulation in terms of a single pressure/flow relationship
But waht id he heart is unable to incrase output?→ Cardiac disease
→ will be considered next…