Chp 14 Urinary System
1/131
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
132 Terms
What is the primary function of the kidneys?
To maintain homeostasis by regulating the volume, electrolyte composition, and osmolarity of extracellular fluid (ECF).
How do the kidneys eliminate excess substances?
Through urine production, which can either eliminate or limit the loss of substances.
What is the minimum amount of urine the kidneys must produce daily?
500 mL of waste-filled urine.
What are the main functions of the kidneys?
Maintain water balance, osmolarity, plasma volume, acid-base balance, eliminate metabolic wastes, excrete foreign compounds, produce renin and erythropoietin, and convert vitamin D into its active form.
What structures make up the urinary system?
The kidneys, ureters, urinary bladder, and urethra.
What are the two main regions of the kidney?
The outer renal cortex and the inner renal medulla.
What is the nephron?
The functional unit of the kidney responsible for urine formation.
What are the two types of nephrons?
Cortical nephrons and juxtamedullary nephrons.
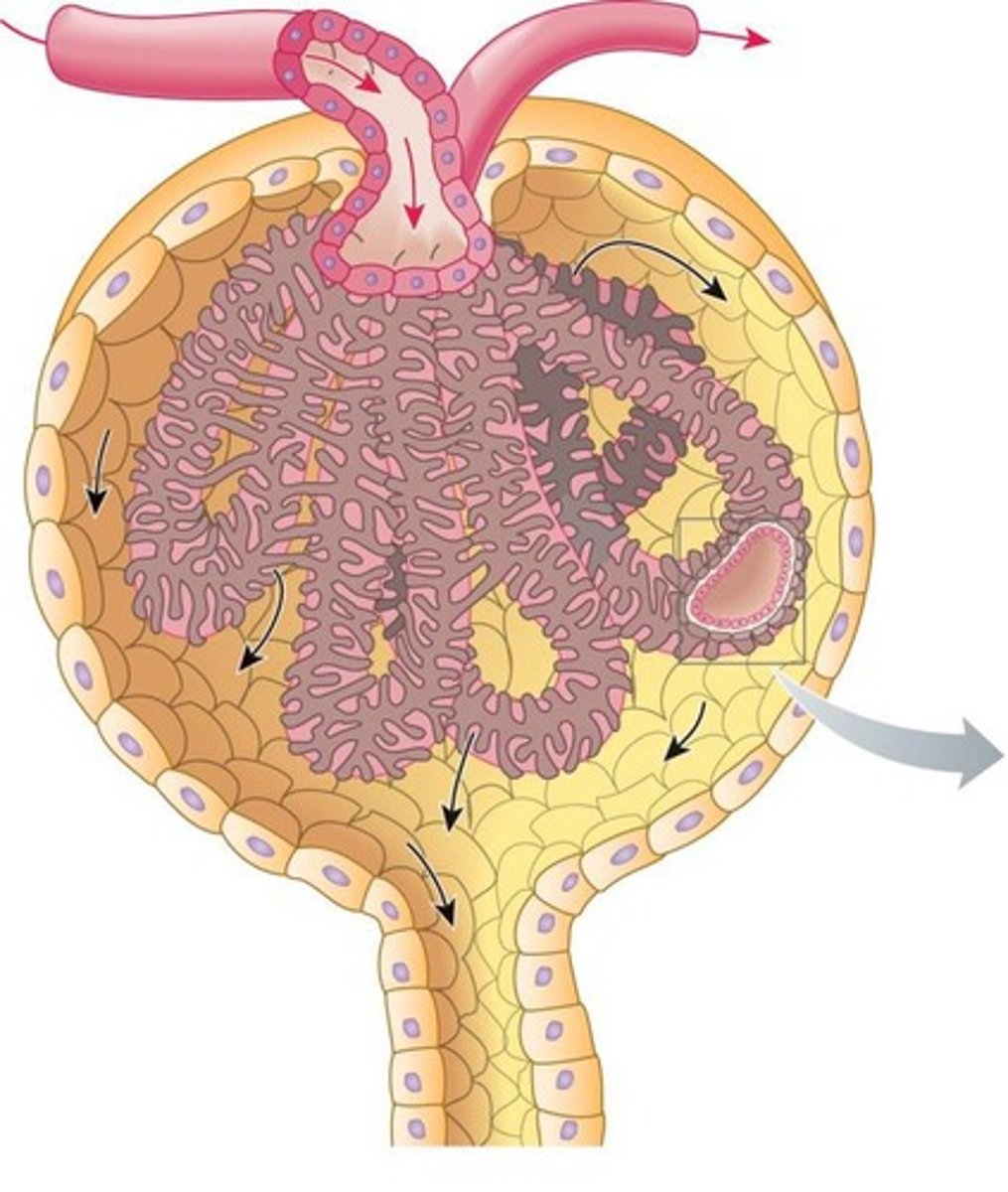
What is the role of the glomerulus in the nephron?
It filters protein-free plasma into the tubular component.
What is the process of glomerular filtration?
About 20% of the plasma entering the glomerulus is filtered through glomerular capillaries.
What occurs during tubular reabsorption?
Valuable substances are returned from the tubular lumen to the peritubular capillary plasma.
What is tubular secretion?
The selective transfer of substances from peritubular capillary blood into the tubular lumen.
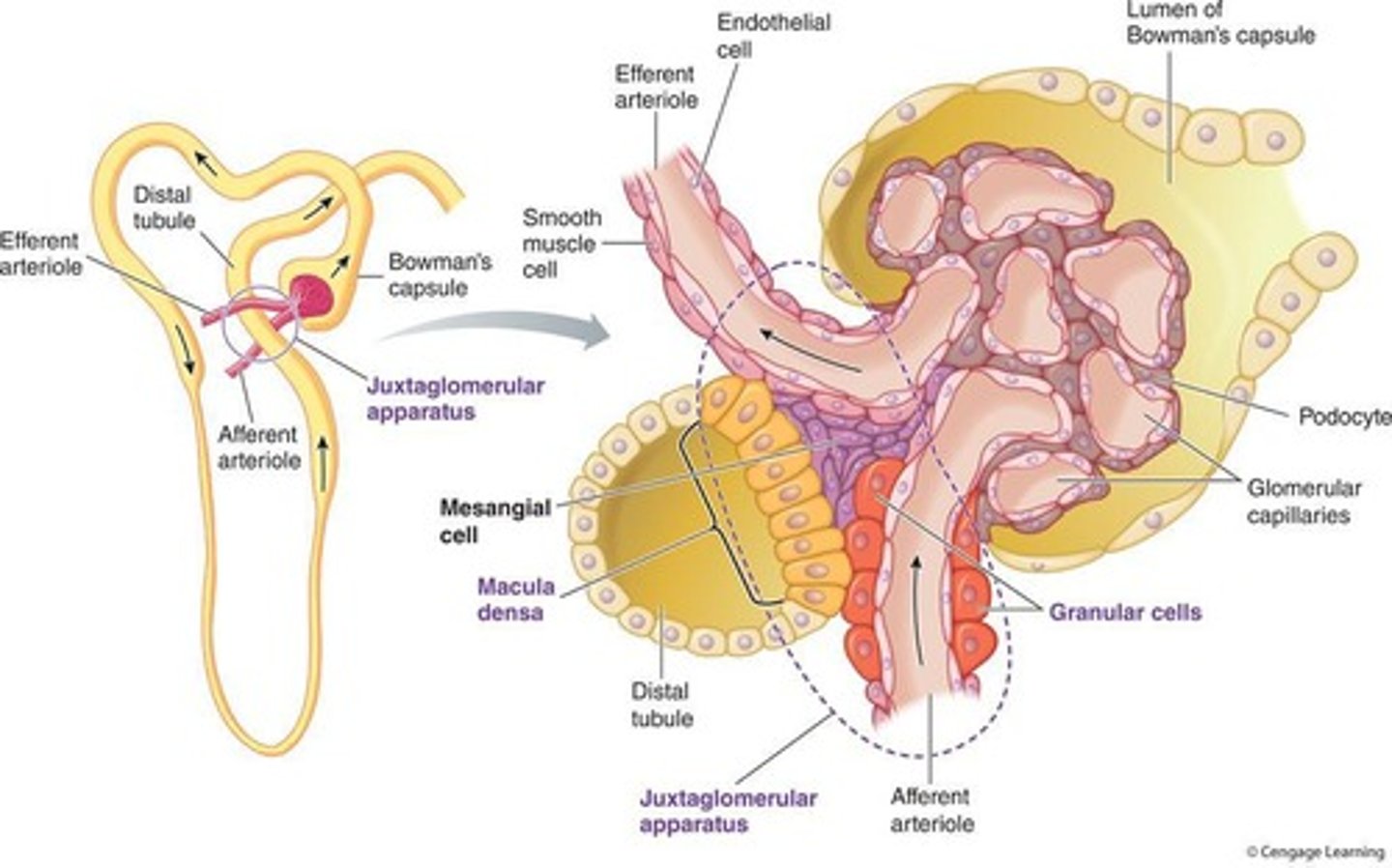
What is the significance of the juxtaglomerular apparatus?
It produces substances involved in the control of kidney function.
How much filtrate do the kidneys produce daily?
180 liters, with about 178.5 liters being reabsorbed.
What is the function of the loop of Henle?
It establishes an osmotic gradient in the renal medulla important for urine concentration.
What is the role of the collecting duct?
It allows for controlled reabsorption of sodium and water, and secretion of potassium and hydrogen ions.
What happens to the 80% of plasma that is not filtered through the glomerulus?
It leaves through the efferent arteriole.
What is the overall purpose of the renal processes?
To maintain the proper interstitial fluid environment for optimal cell function by regulating and excreting substances.
What is the function of erythropoietin produced by the kidneys?
It stimulates red blood cell production.
What is the role of renin in the kidneys?
It is involved in salt conservation and blood pressure regulation.
How do the kidneys help maintain acid-base balance?
By adjusting urinary output of hydrogen ions (H+) and bicarbonate.
What is the significance of maintaining osmolarity in body fluids?
It prevents detrimental shrinking or swelling of cells.
What is the renal pelvis?
The funnel-shaped structure that collects urine from the collecting ducts and channels it into the ureter.
What is the role of peritubular capillaries?
They supply renal tissue and are involved in exchanges with the fluid in the tubular lumen.
What is the function of Bowman's capsule?
It collects the glomerular filtrate.
What are the three layers of the glomerular membrane?
1. Glomerular capillary wall (fenestrated endothelial cells), 2. Basement membrane (collagen and glycoproteins), 3. Inner layer of Bowman's capsule (podocytes).
What is the function of the glomerular capillary wall?
It consists of a single layer of perforated endothelial cells with large pores, making it 100 times more permeable than other capillaries.
What role does the basement membrane play in glomerular filtration?
It provides structural strength and discourages the filtration of small plasma proteins like albumin.
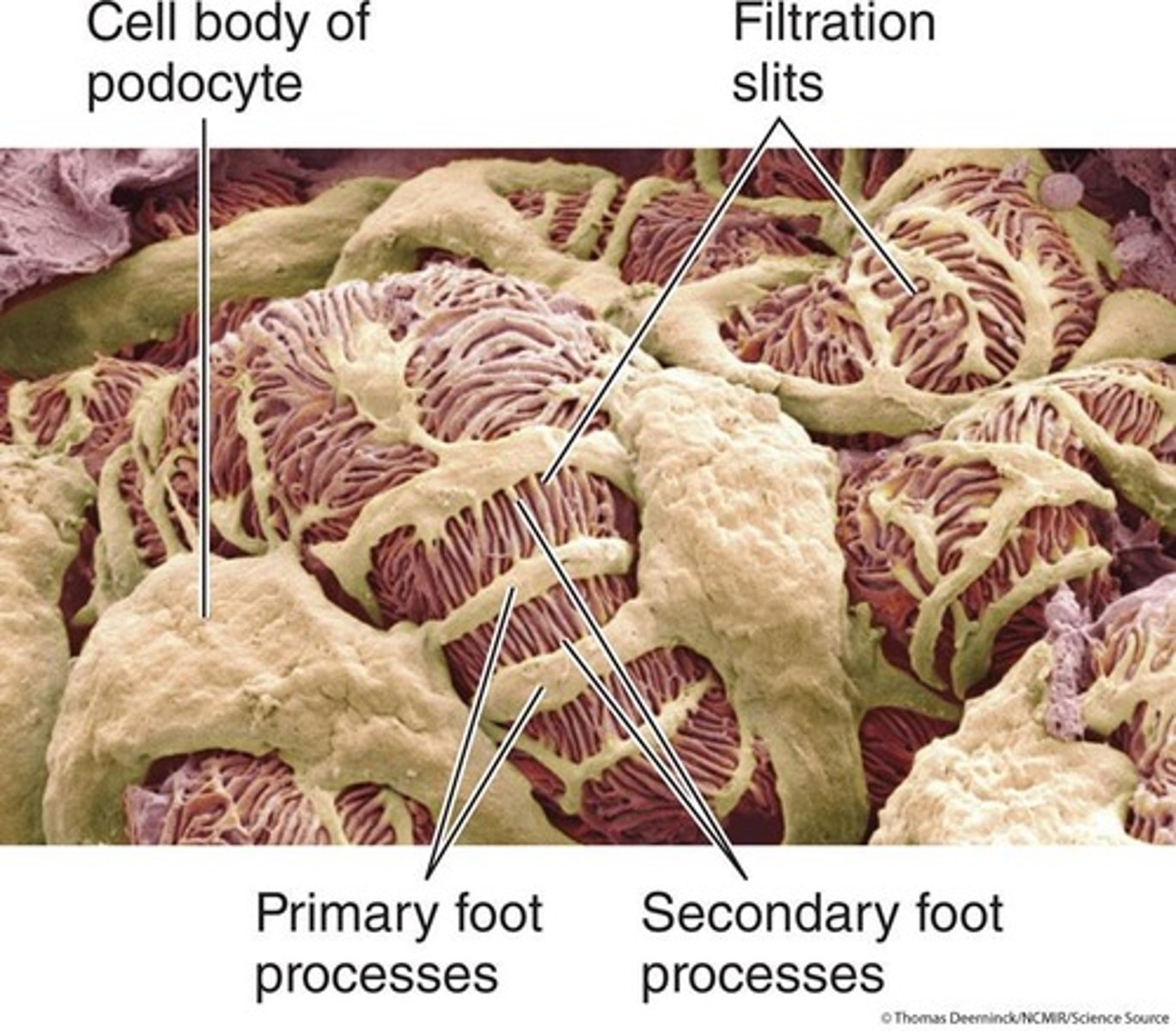
What are podocytes and their function in the glomerulus?
Podocytes are octopus-like epithelial cells that encircle the glomerulus and form filtration slits that can be adjusted in size.
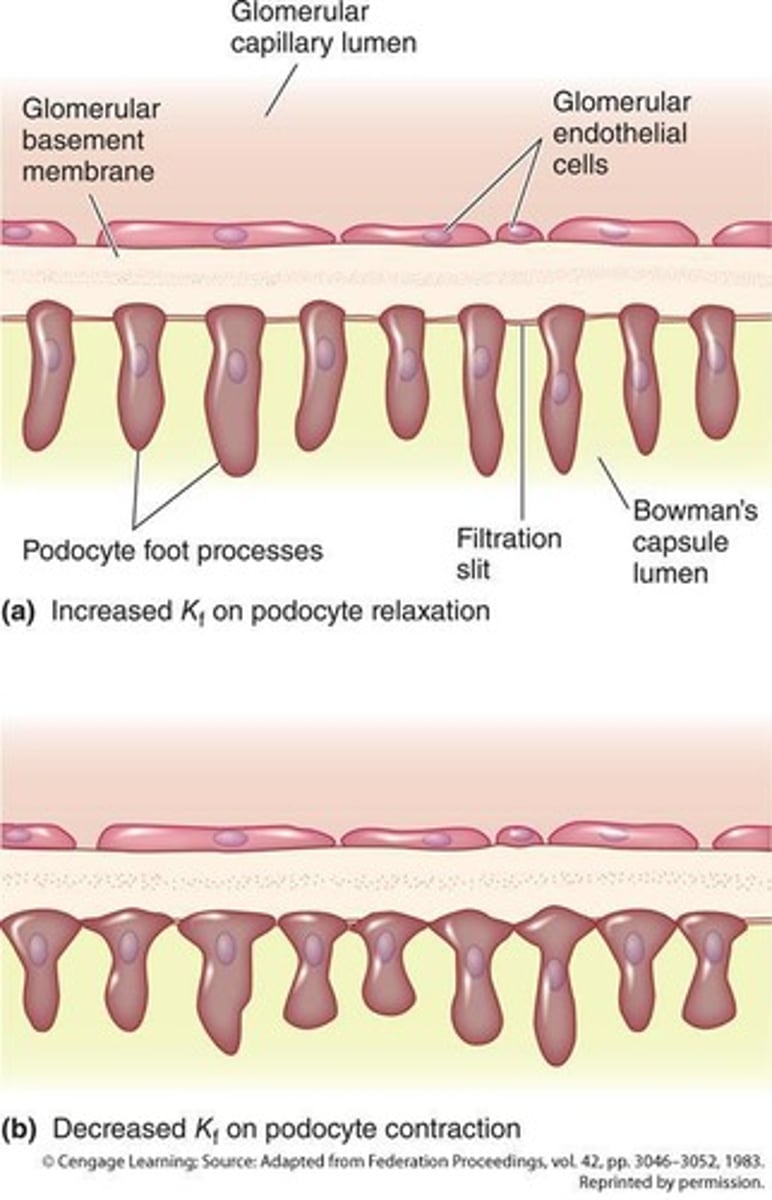
What must a substance pass through to be filtered in the glomerulus?
1. Pores between endothelial cells, 2. Acellular basement membrane, 3. Filtration slits between podocyte foot processes.
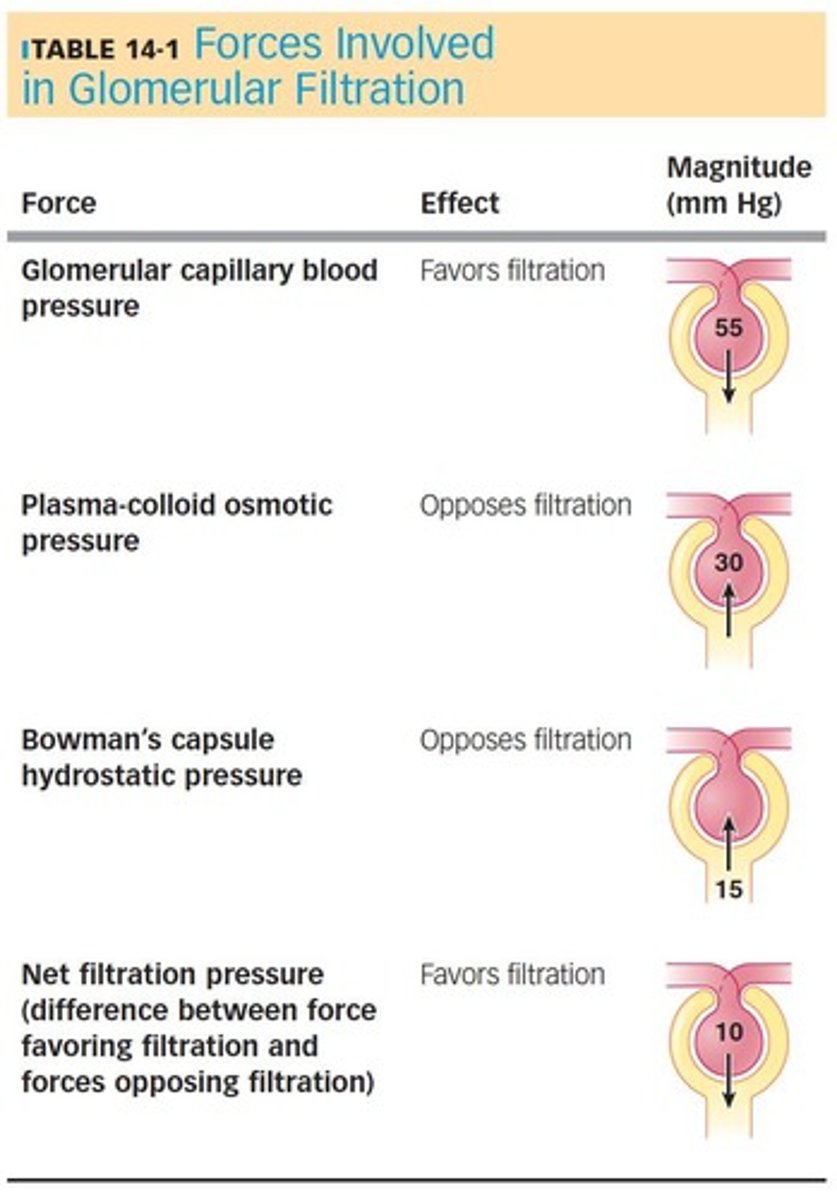
What is the primary force driving glomerular filtration?
Glomerular capillary blood pressure, which is the fluid pressure exerted by blood within the glomerular capillaries.
What opposes glomerular filtration?
1. Plasma-colloid osmotic pressure (due to plasma proteins), 2. Bowman's capsule hydrostatic pressure (fluid pressure in the tubule).
How is the glomerular filtration rate (GFR) calculated?
GFR = Kf x NFP, where Kf is the filtration coefficient and NFP is the net filtration pressure.
What factors influence the glomerular filtration rate?
GFR depends on net filtration pressure, glomerular surface area, and permeability.
What are the two major control mechanisms for adjusting GFR?
1. Autoregulation, 2. Extrinsic sympathetic control.
What is autoregulation of GFR?
Intrinsic mechanisms initiated by the kidneys to maintain GFR despite changes in arterial blood pressure.
What is the myogenic mechanism in autoregulation?
A smooth muscle property where the afferent arteriole constricts in response to being stretched.
What is the tubuloglomerular feedback mechanism?
It involves the juxtaglomerular apparatus detecting changes in salt levels and adjusting the afferent arteriole's diameter accordingly.
What is the importance of autoregulation in the kidneys?
It prevents excessive water and solute loss during exercise and maintains filtration when blood pressure drops.
How does extrinsic sympathetic control affect GFR?
It can intentionally change GFR by reducing urine output in response to decreased plasma volume.
What is the role of the baroreceptor reflex in GFR control?
It mediates sympathetic vasoconstriction in arterioles, affecting blood flow and GFR.
How can changes in the filtration coefficient influence GFR?
Filtration coefficient, which depends on surface area and permeability, can be modified by contraction of mesangial cells and podocytes.
What happens when mesangial cells contract?
They close off portions of filtering capillaries, reducing the surface area available for filtration.
What effect does podocyte contraction have on filtration?
It decreases the number of open filtration slits, reducing permeability.
What percentage of cardiac output do the kidneys receive?
20% to 25%
What is the primary function of the kidneys despite their small body weight?
To perform regulatory and excretory functions on large volumes of plasma.
What is tubular reabsorption?
The process that allows essential materials filtered by the kidneys to return to the blood.
What percentage of filtered water is reabsorbed by the kidneys?
About 99%
What percentage of filtered sugar is reabsorbed?
100%
What percentage of filtered salt is reabsorbed?
99.5%
What are the five barriers involved in transepithelial transport during tubular reabsorption?
1. Luminal membrane of tubular cell 2. Cytosol 3. Basolateral membrane 4. Interstitial fluid 5. Capillary wall
What is the difference between passive and active reabsorption?
Passive reabsorption occurs down gradients without energy, while active reabsorption requires energy against gradients.
What is the role of sodium (Na+) in tubular reabsorption?
Na+ reabsorption is crucial for reabsorbing glucose, amino acids, water, and chloride.
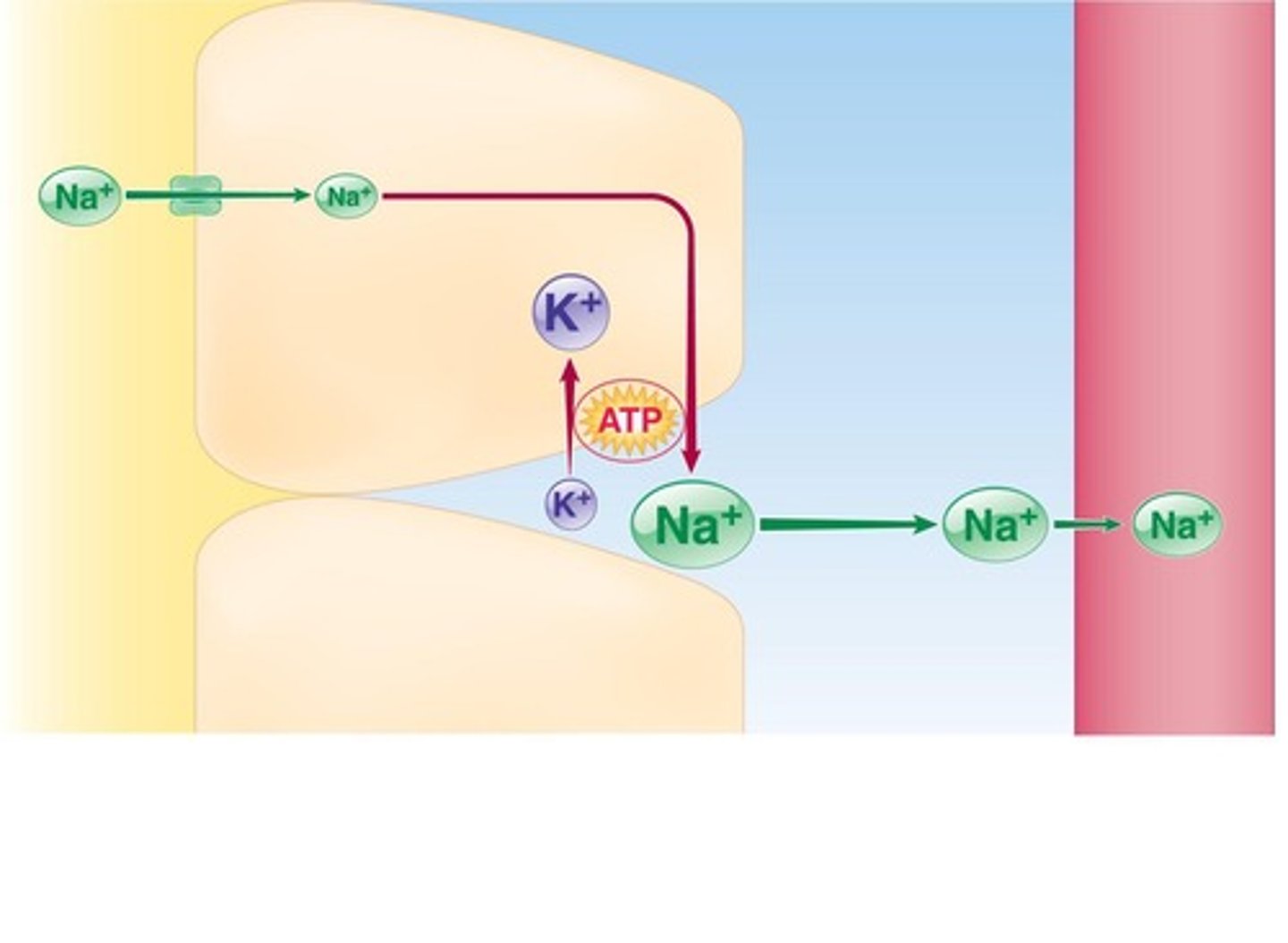
What percentage of Na+ is reabsorbed in the proximal tubule?
67%
What percentage of Na+ is reabsorbed in the loop of Henle?
25%
What percentage of Na+ is reabsorbed in the distal and collecting tubules?
8%
How does the Na+-K+ ATPase pump function in the kidneys?
It actively extrudes Na+ from the cell, maintaining a concentration gradient for reabsorption.
What hormonal system regulates Na+ reabsorption?
The renin-angiotensin-aldosterone system (RAAS).
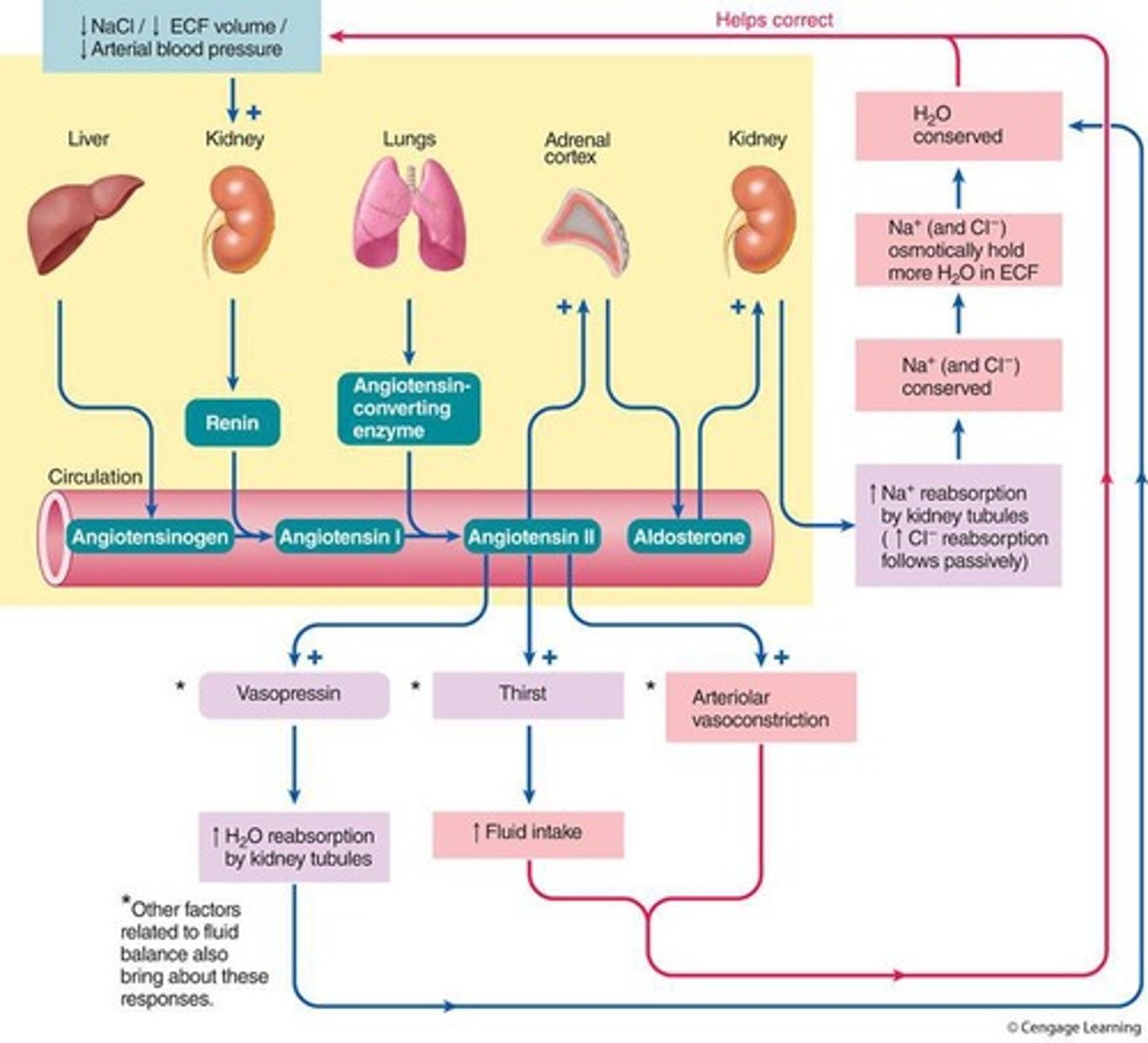
What triggers the secretion of renin in the kidneys?
A fall in NaCl, ECF volume, and arterial blood pressure.
What effect does aldosterone have on Na+ reabsorption?
It increases Na+ reabsorption by inserting additional channels and pumps in the principal cells.
What are principal cells and intercalated cells in the kidneys?
Principal cells are involved in Na+ and water reabsorption, while intercalated cells are involved in acid-base balance.
What is the impact of increased RAAS activity on health?
It can lead to hypertension and fluid retention in conditions like congestive heart failure.
What are diuretics and how do they affect the kidneys?
Diuretics increase urine production by inhibiting tubular reabsorption of Na+.
What is the relationship between Na+ reabsorption and blood pressure?
Changes in Na+ levels affect blood volume and pressure due to osmotic activity.
What is the significance of sodium reabsorption in the distal and collecting tubules?
It is variable and subject to hormonal control, helping to regulate extracellular fluid volume.
What is the role of sodium reabsorption in the ascending limb of the loop of Henle?
It plays a key role in reabsorbing chloride and urine concentration.
How does the Na+-K+ ATPase pump create a concentration gradient?
By actively extruding Na+ from the tubular cells, allowing passive transport from the tubular lumen.
What hormones oppose the effects of the RAAS on sodium reabsorption?
Atrial natriuretic peptide (ANP) and brain natriuretic peptide (BNP)
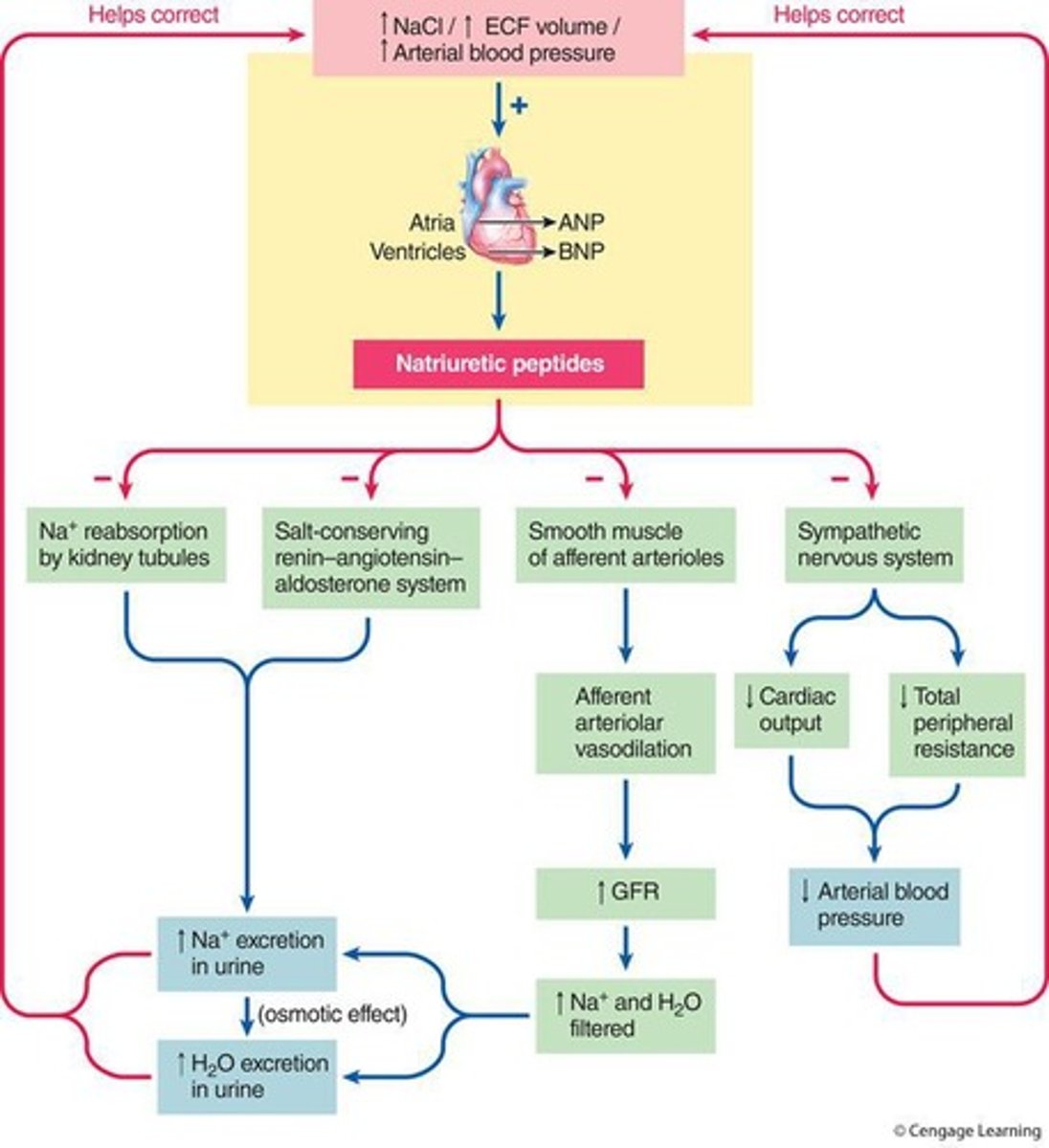
What is the process called that involves the excretion of large amounts of sodium in urine?
Natriuresis
Where are sodium and glucose cotransporters (SGLT) located in the kidney?
In the proximal tubule
What is the function of glucose transporters (GLUT) in the kidneys?
Facilitates passive diffusion of glucose into the plasma
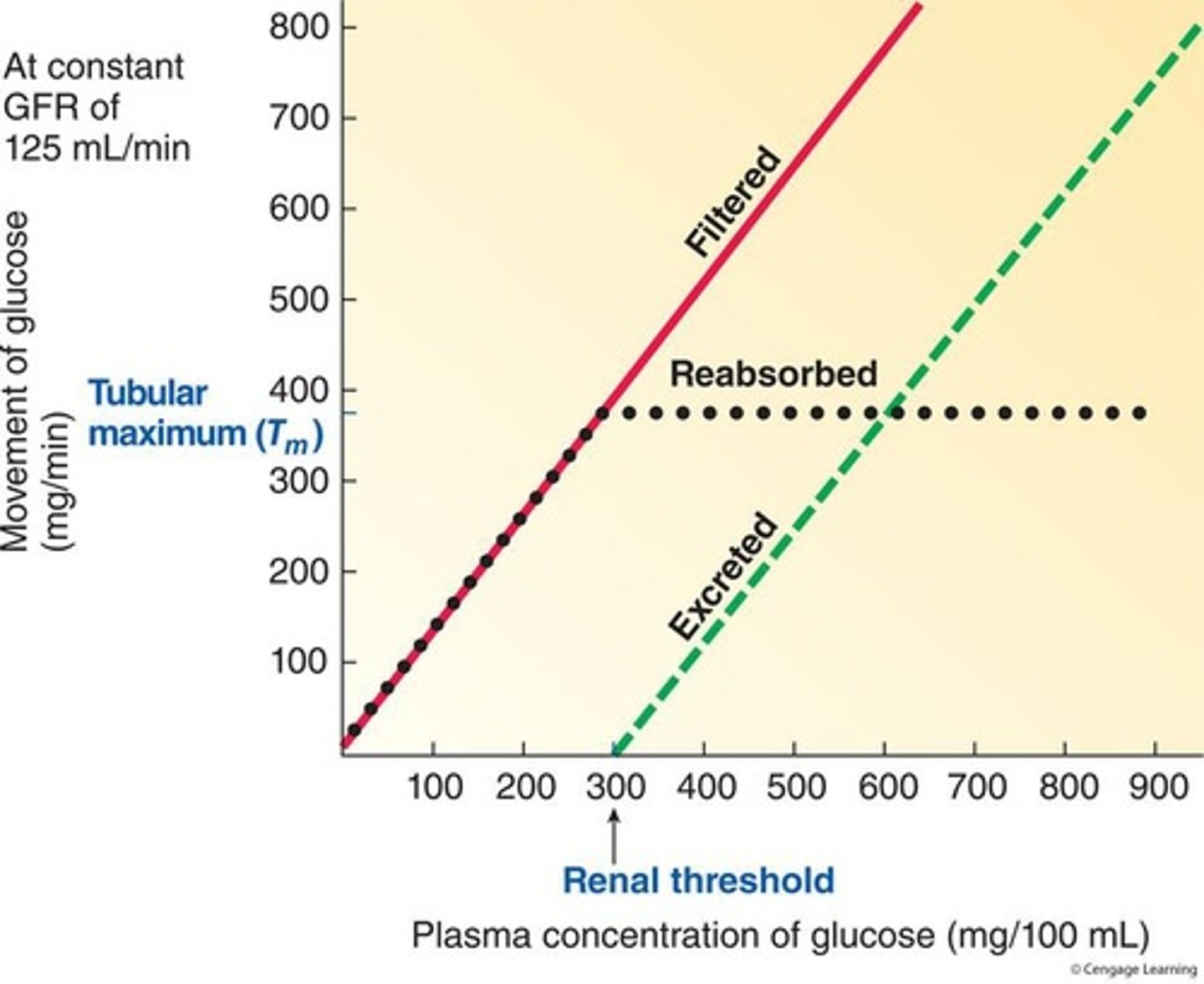
What is the tubular maximum?
The upper limit for how much of a substance can be actively transported in a given period
What happens when the quantity of a substance filtered exceeds the tubular maximum?
The excess is not reabsorbed and escapes into the urine
What is the renal threshold for glucose?
300 mg/100 mL of plasma
Why do kidneys not regulate glucose levels?
They normally reabsorb all glucose in a healthy person
How does phosphate reabsorption differ from glucose reabsorption in the kidneys?
Phosphate reabsorption is regulated by the kidneys, while glucose is not.
What role does parathyroid hormone play in renal handling of phosphate?
It can alter renal thresholds for phosphate and calcium based on the body's needs.
What is the relationship between active Na+ reabsorption and passive reabsorption of chloride?
Chloride is passively reabsorbed down the electrical gradient created by Na+ reabsorption.
How is water reabsorbed in the kidneys?
Water is absorbed osmotically as it follows actively reabsorbed Na+.
What percentage of urea is passively reabsorbed in the kidneys?
50% of urea is passively reabsorbed.
Which ions are primarily secreted during tubular secretion?
H+ and K+ ions, along with organic anions and cations.
How does renal H+ secretion contribute to acid-base balance?
It helps regulate the body's acid-base balance.
What effect does aldosterone have on potassium ion secretion?
Aldosterone controls K+ secretion in the distal and collecting tubules.
What is the relationship between H+ and K+ secretion?
Increased H+ secretion results in decreased K+ secretion and vice versa.
Why is regulating plasma K+ concentration important?
K+ is crucial for the membrane electrical activity of excitable tissues, affecting cardiac rhythm.
What are the two distinct secretory carriers found in the proximal tubule?
One for organic anions and one for organic cations.
What is the primary function of the organic ion secretory system?
To increase excretion of organic ions, eliminate nonfilterable organic ions, and remove foreign organic chemicals.
What does plasma clearance measure?
The volume of plasma cleared of a particular substance per minute, indicating the kidneys' effectiveness in removing substances.
What is the plasma clearance rate for a substance that is filtered but not reabsorbed or secreted?
It always equals the Glomerular Filtration Rate (GFR).
Which substance can be used to approximate GFR?
Creatinine.
What is the plasma clearance rate for a substance that is filtered and reabsorbed?
It is always less than the GFR.
What is the plasma clearance rate for a substance that is filtered and secreted?
It is always greater than the GFR.
What role does the vertical osmotic gradient play in urine excretion?
It allows the kidneys to produce urine of varying concentrations based on body needs.
What is the driving force for water reabsorption in the kidneys?
An osmotic gradient between the tubular lumen and surrounding interstitial fluid.
How do long Henle's loops contribute to the osmotic gradient?
They establish a vertical osmotic gradient by countercurrent multiplication.
What is the permeability of the descending limb of the loop of Henle?
It is highly permeable to water but does not actively absorb Na+.
What is the function of the ascending limb of the loop of Henle?
It actively transports NaCl out of the tubular lumen and is impermeable to water.
What are the benefits of countercurrent multiplication?
It establishes a vertical osmotic gradient and allows the kidneys to concentrate urine.
What percentage of water is automatically reabsorbed from the proximal tubule?
65%.
What percentage of water is reabsorbed from the loop of Henle?
15%.