CO2026 Viruses + HIV
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
86 Terms
What virus(es) is a part of the matonaviridae family?
Rubella virus
What is the reservoir for the Rubella virus and how is it transmitted?
Reservoir: human-only
Transmission: Respiratory droplets, aerosols; Vertical transmission to fetus
All the viruses are human-only reservoirs. Molluscum contagiosum and Adenovirus have human-only reservoirs as well as what other reservoir for each?
Molluscum: human-only + can survive in pools, hot tubs
Adenovirus: Human-only + can survive in water (poorly chlorinated pools)

Which viral families are ssRNA positive, linear, and non-segmented?
Matonaviridae (rubella), Picornaviridae (Coxsackievirus)
What is a risk factor for developing the rubella virus? What symptoms does it cause and what can it cause if transmitted to a fetus?
Risk factors: unvaccinated
Symptoms: rash starts on face, spreads; 3 days with fever, forchheimer spots on soft palate, low grade fever
Congenital Rubella Syndrome- heart defects, cataracts, blindness, deafness

How do you diagnose rubella virus? How can you prevent it?
Diagnose: IgM (current infection), RT-PCR (for congenital)
Prevention: live-attenuated MMR vaccine
Is Matonaviridae enveloped or non-enveloped?
enveloped
What is the paramyxoviridae family composed of? Are they enveloped?
Rubeola (measles) virus, Mumps virus; enveloped
Which family(ies) are ssRNA (negative), linear, and non-segmented?
Paramyoxviridae
Rubeola (Measles) virus has what type of surface proteins? How long is the incubation period?
hemagglutinin- part of influenza vaccine; 10-14 days (HIGHLY INFECTIOUS)
What is a risk factor for developing Rubeola (measles) virus? What are its defining symptoms? (HINT: 3 C's + more)
Risk factor: unvaccinated
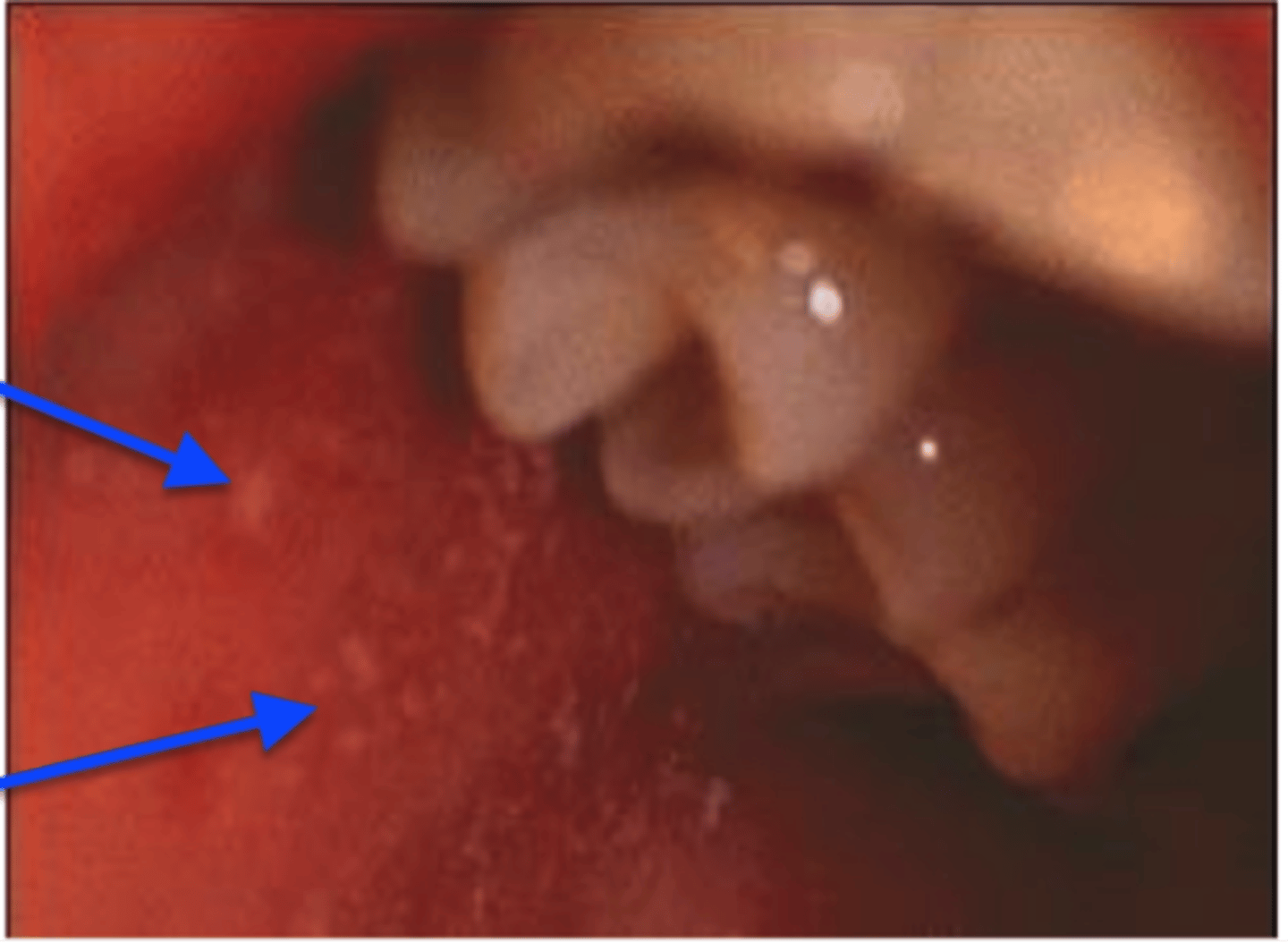
Symptoms: Koplik spots on buccal mucosa (white lesions with surrounding redness), a rash that starts at hairline, spreads down, accompanied by a higher fever (104 degrees)
-3 C's: cough, coryza (runny nose), conjunctivitis)
How can you diagnose the paramyoxviridiae family (rubeola and mumps)? How do you treat? How can you prevent?
Sertology - IgM or RT-PCR
Treatment: supportive care and isolate
Prevention: vaccination, live, attenuated
How is the paramyxoviridae family (rubeola and mumps) spread?
respiratory droplets/aerosols

What cells are affected if you get Mumps virus?
epithelial cells of parotid glands and T-cells
What symptoms can mumps cause?
Parotitis- swelling of salivary gland on 1 or both sides (swollen neck; mumps has lumps)
pain or chewing on acidic foods/drinks (ex. orange juice)
Describe the Picornaviridae family and what viruses are composed within it.
Non-enveloped, ssRNA (positive), linear, non-segmented
Viruses: coxsackievirus
How can the coxsackievirus be transmitted?
respiratory droplets/aerosols, fecal-oral, direct contact with lesions (HFMD)
What are some risk factors for developing coxsackievirus?
infants, kids, crowded areas (ex. schools)
What symptoms does coxsackievirus cause?
hand foot mouth disease, pleurodynia (sharp chest), myocarditis, pericarditis, herpangia (fever, sore thorat, lesions in pharynx)

Which virus/family does the following describe?
-enveloped (large virus)
-dsDNA, linear
-replicates in cytoplasm due to having own DNA polymerase
Poxviridae- Molluscum contagiosum virus
How is Molluscum contagiosum transmitted?
direct person-person contact with lesions, fomites (surfaces)
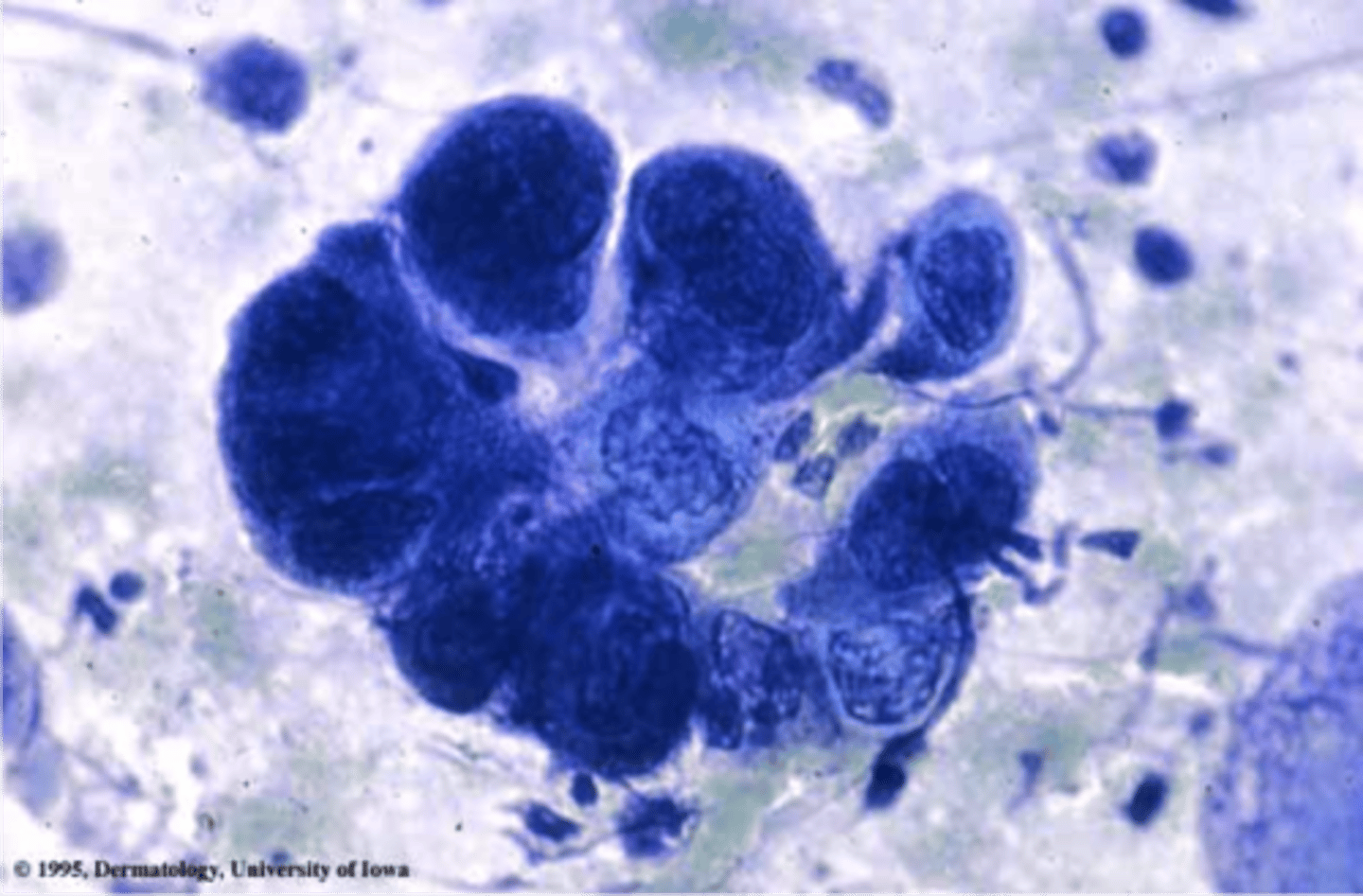
What symptoms does Molluscum contagiosum cause?
skin lesions- skin colored, small, raised, dome-shaped with a central umbilication

How does the staining of Molluscum contagiosum help diagnose it?
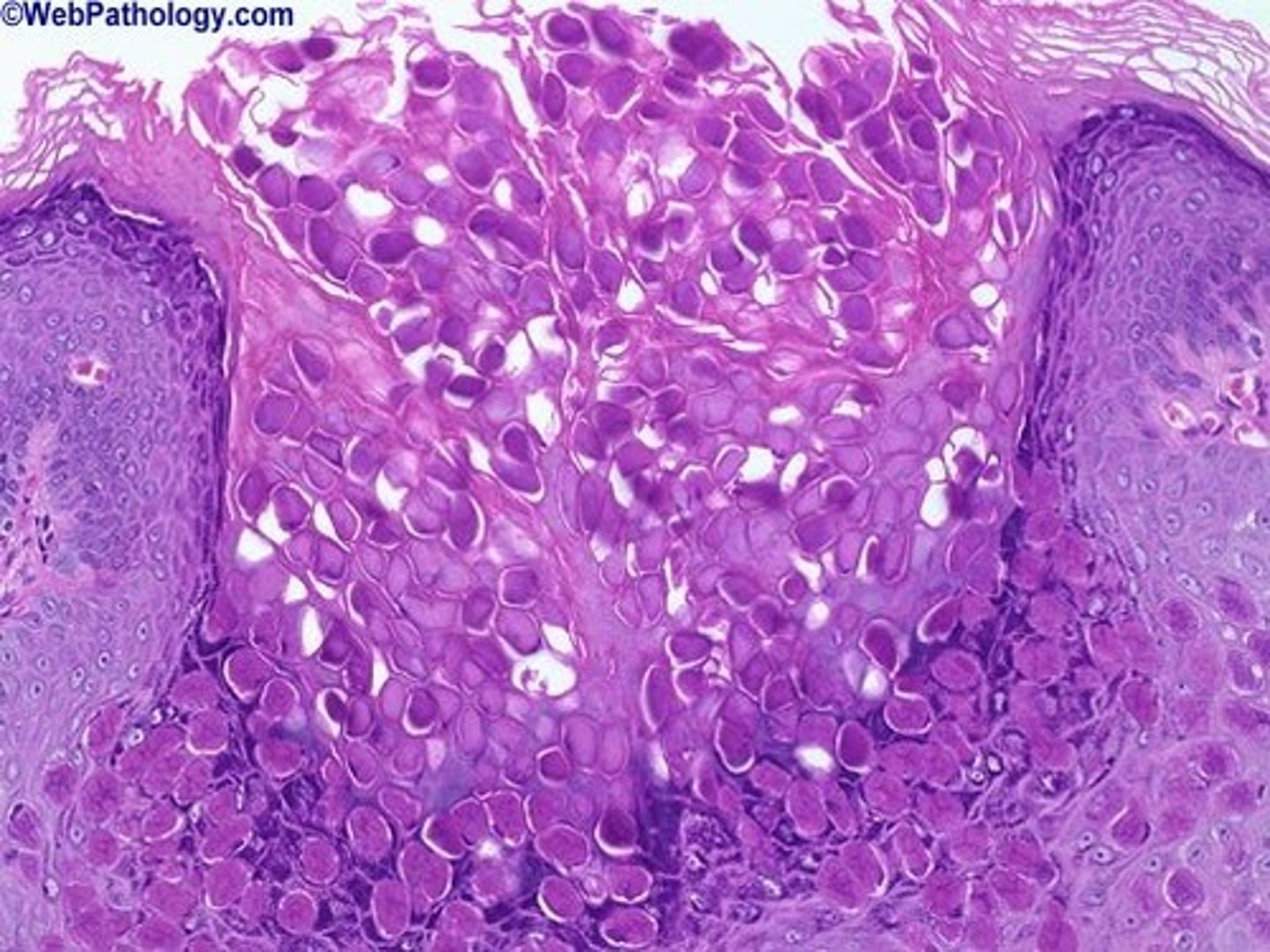
Henderson bodies - large eosinophilic staining lesions in keratinocytes of lesions, bring pink inclusions
Describe the parvoviridae family.
non-enveloped, ssDNA, linear (parvovirus B19)
How is the parvovirus B19 spread? What cell types are infected?
respiratory droplets/aerosols, vertical;
RBC precursors, neutrophils, fetal myocardial cells
What symptoms can Parvovirus B19 cause?
fifth disease "slapped cheek syndrome" which can spread to trunk, arthritis,

Describe the herpesviridae family. What viruses compose it?
enveloped, dsDNA, linear, get envelope from nuclear membrane, establish latency;
Herpes Simplex Virus 1 (HSV1)
Varicella Zoster Virus (VZV)
Cytomegalovirus (CMV)
Roseola virus (Human Herpes Virus 6)
Humans Herpes Virus 8 (HHV8)
How is herpes simplex virus 1 spread?
direct contact with lesions
What does HSV1 infect? Where do they remain latent?
Infects epithelial cells; latency in sensory neurons
What symptoms does someone with HSVI get?
ocular herpes (keratitis), herpes labialis - cold sores, tingling, burning, itching before lesions appear, gingivostomatitis, herpetic whitlow
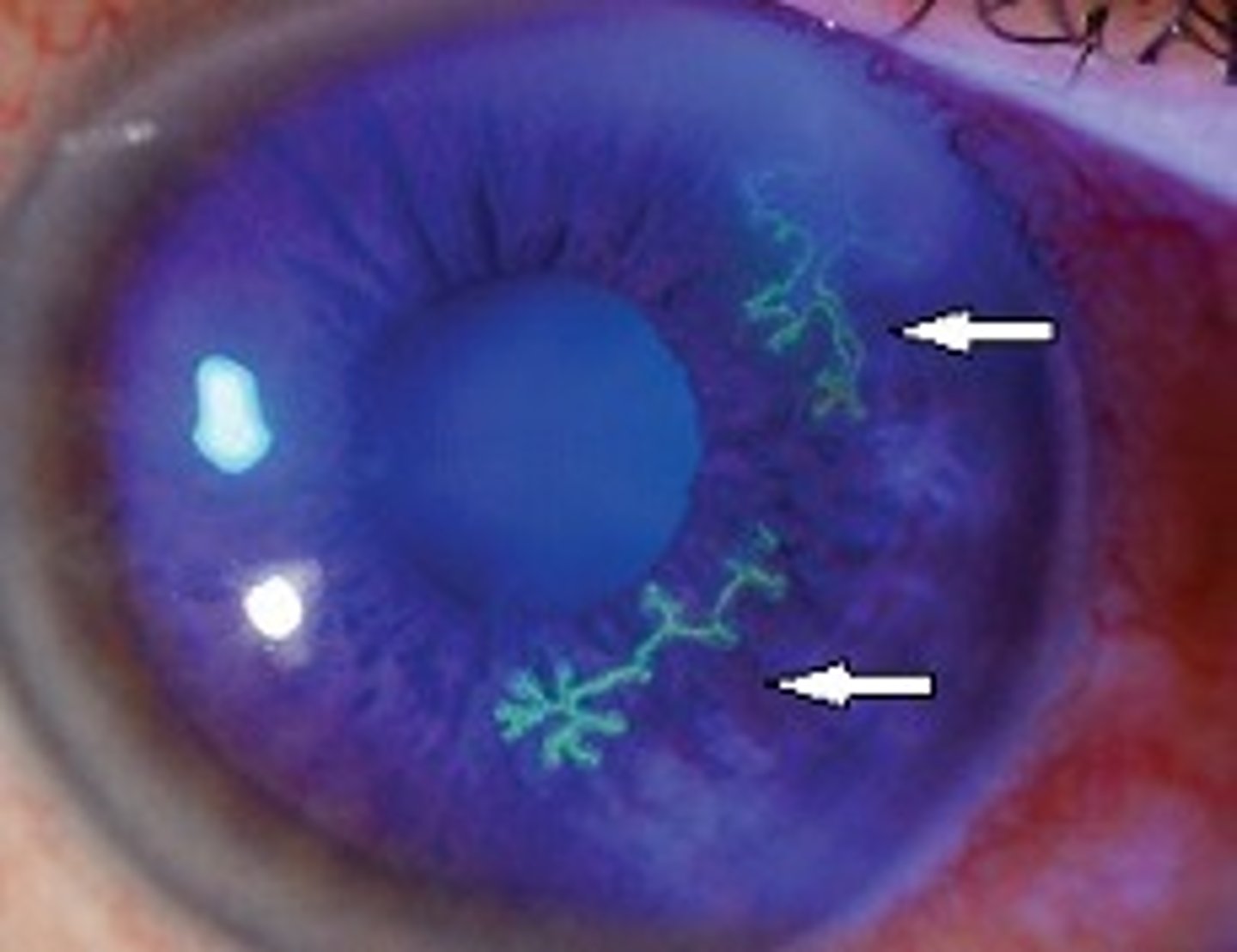
How can you diagnose herpes simplex virus 1?
Tzanck smear stain - multinculeated giant cells
How can you treat HSV1?
Acyclovir
How is Varicella Zoster virus transmitted? What does cells does it affect and where is it latent?
respiratory droplets/aerosols, direct contact with lesions that have not crusted over, vertical; infects epithelial cells, latency in sensory neurons (same as HSVI)
What does Varicella Zoster virus cause? (for both varicella and zoster)
Varicella- fever, rash that progresses from macules to papules to fluid-filled vesicles to fluid-filled vesicles, eventually crust
Zoster- shingles; across dermatomes of the skin

How can you prevent the Varicella Zoster virus? (both components) What are some other treatments?
varicella vaccine- live attenuated
zoster vaccine- recombinant surface glycoprotein
-cyclovir (Acyclovir, Valacyclovir, and Famciclovir)
What diagnostic test is typically used in most viruses?
serology- IgM (when available)
-PCR if not
How is roseola virus- Human Herpes Virus 6 transmitted?
respiratory droplets/aerosols, vertical
What cell type is infected with roseola virus- HHV6? What is the risk factor for developing this?
CD4 T-cells; infants
What are the symptoms of being infected with roseola- HHV6?
Exanthem subitum/ Sixth disease- high fever suddenly appears which can cause seizures, rash appears after fever goes away, starts on the neck and trunk

How long is the incubation period for Molluscum contagiosum?
Molluscum- 2 weeks to 6 months (2-3 month avg.)
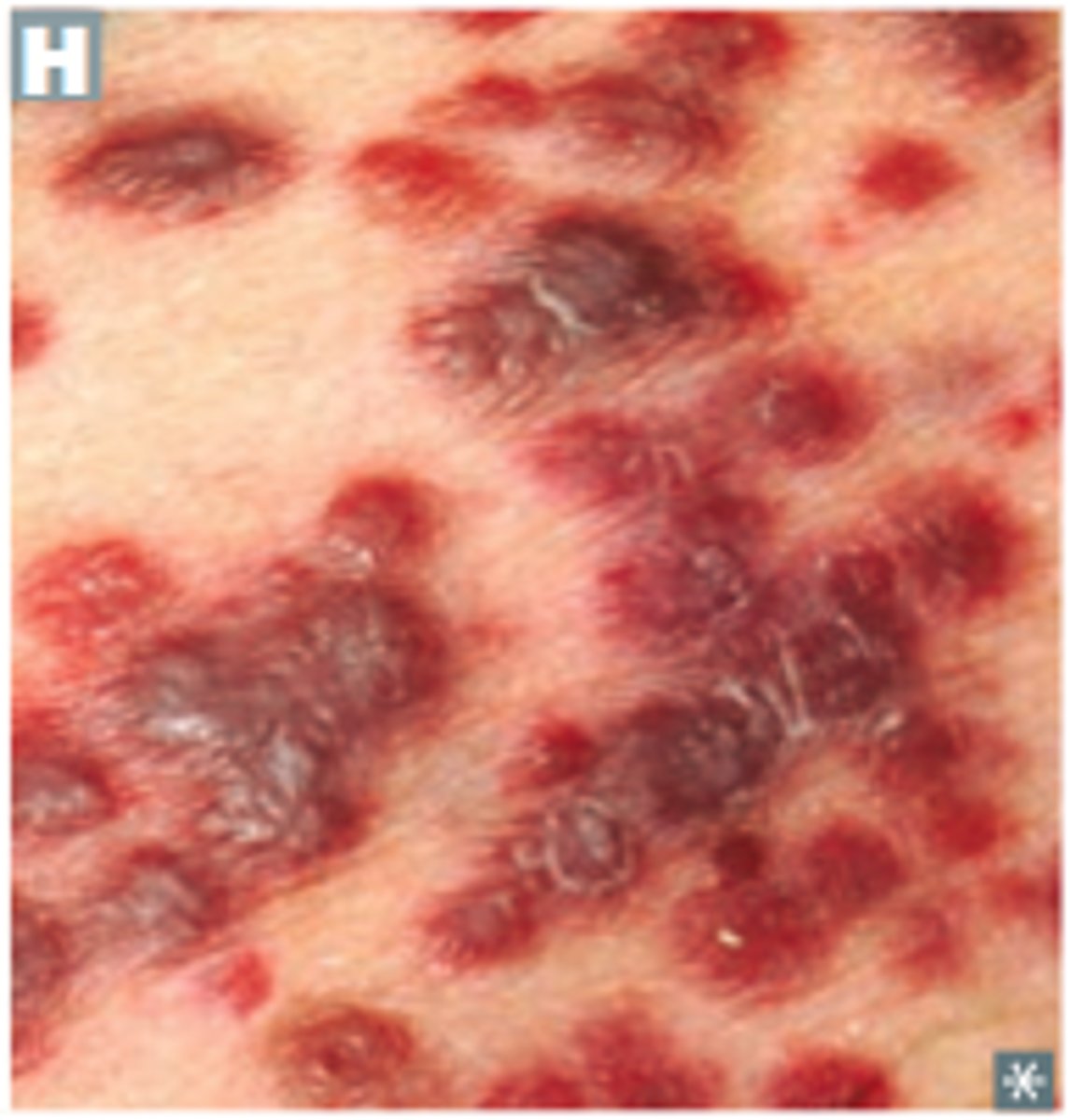
What symptoms does HHV8 cause?
Kaposi's sacroma- cancer that develops in mucous membranes (gums-making it hard to eat), skin, internal organs- dark red/purple lesions as plaques or patches (only in HIV positive patients),
What are the microbe characteristics of HIV? (family and what type of RNA/DNA, etc.)
Retroviridae- enveloped ssRNA positive sense, linear, 2 copies
What cells does HIV infect? Where does it bind?
infects CD4 T-cells via gp120 and CD4 receptor binding
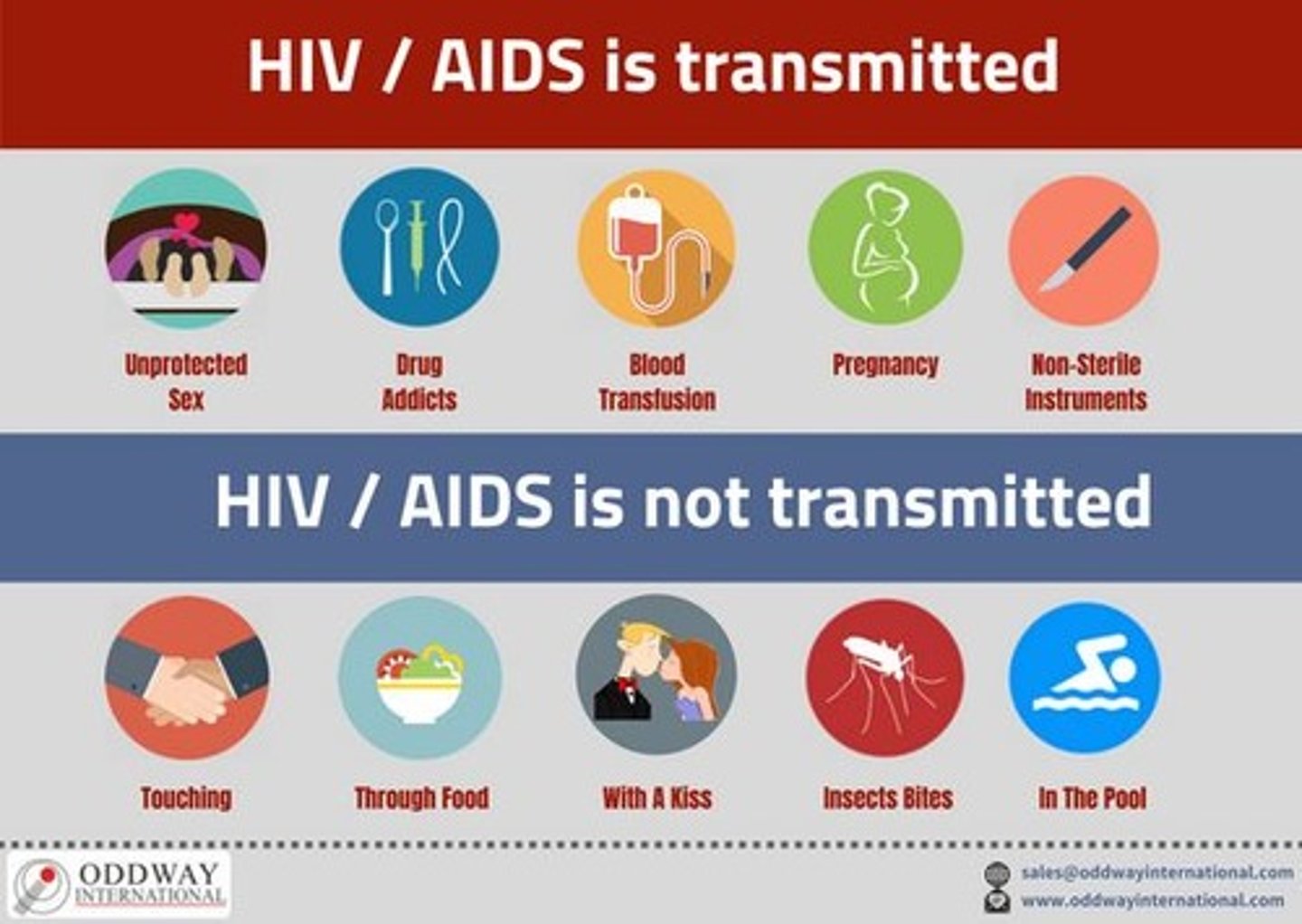
How is HIV transmitted?
body fluids: blood, semen, vaginal secretions, breast milk
direct contact: sexual contact, blood transfusion, during natural birth vertically, sharing needles, needlestick injury
What countries/areas of the world are most affected by HIV? What demographics are most at risk for developing it?
Sub-Saharan Africa (South Africa = highest), Russia; Black/African American, Hispanic/Latino
The HIV virus binds via ____ and fuses with the host cell (___). What are the coreceptors?
gp120; CD4
coreceptors: CXCR4 or CCR5
What is the fusion of HIV aided by?
viral surface protein gp41
The HIV virus, once it fuses, gets uncoated and there is a release of what 2 main viral proteins? What is there function?
Reverse transcriptase- convert viral RNA to DNA
Integrase- new viral DNA gets integrated into host DNA
Where does HIV replicate?
RNA virus replicates in nucleus
The newly viral integrated HIV viral DNA is transcribed by the host cell's machinery to make new HIV RNA, some of which is translated into ___________
HIV proteins
HIV RNA and proteins move to the cell surface once translated and transcribed respectively, where they are assembled into new virus. The immature HIV viruses exit the cell and release _______. What does this do?
Protease- cleaves the proteins to yield mature HIV viruses that can infect the next cell
What do CCR5 antagonists do?
block CCR5 coreceptor needed in addition to the CD4 receptor for binding to the CD4 surface
What do Attachment inhibitors do?
bind to gp120 protein on the outer surface of HIV, preventing HIV from entering CD4 cells
What do post-attachment inhibitors do?
block CD4 receptors on the surface cell surfaces that HIV needs to enter the cells
What do fusion inhibitors do?
block fusion of HIV envelope and CD4 cell membrane preventing entry of HIV into CD4 cell
What do Nucleoside RT inhibitors (NRTIs) do?
have nucleoside structurally similar to T-cell DNA nucleoside, this mimicry enabling NRTA to integrate T-cell DNA to stop production of viral DNA proteins
What do Non-Nucleoside RT Inhibitors (NNRTIs) do?
bind directly to the HIV's reverse transcriptase enzyme that inhibits its activity
What do integrase strand transfer inhibitors do?
inhibit integrase necessary for HIV to insert its viral DNA into the CD4 cell DNA for replication
What do protease inhibitors do?
block protease needed to produce infectious HIV particles (will not release viruses from T cells- little bit of envelope stuck on membrane)
During early period after primary infection of HIV, widespread dissemination of virus and a sharp decrease in ______ in blood. What occurs after this?
CD4 T cells; an immune response to HIV
When the immune system responses to HIV, there is a decrease in ______ followed by a prolonged period of ______.
detectable viremia; clinical latency
CD4 T cell count continues to decrease until it reaches a critical level below which there is a substantial risk of _________.
opportunistic infections
What is the HIV capsid protein called and where is it released? What does viremia mean?
p24 into cytoplasm; viremia= presence of virus in blood (low during latency)
What are CTL- cytotoxic T-cells (CD8) responsible for? What does the HIV envelope (ENV) do?
CD8- infection control
HIV envelope- neutralize from new cell infection (antibody to gp120)
What does your CD4 level have to be in order to have an AIDS diagnosis?
below 200 cells/uL
What are the symptoms of primary infection of HIV? What about acute HIV syndrome?
Primary infection- no signs/symptoms for first 2-4 weeks, "mono-lile"
Acute HIV syndrome: mononucleosis-like symptoms- fever, night sweats, malaise, sore throat, rash, lymphoadenopathy, GI upset, myalgias
The acute HIV syndrome coincides with ____ in viral RNA in the blood as viruses are being produced and a drop in the number of ______.
spike; CD4 #
What occurs in clinical latency of HIV? What does the viral load remaining in clinical latency indicate?
no signs, virus produced at lower levels, can be for years; viral load remaining after the patient exits the acute stage indicates the probability they will progress to AIDS and how fast (PCR done in blood to see baseline RNA)
AIDS-Related complex occurs as CD4 numbers drop below _______. What symptoms occur?
500 cells/uL; Generalized lymphadenopathy, fever, weight loss
T or F: There is variable progression from initial infection through latency to AIDS.
true- means some stay in latency longer than others through medication
On HIV medications, virus is _______ in lab studies.
undetectable- cannot transmit HIV to sexual partner
When someone has AIDS, ________ tend to occur. Some have prophylaxis (an attempt to prevent disease)
opportunistic infections
What do you screen for regardless of CD4 count in HIV-positive individuals?
Mycobacterium tuberculosis- acid-fast bacillus for latent infection (TB will reactivate if present in HIV individuals)
If an HIV position patient has less than 200 CD4 cells/uL, what infections may occur? State the prophylaxis if there is one.
Pneumocystis jivorecii (PCP)- monomorphic fungus- pneumonia (use Trimethoprim-sulfamethoxazole - TMP-SMX for prophylaxis)
Coccidiodes immitis- use flucanzole
HHV8- causes Kaposi's sarcoma (no prevention)
Cryptosporidium parvum- protozoan, watery diarrhea (no prevention)
Candida albicans-oral thrush
Herpes simplex virus- reactivation that can cause encephalitis, keratitis
If an HIV position patient has less than 100 CD4 cells/uL, what infections may occur? State the prophylaxis if there is one.
Toxoplasma gondii- protozoan, reactivation in CNS (use Trimethoprim-sulfamethoxazole- TMP-SMX for prophylaxis)
Cryptoccocus neoformans- monomorphic yeast, encapsulated, meningitis
Histoplasma capsulatum- dimorphic yeast, disseminated infection, endemic to Ohio/Mississippi River Valleys (use Itraconazole)
Candida albicans- esophagitis
If an HIV position patient has less than 50 CD4 cells/uL, what infections may occur? List the prophylaxis if any.
Mycobacterium avium complex (MAC)- Acid-fast bacilli- disseminated infections, multiple body sites (Prophylaxis: Rifabutin, Azithromycin)
Cytomegalovirus- reactivation causing esophagitis, retinits
List the Neoplasma/non-infections that are AIDS-defining
Encephalopathy- AIDS-related dementia (lack of antiretroviral therapy increases risk of developing)
*infected monocytes can bring HIV into CNS- pro-inflammation response, direct damage*
Non-Hodgkin's lymphoma- brain
Kaposi's sarcoma- HHV8
Cervical cancer- HPV
What should you give to a mother who has HIV prior to birth? What else should the mother do in order to prevent her child from developing Pediatric HIV?
Zidovudine; no breast feeding
Pediatric HIV can be acquired at birth. Infants are given ___________ for the first 2-6 weeks then given a PCR to determine if HIV-negative or positive b/c they could still have their mom's antibodies in the beginning.
HIV antivirals
What are some of the characteristics of HIV-2?
-less common
-less infectious
-less fatal and progresses more slowly
In order to diagnose HIV, what is the first test you conduct? What test do you conduct to differentiate it from HIV-1 to HIV-2 if positive after first test?
first test = look for HIV antibodies and p24 antigen (protein of capsid)
Nucleic Acid test (NAT)
What does ELISA look for?
antigen --> p24 which is detected earlier than antibodies
What does an immunoassay do if positive for p24?
differentiate between HIV-1 or 2
If someone is positive for p24 but negative with the immunoassay, what testing do you do?
Nucleic acid testing
What is the main goal of HAART?
manage and reduce HIV drug resistance --> mutates rapidly, no "drug holidays"
drug holidays = person stops taking, HIV becomes resistant to many drugs
_________ reduces risk of HIV from sexual activity by 99%. Maximal protection achieved and is receptive within 7 or at 7 days of anal intercourse, 21 days after vaginal.
Pre-Exposure Prophylaxis (PrEP)