Mod 1 - Wk 2 Neurovascular Protocols Review
1/69
Earn XP
Description and Tags
These flashcards encompass the key concepts and procedures related to Neuro CT Vascular Imaging, crucial for understanding and performing these medical imaging techniques.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
70 Terms
What is the purpose of Neuro CT vascular imaging?
To evaluate the arterial and venous blood supply of the brain, especially in acute neurological emergencies.
What major conditions are assessed using CT neuro vascular imaging?
Stroke, arteriovenous malformations, stenosis, dissection, and vessel occlusion.
What are common indications for CT neuro vascular scans?
Suspected stroke, AVM, stenosis, dissection, occlusion, and follow-up imaging after vascular events.
Why is CTA commonly included in major trauma CT exams?
To assess for suspected vascular damage.
What are the four main CT neuro vascular protocols?
CTA Head (Circle of Willis), CTA Stroke (Arch to Vertex), CT Perfusion, and CT Venogram.
When is a Neuro CTA requested?
For stroke symptoms, high stroke risk, aneurysm diagnosis, vascular malformations, dissections, and suspected traumatic vascular injury.
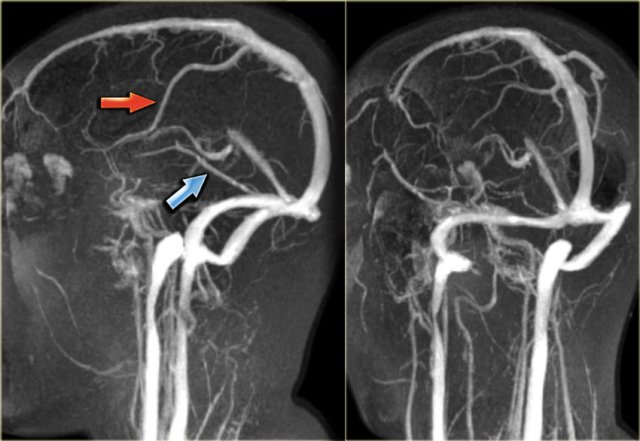
Why is CTA especially useful in acute ischemic stroke?
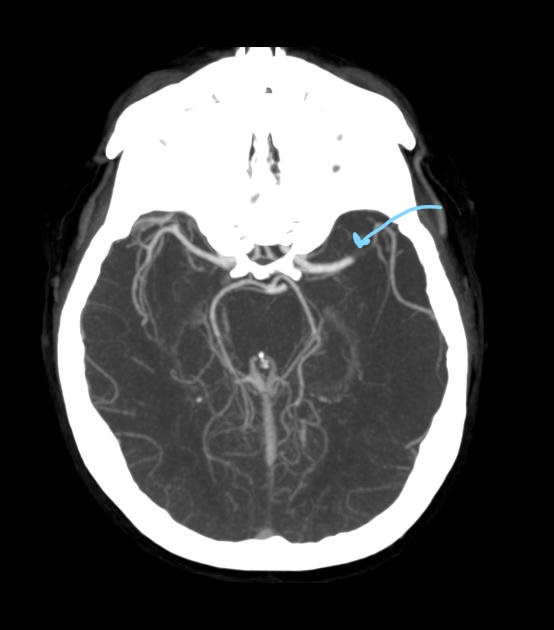
It identifies the site of vessel occlusion by showing the abrupt cessation of contrast in the affected artery.
What is a Maximum Intensity Projection (MIP)?
A reconstruction technique that displays only high HU voxels to enhance visualization of contrast-filled vessels.
Approximately how much of the original CTA data is represented in a MIP image?
About 10%.
Why are MIPs essential for CTA interpretation?
They remove low-attenuation tissue and highlight vascular anatomy.
What IV size is required for Neuro CTA?
20G or larger peripheral IV.
Where should the IV ideally be placed for Neuro CTA?
Right antecubital fossa.
What is the typical contrast volume and injection rate for CTA Neuro?
Approximately 90–100 mL at ~3.5 mL/s.
Where is bolus monitoring performed for CTA Neuro?
At the level of the aortic arch.
Why is an 8–10 second scan delay used during bolus monitoring?
To allow IV monitoring and minimize unnecessary scans.
What instruction should be given to the patient regarding swallowing during CTA?
Swallow once, then do not swallow until the scan is complete.
How can IV patency be confirmed during contrast injection?
By feeling a 'hum' under the skin at the IV site.
Why is image reconstruction a critical technologist responsibility?
Optimal MPRs are required for accurate diagnosis.
What reconstruction thickness is used for axial thin images?
0.6 mm.
What kernel is used for detailed vascular anatomy in thin axial images?
Mediastinum (B45).
What plane best demonstrates the Circle of Willis?
Axial and coronal head MIPs.
Why are sagittal oblique neck MIPs important?
They demonstrate the carotid bifurcation and internal/external carotid arteries.
What is a stroke?
A sudden, non-traumatic vascular insult to the brain.
What does the phrase 'Time is tissue' mean?
Brain cells begin dying shortly after blood flow is interrupted.
What causes an ischemic stroke?
Obstruction of a cerebral artery by an embolus or thrombus.
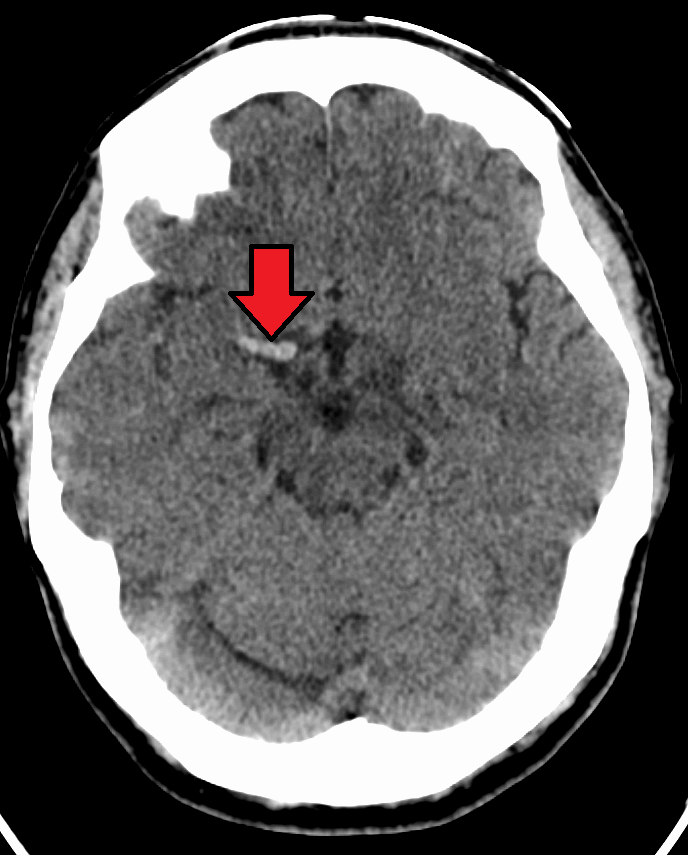
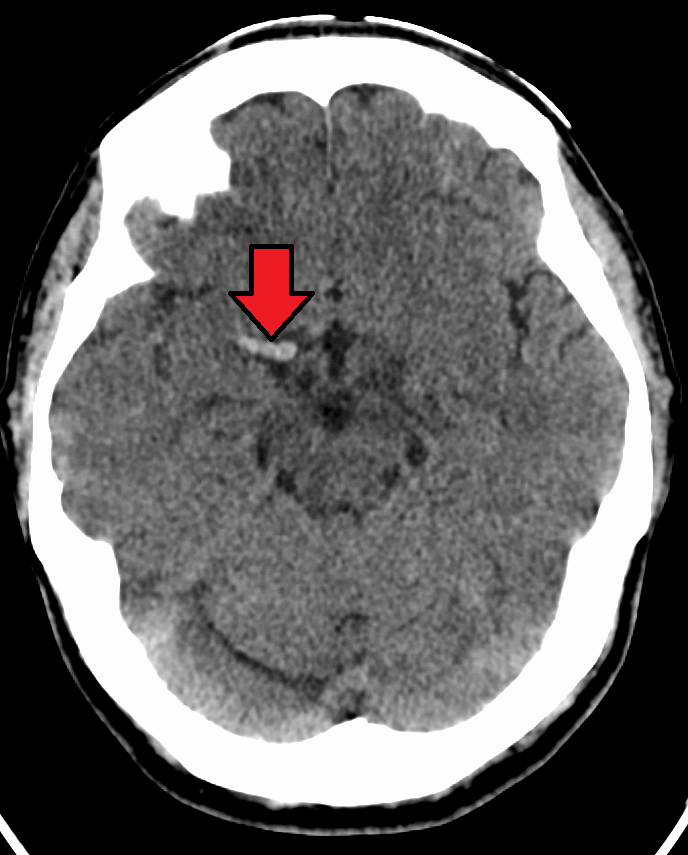
How does ischemic stroke appear on CT?
Hypodense (darker) compared to normal brain tissue.
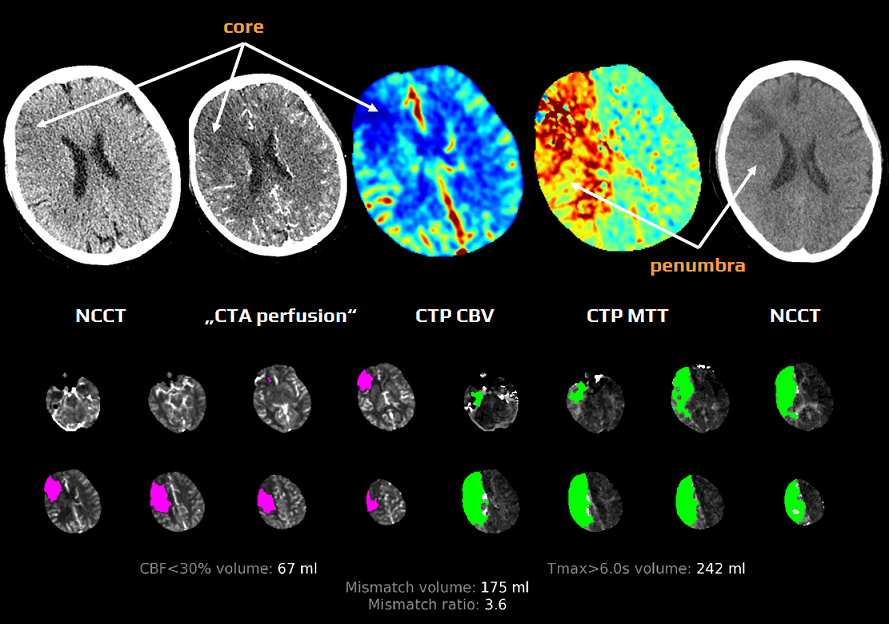
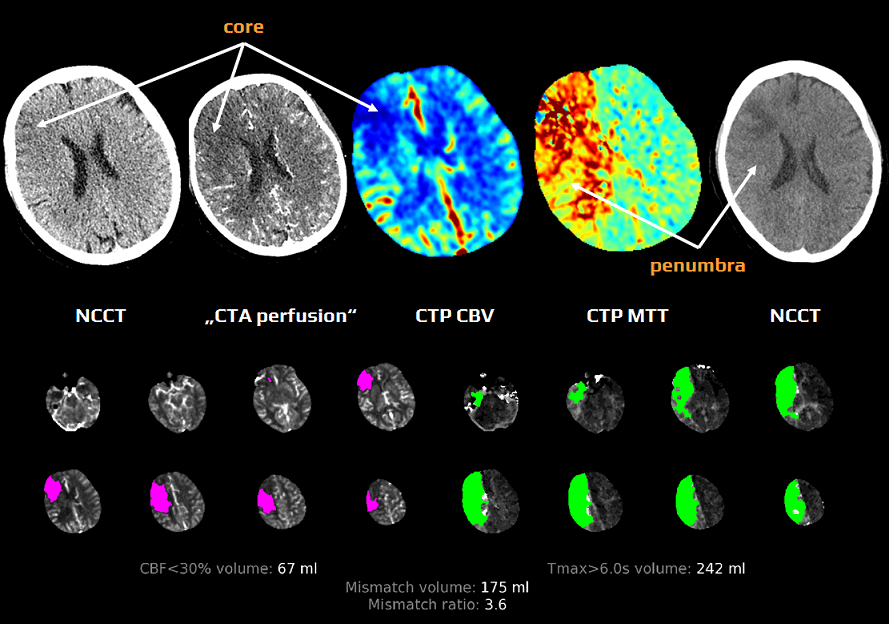
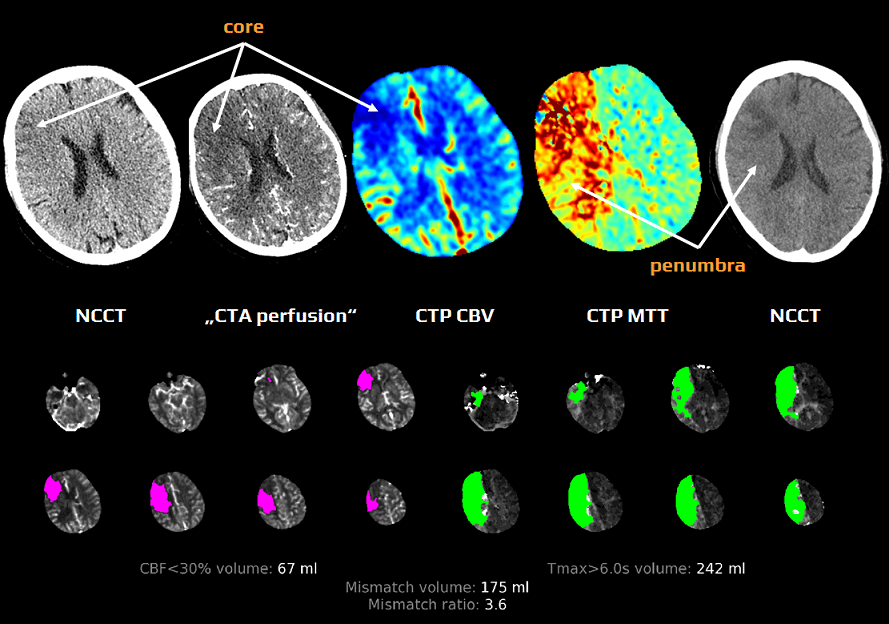
What is the stroke core?
The central region of irreversibly damaged brain tissue.
What is the penumbra?
Surrounding brain tissue that is damaged but salvageable.
Where can emboli causing ischemic stroke originate from?
Atherosclerotic plaque, deep veins of the leg, or the heart.
What is tPA?
A thrombolytic agent used to dissolve clots.
How can tPA be administered?
Intravenously or intra-arterially.
Why is tPA use carefully considered?
It has significant risks and multiple contraindications.
What causes a hemorrhagic stroke?
Rupture of a weakened blood vessel.
How does acute hemorrhage appear on CT?
Hyperdense (bright/white).
Why is CTA not performed if hemorrhage is detected?
Contrast enhancement may be mistaken for active bleeding.
What is a TIA?
A transient ischemic attack or 'mini-stroke' caused by a temporary clot.
Is a TIA usually visible on CT?
No.
What is a 'Hot Stroke'?
A suspected active stroke within the treatment window.
Why are stroke patients prioritized in CT?
Treatment decisions depend on rapid imaging results.
What is the first scan performed in a Hot Stroke protocol?
Non-contrast CT Head.
Why must non-contrast CT be performed first?
To rule out intracranial hemorrhage.
What must the technologist do if hemorrhage is seen?
Alert the radiologist and cancel the CTA.
What does the CTA Arch to Vertex assess?
Arterial circulation from the aortic arch to the brain.
At what step is contrast administered in the Hot Stroke protocol?
During the CTA.
What is the purpose of CT Perfusion in stroke imaging?
To differentiate stroke core from penumbra.
Is additional contrast injected for perfusion following CTA?
No.
What is blood flow mapping?
Post-processing analysis used to identify salvageable brain tissue.
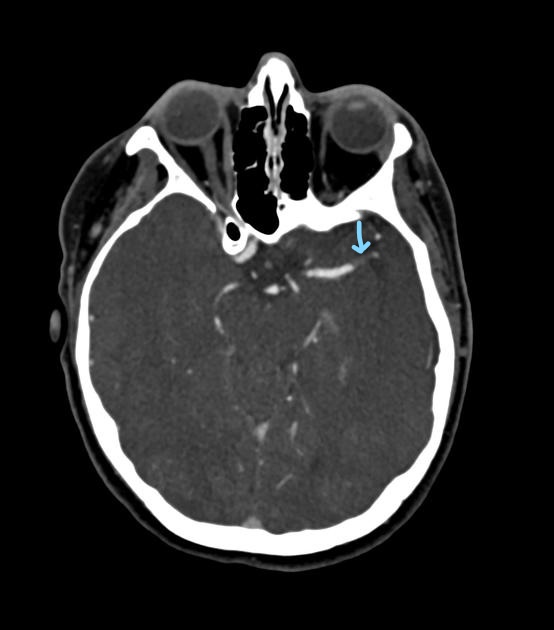
What does a hyperdense MCA sign indicate?
An occlusive thrombus in the middle cerebral artery.
Should CTA proceed if a hyperdense artery is seen but no bleed is present?
Yes.
What is the main goal of Neuro CT Perfusion?
To identify infarcted tissue and quantify salvageable penumbra.
Why may non-contrast CT appear normal in acute ischemic stroke?
Density changes may not yet be visually detectable.
What type of scan is CT Perfusion considered?
A functional, dynamic scan.
How long does a typical perfusion scan last?
Approximately 40–60 seconds.
Why are sampling intervals greater than 2 seconds undesirable?
They reduce the accuracy of perfusion maps.
What IV size is required for Neuro Perfusion?
18G or larger.
What is the contrast protocol for perfusion?
40–60 mL at 5–6 mL/s with a saline chaser.
Why must the patient be immobilized during perfusion imaging?
Motion artifacts can invalidate perfusion analysis.
What does Mean Transit Time (MTT) or Time to Peak (TTP) measure?
Time for contrast to reach peak enhancement in brain tissue.
What is Cerebral Blood Flow (CBF or rCBF)?
The rate of blood flow through brain tissue.
What is Cerebral Blood Volume (CBV)?
The volume of blood within a given amount of brain tissue.
What is the purpose of a CT Venogram?
To evaluate cerebral veins and venous sinuses.
What condition is CTV most commonly used to assess?
Dural sinus thrombosis.
What patient populations are at increased risk for venous thrombosis?
Patients with coagulopathies, lupus, and postpartum patients.
Why may CTV be performed before posterior craniotomy?
To map dural sinuses adjacent to the skull.
During which phase of circulation is CTV acquired? (Evaluates Venous drainage of the brain)
Venous phase.
Approximately when does venous enhancement occur after injection?
Around 35 seconds.
What scan delay is typically used for CTV?
35–40 seconds.
What is the scan range for CTV?
Base of the skull through the vertex.
Why must the entire cranium be included in the SFOV?
Dural sinuses are closely associated with the inner skull table.
How do CTV reconstructions compare to CTA reconstructions?
They use the same MPRs, vascular kernels, and MIP filters.