Microbiology 2
1/84
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
What is Mycology?
Study of fungi
(They are aerobic or facultatively anaerobic chemoheterotrophs)
What makes Fungi different to Bacteria
Fungi has sterols present in membrane
the sterols are used for sexual and asexual reproduction
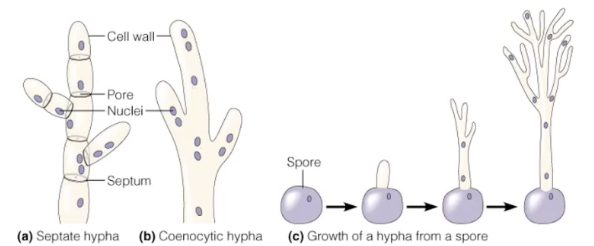
Thallus? Hyphae?
Thallus = the whole body of the fungus
The thallus is made of long thread-like structures called hyphae
Functions of hyphae
Vegetative hyphae → grow into the surface/food, absorb nutrients (the “feeding” part)
Reproductive (aerial) hyphae → grow upwards, produce spores (the “spreading/reproduction” part)
Asexual Reproduction
Methods:
Fragmentation of hyphae → pieces of hyphae grow into new fungi
Spores → tiny “seeds” that grow into new fungi
Types of asexual spores
Types of asexual spores:
Conidiospore, Arthrospore, Blastospore → not in a sac (just free spores)
Sporangiospore → inside a sac (sporangium) at the end of a stalk called a sporangiophore
Sexual Reproduction
A haploid nucleus (+ strain) from one fungus enters the cytoplasm of a haploid nucleus (- strain) from another fungus
Only the cytoplasm fuse at this stage, nuclei remain separate for now
The + and - nuclei fuse to form a diploid nucleus (zygote nucleus)
The diploid nucleus undergoes meiosis to produce haploid sexual spores
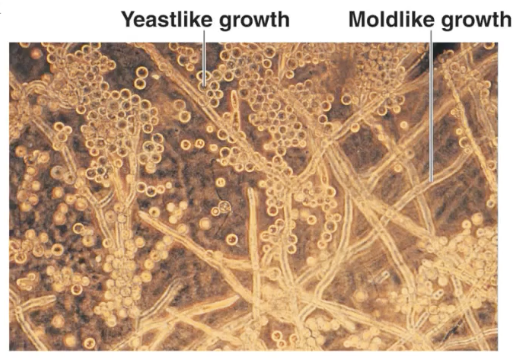
Dimorphism
Some fungi can grow as unicellular (yeast) or as Mold
For most, the temp can tell us which one
37C for yeast and 25C for Mold
Lichens
A partnership (symbiosis) between:
A fungus (provides structure, protection, holds water)
Algae (provides food by photosynthesis)
Good and Bad Algae
Good algae
Convert CO2 to O2
Are food
Can be symbiotic
Bad algae
Algal bloom= use O2 off other algae
Toxins and pests
Protozoa
Trophozoite → the active feeding and growing form
Cyst → a dormant, resistant form that helps survive harsh conditions
Excavate
…are flagellated unicellular organisms
(Unusual as they have no mitochondria and reproduce by fission)
Phylum Amoebozoa
Protozoa (unicellular, eukaryotic organisms)
Move by pseudopodia (“false feet”) → temporary extensions of the cytoplasm
Feed by phagocytosis → engulfing food particles with pseudopodia
Much larger than bacteria
Phylum Apicomplexans
Obligate intracellular parasites → must live inside host cells to surviv
Have special organelles at the apex that help them penetrate host cells
No movement structures
Two-host life cycle:
Mosquito = definitive host (sexual reproduction happens here)
Human = intermediate host (asexual reproduction happens here)
Life Cycle of Plasmodium vivax
1. Mosquito bite (infection begins)
Female Anopheles mosquito bites human → injects sporozoites
2. Liver stage
Sporozoites travel in blood → enter liver cells
Multiply asexually → release merozoites into blood
3. Blood stage (causes malaria symptoms)
Merozoites enter red blood cells (RBCs)
Inside RBCs → grow into trophozoites (“ring stage”)
Multiply → RBC bursts → releases more merozoites → infect more RBCs
4. Sexual stage in humans
Some parasites in RBCs develop into male and female gametocytes (sexual forms)
These stay in the blood, waiting for the next mosquito bite
5. Back to mosquito (sexual reproduction)
Mosquito bites infected human → takes in gametocytes
In mosquito gut → gametocytes fuse → form zygote → develops into sporozoites
Sporozoites migrate to mosquito’s salivary glands
6. Cycle restarts
Mosquito bites another human → injects sporozoites again
Toxoplasma gondii
Transmission: Mainly from cats (in cat feces), or from undercooked meat
Disease: Toxoplasmosis
Usually mild in healthy people
Dangerous in pregnancy → can cross placenta and cause fetal infections (brain/eye damage, miscarriage)
Cryptosporidium
Transmission: Fecal–oral route (especially contaminated water)
Disease: Cryptosporidiosis
Watery diarrhea, stomach cramps
Very severe in immunocompromised patients (e.g., AIDS)
Helminths
WORMS
Reduced digestive system → many absorb nutrients directly from host
Reduced nervous system → don’t need to sense much, host provides environment
Reduced locomotion → little need to move; host carries them
Complex reproduction → produce lots of eggs to ensure transmission
Groups of Helminths
Flatworms (Platyhelminthes)
Trematodes (flukes) → flat, leaf-shaped; suckers for attachment
Cestodes (tapeworms) → long, segmented; no digestive system, absorb nutrients
Roundworms (Nematodes)
Cylindrical, complete digestive system (mouth → anus)
Many are parasites of humans and animal
Trematodes (Flukes)
Example: Lung Fluke (Paragonimus spp.)
Transmission: Eating undercooked freshwater crabs or crayfish with cysts.
Life cycle:
Eggs → water → hatch → infect snails (intermediate host).
From snail → infect crabs/crayfish.
Humans eat undercooked crab → larvae migrate from intestine → lungs.
Symptoms: Chronic cough, bloody sputum, chest pain (mimics TB).
Hosts: Snail = intermediate; Human = definitive.
Cestodes (Tapeworms)
Example: Beef Tapeworm (Taenia saginata)
Transmission: Eating undercooked beef with cysts (larvae).
Life cycle:
Eggs in human feces contaminate grass → cows eat eggs.
Larvae form cysts in cow muscle.
Humans eat undercooked beef → adult worm develops in intestine.
Symptoms: Often mild; abdominal discomfort, weight loss, visible proglottids in stool.
Hosts: Cow = intermediate; Human = definitive.
Nematodes (Roundworms)
a) Pinworm (Enterobius vermicularis)
a) Pinworm (Enterobius vermicularis)
Transmission: Fecal-oral (ingestion of eggs, especially in children).
Life cycle: Eggs hatch in intestine → adults live in colon → females lay eggs around anus at night.
Symptoms: Intense perianal itching, especially at night.
Host: Human only (direct cycle).
Nematodes (Roundworms)
b) Ascaris lumbricoides (giant intestinal roundworm)
b) Ascaris lumbricoides (giant intestinal roundworm)
Transmission: Ingesting eggs in contaminated food/water.
Life cycle: Eggs hatch in intestine → larvae migrate through blood → lungs → coughed up and swallowed → mature in intestine.
Symptoms: Abdominal pain, intestinal blockage, coughing (lung migration).
Host: Human only.
Nematodes (Roundworms)
c) Hookworm (Ancylostoma, Necator)
c) Hookworm (Ancylostoma, Necator)
Transmission: Larvae penetrate skin (often bare feet, soil contaminated with feces).
Life cycle: Larvae enter bloodstream → lungs → coughed up and swallowed → intestine.
Symptoms: Anemia (they suck blood), fatigue, malnutrition.
Host: Human only.
Arthropods as Vectors
Arthropods = animals with:
Segmented bodies
Hard exoskeleton (outside skeleton)
Jointed legs
Vector = an arthropod that carries and transmits disease-causing microorganisms (pathogens) from one host to another.
Microbial classification and biological basis
Taxonomy: Classification based on observable traits (phenotype), e.g., shape, staining, biochemical tests.
Phylogeny: Classification based on evolutionary history (genotype), e.g., DNA, RNA, protein sequences.
Both help understand what an organism is like and how it evolved.
Classification of Organisms
Organisms are grouped into taxa (Domain → Kingdom → Phylum → … → Genus → Species).
Binomial nomenclature: Genus (capitalized) + species (lowercase), italicized, e.g., Escherichia coli.
Classification reflects both similar traits and evolutionary relationships.
The tools used for classification of various organisms.
Morphology: Shape, flagella, endospores
Staining: Gram-positive/negative, acid-fast
Biochemical tests: Sugar fermentation, enzyme activity, selective media
Serology: Antibodies detection (ELISA, slide agglutination)
Phage typing: Bacteriophage sensitivity
Molecular methods: rRNA sequencing, PCR, DNA fingerprinting
Prokaryotic groupings include Bacteria and Archaea, each with subgroups and example species.
Archaea Classification
Methanogens: produce methane from CO2
Extreme halophiles: require high salt
Thermoacidophiles: live in high temperature and acidic environments, use sulfur
Types of bacteria (special bacteria)
Giant bacteria: unusually large bacterial cells
Intracellular bacteria: live inside host cells (e.g., Rickettsia, Chlamydia)
Gliding bacteria: move without flagella
Other examples: spore-forming bacteria (Bacillus, Clostridium), wall-less bacteria (Mycoplasma)
Non-proteobacteria
Cyanobacteria: oxygenic photosynthesis, some fix nitrogen
Phototrophic bacteria: purple and green bacteria, anoxygenic photosynthesis
Gram-positive bacteria: cocci, endospore-forming rods, non-spore-forming rods, irregular rods, Mycobacteria
Spirochaetes: Treponema, Borrelia, Leptospira
Chlamydias: obligate intracellular parasites
Mycoplasmas: no cell wall
Proteobacteria
Gram-negative, physiologically diverse
Subdivisions:
α: Rickettsia, Bartonella, Brucella, Rhizobium
β: Burkholderia, Bordetella, Neisseria
γ: Pseudomonas, Legionella, Vibrio, Enterobacteriales (E. coli, Salmonella)
δ: Bdellovibrio, Desulfovibrio
ε: Campylobacter, Helicobacter
Sterilisation
Removal of all microorganisms
Commercial sterilisation
Removal of microorganisms in food which may cause diseases
Disinfection
Removal of common microorganism from surfaces
Pasteurisation
Definition: Controlled heating to kill pathogens and spoilage microbes, but not all microbes
Example: Milk (heated at 72°C for 15 sec)
Purpose: Safe to drink, but still contains some microbes → NOT sterilisation
Filtration
Definition: Physical removal of microbes by passing liquid or air through a filter with tiny pores
Example: Sterilising heat-sensitive liquids (antibiotics, vaccines)
Note: Can remove bacteria, but viruses may pass through unless ultra-filters are used
Refrigeration
Definition: Cooling slows down microbial metabolism and growth
Example: Food storage at 4°C
Effect: Slows growth, doesn’t kill
Lyophilisation (Freeze-drying)
Definition: Combination of freezing and drying to preserve microbes or food
Process: Frozen → water removed by vacuum
Effect: Keeps cultures/food stable for years. Microbes are dormant, not dead
Example: Preservation of bacterial cultures, coffee
Desiccation (Drying)
Definition: Removal of water → microbes cannot grow or reproduce
Effect: Many survive and grow again when water is added
Example: Dried fruits, jerky
Osmotic Pressure
Definition: High salt or sugar concentration draws water out of microbial cells
Effect: Prevents growth, but not always lethal
Example: Salted fish, honey, jams
Methods of Moist Heat Control
Boiling (100 °C)
Kills most bacteria, fungi, protozoa, and viruses
But does not reliably kill endospores
Example: Disinfecting baby bottle
Autoclave (Steam under Pressure)
121 °C, 15 psi, 15 minutes
Steam under pressure reaches higher temperatures than boiling
Sterilises → kills all microbes, including endospores
Used for: surgical instruments, lab media, dressings, waste
Dry Heat Sterilisation
Kills microbes by oxidation (burning) instead of protein denaturation (like moist heat).
Methods:
Flaming, passing instruments (like inoculating loop) through a flame
Incineration, burning waste materials (medical dressings, carcasses)
Hot-air sterilisation (oven), 170 °C for 2 hours → sterilises glassware, metal instruments
Static
The growth of the micrograms has be stopped for now
Cidal
Microorganism has been killed and wont become alive again
MIC – Minimum Inhibitory Concentration
The lowest concentration of a drug that inhibits visible growth of a microorganism
MIC – Methods
Disc Diffusion
Paper discs with antibiotic are placed on agar inoculated with bacteria
Antibiotic diffuses outward → creates a zone of inhibition (clear area)
Larger zone = more effective drug
Qualitative: Sensitive, Intermediate, or Resistant
E-test (Epsilometer test)
Plastic strip with a gradient of antibiotic concentration placed on agar with bacteria
Elliptical zone of inhibition forms
The point where the zone edge meets the strip = the MIC value (in µg/mL)
More precise than disc diffusion
Broth Dilution Test
Bacteria are grown in liquid broth with different concentrations of antibiotic
The lowest concentration with no visible growth = MIC
Can also determine MBC (Minimum Bactericidal Concentration) if plated afterwards
Antimicrobial drugs
Treatment of microorganisms within infected host is chemotherapy
These drugs must be selectively toxic (not to kill the host)
Narrow spectrum affects a specific type of microbe
Broad spectrum is active against many different types of microbes
Site and mode of action
Inhibition of cell wall synthesis
Interference with synthesis of peptidoglycan by preventing elongation of the polymer
Interference with protein synthesis by binding to ribosomes and preventing attachment of t-RNA and therefore arresting translation
Injury to plasma membrane
Inhibition of nucleic acid synthesis
Interference with metabolic function
Antiviral drugs
Antiprotozoal drugs
Anthelminthics
Effects of antimicrobial agent use
Destruction of the microbe (cidal effect)
Stops microbes growth (static effect)
Rise of antibiotic resistance
Occurrence of superinfections
Combination
Synergism= enhanced effect
Antagonism= interfere with the others action
No effect
Antibiotic resistance
Acquisition= the microbes have the gene to protect themselves
Mutation= they have under gone a change which activate the gene
Mechanisms of antibiotic resistance
Organism lacks structure an antibiotic inhibits.
Organism impermeable to an antibiotic
Organism inactivates an antibiotic
Organism modifies a target structure of an antibiotic
Organism alters a biological pathway an antibiotic blocks
Organism actively pumps out the incoming antibiotic
Define
Colonisation
Pathology
Etiology
Pathogenesis
Infection
Disease
Colonisation: occupation of specific niches of the host by harmless or symbiotic microorganisms (normal flora)
Pathology: the study of disease
Etiology: the cause of a disease
Pathogenesis: the development of disease
Infection: invasion of the body by pathogens (disease may or may not be the result. the invading microbe may exist in equilibrium with the host defence systems and the host becomes a carrier (typhoid Mary)
Disease: an abnormal state in which the body is not performing normal functions
Define
Commensalism
Mutualism
Parasitism
Opportunistic Infection
Commensalism: one organism benefits and the other is unaffected
Mutualism: both organisms benefit
Parasitism: one organism benefits to the detriment of the other
Opportunistic infection: changes in the normal flora by deodorants, caustic soaps, antibiotics or change in the health status can lead to opportunistic infections
Define
Synergism
Antagonism
Synergism: two microbes work together to make a disease worse
Antagonism: normal microbiota protect us by blocking harmful microbes
Koch's postulates:
Isolate same agent of disease from every infected tissue
Purify in culture
Re-create the disease in a healthy animal using purified agent
Demonstrate that re-created disease is due to the same agent
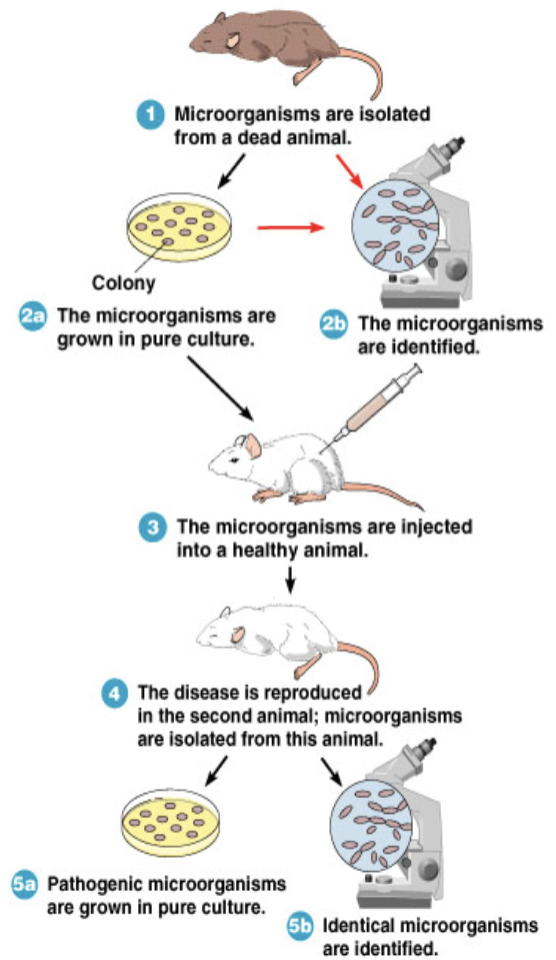
Exceptions to Koch's Postulates
Organisms that do not grow well or at all on artificial medium organisms
Some disease symptoms can be caused by several different
Modes of Transmission
Communicable diseases
Transmitted from person
TB, Hep B and C
Contagious diseases
Highly infectious, fast spreading from person to person
Chicken pox, measles, flu
Non-communicable diseases
Accidentally introduced into host
Tetanus
Define
Local Infection
Systemic Infection
Focal Infection
Local infection= small area of the body
Systemic= most of the body is affected by spreading organism
Focal infection= spread via lymph or blood system to other parts of the body.
Define
Bacteraemia
Veremia
Septicaemia
Toxaemia
Bacteraemia is presence of bacteria in blood
Viremia is presence of virus in blood
Septicaemia is multiplication of bacteria in blood
Toxaemia is presence of toxin (like tetanus) in blood
SARS-CoV: A classic zoonosis
Inter-species contact:
Chinese wholesale animal markets house >100 species simultaneously
Cross-species transmission
Many species are susceptible
civets, ferret badgers, monkeys, rodents, cats, pigs
Sustained transmission
Civet-to-civet and human-to-human transmission documented
Adaptation
Spike protein binds to host cell receptors and determines host specificity
Rapid evolution following initial infections in civets and people
SARS-CoV from initial outbreak (2002) showed greater affinity for human receptors than civet viruses or later (2004) mild human cases
Disease development
Incubation period
Time between invasion of the host and onset of symptoms
Prodromal period
Onset of mild general symptoms
Period of illness
Acute phase of disease with maximum symptom display
Decline period
Easing of the symptoms (secondary infection risk)
Convalescence
Period to full recovery
EPIDEMIOLOGY
The study of where, when and how often specific diseases occur and how they are transmitted in host populations
Fathered by John Show in 1848-1849, he monitored epidemic of cholera in London
Descriptive epidemiology, (collection of data)
Retrospective - collecting information of past cases
Prospective - studying healthy individuals who are likely targets of next outbreak and then following the cases as they become subjects of disease
Analytical epidemiology
Analysing collected data to determine the probable cause
Case control - comparing data from affected and non-affected individuals during disease period/outbreak to determine predisposing factors such as age, sex, genotype or location (backwards)
Cohort - comparing matched groups of individuals, with and without disease history (forwards)
Experimental epidemiology
Hypothesis followed by testing the hypothesis by differential treatment of matched groups, say with particular drug and placebo
Case reporting is very important in every study
Mortality - incidents of death due to a particular disease
Morbidity - incidence of disease in the population
Define
Pathogenicity
Virulence
Portals of Entry
Pathogenicity= the ability to cause disease by overcoming host defences
Virulence= degree of pathogenicity
Portals of entry= entry point of pathogen into the host mucus membrane, skin, parenteral or subcutaneous deposition (via vector)
Mucous Membrane
The most common entry for microbes are the reparatory and gastro intestinal mucosa
Then the genitio urinary tract and the conjunctiva
Cutaneous: Skin
Cuts or abrasions
Hair follicles
Sweat glands
Invaders such as hookworm larvae can bore through intact skin
Some fungi can utilise keratin as a food source and infect the skin
Parenteral
(below the tissue)
Bites, injections, cuts
Preferred portal of entry
To cause disease, the microorganism has to enter a host in a specific way, otherwise it becomes subject to host defences
Eg Salmonella typhi will cause disease when ingested but not when enters through skin
Streptococci can cause pneumonia when inhaled, but no disease occurs if they are ingested
Infectious dose
The greater the number of invading cells, the greater is the chance of disease
ID50= Infected 50%
LD50= Kills 50%
Pathogenicity Determinants
Adherence
Adherence
Ability to attach to host tissues
Adhesins may be non-specific structures on the cell wall such as glycoproteins, lipoproteins and LPS or specifically encoded structures such as fimbriae
The receptors on the host cells are usually sugars, these are NOT present for the benefit of the microbes
Some adhesin, receptor reactions are so specific that microbes can only attach and penetrate a particular type of cells only
Eg Neisseria gonorrhoeae fimbriae can only attach to columnar epithelial cells.
Pathogenicity Determinants
Capsules
Capsules
Glycocalyx layer surrounding the cell wall forms a capsule
It resists phagocytosis by macrophages, by preventing adherence
Host defence then must produce antibodies to the capsule antigen which in turn opsonise the capsule and allow phagocytosis
Production of capsules is a known virulence factor
Capsules are not always related to virulence, can be utilised by bacteria to form biofilms
Degradative enzymes
Leucocidins: destroy leucocytes
Haemolysins: destroy red blood cells
Coagulases: clot fibrinogen in blood , avoid phagocytosis (hide)
Kinases: break down fibrin, dissolve blood clots which would isolate infection (spread)
Hyaluronidase: hydrolyses connective tissue
Collagenase; breaks down collagen, causes major tissue damage
Necrotising factors; lecithinase, proteases, siderophores etc
Invasion into host cells
Attachment of bacterial cells induces production of proteins called invasins (invasols)
Alter host cell membrane
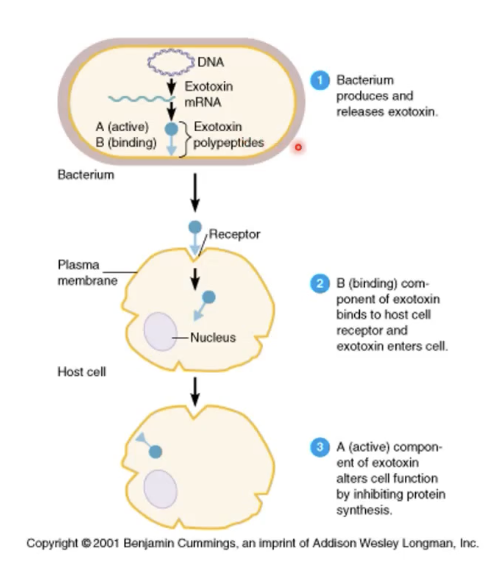
Exotoxins
Living bacteria
Damage and kill cells directly Cytotoxins (diphtheria and erythrogenic)
Neurotoxins
Botulinum toxin is produces Clostridium botulinum
Blocks release of neurotransmitter acetylcholine and prevents muscle contraction (flaccid paralysis)
Tetanus toxin is produced by Clostridium tetani
Blocks Glycine release and muscle relaxation (lockjaw)
Enterotoxins
Intestinal system
Poopy water
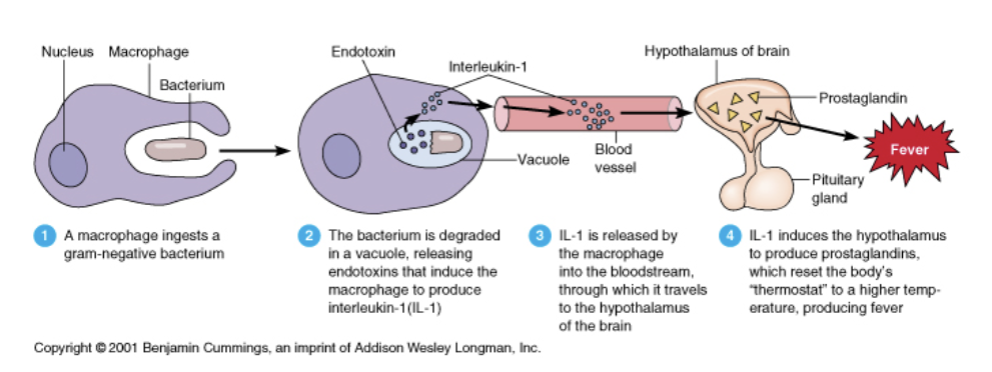
Endotoxins
Endotoxins are part of cell wall of gram neg bacteria
Causes pyrogenic response and septic (or endotoxic shock)
Plasmids and lysogenic bacteriophage
Can carry virulence factors, genes encoding toxins fimbriae, degradative enzymes
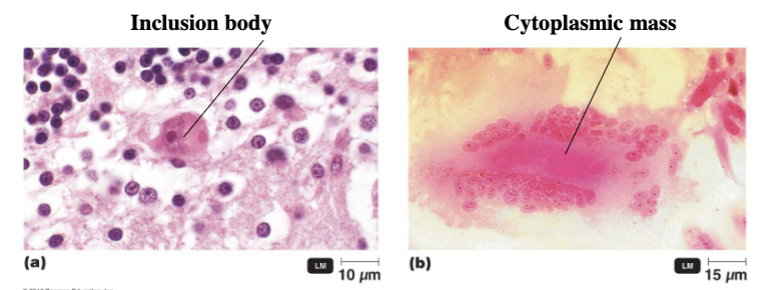
Cell damage of host cell by viruses - cytopathic effect
Some effects that viral infection has on the host cells are very specific to the infecting virus
Arrest of cell cycle
Formation of inclusion bodies
Formation of syncytium-fused cells (fused cells)
Flagella
Long filamentous appendage that move bacteria
Monotrichouse= single at one pole of the cell
Amphitricha's= single at both poles of the cell
Lophotrichouse= two or more at one pole of the cell
Peritrichous= distributed all over the cell
Axial Filaments (endoflagella)
Fimbriae and Pili
Fimbriae is used for attachment to host tissue
Pili is involved in motility and transfers plasmid DNA between bacteria